Published online Apr 28, 2021. doi: 10.3748/wjg.v27.i16.1738
Peer-review started: January 10, 2021
First decision: February 11, 2021
Revised: February 15, 2021
Accepted: March 22, 2021
Article in press: March 22, 2021
Published online: April 28, 2021
Processing time: 100 Days and 16.4 Hours
The coronavirus disease 2019 (COVID-19) outbreak has drawn the scientific community's attention to pre-existing metabolic conditions that could aggravate the infection, causing extended viral shedding, prolonged hospitalization, and high death rates. Metabolic dysfunction-associated fatty liver disease (MAFLD) emerges as a surrogate for COVID-19 severity due to the constellation of metabolic alterations it entails. This review outlines the impact MAFLD exerts on COVID-19 severity in obese subjects, besides the possible mechanistic links to the poor outcomes. The data collected showed that MAFLD patients had poorer COVID-19 outcomes than non-MAFLD obese subjects. MAFLD is generally accompanied by impaired glycemic control and systemic arterial hypertension, both of which can decompensate during the COVID-19 clinical course. Also, MAFLD subjects had higher plasma inflammatory marker concentrations than non-MAFLD subjects, which might be related to an intensified cytokine storm syndrome frequently associated with the need for mechanical ventilation and death. In conclusion, MAFLD represents a higher risk than obesity for COVID-19 severity, resulting in poor outcomes and even progression to non-alcoholic steatohepatitis. Hepatologists should include MAFLD subjects in the high-risk group, intensify preventive measurements, and prioritize their vaccination.
Core Tip: It is notorious that obesity represents a risk for coronavirus disease 2019 (COVID-19) severity. However, COVID-19 often causes liver alterations or provokes the progression of pre-existing liver diseases. This review outlines the role of metabolic dysfunction-associated fatty liver disease in COVID-19 severity. The evidence available thus far supports the notion that metabolic dysfunction-associated fatty liver disease represents a more intense risk than obesity for hospitalization, extended viral shedding, and death. A pro-inflammatory state with inflammasome activation, implying increased susceptibility to cytokine storm syndrome, underlies these findings and emerges as, in addition to massive vaccination of subjects with liver diseases, potential targets for therapeutic strategies.
- Citation: Vasques-Monteiro IML, Souza-Mello V. Coronavirus disease 2019 severity in obesity: Metabolic dysfunction-associated fatty liver disease in the spotlight. World J Gastroenterol 2021; 27(16): 1738-1750
- URL: https://www.wjgnet.com/1007-9327/full/v27/i16/1738.htm
- DOI: https://dx.doi.org/10.3748/wjg.v27.i16.1738
The infection caused by the coronavirus severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [coronavirus disease 2019 (COVID-19), Beta-coronavirus genus, Coronaviridae family] was declared as a pandemic in March 2020 by the World Health Organization and caused an unprecedented burden to health systems worldwide because of its harmful evolution to severe acute respiratory syndrome[1,2]. Although most cases are asymptomatic, this fact facilitated the rapid viral spread worldwide, resulting in overloaded hospitals due to the extended hospitalizations and the frequent need for mechanical ventilation that severe COVID-19 requires[3,4]. From December 2019 to February 14, 2021, COVID-19 caused almost 2.4 million deaths, and more than 108 million confirmed cases in 222 countries or territories[1].
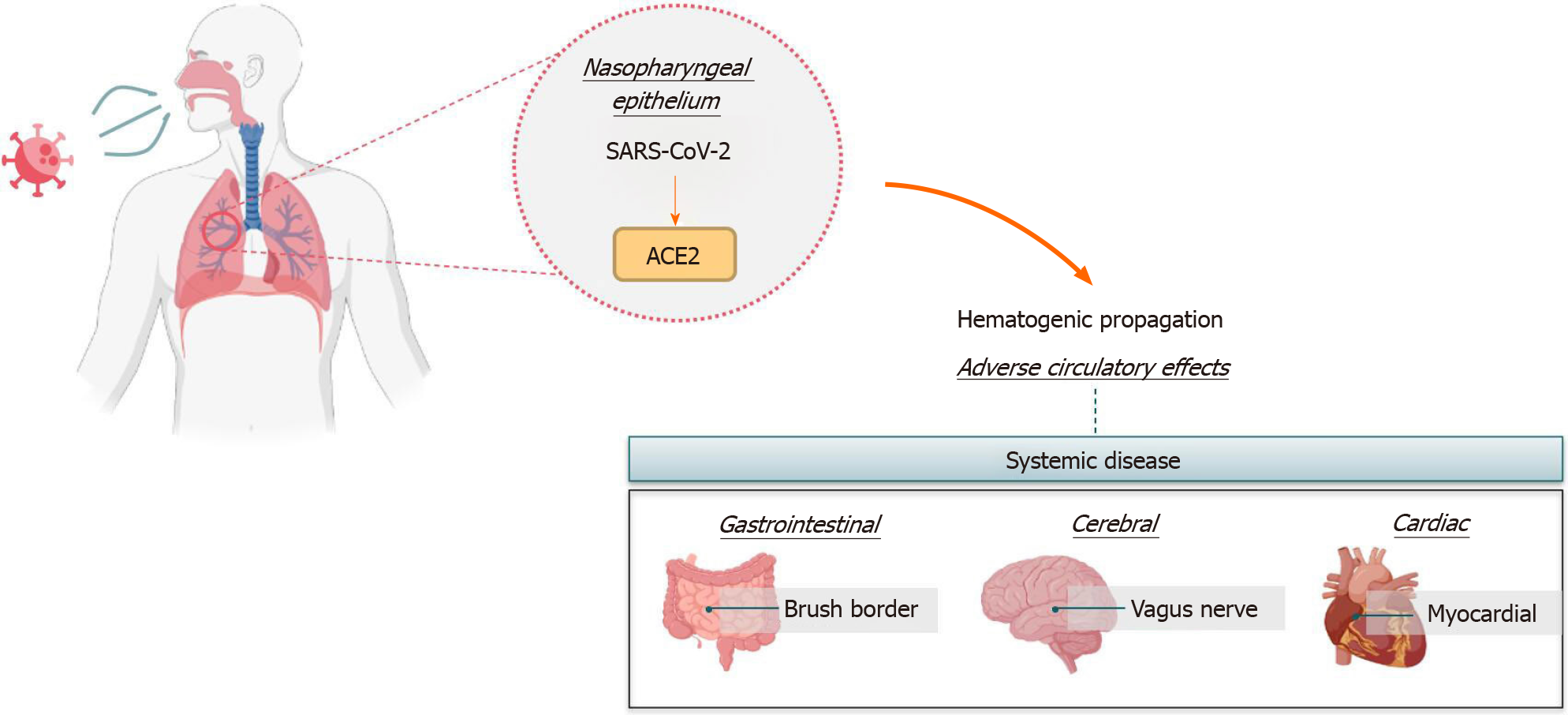
The SARS-CoV-2 relies on binding to the angiotensin-converting enzyme 2 (ACE2) receptor to enter target cells and start viral shedding[5]. Much as the infection frequently happens through the nasopharyngeal epithelium and has the lungs as the chief target with respiratory commitment, COVID-19 represents a systemic disease with adverse cardiac, circulatory, and cerebral outcomes after hematogenic propagation and virus neurotropism for the vagus nerve that links lungs to the central nervous system[6-8]. Of note, the presence of ACE2 receptors in the brush border of intestinal enterocytes and cholangiocytes makes possible the occurrence of gastrointestinal symptoms and aggravation of pre-existing metabolic diseases[9,10]. Figure 1 summarizes the most common infection and propagation pathways of SARS-CoV-2 with adverse effects in the human body.
In this regard, overweight emerged as a high-risk factor to hospitalization due to COVID-19, surpassed only by age ≥ 65 in the New York population[11], emphasizing the high risk of severe COVID-19. Body mass gain yields metabolic alterations that start in the adipose tissue, with hypertrophy and hyperplasia as attempts to buffer excessive energy intake by fat storage[12]. In the long run, adipogenesis capacity exhausts, and the existing enlarged adipocytes trigger lipolysis to manage a continuous lipid accumulation through lipogenesis[13,14]. At this stage, excessive non-esterified fatty acids (NEFAs) are diverted to other organs like the liver and drive steatosis[15].
