Published online Feb 28, 2020. doi: 10.3748/wjg.v26.i8.877
Peer-review started: December 10, 2019
First decision: January 7, 2020
Revised: January 16, 2020
Accepted: January 19, 2020
Article in press: January 19, 2020
Published online: February 28, 2020
Processing time: 79 Days and 22.8 Hours
Juvenile polyps are the most common type of polyps in children but are rare in adults. Inflammatory bowel disease (IBD) patients have a similar spectrum of symptoms as patients with juvenile polyps. Both patients with juvenile polyps and those with active IBD have high fecal calprotectin levels. Four cases of children with ulcerative colitis (UC) with solitary juvenile polyps and one case of an adult with UC with juvenile polyposis syndrome have been reported upon diagnosis of UC, while there have been no cases of adults with UC with solitary juvenile polyp reported in the literature.
A 37-year-old man with a 12-year history of UC was admitted to our clinic because of increased stool frequency. UC was diagnosed at the age of 25. As the lesion was confined to the rectum, sulfasalazine suppositories or mesalazine suppositories were used. The patient was followed in an outpatient clinic, and colonoscopy was performed every one or two years. The latest examination was undertaken three years prior in the presence of proctitis. Recently, the patient complained of three to five bowel movements a day. There was mucus in the stool but no visible blood. Colonoscopy revealed a solitary polyp, about 1.5 cm in diameter, with a short and broad peduncle in the transverse colon surrounded by congestive and edematous mucosa. The patient had no family history of colorectal polyps or cancer. The polyp was successfully removed by endoscopic mucosal resection. Histopathological examination revealed that the polyp was a juvenile polyp without any malignant signs. Immunohistochemical staining for p53 showed wild-type expression and p53 overexpression was not detected. Ki-67 labeling index was 3%.
This is the first case of an adult UC patient with a solitary juvenile polyp at the 12-year follow-up. The correlation between juvenile polyps and the activity of IBD needs further study.
Core tip: Juvenile polyps are the most common type of polyps in children but are rare in adults. Although sporadic juvenile polyps are not associated with an increased cancer risk, they may also undergo dysplastic changes. Inflammatory bowel disease patients have a similar spectrum of symptoms as patients with juvenile polyps. Both patients with juvenile polyps and those with active inflammatory bowel disease have high fecal calprotectin levels. Here, we present the first case of adult ulcerative colitis patient with a solitary juvenile polyp, which was treated by endoscopic mucosal resection, at his 12-year follow-up.
- Citation: Chen YW, Tu JF, Shen WJ, Chen WY, Dong J. Diagnosis and management of a solitary colorectal juvenile polyp in an adult during follow-up for ulcerative colitis: A case report. World J Gastroenterol 2020; 26(8): 877-882
- URL: https://www.wjgnet.com/1007-9327/full/v26/i8/877.htm
- DOI: https://dx.doi.org/10.3748/wjg.v26.i8.877
Juvenile polyposis syndrome (JPS) is an autosomal dominant disease characterized by multiple hamartomatous polyps throughout the gastrointestinal tract. Individuals with JPS are at an increased risk for colorectal and gastric cancers[1,2]. In contrast to JPS, sporadic juvenile polyps of the colon, which are usually solitary, do not predict a malignancy[3,4]. Colonic juvenile polyps are the most common type of polyps in children but are rare in adults[5,6]. Here we present the first case of an adult with solitary juvenile polyp in a patient with ulcerative colitis (UC) during follow-up in his clinical remission.
A 37-year-old man with a 12-year history of UC was admitted to our clinic because of increased stool frequency.
The patient complained of three to five bowel movements a day for about 1 wk. There was mucus in stools but no visible blood.
UC was diagnosed at the age of 25 years, based on clinical, biological, endoscopic, and histological findings. As the lesion was confined to the rectum, sulfasalazine suppositories or mesalazine suppositories were used. The patient was followed in an outpatient clinic, and colonoscopy was performed every one or two years. The latest examination was performed three years prior in the presence of proctitis.
The patient has hypertension for years which is controlled with medicine. He had no family history of UC, colorectal polyps, or cancer.