Hepatic steatosis is known as the hepatic manifestation of metabolic syndrome. Hence, metabolic disturbances such as insulin resistance, systemic arterial hypertension, and meta-inflammation, typical from obesity, coexist with this hepatic impairment[15,16]. Therefore, it was recently renamed metabolic dysfunction-associated fatty liver disease (MAFLD) as it represents better the constellation of metabolic impairments involved in its etiology than the former acronym non-alcoholic fatty liver disease[17].
MAFLD in obesity comprises lipotoxic effects on the liver by proinflammatory adipokines that influence hepatic energy metabolism in an endocrine fashion[18]. The inflamed adipose tissue has been linked to enhanced viral systemic spread, entry, and viral shedding in COVID-19 obese subjects[19]. This hypothesis complies with an intensified cytokine storm in obese patients with COVID-19, explaining the poor outcomes[20].
Among the metabolic impairments caused by excessive body fat, pre-existing MAFLD can result in COVID-19 patients being more prone to hospitalization and worsening metabolic conditions[21]. This review outlined the impact MAFLD exerts on COVID-19 severity in obese subjects in addition to the possible mechanistic links to poor outcomes. The information gathered relating to COVID-19 was that available on PubMed from the beginning of the pandemic until the end of 2020.
MAFLD is the most common chronic hepatic disease worldwide. Its global prevalence is around 25%, with the highest prevalence in the Middle East (31.79%) and South America (30.45%)[22]. MAFLD is not a disease exclusive of obesity, but obese subjects fall victim to fatty liver more frequently, as their insulin-resistant and proinflammatory adipokine profile converge to the accumulation of ectopic fat[18,23]. Recent evidence shows the presence of obesity among 51.34% of MAFLD patients and 81.83% of patients with non-alcoholic steatohepatitis (NASH)[22]. Although MAFLD silently initiates without symptoms, its harmful progression towards NASH (with hepatic fibrosis), cirrhosis, or hepatocellular carcinoma challenges the scientific community to understand its metabolic basis.
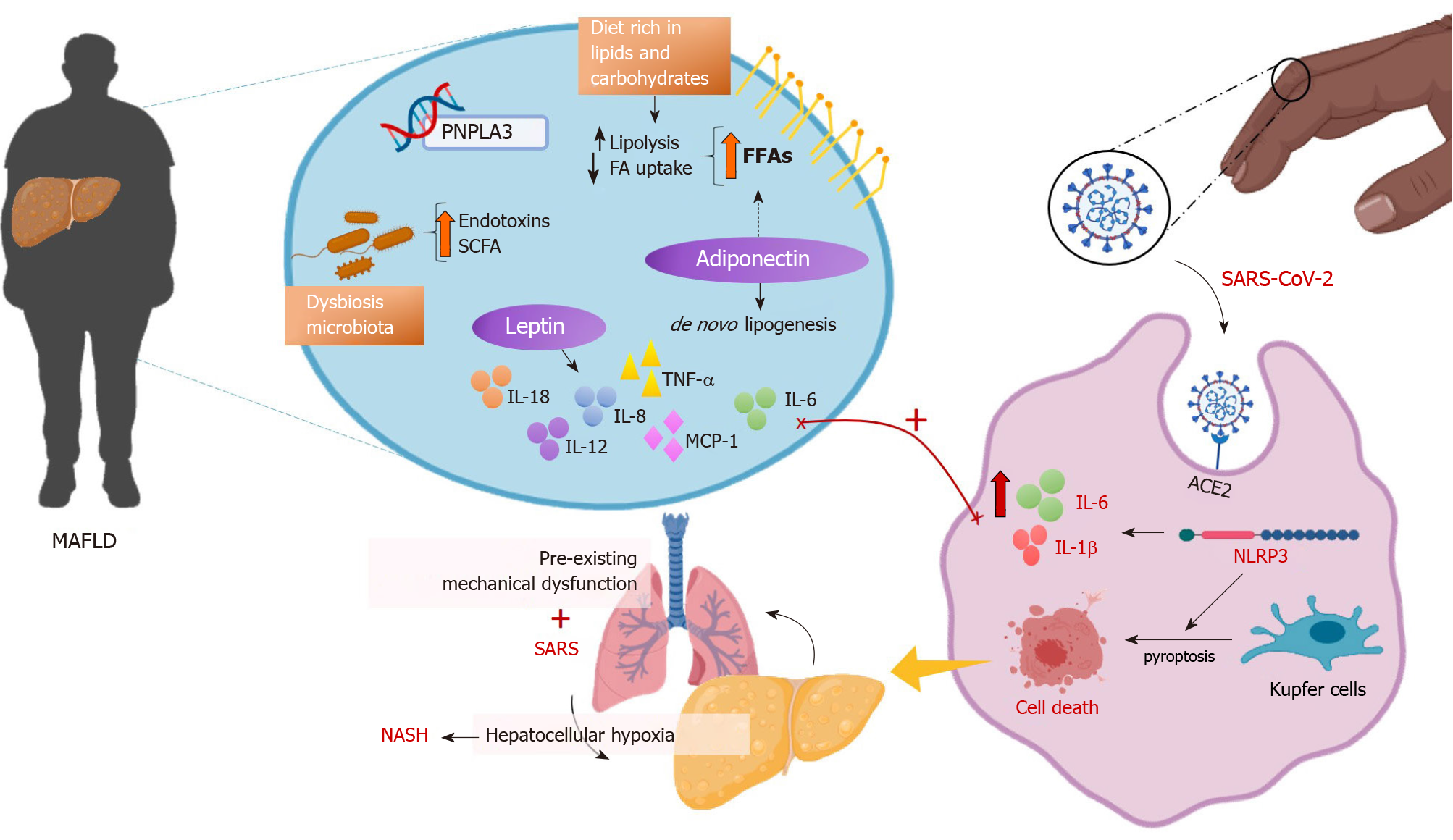
The pathogenesis of fatty liver is multifactorial and linked to diet, metabolic factors, intestinal microorganisms, and genetics. Exposure of hepatocytes to high levels of lipids and carbohydrates, usually included in the diet of obese individuals, leads to glucolipotoxicity and predisposes to MAFLD. Excessive circulating NEFAs come from accelerated lipolysis and reduced fatty acid uptake in subcutaneous adipose tissue, triggering ectopic fat accumulation (in the liver, skeletal muscle) and, therefore, insulin resistance in multiple organs[24]. The release of NEFAs from dysfunctional and insulin-resistant adipocytes causes lipotoxicity, induced by the ectopic accumulation of toxic metabolites stemmed from triglycerides. Hence, inflammatory pathways are activated, and cellular dysfunction occurs with liver incapacity to eliminate excessive NEFAs, ending up in lipoapoptosis, an essential feature of NASH[18].
Hepatic steatosis comprises approximately 60% of hepatic triglycerides from adipose tissue, 25% from de novo lipogenesis and 15% from dietary lipids[25]. Moreover, visceral adipose tissue is more closely related to the fatty liver than subcutaneous adipose tissue, possibly because the former is more resistant to insulin than the latter[26]. Increasing evidence shows that during adipose tissue expansion in obesity, there are changes in the expression and secretion of adipokines, favoring pro-inflammatory mediators for the development of MAFLD, progression to NASH, and possible development of liver cirrhosis[27]. Leptin and adiponectin are the adipokines widely described in the literature as influences on fatty liver development.
In animal models of MAFLD, leptin seems to have a double action: It can protect from hepatic steatosis, at least in the early stages of the disease, but it also can act as an inflammatory and fibrogenic factor when the disease persists or progresses, that is when the mechanisms of counterweight do not limit it[28-30]. In this sense, leptin can directly increase the production of pro-inflammatory cytokines, such as tumor necrosis factor (TNF)-α, interleukin (IL)-6, IL-12, and IL-18, the chemokines IL-8 and monocyte chemoattractant protein 1, and the lipid mediators prostaglandin E2, leukotrienes, and LTB4, being responsible for the noxious MAFLD progression[26]. Persisting hyperleptinemia promotes liver inflammation and fibrosis as the disease progresses to NASH.