The patient’s temperature was 36.7 °C, heart rate was 74 bpm, respiratory rate was 16 breaths per minute, and blood pressure was 134/95 mmHg. The physical examination revealed no positive sign.
Blood analysis revealed mild erythrocytosis (5.92 × 109/L), with a haemoglobin level of 181 g/L and normal white blood cell and platelet counts. Prothrombin time and D-dimer were normal, and partial thromboplastin time was slightly increased by 0.2 s. Fecal occult blood test showed a positive result “+”. Immunoglobulin (Ig) A was 3.92 g/L (0.6-3.3 g/L). IgM, IgG, thyroid hormones, rheumatoid factors, serum tumor markers, and urine analysis, as well as electrocardiogram were normal. We did not test fecal calprotectin in this case.
Abdominal ultrasound showed mild fatty liver and chronic cholecystitis with multiple polyps. Cardiac ultrasound and chest computed tomography scan were normal.
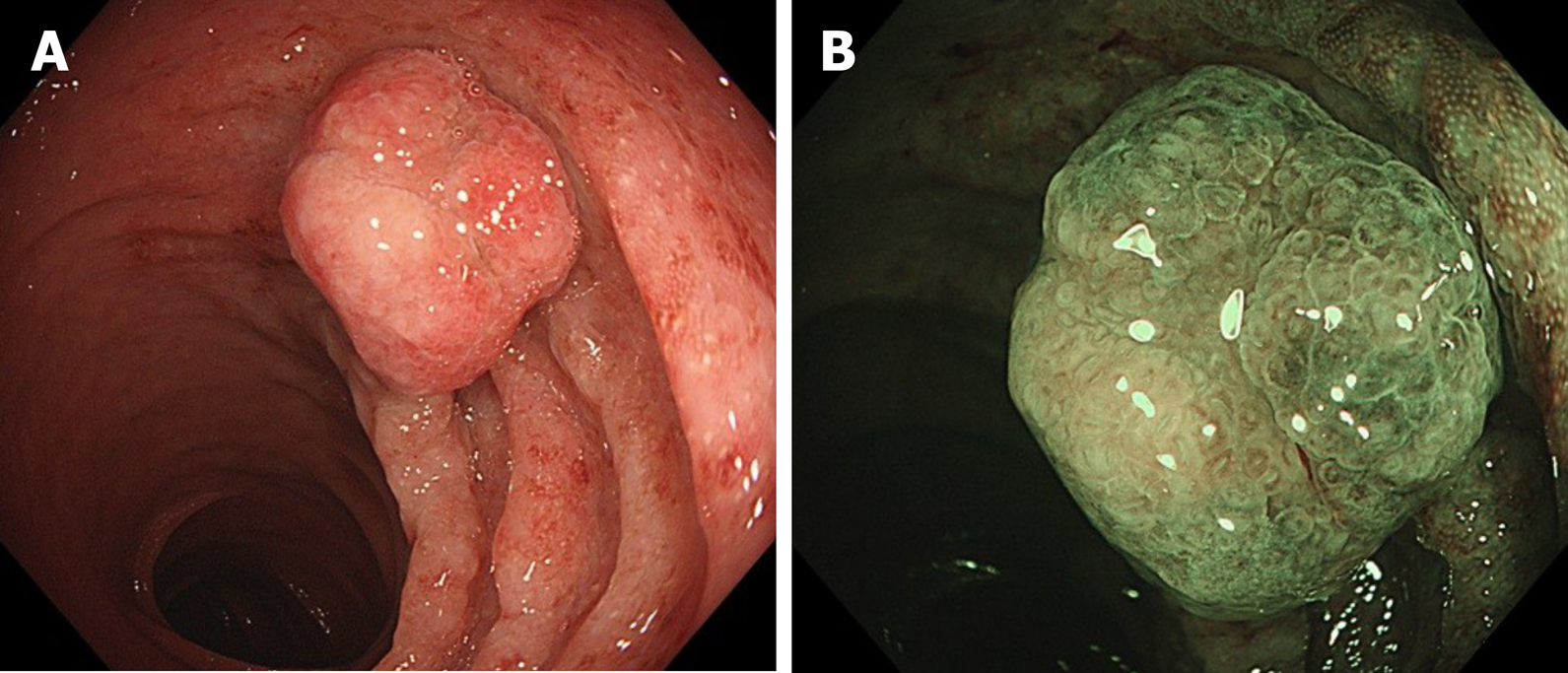
Colonoscopy revealed a solitary polyp, about 1.5 cm in diameter, with a short broad peduncle in the transverse colon surrounded by congestive and edematous mucosa. The surface of the polyp was mild lobulations without erosions or ulcerations (Figure 1).