On the contrary, adiponectin decreases as the fat mass increases. At physiological conditions, adiponectin exerts an anti-steatotic effect on hepatocytes by increasing beta-oxidation, while decreasing gluconeogenesis, fatty acid input to the liver, and de novo lipogenesis. Furthermore, high molecular weight adiponectin isoform has anti-inflammatory properties like TNF-α blockade and downregulation, resulting in insulin resistance alleviation[29]. In the case of positive energy balance and overweight onset, this critical balance is disrupted towards the side of TNF-α, contributing to chronic low-grade inflammation, insulin resistance, and MAFLD[26]. In humans, patients with fatty liver exhibit low adiponectin concentrations, whereas control subjects show high adiponectin concentrations. However, the adiponectin concentrations are even lower in patients with NASH than in MAFLD. It can be argued that, initially, adipokine actions can limit hepatic steatosis, but as adipose tissue expands, adipokine changes become harmful and contribute to MAFLD progression[18].
An innovative concept proposes that the gut-liver axis plays a crucial role in the pathogenesis and progression of MAFLD[31]. Although there are some controversies, animal and human studies show that gut microbiota from obese subjects comprises an increase in the relative abundance of firmicutes followed by a decrease of bacteroidetes[32]. Moreover, a higher prevalence of gram-negative bacteria, such as proteobacteria, and reduced phylum-level diversity are usual features in non-alcoholic fatty liver disease patients[33]. Changes in the gut microbiota in obesity disrupt the intestinal endothelial barrier, eliciting systemic bacterial translocation and hepatic inflammation by microbiota-related endotoxins and short-chain fatty acids that reach the liver through the portal vein[26].
Concerning a possible genetic predisposition to MAFLD, the adipose tissue of obese patients with fatty liver has upregulation of pro-inflammatory genes and macrophages-producing cytokines compared to obese subjects that do not develop MAFLD[34]. This observation raises the hypothesis of a genetic polymorphism that explains why some obese individuals develop MAFLD, while others do not[35]. Briefly, an allele in the PNPLA3 gene is a surrogate for the MAFLD onset and hepatic inflammation[36]. Other genes like FDFT1, TM6SF2, GCKR, and MBAT7 have already been linked to the progression of MAFLD[37]. However, the complete identity of "MAFLD related to genetics" still needs to be further investigated.
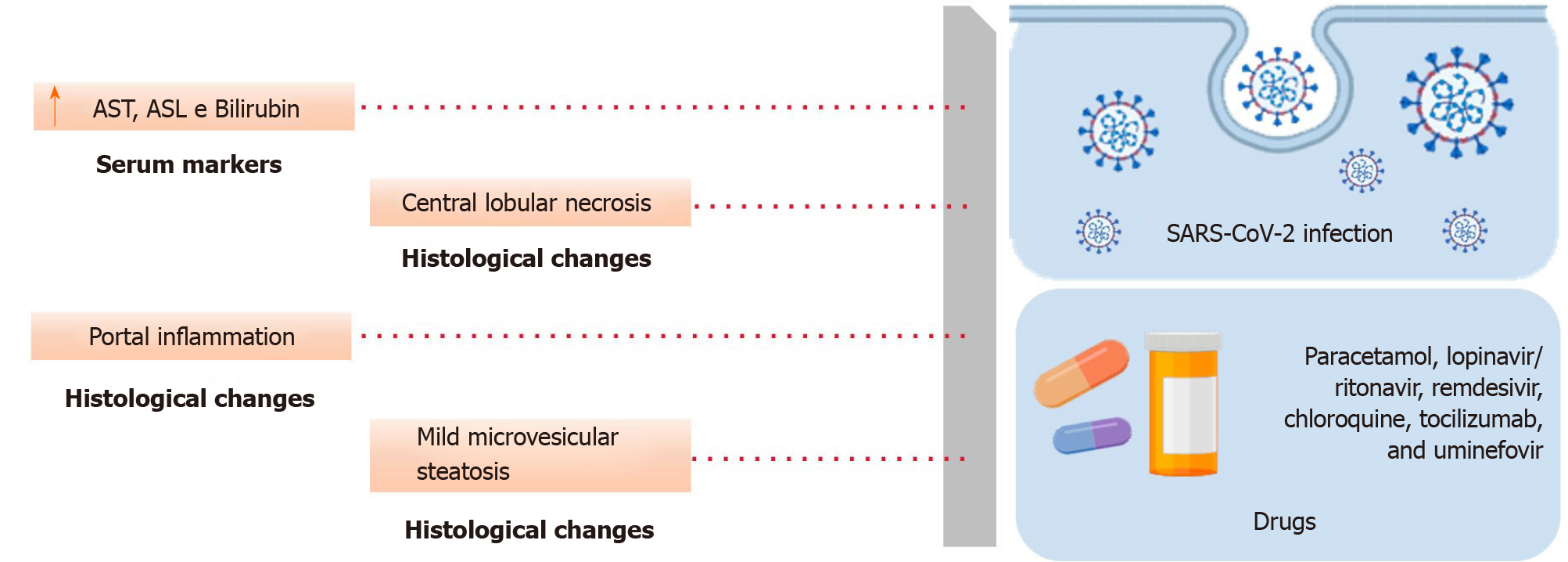
The clinical course of COVID-19 encompasses elevated aspartate aminotransferase and alanine aminotransferase combined with a mild rise in bilirubin levels[38]. A study in China found that 37.3% of patients had an abnormal liver function at hospital admission[39]. In Mexico, 96.8% of patients (n = 150) had a liver impairment but without an association between abnormal liver function tests and mortality[40]. A Chinese study has suggested aspartate aminotransferase as a promising marker to predict hospital stay, with higher values suggestive of prolonged periods. However, this information might not apply to different populations and should be better addressed[41].
Concerning histological liver changes, a post-mortem study in Belgium revealed histological alterations in all 14 deceased COVID-19 patients, with central lobular necrosis and portal inflammation as the most frequent hepatic histological damages[42]. In agreement with this, COVID-19 patients with acute respiratory distress syndrome showed mild microvesicular steatosis and lobular and portal activity in China[43]. The most common post-mortem histological findings in 40 North Americans that died from COVID-19 were fatty liver (75%), mild acute hepatitis (50%), and portal inflammation (50%). However, the fat distribution pattern was not typical of MAFLD and might stem from the administration of steroids during hospitalization[44].
In line with these previous findings, a Chinese study showed 96% of hepatocellular liver injury among COVID-19 hospitalized subjects, with 50% of them presenting liver injury at hospital admission and 75.2% showing liver injury during hospital stay[45]. This observation emphasizes that not only could the pre-existing hepatic disease produce a severe form of COVID-19, but the virus itself can trigger liver damage. Indeed, it is hard to distinguish whether liver injury during hospital stay stemmed from the COVID-19 infection or some drugs used as attempts to stop viral replication[45,46]. Hepatotoxic effects of paracetamol, lopinavir/ritonavir, remdesivir, chloroquine, tocilizumab, and uminefovir can cause microvesicular steatosis and mild hepatic inflammation[47]. These findings are depicted in Figure 2.
MAFLD is considered a pre-existing condition that turns individuals more vulnerable to COVID-19 infection and virus-related complications. Furthermore, these patients may have an increased risk of MAFLD to NASH progression, a long-term consequence of viral infection[48]. As MAFLD is frequently associated with overweight/obesity, it is sometimes hard to separate the single effect each one exerts on COVID-19 severity. Herein, we outlined the most recent evidence after almost 1 year from the beginning of the pandemic.
The presence of MAFLD could predict severe COVID-19 (more than 2-fold prevalence) and critical illness in patients younger than 60 years old in China[49], in addition to longer viral shedding time (17.5 d vs 12.1 d on average)[45]. Furthermore, Chinese MAFLD patients without type 2 diabetes showed a 4-fold high risk for severe COVID-19, and a 12% increase in the risk for severe COVID-19 for each 1-unit augmentation in body mass index[50]. Obesity conferred a 6 times greater risk of severe infection in Chinese patients with MAFLD [odds ratio (OR) did not adapt 5.77, P = 0.029]. The association of obesity with COVID-19 severity remained after adjusting for many factors (age, sex, smoking habits, diabetes, hypertension, and dyslipidemia, OR compatible 6.32, P = 0.033)[51].
Conversely, a study considering a large sample in the United States pointed out MAFLD/NASH as a greater risk for hospitalization than obesity itself[52]. In line with this, increased rates of COVID-19 clinical severity among MAFLD patients have been observed even after controlling for obesity, suggesting that the effect of MAFLD on disease severity may be more expressive than increased body mass index[53]. MAFLD/NASH might have a significant role in maximizing chronic inflammation and hypercoagulability, emerging as a pivotal surrogate for severe COVID-19 cases[52].