The final diagnosis was colonic polyp.
The polyp was successfully removed by endoscopic mucosal resection (EMR).
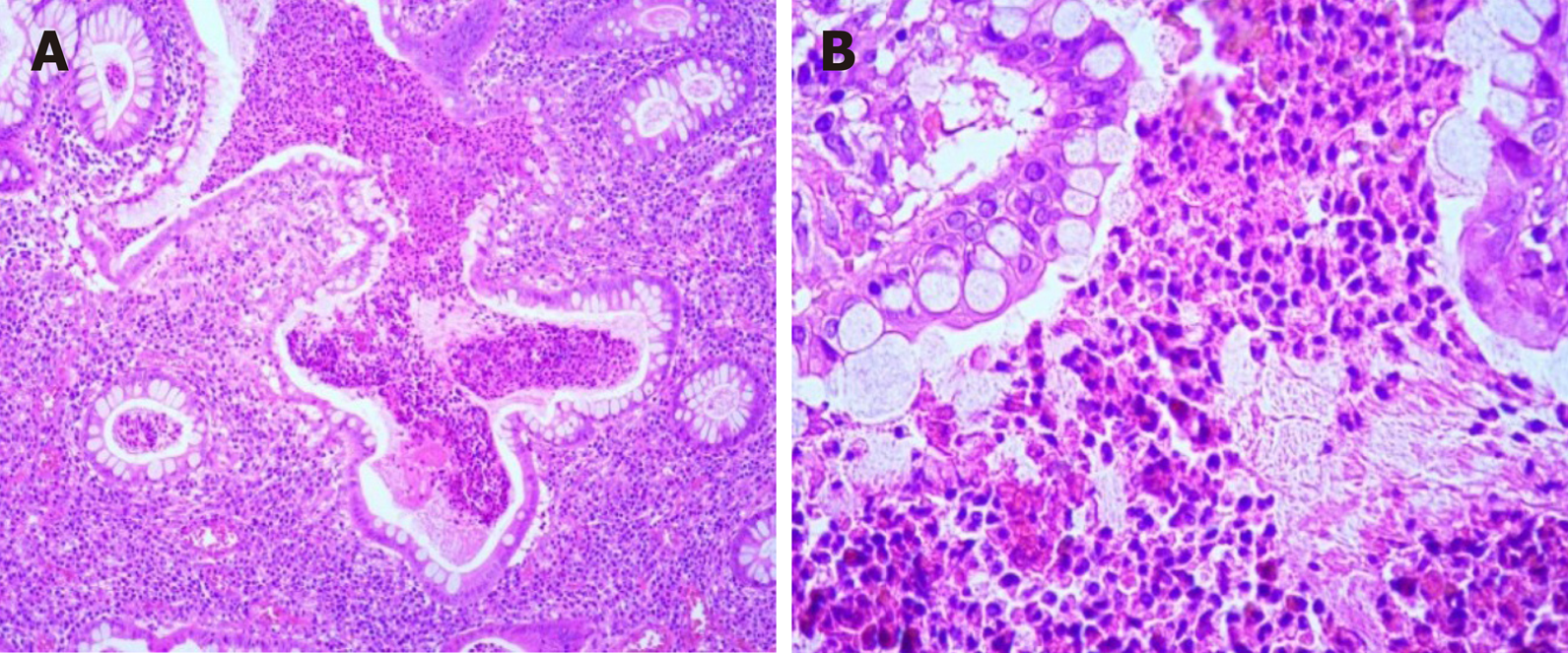
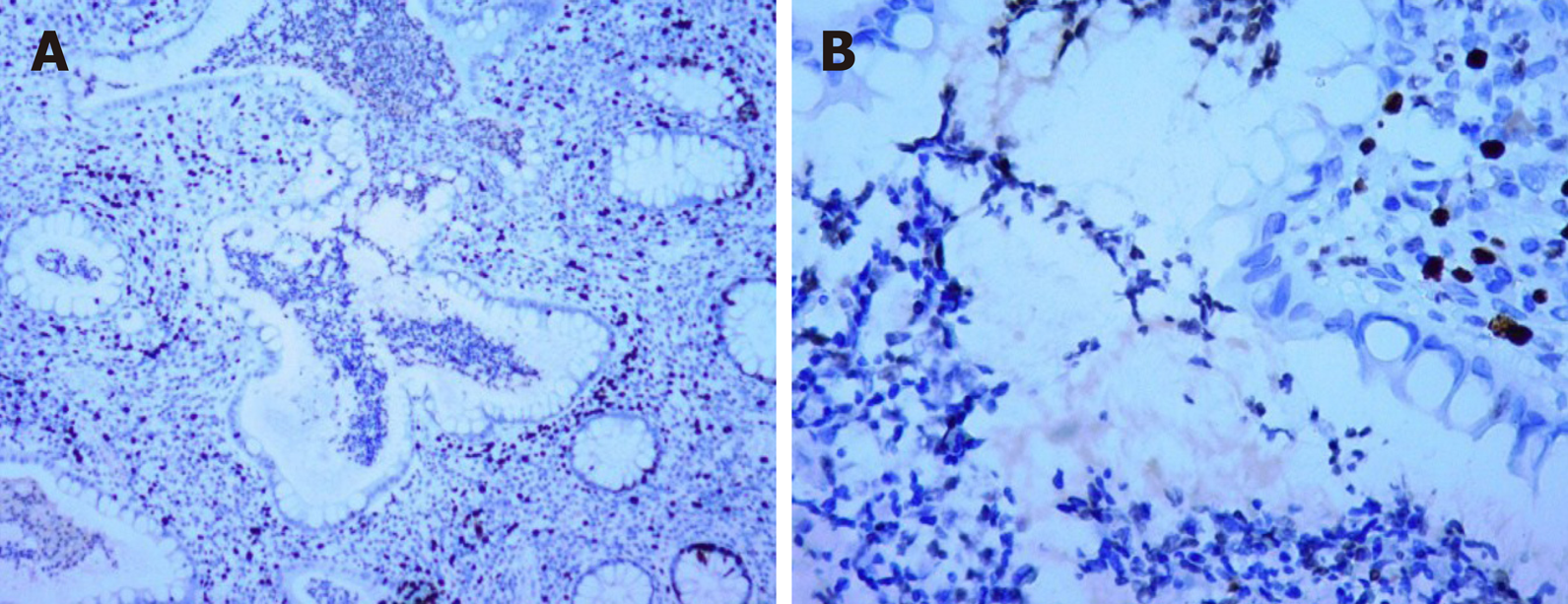
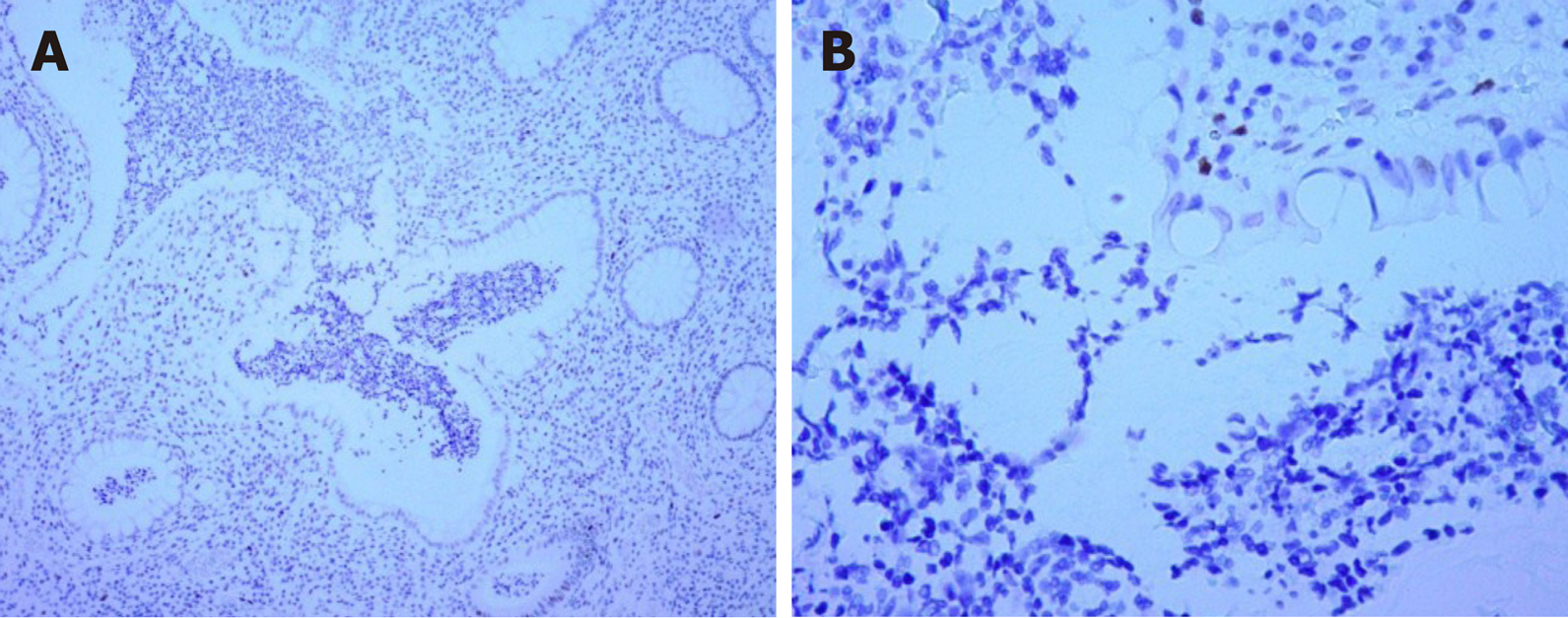
Histopathological examination revealed that the polyp was a juvenile polyp without any malignant signs (Figure 2). Immunohistochemical staining for p53 showed wild-type expression and p53 overexpression was not detected (Figure 3). Ki-67 labeling index was 3% (Figure 4).
JPS is a rare autosomal dominant hereditary disorder characterized by multiple distinct juvenile polyps in the gastrointestinal tract and an increased risk of colorectal cancer[1,2]. The cumulative lifetime risk of colorectal cancer is 39%, and the relative risk is 34% (95%CI: 14.4%-65.7%)[1]. In contrast, sporadic juvenile polyps of the colon are not associated with an increased cancer risk[4]. However, sporadic juvenile polyps may also undergo dysplastic changes[7-9]. The incidence of juvenile polyps in the Danish population was estimated to be between 1:45000 and 1:65000[8]. It has been reported that juvenile polyps occur in 2% of children and adolescents, accounting for the majority of polyps in children (approximately 80%-90%)[4,5]. In adults, hyperplastic polyps and adenomas are the most common types of polyps.
Small colonic juvenile polyps without dysplastic changes or severe symptoms are suitable for endoscopic polypectomy. However, in multiple or diffuse juvenile polyposis coli, colectomy may be necessary[10]. EMR or endoscopic submucosal dissection has been indicated to be safe and effective for sporadic, semipedunculated or sessile large juvenile polyps[11].
Juvenile polyps are hamartomas. It is a great challenge to differentiate sporadic juvenile polyps from JPS[12]. Approximately 82.9% of sporadic juvenile polyps occur in the rectosigmoid colon[8]. Juvenile polyps showed similar clinical manifestations as other types of polyps, such as rectal bleeding, abdominal pain, diarrhea, and prolapse. For endoscopy findings, juvenile polyps vary in size from a few millimeters of sessile nodules to as large as several centimeters of pedunculated lesions. Small polyps are usually rounded and smooth, while larger polyps may be multilobulated. A small white exudate may also be found[12].The surface of polyps is often accompanied by erosion and granulation tissue hyperplasia[13]. Small granules called chicken skin mucosa can spread around juvenile polyps[14] and can also appear in advanced colorectal adenoma[15].
The diagnosis of juvenile polyps mainly depends on histopathology. Juvenile polyps are composed of differentiated glandular ducts. The glandular cavity is expanded to various degrees. There are a large number of dilated small vessels and inflammatory cells, such as lymphocytes, plasma cells, neutrophils, and eosinophils in the stroma. The fibrous tissues contain mucinous gland hyperplasia and mucous cysts of different sizes. It is difficult to distinguish inflammatory polyps from juvenile polyps because early lesions can have granulation tissue-like stroma, as observed in patients with inflammatory bowel disease (IBD)[14,16].
IBD patients may present with diarrhea, abdominal pain, hematochezia, fever, anemia, etc. They have a similar spectrum of symptoms as patients with juvenile polyps. Fecal calprotectin (FCP) has been used as a noninvasive biomarker for IBD and has been proven to be associated with disease activity. Similarly, in patients with juvenile polyps, FCP levels are also elevated[17]. However, the level of FCP drops after polypectomy[18]. IBD and juvenile polyps cannot be differentiated by FCP levels[17]. Fecal calprotectin test was not performed in this case, which is a minor flaw of this research. Several cases of IBD with JPS have been reported. In 1987, Gryboski and Barwick[19] described four cases of children with UC who had solitary juvenile polyps. The case of an adult UC patient with juvenile polyposis syndrome was first reported in 2011[20], but there have been no cases of adults with UC with solitary juvenile polyps. IBD patients, UC patients in particular, are more likely to develop colorectal cancer. Chronic inflammation is believed to be linked to carcinogenesis. Inflammatory cells can impact the regulation of genes governing the prevention of carcinogenesis, e.g., p53[21]. As mentioned in previous discussions, since inflammatory cells were involved in the development of juvenile polyp, and the likely p53 overexpression when dysplastic change or cancerization occur[22], it is possible that inflammation-cancer is one pathway of the cancerization of juvenile poly, while further study is needed to confirm this assertion. Thus far, the association between juvenile polyps and IBD is still unknown.
We report the case of an adult UC patient with a solitary colonic juvenile polyp, about 1.5 cm in diameter, with a short and broad peduncle at his 12-year follow-up. The polyp was successfully removed by EMR without any complications. To our knowledge, this is the first such case reported in the literature. The patient will receive close follow-up and the correlation between juvenile polyps and IBD needs further study.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and Hepatology
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Tsuchiya A, Tandon RK, Sitkin S S-Editor: Zhang L L-Editor: Wang TQ E-Editor: Zhang YL
| 1. | Brosens LA, van Hattem A, Hylind LM, Iacobuzio-Donahue C, Romans KE, Axilbund J, Cruz-Correa M, Tersmette AC, Offerhaus GJ, Giardiello FM. Risk of colorectal cancer in juvenile polyposis. Gut. 2007;56:965-967. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 174] [Cited by in RCA: 168] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 2. | Latchford AR, Neale K, Phillips RK, Clark SK. Juvenile polyposis syndrome: a study of genotype, phenotype, and long-term outcome. Dis Colon Rectum. 2012;55:1038-1043. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 108] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 3. | Nugent KP, Talbot IC, Hodgson SV, Phillips RK. Solitary juvenile polyps: not a marker for subsequent malignancy. Gastroenterology. 