A study in Brazil showed that hepatic steatosis was found in computed tomography (CT) among 31.9% of COVID-19 positive patients, while only 7.1% of COVID-19 negative subjects showed hepatic steatosis. The OR was 4.698 after adjusting for age and sex, but they did not evaluate the severity or poor clinical outcomes[54]. In this context, a meta-analysis carried out with six Chinese studies with 1293 participants revealed that patients with COVID-19 showed a high percentage of MAFLD and increased risk of COVID-19 severity, indicating a need for intensive monitoring of MAFLD patients with COVID-19[55].
In agreement with this, MAFLD entails a constellation of metabolic abnormalities that can be aggravated during viral infection. Through univariate analysis, it was shown that metabolic syndrome leads to a higher cumulative incidence of COVID-19, with liver damage being the most associated with this outcome[56]. Moreover, COVID-19 can cause hypoglycemia or hyperglycemia, compromising glycemic control due to sedentarism, anxiety, or viral tropism to pancreatic tissue[57]. Continuous monitoring of blood glucose is encouraged as hypoglycemia should be avoided, and glycemia should not exceed 180 mg/dL or 10 mmol/L in COVID-19 patients. MAFLD patients commonly show hypertension, and surveillance of medication and blood pressure levels can avoid shock in severe COVID-19 cases[58].
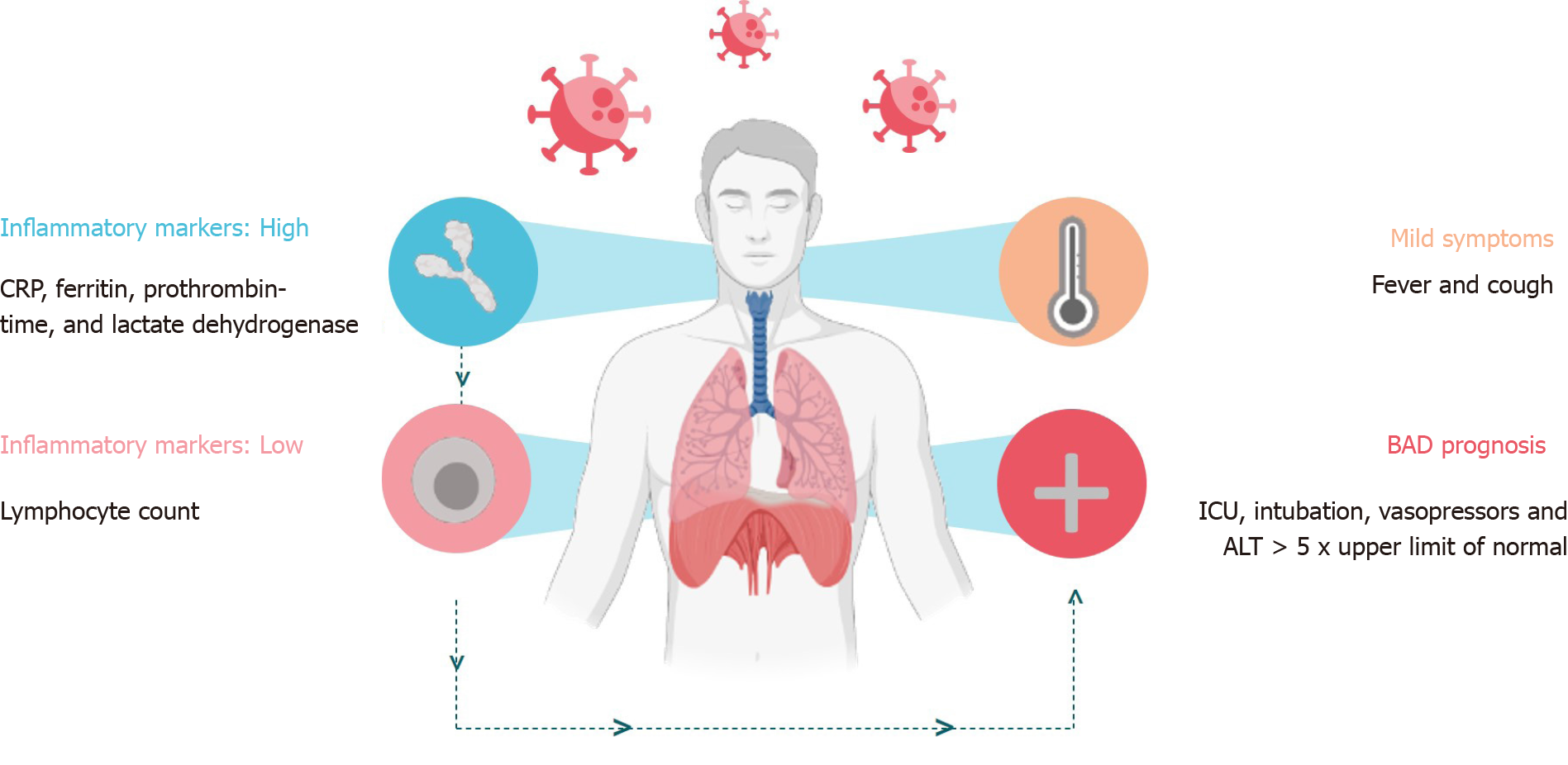
Despite showing similar COVID-19 symptoms to non-MAFLD, fever in 66.8% and cough in 55.7% of patients[39], MAFLD patients showed higher chances of intensive care unit admission (intensive care unit, OR: 1.60), intubation (2.51), need for vasopressors (1.22), and alanine aminotransferase > 5 times upper limit of normal (2.12)[59]. In univariate analyses, when compared with patients without chronic liver disease, subjects with MAFLD had significantly higher rates of intensive care unit admission (50.9% vs 35.2%, P = 0.0095) and need for mechanical ventilation (49.1% vs 30.4%, P = 0.006)[53].
A possible explanation for increased COVID-19 severity due to MAFLD includes higher C reactive protein (CRP) (107 vs 91.2 mg/L, P = 0.05) concentrations in COVID-19 patients with MAFLD than controls without MAFLD in London[60]. This favored pro-inflammatory state can result in high death rates, as MAFLD patients who died during hospitalization had higher concentrations of inflammatory markers like ferritin[61], prothrombin time, and lactate dehydrogenase than patients with MAFLD who survived hospitalization[60]. Notably, the combination of high CRP levels with low lymphocyte count predicted prolonged hospital stay (median 23 vs 18 d; P = 0.037) and a higher proportion of severe COVID-19 (33.3% vs 14.7%, P = 0.007) compared to non-obese patients[50]. Figure 3 outlines the mild symptoms and the factors that lead to severe forms of COVID-19.
Concerning imaging exams and COVID-19 prognosis in MAFLD patients, a CT study in the Mexican population proposed the liver to spleen ratio (CTL/S) as a surrogate for the diagnosis of MAFLD in COVID-19 patients, given that spleen does not store fat. Both organs are visualized in the CT performed to evaluate the degree of pulmonary commitment because it shows the upper abdomen, and the CTL/S ≤ 0.9 indicated the presence of fatty liver. Hepatic steatosis was associated with severe COVID-19 pneumonia, and CTL/S could be a substantial aid to estimate the prognosis of COVID-19 in MAFLD patients[62].
A recent systematic review evaluating clinical studies from China, Israel, and the United States showed that the presence of hepatic steatosis is a predictor for symptomatic and severe COVID-19, even after the adjustment for obesity presence (OR: 2.358, P < 0.001)[63]. Moreover, COVID-19 infection in pre-existing chronic liver disease patients from 13 different Asian countries caused decompensation in 20% of the cirrhotic patients with high mortality. Among MAFLD patients, the presence of comorbidities like obesity and type 2 diabetes entailed a risk of liver injuries due to COVID-19 infection[64]. In agreement, a recent Indian study using non-COVID-19 cirrhotic patients as controls showed that COVID-19 infection resulted in a 100% mortality rate in patients with acute-on-chronic liver failure in comparison with 53.3% in acute-on-chronic liver failure controls. The poor outcome that COVID-19 imposes on cirrhotic patients includes the need for mechanical ventilation and urges physicians and hepatologists to consider patients with chronic liver diseases as a high-risk group for COVID-19 and guarantee rigorous preventive measures[65].
The post-mortem evaluation of the livers from people that died of COVID-19 often reveals that the virus causes inflammatory and immune-mediated liver damage rather than cytopathic harm[43]. The observation of different immune cell exudates near the portal area reinforces this hypothesis and links hepatic damage to the cytokine storm syndrome (CSS), which emerges as a promising explanation for the increased severity of COVID-19 in obese patients with MAFLD[66,67].
To put it simply, CSS comprises the activation of inflammasomes and the following release of pro-inflammatory cytokines like IL-1β and IL-6[68,69]. The inflammasomes are complexes of proteins that reside in macrophages, activated by tool-like receptors binding to a pathogen-associated molecular pattern or damage-associated molecular patterns[70,71]. The liver has the largest macrophage reservoir in the body (the Kupfer cells); and, therefore, the activation of the NLR family pyrin domain containing 3 (NLRP3) inflammasome can damage this organ and acts as a promising marker of COVID-19 severity in obese patients[43,72].
The adipose tissue expansion in obesity triggers fatty liver and inflammasome activity by lipotoxicity[73]. The dramatic changes that adipose tissue macrophages undergo during weight gain (polarization to M1 state) reflect in the Kupfer cells that produce inflammatory chemokines and cytokines, generating hepatic insulin resistance and inflammation[74,75]. In this context, IL-6 emerges as a pivotal marker of COVID-19 worsening as it can trigger the CSS[76], besides being generally high in obese and MAFLD subjects[77].
It can be supposed that the obese patient with MAFLD before catching COVID-19 could show a maximized CSS, which might be linked to the increased need for longer hospitalizations and intensive care. Consistent with this suggestion, inflammasome activation elicits massive augmentation of pro-inflammatory cytokine concentrations and induces pyroptosis[78]. Cell death mediated by pyroptosis in macrophages relies on NLRP3 activation and provokes severe acute respiratory syndrome in COVID-19 patients, picturing a frame of aggravated disease by the CSS in MAFLD patients[79]. Furthermore, severe obese subjects can show serious infections in the lower respiratory tract due to mechanical dysfunction, which also makes them more prone to secondary infections[80].
Additional mechanisms related to the intensification of COVID-19 in MAFLD obese patients include the hepatocellular hypoxia in chronic liver diseases that leads to ACE2 overexpression[81]. Hence, these changes can cope with MAFLD progression towards NASH by the overexpression of ACE2 in endothelial cells and the consequent increased reactive oxygen species production, inflammatory pathways activated in the Kupfer cells, and peroxisome proliferator-activated receptor-alpha down-regulation with pro-lipogenic gene expression and steatosis maximization[82,83]. In this regard, the presence of hepatic steatosis before viral infection can amplify the symptoms of COVID-19 as the lipotoxicity sustains the activation of Kupfer cells and allows the progression to liver fibrosis. The main pathways involved with the severity of COVID-19 in MAFLD patients are depicted in Figure 4.
In conclusion, pre-existing MAFLD increases the risk of severe COVID-19 that requires hospitalization. MAFLD itself can represent an increased predisposition to CSS, and high CRP concentrations, NLRP3 activation, and IL-6 concentrations emerge as likely surrogates for the need for mechanical ventilation, with high death rates or evolution to NASH among survivors.
It is urgent to consider that MAFLD surpassed obesity as a risk factor to COVID-19 severity in populations with diverse genetic backgrounds. Therefore, MAFLD subjects should be ranked high-risk to catch COVID-19, submitted to rigorous preventive measurements, and classified as a prioritized group for vaccination.
The authors would like to thank all physicians, health professionals, and researchers for working uninterruptedly during pandemics. Your dedication helped to gather the information that saved millions of lives and resulted in vaccines in an unprecedented minimal time.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Brazil
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ma J S-Editor: Zhang L L-Editor: Filipodia P-Editor: Liu JH
| 1. | World Health Organization. WHO Coronavirus Disease (COVID-19) Dashboard 2021 [cited 19 January 2021]. Available from: https://covid19.who.int/. |
| 2. | Wu D, Wu T, Liu Q, Yang Z. The SARS-CoV-2 outbreak: What we know. Int J Infect Dis. 2020;94:44-48. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 771] [Cited by in RCA: 700] [Article Influence: 140.0] [Reference Citation Analysis (0)] |
| 3. | Albano D, Bertagna F, Bertoli M, Bosio G, Lucchini S, Motta F, Panarotto MB, Peli A, Camoni L, Bengel FM, Giubbini R. Incidental Findings Suggestive of COVID-19 in Asymptomatic Patients Undergoing Nuclear Medicine Procedures in a High-Prevalence Region. J Nucl Med. 2020;61:632-636. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 131] [Article Influence: 26.2] [Reference Citation Analysis (0)] |
| 4. | Goyal P, Choi JJ, Pinheiro LC, Schenck EJ, Chen R, Jabri A, Satlin MJ, Campion TR Jr, Nahid M, Ringel JB, Hoffman KL, Alshak MN, Li HA, Wehmeyer GT, Rajan M, Reshetnyak E, Hupert N, Horn EM, Martinez FJ, Gulick RM, Safford MM. Clinical Characteristics of Covid-19 in New York City. N Engl J Med. 2020;382:2372-2374. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1644] [Cited by in RCA: 1617] [Article Influence: 323.4] [Reference Citation Analysis (0)] |
| 5. | Zubair AS, McAlpine LS, Gardin T, Farhadian S, Kuruvilla DE, Spudich S. Neuropathogenesis and Neurologic Manifestations of the Coronaviruses in the Age of Coronavirus Disease 2019: A Review. JAMA Neurol. 2020;77:1018-1027. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 714] [Cited by in RCA: 654] [Article Influence: 130.8] [Reference Citation Analysis (0)] |
| 6. | Chigr F, Merzouki M, Najimi M. Autonomic Brain Centers and Pathophysiology of COVID-19. ACS Chem Neurosci. 2020;11:1520-1522. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 55] [Cited by in RCA: 60] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 7. | Ellul MA, Benjamin L, Singh B, Lant S, Michael BD, Easton A, Kneen R, Defres S, Sejvar J, Solomon T. Neurological associations of COVID-19. Lancet Neurol. 2020;19:767-783. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1512] [Cited by in RCA: 1393] [Article Influence: 278.6] [Reference Citation Analysis (0)] |
| 8. | Mitrani RD, Dabas N, Goldberger JJ. COVID-19 cardiac injury: Implications for long-term surveillance and outcomes in survivors. Heart Rhythm. 2020;17:1984-1990. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 193] [Cited by in RCA: 176] [Article Influence: 35.2] [Reference Citation Analysis (0)] |
| 9. | Hamming I, Timens W, Bulthuis ML, Lely AT, Navis G, van Goor H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol. 2004;203:631-637. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3643] [Cited by in RCA: 4149] [Article Influence: 197.6] [Reference Citation Analysis (0)] |
| 10. | Qi F, Qian S, Zhang S, Zhang Z. Single cell RNA sequencing of 13 human tissues identify cell types and receptors of human coronaviruses. Biochem Biophys Res Commun. 2020;526:135-140. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 523] [Cited by in RCA: 741] [Article Influence: 148.2] [Reference Citation Analysis (0)] |
| 11. | Petrilli CM, Jones SA, Yang J, Rajagopalan H, O'Donnell L, Chernyak Y, Tobin KA, Cerfolio RJ, Francois F, Horwitz LI. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study. BMJ. 2020;369:m1966. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1590] [Cited by in RCA: 1818] [Article Influence: 363.6] [Reference Citation Analysis (1)] |
| 12. | Gustafson B, Smith U. Regulation of white adipogenesis and its relation to ectopic fat accumulation and cardiovascular risk. Atherosclerosis. 2015;241:27-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 77] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 13. | Gustafson B, Hammarstedt A, Hedjazifar S, Smith U. Restricted adipogenesis in hypertrophic obesity: the role of WISP2, WNT, and BMP4. Diabetes. 2013;62:2997-3004. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 105] [Cited by in RCA: 115] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 14. | Saponaro C, Gaggini M, Carli F, Gastaldelli A. The Subtle Balance between Lipolysis and Lipogenesis: A Critical Point in Metabolic Homeostasis. Nutrients. 2015;7:9453-9474. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 265] [Cited by in RCA: 370] [Article Influence: 37.0] [Reference Citation Analysis (0)] |
| 15. | Cusi K. Role of insulin resistance and lipotoxicity in non-alcoholic steatohepatitis. Clin Liver Dis. 2009;13:545-563. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 181] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 16. | Cildir G, Akıncılar SC, Tergaonkar V. Chronic adipose tissue inflammation: all immune cells on the stage. Trends Mol Med. 2013;19:487-500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 189] [Cited by in RCA: 225] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 17. | Eslam M, Sanyal AJ, George J; International Consensus Panel. MAFLD: A Consensus-Driven Proposed Nomenclature for Metabolic Associated Fatty Liver Disease. Gastroenterology 2020; 158: 1999-2014. e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2367] [Cited by in RCA: 2205] [Article Influence: 441.0] [Reference Citation Analysis (1)] |
| 18. | Polyzos SA, Kountouras J, Mantzoros CS. Obesity and nonalcoholic fatty liver disease: From pathophysiology to therapeutics. Metabolism. 2019;92:82-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 453] [Cited by in RCA: 808] [Article Influence: 134.7] [Reference Citation Analysis (0)] |
| 19. | Ryan PM, Caplice NM. Is Adipose Tissue a Reservoir for Viral Spread, Immune Activation, and Cytokine Amplification in Coronavirus Disease 2019? Obesity (Silver Spring). 2020;28:1191-1194. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 193] [Cited by in RCA: 227] [Article Influence: 45.4] [Reference Citation Analysis (0)] |
| 20. | Dugail I, Amri EZ, Vitale N. High prevalence for obesity in severe COVID-19: Possible links and perspectives towards patient stratification. Biochimie. 2020;179:257-265. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 21. | Portincasa P, Krawczyk M, Smyk W, Lammert F, Di Ciaula A. COVID-19 and non-alcoholic fatty liver disease: Two intersecting pandemics. Eur J Clin Invest. 2020;50:e13338. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 108] [Cited by in RCA: 99] [Article Influence: 19.8] [Reference Citation Analysis (0)] |
| 22. | Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64:73-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5322] [Cited by in RCA: 7533] [Article Influence: 837.0] [Reference Citation Analysis (0)] |
| 23. | Xian YX, Weng JP, Xu F. MAFLD vs. NAFLD: shared features and potential changes in epidemiology, pathophysiology, diagnosis, and pharmacotherapy. Chin Med J (Engl). 2020;134:8-19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 73] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 24. | Magkos F, Mantzoros CS. Body fat redistribution and metabolic abnormalities in HIV-infected patients on highly active antiretroviral therapy: novel insights into pathophysiology and emerging opportunities for treatment. Metabolism. 2011;60:749-753. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 32] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 25. | Donnelly KL, Smith CI, Schwarzenberg SJ, Jessurun J, Boldt MD, Parks EJ. Sources of fatty acids stored in liver and secreted via lipoproteins in patients with nonalcoholic fatty liver disease. J Clin Invest. 2005;115:1343-1351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2112] [Cited by in RCA: 2595] [Article Influence: 129.8] [Reference Citation Analysis (0)] |
| 26. | Polyzos SA, Kountouras J, Mantzoros CS. Adipose tissue, obesity and non-alcoholic fatty liver disease. Minerva Endocrinol. 2017;42:92-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 142] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 27. | Polyzos SA, Kountouras J, Mantzoros CS. Adipokines in nonalcoholic fatty liver disease. Metabolism. 2016;65:1062-1079. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 206] [Cited by in RCA: 257] [Article Influence: 28.6] [Reference Citation Analysis (0)] |
| 28. | Polyzos SA, Kountouras J, Mantzoros CS. Leptin in nonalcoholic fatty liver disease: a narrative review. Metabolism. 2015;64:60-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 165] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 29. | Polyzos SA, Kountouras J, Zavos C, Tsiaousi E. The role of adiponectin in the pathogenesis and treatment of non-alcoholic fatty liver disease. Diabetes Obes Metab. 2010;12:365-383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 168] [Cited by in RCA: 199] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 30. | Imajo K, Fujita K, Yoneda M, Nozaki Y, Ogawa Y, Shinohara Y, Kato S, Mawatari H, Shibata W, Kitani H, Ikejima K, Kirikoshi H, Nakajima N, Saito S, Maeyama S, Watanabe S, Wada K, Nakajima A. Hyperresponsivity to low-dose endotoxin during progression to nonalcoholic steatohepatitis is regulated by leptin-mediated signaling. Cell Metab. 2012;16:44-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 240] [Cited by in RCA: 275] [Article Influence: 21.2] [Reference Citation Analysis (0)] |
| 31. | Silva-Veiga FM, Miranda CS, Martins FF, Daleprane JB, Mandarim-de-Lacerda CA, Souza-Mello V. Gut-liver axis modulation in fructose-fed mice: a role for PPAR-alpha and linagliptin. J Endocrinol. 2020;247:11-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 26] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 32. | Turnbaugh PJ, Ley RE, Mahowald MA, Magrini V, Mardis ER, Gordon JI. An obesity-associated gut microbiome with increased capacity for energy harvest. Nature. 2006;444:1027-1031. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9796] [Cited by in RCA: 8752] [Article Influence: 460.6] [Reference Citation Analysis (1)] |
| 33. | Porras D, Nistal E, Martínez-Flórez S, González-Gallego J, García-Mediavilla MV, Sánchez-Campos S. Intestinal Microbiota Modulation in Obesity-Related Non-alcoholic Fatty Liver Disease. Front Physiol. 2018;9:1813. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 72] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 34. | du Plessis J, van Pelt J, Korf H, Mathieu C, van der Schueren B, Lannoo M, Oyen T, Topal B, Fetter G, Nayler S, van der Merwe T, Windmolders P, Van Gaal L, Verrijken A, Hubens G, Gericke M, Cassiman D, Francque S, Nevens F, van der Merwe S. Association of Adipose Tissue Inflammation With Histologic Severity of Nonalcoholic Fatty Liver Disease. Gastroenterology 2015; 149: 635-48. e14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 193] [Cited by in RCA: 242] [Article Influence: 24.2] [Reference Citation Analysis (0)] |
| 35. | Lonardo A, Mantovani A, Lugari S, Targher G. Epidemiology and pathophysiology of the association between NAFLD and metabolically healthy or metabolically unhealthy obesity. Ann Hepatol. 2020;19:359-366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 100] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
| 36. | Romeo S, Kozlitina J, Xing C, Pertsemlidis A, Cox D, Pennacchio LA, Boerwinkle E, Cohen JC, Hobbs HH. Genetic variation in PNPLA3 confers susceptibility to nonalcoholic fatty liver disease. Nat Genet. 2008;40:1461-1465. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2701] [Cited by in RCA: 2596] [Article Influence: 152.7] [Reference Citation Analysis (0)] |
| 37. | Lau LHS, Wong SH. Microbiota, Obesity and NAFLD. Adv Exp Med Biol. 2018;1061:111-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 57] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 38. | Sharma P, Kumar A. Metabolic dysfunction associated fatty liver disease increases risk of severe Covid-19. Diabetes Metab Syndr. 2020;14:825-827. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 46] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 39. | Huang R, Zhu L, Wang J, Xue L, Liu L, Yan X, Huang S, Li Y, Zhang B, Xu T, Li C, Ji F, Ming F, Zhao Y, Cheng J, Wang Y, Zhao H, Hong S, Chen K, Zhao XA, Zou L, Sang D, Shao H, Guan X, Chen X, Chen Y, Wei J, Zhu C, Wu C. Clinical features of COVID-19 patients with non-alcoholic fatty liver disease. Hepatol Commun. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 61] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 40. | Lopez-Mendez I, Aquino-Matus J, Gall SM, Prieto-Nava JD, Juarez-Hernandez E, Uribe M, Castro-Narro G. Association of liver steatosis and fibrosis with clinical outcomes in patients with SARS-CoV-2 infection (COVID-19). Ann Hepatol. 2021;20:100271. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 48] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 41. | Gu X, Li X, An X, Yang S, Wu S, Yang X, Wang H. Elevated serum aspartate aminotransferase level identifies patients with coronavirus disease 2019 and predicts the length of hospital stay. J Clin Lab Anal. 2020;34:e23391. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 42. | Schmit G, Lelotte J, Vanhaebost J, Horsmans Y, Van Bockstal M, Baldin P. The Liver in COVID-19-Related Death: Protagonist or Innocent Bystander? Pathobiology. 2021;88:88-94. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 43. | Xu Z, Shi L, Wang Y, Zhang J, Huang L, Zhang C, Liu S, Zhao P, Liu H, Zhu L, Tai Y, Bai C, Gao T, Song J, Xia P, Dong J, Zhao J, Wang FS. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8:420-422. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5228] [Cited by in RCA: 5781] [Article Influence: 1156.2] [Reference Citation Analysis (2)] |
| 44. | Lagana SM, Kudose S, Iuga AC, Lee MJ, Fazlollahi L, Remotti HE, Del Portillo A, De Michele S, de Gonzalez AK, Saqi A, Khairallah P, Chong AM, Park H, Uhlemann AC, Lefkowitch JH, Verna EC. Hepatic pathology in patients dying of COVID-19: a series of 40 cases including clinical, histologic, and virologic data. Mod Pathol. 2020;33:2147-2155. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 130] [Cited by in RCA: 181] [Article Influence: 36.2] [Reference Citation Analysis (0)] |
| 45. | Ji D, Qin E, Xu J, Zhang D, Cheng G, Wang Y, Lau G. Non-alcoholic fatty liver diseases in patients with COVID-19: A retrospective study. J Hepatol. 2020;73:451-453. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 336] [Cited by in RCA: 408] [Article Influence: 81.6] [Reference Citation Analysis (2)] |
| 46. | Sun J, Aghemo A, Forner A, Valenti L. COVID-19 and liver disease. Liver Int. 2020;40:1278-1281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 200] [Cited by in RCA: 219] [Article Influence: 43.8] [Reference Citation Analysis (0)] |
| 47. | Zhang P, Zhu L, Cai J, Lei F, Qin JJ, Xie J, Liu YM, Zhao YC, Huang X, Lin L, Xia M, Chen MM, Cheng X, Zhang X, Guo D, Peng Y, Ji YX, Chen J, She ZG, Wang Y, Xu Q, Tan R, Wang H, Lin J, Luo P, Fu S, Cai H, Ye P, Xiao B, Mao W, Liu L, Yan Y, Liu M, Chen M, Zhang XJ, Wang X, Touyz RM, Xia J, Zhang BH, Yuan Y, Loomba R, Liu PP, Li H. Association of Inpatient Use of Angiotensin-Converting Enzyme Inhibitors and Angiotensin II Receptor Blockers With Mortality Among Patients With Hypertension Hospitalized With COVID-19. Circ Res. 2020;126:1671-1681. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 775] [Cited by in RCA: 888] [Article Influence: 177.6] [Reference Citation Analysis (0)] |
| 48. | Portincasa P, Krawczyk M, Machill A, Lammert F, Di Ciaula A. Hepatic consequences of COVID-19 infection. Lapping or biting? Eur J Intern Med. 2020;77:18-24. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 84] [Cited by in RCA: 78] [Article Influence: 15.6] [Reference Citation Analysis (0)] |
| 49. | Zhou YJ, Zheng KI, Wang XB, Yan HD, Sun QF, Pan KH, Wang TY, Ma HL, Chen YP, George J, Zheng MH. Younger patients with MAFLD are at increased risk of severe COVID-19 illness: A multicenter preliminary analysis. J Hepatol. 2020;73:719-721. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 104] [Cited by in RCA: 106] [Article Influence: 21.2] [Reference Citation Analysis (0)] |
| 50. | Gao F, Zheng KI, Wang XB, Sun QF, Pan KH, Wang TY, Chen YP, Targher G, Byrne CD, George J, Zheng MH. Obesity Is a Risk Factor for Greater COVID-19 Severity. Diabetes Care. 2020;43:e72-e74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 319] [Cited by in RCA: 270] [Article Influence: 54.0] [Reference Citation Analysis (0)] |
| 51. | Zheng KI, Gao F, Wang XB, Sun QF, Pan KH, Wang TY, Ma HL, Chen YP, Liu WY, George J, Zheng MH. Letter to the Editor: Obesity as a risk factor for greater severity of COVID-19 in patients with metabolic associated fatty liver disease. Metabolism. 2020;108:154244. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 250] [Cited by in RCA: 233] [Article Influence: 46.6] [Reference Citation Analysis (0)] |
| 52. | Bramante C, Tignanelli CJ, Dutta N, Jones E, Tamariz L, Clark JM, Usher M, Metlon-Meaux G, Ikramuddin S. Non-alcoholic fatty liver disease (NAFLD) and risk of hospitalization for Covid-19. medRxiv. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 45] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 53. | Hashemi N, Viveiros K, Redd WD, Zhou JC, McCarty TR, Bazarbashi AN, Hathorn KE, Wong D, Njie C, Shen L, Chan WW. Impact of chronic liver disease on outcomes of hospitalized patients with COVID-19: A multicentre United States experience. Liver Int. 2020;40:2515-2521. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 89] [Cited by in RCA: 117] [Article Influence: 23.4] [Reference Citation Analysis (2)] |
| 54. | Medeiros AK, Barbisan CC, Cruz IR, de Araújo EM, Libânio BB, Albuquerque KS, Torres US. Higher frequency of hepatic steatosis at CT among COVID-19-positive patients. Abdom Radiol (NY). 2020;45:2748-2754. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 43] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 55. | Pan L, Huang P, Xie X, Xu J, Guo D, Jiang Y. Metabolic associated fatty liver disease increases the severity of COVID-19: A meta-analysis. Dig Liver Dis. 2021;53:153-157. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 62] [Article Influence: 15.5] [Reference Citation Analysis (1)] |
| 56. | Ghoneim S, Butt MU, Hamid O, Shah A, Asaad I. The incidence of COVID-19 in patients with metabolic syndrome and non-alcoholic steatohepatitis: A population-based study. Metabol Open. 2020;8:100057. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 57] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 57. | Zhou J, Tan J. Diabetes patients with COVID-19 need better blood glucose management in Wuhan, China. Metabolism. 2020;107:154216. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 93] [Cited by in RCA: 102] [Article Influence: 20.4] [Reference Citation Analysis (0)] |
| 58. | Wong GL, Wong VW, Thompson A, Jia J, Hou J, Lesmana CRA, Susilo A, Tanaka Y, Chan WK, Gane E, Ong-Go AK, Lim SG, Ahn SH, Yu ML, Piratvisuth T, Chan HL; Asia-Pacific Working Group for Liver Derangement during the COVID-19 Pandemic. Management of patients with liver derangement during the COVID-19 pandemic: an Asia-Pacific position statement. Lancet Gastroenterol Hepatol. 2020;5:776-787. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 73] [Cited by in RCA: 62] [Article Influence: 12.4] [Reference Citation Analysis (1)] |
| 59. | Chen VL, Hawa F, Berinstein JA, Reddy CA, Kassab I, Platt KD, Hsu CY, Steiner CA, Louissaint J, Gunaratnam NT, Sharma P. Hepatic Steatosis Is Associated with Increased Disease Severity and Liver Injury in Coronavirus Disease-19. Dig Dis Sci. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 35] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 60. | Forlano R, Mullish BH, Mukherjee SK, Nathwani R, Harlow C, Crook P, Judge R, Soubieres A, Middleton P, Daunt A, Perez-Guzman P, Selvapatt N, Lemoine M, Dhar A, Thursz MR, Nayagam S, Manousou P. In-hospital mortality is associated with inflammatory response in NAFLD patients admitted for COVID-19. PLoS One. 2020;15:e0240400. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 57] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 61. | Ji D, Zhang D, Yang T, Mu J, Zhao P, Xu J, Li C, Cheng G, Wang Y, Chen Z, Qin E, Lau G. Effect of COVID-19 on patients with compensated chronic liver diseases. Hepatol Int. 2020;14:701-710. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 49] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 62. | Palomar-Lever A, Barraza G, Galicia-Alba J, Echeverri-Bolaños M, Escarria-Panesso R, Padua-Barrios J, Halabe-Cherem J, Hernandez-Molina G, Chargoy-Loustaunau TN, Kimura-Hayama E. Hepatic steatosis as an independent risk factor for severe disease in patients with COVID-19: A computed tomography study. JGH Open. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 63. | Sachdeva S, Khandait H, Kopel J, Aloysius MM, Desai R, Goyal H. NAFLD and COVID-19: a Pooled Analysis. SN Compr Clin Med. 2020;1-4. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 64] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 64. | Sarin SK, Choudhury A, Lau GK, Zheng MH, Ji D, Abd-Elsalam S, Hwang J, Qi X, Cua IH, Suh JI, Park JG, Putcharoen O, Kaewdech A, Piratvisuth T, Treeprasertsuk S, Park S, Wejnaruemarn S, Payawal DA, Baatarkhuu O, Ahn SH, Yeo CD, Alonzo UR, Chinbayar T, Loho IM, Yokosuka O, Jafri W, Tan S, Soo LI, Tanwandee T, Gani R, Anand L, Esmail ES, Khalaf M, Alam S, Lin CY, Chuang WL, Soin AS, Garg HK, Kalista K, Batsukh B, Purnomo HD, Dara VP, Rathi P, Al Mahtab M, Shukla A, Sharma MK, Omata M; APASL COVID Task Force; APASL COVID Liver Injury Spectrum Study (APCOLIS Study-NCT 04345640). Pre-existing liver disease is associated with poor outcome in patients with SARS CoV2 infection; The APCOLIS Study (APASL COVID-19 Liver Injury Spectrum Study). Hepatol Int. 2020;14:690-700. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 217] [Cited by in RCA: 216] [Article Influence: 43.2] [Reference Citation Analysis (1)] |
| 65. | Shalimar, Elhence A, Vaishnav M, Kumar R, Pathak P, Soni KD, Aggarwal R, Soneja M, Jorwal P, Kumar A, Khanna P, Singh AK, Biswas A, Nischal N, Dar L, Choudhary A, Rangarajan K, Mohan A, Acharya P, Nayak B, Gunjan D, Saraya A, Mahapatra S, Makharia G, Trikha A, Garg P. Poor outcomes in patients with cirrhosis and Corona Virus Disease-19. Indian J Gastroenterol. 2020;39:285-291. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 50] [Cited by in RCA: 45] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 66. | Li J, Fan JG. Characteristics and Mechanism of Liver Injury in 2019 Coronavirus Disease. J Clin Transl Hepatol. 2020;8:13-17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 199] [Cited by in RCA: 206] [Article Influence: 41.2] [Reference Citation Analysis (2)] |
| 67. | Conti P, Ronconi G, Caraffa A, Gallenga CE, Ross R, Frydas I, Kritas SK. Induction of pro-inflammatory cytokines (IL-1 and IL-6) and lung inflammation by Coronavirus-19 (COVI-19 or SARS-CoV-2): anti-inflammatory strategies. J Biol Regul Homeost Agents. 2020;34:327-331. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 593] [Reference Citation Analysis (0)] |
| 68. | Tisoncik JR, Korth MJ, Simmons CP, Farrar J, Martin TR, Katze MG. Into the eye of the cytokine storm. Microbiol Mol Biol Rev. 2012;76:16-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1171] [Cited by in RCA: 1324] [Article Influence: 101.8] [Reference Citation Analysis (1)] |
| 69. | Schmidt-Arras D, Rose-John S. IL-6 pathway in the liver: From physiopathology to therapy. J Hepatol. 2016;64:1403-1415. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 460] [Cited by in RCA: 651] [Article Influence: 72.3] [Reference Citation Analysis (0)] |
| 70. | López-Reyes A, Martinez-Armenta C, Espinosa-Velázquez R, Vázquez-Cárdenas P, Cruz-Ramos M, Palacios-Gonzalez B, Gomez-Quiroz LE, Martínez-Nava GA. NLRP3 Inflammasome: The Stormy Link Between Obesity and COVID-19. Front Immunol. 2020;11:570251. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 66] [Cited by in RCA: 62] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 71. | Swanson KV, Deng M, Ting JP. The NLRP3 inflammasome: molecular activation and regulation to therapeutics. Nat Rev Immunol. 2019;19:477-489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1426] [Cited by in RCA: 3158] [Article Influence: 631.6] [Reference Citation Analysis (0)] |
| 72. | Lefere S, Tacke F. Macrophages in obesity and non-alcoholic fatty liver disease: Crosstalk with metabolism. JHEP Rep. 2019;1:30-43. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 123] [Cited by in RCA: 190] [Article Influence: 31.7] [Reference Citation Analysis (0)] |
| 73. | Rheinheimer J, de Souza BM, Cardoso NS, Bauer AC, Crispim D. Current role of the NLRP3 inflammasome on obesity and insulin resistance: A systematic review. Metabolism. 2017;74:1-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 208] [Article Influence: 26.0] [Reference Citation Analysis (1)] |
| 74. | Vandanmagsar B, Youm YH, Ravussin A, Galgani JE, Stadler K, Mynatt RL, Ravussin E, Stephens JM, Dixit VD. The NLRP3 inflammasome instigates obesity-induced inflammation and insulin resistance. Nat Med. 2011;17:179-188. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2148] [Cited by in RCA: 2049] [Article Influence: 146.4] [Reference Citation Analysis (0)] |
| 75. | Luo W, Xu Q, Wang Q, Wu H, Hua J. Effect of modulation of PPAR-γ activity on Kupffer cells M1/M2 polarization in the development of non-alcoholic fatty liver disease. Sci Rep. 2017;7:44612. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 128] [Cited by in RCA: 225] [Article Influence: 28.1] [Reference Citation Analysis (0)] |
| 76. | Feng G, Zheng KI, Yan QQ, Rios RS, Targher G, Byrne CD, Poucke SV, Liu WY, Zheng MH. COVID-19 and Liver Dysfunction: Current Insights and Emergent Therapeutic Strategies. J Clin Transl Hepatol. 2020;8:18-24. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 289] [Cited by in RCA: 278] [Article Influence: 55.6] [Reference Citation Analysis (0)] |
| 77. | Simon TG, Trejo MEP, McClelland R, Bradley R, Blaha MJ, Zeb I, Corey KE, Budoff MJ, Chung RT. Circulating Interleukin-6 is a biomarker for coronary atherosclerosis in nonalcoholic fatty liver disease: Results from the Multi-Ethnic Study of Atherosclerosis. Int J Cardiol. 2018;259:198-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 59] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 78. | Shi CS, Nabar NR, Huang NN, Kehrl JH. SARS-Coronavirus Open Reading Frame-8b triggers intracellular stress pathways and activates NLRP3 inflammasomes. Cell Death Discov. 2019;5:101. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 270] [Cited by in RCA: 317] [Article Influence: 52.8] [Reference Citation Analysis (0)] |
| 79. | Chen IY, Moriyama M, Chang MF, Ichinohe T. Severe Acute Respiratory Syndrome Coronavirus Viroporin 3a Activates the NLRP3 Inflammasome. Front Microbiol. 2019;10:50. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 313] [Cited by in RCA: 416] [Article Influence: 69.3] [Reference Citation Analysis (0)] |
| 80. | Peters U, Suratt BT, Bates JHT, Dixon AE. Beyond BMI: Obesity and Lung Disease. Chest. 2018;153:702-709. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 97] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 81. | Paizis G, Tikellis C, Cooper ME, Schembri JM, Lew RA, Smith AI, Shaw T, Warner FJ, Zuilli A, Burrell LM, Angus PW. Chronic liver injury in rats and humans upregulates the novel enzyme angiotensin converting enzyme 2. Gut. 2005;54:1790-1796. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 236] [Cited by in RCA: 281] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 82. | Chen J, Chen J, Fu H, Li Y, Wang L, Luo S, Lu H. Hypoxia exacerbates nonalcoholic fatty liver disease via the HIF-2α/PPARα pathway. Am J Physiol Endocrinol Metab. 2019;317:E710-E722. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 85] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
| 83. | Hernández A, Reyes D, Geng Y, Arab JP, Cabrera D, Sepulveda R, Solis N, Buist-Homan M, Arrese M, Moshage H. Extracellular vesicles derived from fat-laden hepatocytes undergoing chemical hypoxia promote a pro-fibrotic phenotype in hepatic stellate cells. Biochim Biophys Acta Mol Basis Dis. 2020;1866:165857. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 31] [Article Influence: 6.2] [Reference Citation Analysis (0)] |