1993;105:698-700. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 63] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 4. | Zbuk KM, Eng C. Hamartomatous polyposis syndromes. Nat Clin Pract Gastroenterol Hepatol. 2007;4:492-502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 140] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 5. | Chow E, Macrae F. A review of juvenile polyposis syndrome. J Gastroenterol Hepatol. 2005;20:1634-1640. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 101] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 6. | HORRILLENO EG, ECKERT C, ACKERMAN LV. Polyps of the rectum and colon in children. Cancer. 1957;10:1210-1220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 7. | Dickey W, Alderdice J, McConnell B. Dysplastic change in the solitary juvenile polyp. Endoscopy. 1996;28:641. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 8. | Jelsig AM, Ousager LB, Brusgaard K, Qvist N. Juvenile Polyps in Denmark from 1995 to 2014. Dis Colon Rectum. 2016;59:751-757. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 9. | Jones MA, Hebert JC, Trainer TD. Juvenile polyp with intramucosal carcinoma. Arch Pathol Lab Med. 1987;111:200-201. [PubMed] |
| 10. | Nowicki MJ, Bishop PR. Successful endoscopic removal of an appendiceal polyp in a child with juvenile polyposis syndrome. Gastrointest Endosc. 2011;74:441-443. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Otake K, Uchida K, Inoue M, Matsushita K, Hashimoto K, Toiyama Y, Tanaka K, Nakatani K, Kawai K, Kusunoki M. A large, solitary, semipedunculated gastric polyp in pediatric juvenile polyposis syndrome. Gastrointest Endosc. 2011;73:1313-1314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Syngal S, Brand RE, Church JM, Giardiello FM, Hampel HL, Burt RW; American College of Gastroenterology. ACG clinical guideline: Genetic testing and management of hereditary gastrointestinal cancer syndromes. Am J Gastroenterol. 2015;110:223-62; quiz 263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 957] [Cited by in RCA: 1090] [Article Influence: 109.0] [Reference Citation Analysis (0)] |
| 13. | Brosens LA, Langeveld D, van Hattem WA, Giardiello FM, Offerhaus GJ. Juvenile polyposis syndrome. World J Gastroenterol. 2011;17:4839-4844. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 103] [Cited by in RCA: 107] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 14. | Hirotani A, Sakai E, Nakajima A, Kawana K, Nagase H. Endoscopic findings of atypical juvenile colonic polyps. Gastrointest Endosc. 2016;83:476-7; discussion 477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 15. | Chung EJ, Lee JY, Choe J, Chang HS, Kim J, Yang DH, Ye BD, Byeon JS, Kim KJ, Yang SK, Kim JH, Myung SJ. Colonic Chicken Skin Mucosa is an Independent Endoscopic Predictor of Advanced Colorectal Adenoma. Intest Res. 2015;13:318-325. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 16. | Jelsig AM. Hamartomatous polyps - a clinical and molecular genetic study. Dan Med J. 2016;63. [PubMed] |
| 17. | Zijlstra M, Pluimakers V, Nikkels P, Wolters V, Houwen R. Elevated Faecal Calprotectin Does Not Differentiate Between Inflammatory Bowel Disease and a Juvenile Polyp. J Pediatr Gastroenterol Nutr. 2016;62:e22-e23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Hodgson-Parnell L, Spence O, Chapple K. Solitary juvenile polyp as a cause of elevated faecal calprotectin in an adult. BMJ Case Rep. 2018;2018. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 19. | Gryboski JD, Barwick KW. Juvenile polyps and ulcerative colitis. J Pediatr Gastroenterol Nutr. 1987;6:811-814. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 20. | Elhjouji A, Aitali A, Rouibaa F, Rharrassi I, Zentar A, Sair K. Colorectal juvenile polyposis in an adult with ulcerative colitis. J Visc Surg. 2011;148:64-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 21. | Ullman TA, Itzkowitz SH. Intestinal inflammation and cancer. Gastroenterology. 2011;140:1807-1816. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 738] [Cited by in RCA: 856] [Article Influence: 61.1] [Reference Citation Analysis (0)] |
| 22. | Vanoli A, Lucioni M, Biletta E, Chiaravalli AM, Alvisi C, Luinetti O. A Wolf in Sheep's Clothing: A Sporadic Juvenile Polyp of the Colon Harboring an Intramucosal Adenocarcinoma. Int J Surg Pathol. 2015;23:571-574. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |