Published online Nov 7, 2020. doi: 10.3748/wjg.v26.i41.6391
Peer-review started: July 9, 2020
First decision: September 12, 2020
Revised: September 22, 2020
Accepted: October 13, 2020
Article in press: October 13, 2020
Published online: November 7, 2020
Processing time: 119 Days and 13.7 Hours
At our academic tertiary care medical center, we have noted patients referred for endoscopic retrograde cholangiopancreatography (ERCP) who increasingly require advanced cannulation techniques. This trend is noted despite increased endoscopist experience and annual ERCP volume over the same period.
To evaluate this phenomenon of perceived escalation in complexity of cannulation at ERCP and assessed potential underlying factors.
Demographic/clinical variables and records of ERCP patients at the beginning (2008), middle (2013) and end (2018) of the last decade were reviewed retrospectively. Cannulation approaches were classified as “standard” or “advanced” and duodenoscope position was labeled as “standard” (short position) or “non-standard” (e.g., long, semi-long).
Patients undergoing ERCP were older in 2018 compared to 2008 (69.7 ± 15.2 years vs 55.1 ± 14.7, P < 0.05). Increased ampullary distortion and peri-ampullary diverticula were noted in 2018 (P < 0.001). ERCPs were increasingly performed with a non-standard duodenoscope position, from 2.2% (2008) to 5.6% (2013) and 16.1% (2018) (P < 0.001). Utilization of more than one advanced cannulation technique for a given ERCP increased from 0.7% (2008) to 0.9% (2013) to 6.6% (2018) (P < 0.001). Primary mass size > 4 cm, pancreatic uncinate mass, and bilirubin > 10 mg/dL predicted use of advanced cannulation techniques (P < 0.03 for each).
Complexity of cannulation at ERCP has sharply increased over the past 5 years, with an increased proportion of elderly patients and those with malignancy requiring advanced cannulation approaches. These data suggest that complexity of cannulation at ERCP may be predicted based on patient/ampulla characteristics. This may inform selection of experienced, high-volume endoscopists to perform these complex procedures.
Core Tip: At our tertiary care academic medical center, we have noted patients referred for endoscopic retrograde cholangiopancreatography (ERCP) who increasingly require advanced cannulation techniques. This trend is noted despite increasing endoscopist experience and ERCP volume. We therefore formally evaluated this phenomenon and underlying factors. We found that complexity of cannulation at ERCP has sharply increased over the past 5 years, with more elderly patients and those with malignancy requiring advanced cannulation techniques. These data suggest that cannulation complexity may be predicted based on patient/ampulla characteristics.
- Citation: Barakat MT, Girotra M, Thosani N, Kothari S, Banerjee S. Escalating complexity of endoscopic retrograde cholangiopancreatography over the last decade with increasing reliance on advanced cannulation techniques. World J Gastroenterol 2020; 26(41): 6391-6401
- URL: https://www.wjgnet.com/1007-9327/full/v26/i41/6391.htm
- DOI: https://dx.doi.org/10.3748/wjg.v26.i41.6391
Endoscopic retrograde cholangiopancreatography (ERCP) is among the most technically challenging and high-risk endoscopic procedures. It is performed in approximately 1 per 1000 individuals, with up to 600000 ERCPs performed annually in the United States[1,2]. Successful cannulation of the duct of interest is the crucial initial step in ERCP. As selective ductal cannulation is the most challenging element of ERCP, cannulation success rates largely equate to ERCP success rates and vary widely by center and patient population. Reported successful ductal cannulation rates at ERCP are broad, ranging from 55% to over 90%[3-6]. Some studies have attributed this variability in cannulation rates to the endoscopist and facility ERCP volume, with high volume endoscopists who practice in academic medical centers using state-of-the-art equipment and performing procedures with the support of experienced staff exhibiting higher cannulation rates[7-9]. However one recent study notably found that patient and procedure characteristics are more important than endoscopist or facility characteristics in predicting cannulation success at ERCP[10].
Cannulation of the duct of interest is not only the most crucial step for success of an ERCP procedure, but it also represents the highest risk aspect of ERCP. Similar to cannulation success rates, there has been wide variability in the reported rates of ERCP-associated adverse events, ranging from as low as 2.5% to as high as 14.0%[11-13]. Many of the same factors that are associated with high cannulation rates are also associated with low post-ERCP adverse event rates, including the experience and volume of the endoscopist and facility in which an ERCP is performed[7-9]. Of all ERCP-associated adverse events, post-ERCP pancreatitis is most closely associated with prolonged cannulation efforts, use of advanced cannulation techniques and cannulation failure. Furthermore, post-ERCP pancreatitis is recognized as the most severe adverse event associated with ERCP and contributes most to the 0.1% rate of post-ERCP mortality[14-16]. Understanding trends that affect cannulation rates at ERCP and factors that modulate cannulation success is important, not only for avoiding costly repeat and rescue procedures, but also for minimizing adverse events and taking all possible steps to optimize ERCP outcomes. As the technical complexity of an ERCP and patient characteristics as well as indications for the procedure have been demonstrated to predict cannulation success and adverse event rates, an enhanced understanding of trends in the technical complexity of ERCP is desirable.
The technical complexity of an ERCP is multi-factorial, including goals of the procedure as well as factors such as patient anatomy (e.g., post-surgical, malignancy-associated deformity or infiltration of the stomach/duodenum, eccentrically located or small ampulla and peri-ampullary diverticulum). Some of these factors associated with ERCP complexity are difficult to predict pre-procedure, but the majority can be defined in advance and measures may be possible to minimize ERCP-associated risks. Several ERCP complexity scales have been proposed to reflect and predict the technical challenges and adverse events that may be encountered during a procedure[17-19], but these scales are limited in their generalizability and applicability to modern ERCP practice.
At our tertiary care academic endoscopy unit, we have noted over the last decade, an increase in utilization of advanced biliary cannulation techniques, a shift in ERCP indications and altered anatomy contributing to a perceived escalating complexity of ERCPs. This motivated the present study to systematically evaluate how ERCP has changed over the past decade at our tertiary care academic medical center. ERCPs performed at our institution by a single highly experienced endoscopist were evaluated over the past decade to define changes in patient characteristics, procedure indication and procedure characteristics, which may be driving this perceived increased complexity of ERCP.
ERCP patient records from 2008, 2013 and 2018 were evaluated retrospectively using a prospectively maintained endoscopy database. Demographic data and clinical variables including ERCP indications, cannulation rates and adverse event rates were collected. Demographic data collected included patient age/gender, indication for ERCP, patient co-morbidities and laboratory studies.
Cannulation techniques, classified as “standard” or “advanced” and patients undergoing Goff septotomy, double wire technique, or needle knife precut sphincterotomy and (or a combination thereof) to facilitate biliary access, were noted.
Post-surgical anatomy was documented and non-surgical, acquired anatomical distortion interfering with performance of the procedure was noted. Endoscopy reports and fluoroscopy images associated with each ERCP were reviewed and duodenoscope position necessary to accomplish the ERCP was evaluated by fluoroscopy images and classified as “standard” (short position) or “non-standard” (long, semi-long position or other variant). Ampulla characteristics were recorded, including ampullary distortion, infiltration, and presence of a peri-ampullary diverticulum. Anatomical characteristics of the patient and their impact the procedure were documented, along with the level of anatomical atypia (e.g., oropharyngeal, esophageal, gastric, duodenal, ampullary).
Standard approaches were used for performing ERCPs. Procedures before 2012 were predominately performed under moderate sedation and procedures after 2012 were predominately performed with anesthesia support (monitored anesthesia care or general anesthesia) per our institutional protocol. Our institution’s therapeutic endoscopy fellowship was initiated in 2011 and the therapeutic endoscopy fellow participated in most procedures thereafter. ERCP procedures included in the study were carried out by a single therapeutic endoscopist with over 10 years of therapeutic endoscopy experience at the beginning of the study period (2008).
All analyses were carried out using SAS Enterprise Guide version 7.11 HF3 (SAS Institute Inc., Cary, NC, United States) and Microsoft Excel. Continuous data were analyzed for normality. Because most distributions did not appear normal, Student’s t-test was conducted. Adverse events were analyzed using the Fisher’s exact test for sparsely distributed data. Gender and cannulation rates were assessed by chi-squared test. Regression analyses were conducted using standard approaches. All reported P-values are 2-sided, and all comparisons attained statistical significance at P < 0.05. Correction for repeated measures was performed using standard approaches.
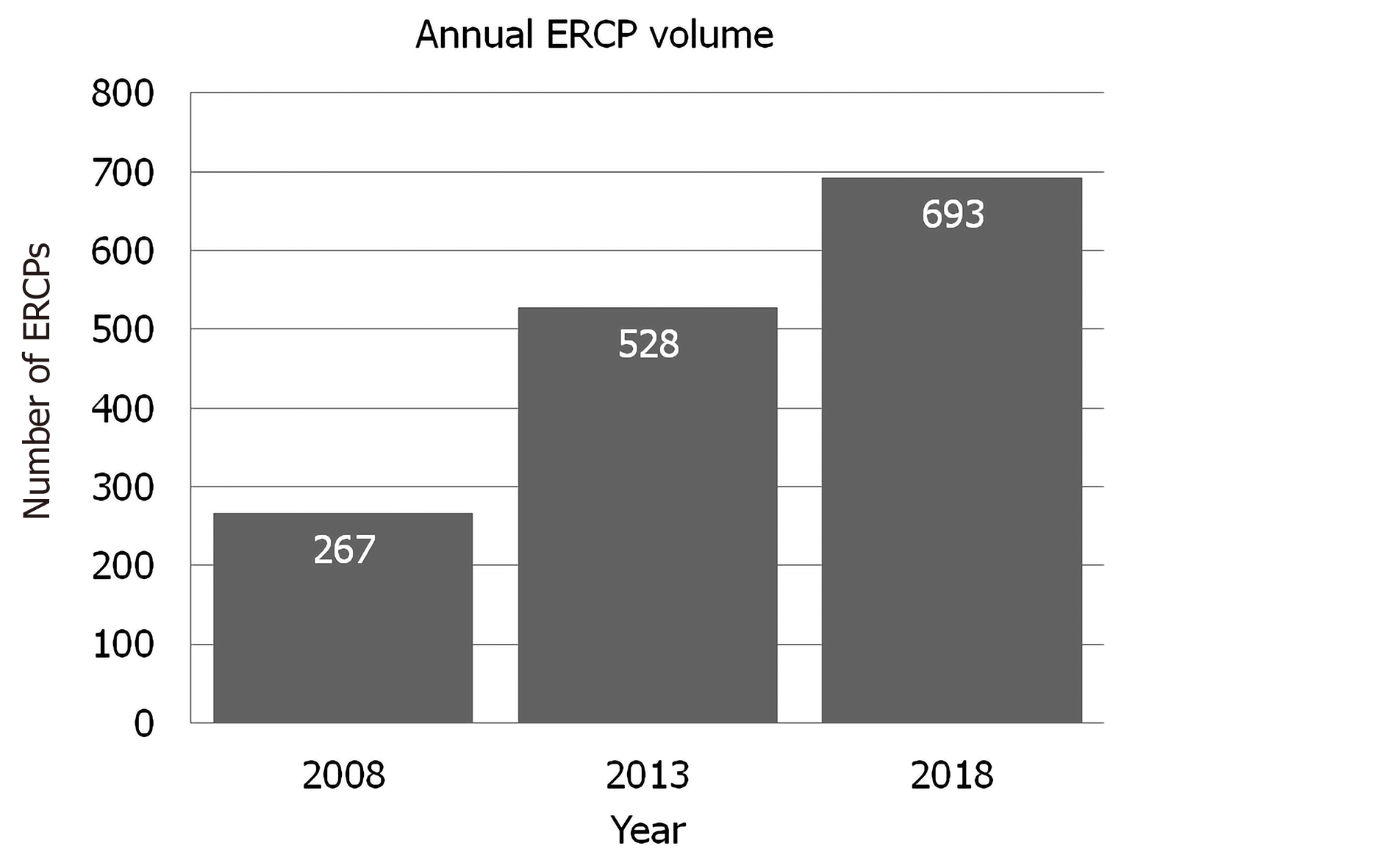
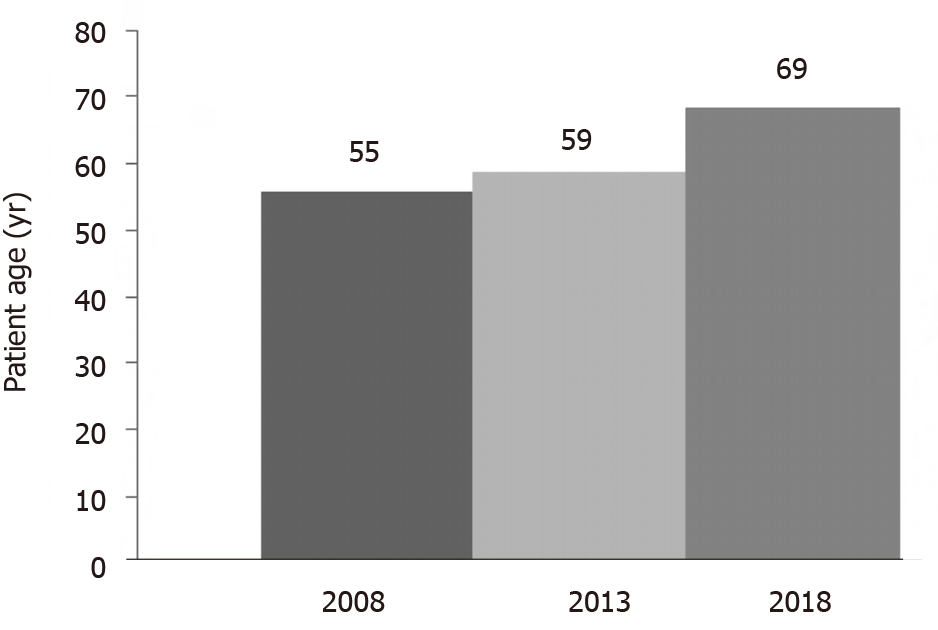
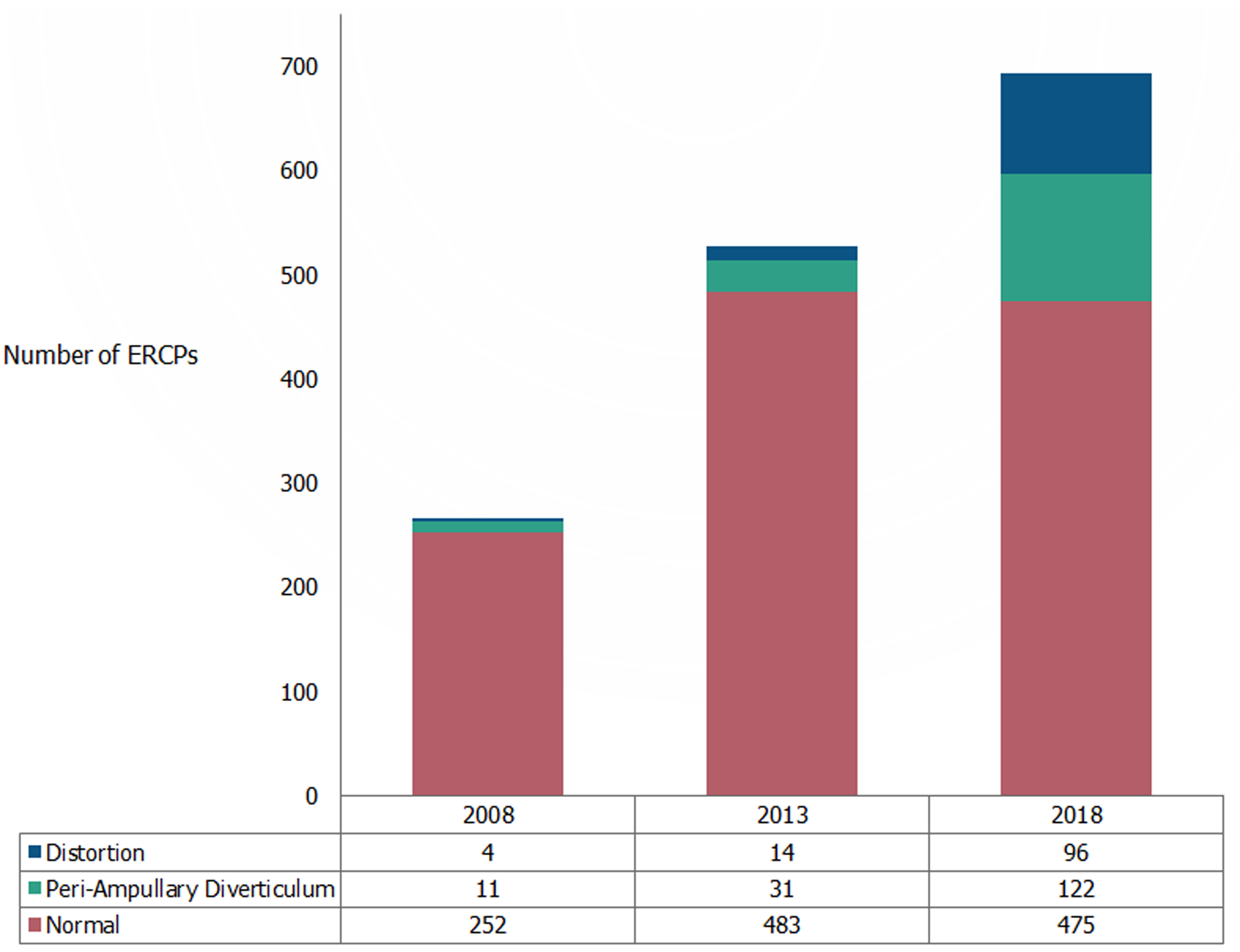
Annual endoscopist ERCP volume progressively increased over the study period, with 267 ERCPs performed in 2008, 528 ERCPs performed in 2013 and 693 ERCPs performed in 2018 (Figure 1). The mean age of ERCP patients was almost 15 years higher in 2018 compared to 2008 (69.7 ± 15.2 years vs 55.1 ± 14.7 years, P < 0.05, Figure 2).
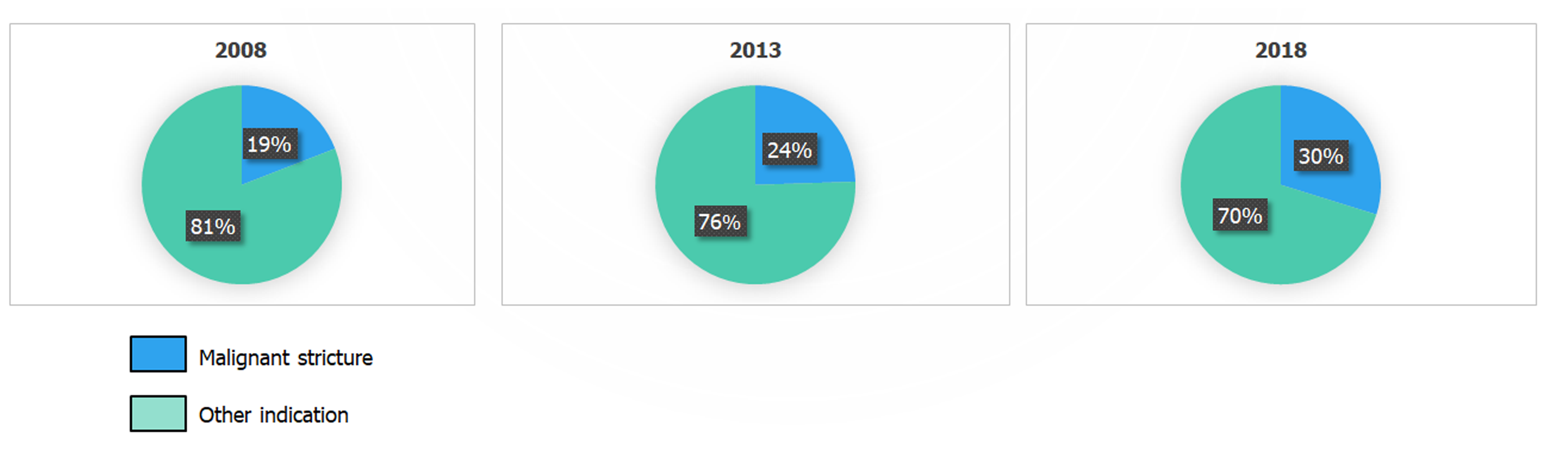
The overall distribution of ERCP indications did not significantly differ over the 10-year study period, when analyzed over the 10 year interval or at 5 year intervals. There was a trend toward an increased proportion of ERCPs performed for biliary stricture evaluation and management, from 19% in 2008 to 24% in 2013 and 29% in 2018 (P = 0.07, Figure 3), however this did not reach statistical significance when correction for repeated measures was performed.
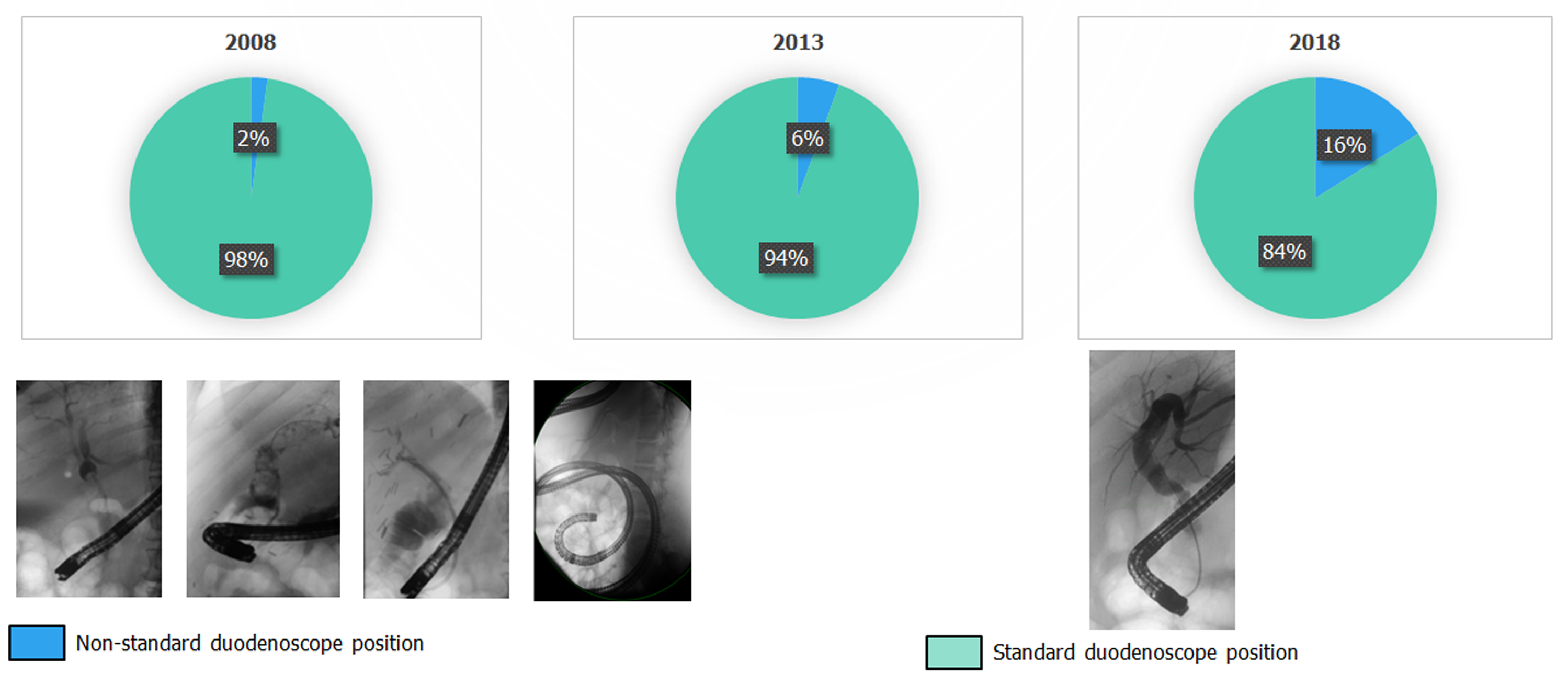
The proportion of ERCPs performed using a non-standard duodenoscope position increased over time, from 2.2% (2008) to 5.6% (2013) and then 16.1% (2018) (P < 0.001, Figure 4).
A progressive increase in the proportion of patients undergoing ERCP with procedures notable for ampullary distortion, peri-ampullary diverticula, tumor infiltration, and duodenal distortion/stenosis was noted in 2018 (P < 0.001, Figure 1) compared to both 2008 and 2013 (Figure 5).
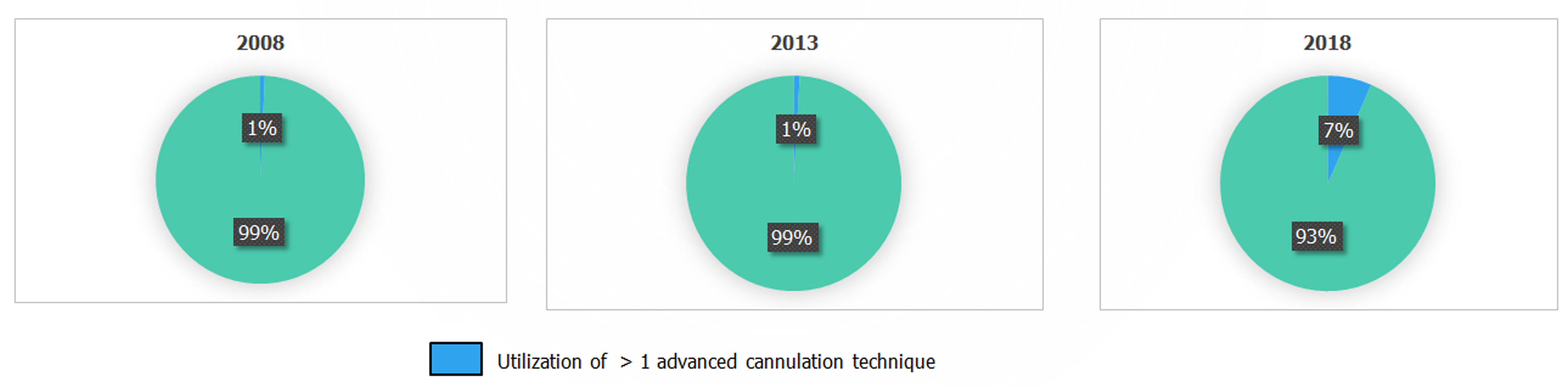
Utilization of greater than one advanced cannulation approach during a single ERCP, a marker for complexity and difficulty of an ERCP, remained relatively stable from 2008 to 2013 (0.7% and 0.9%, respectively), then rose to 6.6% in 2018 (P < 0.001, Figure 6).
In our regression analysis, mass size > 4 cm, pancreatic uncinate process tumor, and a bilirubin level of > 10 mg/dL predicted distortion of the both the ampulla and the duodenum. These features also predicted utilization of advanced biliary access techniques (P < 0.03 for each). Patient age, alkaline phosphatase, Alanine aminotransferase and Aspartate aminotransferase were evaluated in our regression analysis and did not predict anatomical distortion or advanced cannulation technique utilization (P > 0.1 for each).
Oropharyngeal barriers to duodenoscope advancement were evident in 6% of patients in 2018, representing an over 5-fold increase over the past 10 years (Figure 7A). Notably, for three of these patients, oropharyngeal barriers to duodenoscope advancement prevented performance of ERCP. An over 6-fold rise in the proportion of ERCPs with esophageal barriers to duodenoscope advancement was noted over the past 10 years, with an over 2-fold increase in the past 5 years (Figure 7B). In 2018, 8 patients required either esophageal dilation (5) or esophageal stent placement (3) to facilitate ERCP. Gastric barriers to duodenoscope advancement were also increasingly apparent over the study period, with a 2-fold increase in the proportion of patients with gastric barriers to duodenoscope advancement in the past 10 years (Figure 7C). Notably, 5% of patients who underwent ERCP at our center in 2018 had surgically altered gastric anatomy. Duodenal barriers to duodenoscope advancement and cannulation were encountered in a 10% of patients in 2018, which represents a 2-fold increase in the past 5 years (Figure 7D). Notably, 4% of patients required duodenal dilation or duodenal stent placement to accomplish ERCP in 2018.
We demonstrate that, at our tertiary care academic medical center, biliary cannulation has become progressively more complex and challenging over the past decade. The vast majority of ERCPs are performed for biliary indications and biliary cannulation has always been considered challenging for a subset of procedures, even at high volume centers of excellence. Rates of native ampulla cannulation failure of up to 15% have been reported from these centers[20,21]. The American Society for Gastrointestinal Endoscopy has proposed a 90% cannulation rate as indicative of competence in ERCP in its recent privileging and credentialing guidelines[22]. However reported cannulation failure rates during advanced endoscopy training suggest that many trainees are not achieving these cannulation rates by the end of their fellowship training[23,24]. It is reasonable to assume that national cannulation failure rates are even higher, because most United States endoscopists have not undergone advanced endoscopy fellowship training and perform less than 100 ERCPs annually[2,7,25].
A trend toward lower rates of failed cannulation and decreased reliance on one or more advanced biliary access techniques might be expected from a high-volume expert endoscopist whose technical competency would be expected to increase over time. Our initial observation of precisely the inverse trend was the motivation for conducting this study in which we formally evaluated ERCP and cannulation complexity. Our systematic evaluation revealed progressively increasing anatomical complexity, with a higher proportion of patients who have post-surgical altered anatomy and other barriers to duodenoscope advancement and successful cannulation encountered at each level of the upper gastrointestinal tract proximal to the ampulla, from the oropharynx and esophagus to the stomach and duodenum.
The increasing complexity of ERCP over the past decade and the potential for progressively escalating complexity of ERCP over time may render the competency threshold of 90% successful biliary cannulation at ERCP challenging to achieve for even highly trained high volume endoscopists. Furthermore, the increasingly complex ERCPs being performed in the current era limits opportunities for trainee involvement in a substantial proportion of procedures and this, in turn, results in more limited training experience in preparation for management of these complex ERCPs when the trainee becomes an attending therapeutic endoscopist. Limiting or eliminating trainee involvement in biliary cannulations which are anticipated to be challenging may be the most appropriate practice, as cannulation has been found to fail more frequently if a beginner endoscopist initiates cannulation even when an ERCP is straightforward[26]. These issues are worthy of consideration for training future generations of endoscopists. If this trajectory toward increasing complexity of tertiary academic medical center ERCPs is evident at other similar centers, adaptations of therapeutic endoscopy training may be necessary to ensure endoscopist preparedness for these challenging procedures. Possible endoscopy training adaptations might include increased reliance on ERCP simulators, which have been developed and adapted for cannulation training[27-32]. Additionally, an endoscopy training partnership between academic medical centers and community hospitals which perform procedures that tend to be less complex, such as those for young patients to address choledocholithiasis, may be beneficial.
With the increased reliance on advanced biliary cannulation techniques, it is important to identify a reliably effective salvage cannulation approach which is safe and appropriate for use by lower volume endoscopists. We have previously demonstrated, in the largest study to-date of Goff septotomy, that this technique has a safety profile which is similar to standard cannulation techniques and superior to the more commonly used needle knife precut sphincterotomy[33]. While maintaining this favorable safety profile, Goff septotomy cannulation success rates are the highest of available advanced cannulation techniques, at over 87%[33]. Our safety and efficacy data in this recent study suggest that Goff septotomy may be considered as a primary salvage cannulation approach, with needle knife sphincterotomy reserved for Goff septotomy failures. In this era of increasingly complex ERCPs, data are needed from multiple academic and therapeutic endoscopy centers to assess the relative merits and disadvantages of the array of advanced biliary access techniques currently in use.
A key finding of this study is the fact that the complexity of cannulation during ERCP may be predicted by patient and ampullary features. In our regression analysis, a primary pancreatic or liver mass size over 4 cm in greatest dimension, tumor involvement of the pancreatic uncinate process, and bilirubin over 10 mg/dL predicted ampulla/duodenal distortion and utilization of advanced cannulation techniques. Other recent studies have found that the endoscopic appearance of the ampulla modulates the difficulty of and latency to biliary cannulation, with small ampullas and protruding, pendulous ampullas found to be more challenging to cannulate[26]. Additional recent studies have found that the presence of a peri-ampullary diverticulum predict ERCP-associated adverse events[34], and that the angle of the common bile duct may predict rates of post-ERCP pancreatitis for some endoscopists[35]. These tools with which cannulation complexity may be predicted are valuable for risk stratification and identification of patients for whom optimal patient care may include having an experienced attending perform the ERCP without trainee involvement.
Limitations of this study include its retrospective nature, reliance on data from the electronic medical record and procedure report/fluoroscopy image review. These data include only procedures from a single endoscopist, but this also serves as strength of the study in that this study design controls for discrepancies in endoscopist technical skill and evolution of that skill over time.
In conclusion, our tertiary care academic medical center findings indicate sharply increasing complexity of biliary cannulation over the past 5 years, with increasing proportions of elderly patients and those with advanced malignancy with anatomical distortion of the ampulla/duodenum requiring advanced cannulation techniques. These data synergize with recent studies and together suggest that complexity of cannulation may be predictable with consideration of patient and ampulla characteristics. In this new era of ERCP, these data may inform selection of high-volume, experienced endoscopists to perform complex ERCP procedures and these complex procedures may be less amenable to trainee involvement.
Endoscopic retrograde cholangiopancreatography (ERCP) is a technically challenging and high-risk endoscopic procedure. Cannulation of the duct of interest is the essential primary step in performance of a successful ERCP. At our tertiary care endoscopy unit, we have perceived an increase in the complexity of ERCPs, necessitating increased utilization of advanced biliary cannulation techniques.
Based on this impression of increasing cannulation complexity at ERCP, we designed a retrospective study to systematically evaluate the evolution of ERCP complexity over the past decade at our institution.
Our goal was to characterize changes in ERCP complexity over time so that training and practice patterns may be optimized in accordance with these changes. We intend for these findings to enhance understanding about the factors that underlie escalating complexity of cannulation at ERCP and stimulate future research on the topic.
Demographic/clinical variables and medical records of ERCP patients from the beginning (2008), middle (2013) and end (2018) of the last decade were evaluated and cannulation complexity was assessed (categorized as anatomical barriers, utilization of advanced cannulation techniques and duodenoscope position).
Patients undergoing ERCP in 2018 were significantly older compared to those undergoing ERCP in 2008, and a progressive increase in the proportion of procedures challenged by duodenal/ampullary distortion and peri-ampullary diverticula were noted over the same time period. ERCPs were increasingly performed with a non-standard duodenoscope position, and utilization of more than one advanced cannulation approach during a single ERCP increased significantly over the study period. Primary mass size > 4 cm, pancreatic uncinate tumor, and bilirubin > 10 mg/dL predicted use of advanced cannulation techniques.
ERCP cannulation complexity has sharply increased over the past 5 years, with more elderly patients and patients with malignancy undergoing ERCP, necessitating an increased utilization of advanced cannulation techniques. We found that cannulation complexity at ERCP can be predicted based on patient/ampullary characteristics. Anatomical barriers to duodenoscope advancement prior to cannulation are also increasingly common.
In this new era of escalating complexity of cannulation during ERCP, our data may inform triaging of procedures predicated to be highly complex to more experienced, high-volume endoscopists. These highly complex ERCPs may be less amenable to trainee involvement. Our data highlight the increasing importance of excellent advanced endoscopy training for endoscopists who will perform ERCP.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Li Y, Shi H S-Editor: Zhang H L-Editor: A P-Editor: Ma YJ
| 1. | ASGE Standards of Practice Committee, Chandrasekhara Khashab MA, Muthusamy VR, Acosta RD, Agrawal D, Bruining DH, Eloubeidi MA, Fanelli RD, Faulx AL, Gurudu SR, Kothari S, Lightdale JR, Qumseya BJ, Shaukat A, Wang A, Wani SB, Yang J, DeWitt JM. Adverse events associated with ERCP. Gastrointest Endosc. 2017;85:32-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 405] [Cited by in RCA: 531] [Article Influence: 66.4] [Reference Citation Analysis (0)] |
| 2. | Huang RJ, Thosani NC, Barakat MT, Choudhary A, Mithal A, Singh G, Sethi S, Banerjee S. Evolution in the utilization of biliary interventions in the United States: results of a nationwide longitudinal study from 1998 to 2013. Gastrointest Endosc 2017; 86: 319-326. e5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 61] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 3. | Williams EJ, Taylor S, Fairclough P, Hamlyn A, Logan RF, Martin D, Riley SA, Veitch P, Wilkinson M, Williamson PR, Lombard M; BSG Audit of ERCP. Are we meeting the standards set for endoscopy? Gut. 2007;56:821-829. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 160] [Cited by in RCA: 178] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 4. | Strömberg C, Nilsson M. Nationwide study of the treatment of common bile duct stones in Sweden between 1965 and 2009. Br J Surg. 2011;98:1766-1774. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 33] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 5. | Freeman ML, DiSario JA, Nelson DB, Fennerty MB, Lee JG, Bjorkman DJ, Overby CS, Aas J, Ryan ME, Bochna GS, Shaw MJ, Snady HW, Erickson RV, Moore JP, Roel JP. Risk factors for post-ERCP pancreatitis: a prospective, multicenter study. Gastrointest Endosc. 2001;54:425-434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 801] [Cited by in RCA: 835] [Article Influence: 34.8] [Reference Citation Analysis (0)] |
| 6. | Bailey AA, Bourke MJ, Williams SJ, Walsh PR, Murray MA, Lee EY, Kwan V, Lynch PM. A prospective randomized trial of cannulation technique in ERCP: effects on technical success and post-ERCP pancreatitis. Endoscopy. 2008;40:296-301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 164] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 7. | Huang RJ, Barakat MT, Girotra M, Lee JS, Banerjee S. Unplanned Hospital Encounters After Endoscopic Retrograde Cholangiopancreatography in 3 Large North American States. Gastroenterology 2019; 156: 119-129. e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 28] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 8. | Cotton PB. Are low-volume ERCPists a problem in the United States? Gastrointest Endosc. 2011;74:161-166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 38] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 9. | Varadarajulu S, Kilgore ML, Wilcox CM, Eloubeidi MA. Relationship among hospital ERCP volume, length of stay, and technical outcomes. Gastrointest Endosc. 2006;64:338-347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 116] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 10. | Peng C, Nietert PJ, Cotton PB, Lackland DT, Romagnuolo J. Predicting native papilla biliary cannulation success using a multinational Endoscopic Retrograde Cholangiopancreatography (ERCP) Quality Network. BMC Gastroenterol. 2013;13:147. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 55] [Cited by in RCA: 62] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 11. | Deans GT, Sedman P, Martin DF, Royston CM, Leow CK, Thomas WE, Brough WA. Are complications of endoscopic sphincterotomy age related? Gut. 1997;41:545-548. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 46] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 12. | Suissa A, Yassin K, Lavy A, Lachter J, Chermech I, Karban A, Tamir A, Eliakim R. Outcome and early complications of ERCP: a prospective single center study. Hepatogastroenterology. 2005;52:352-355. [PubMed] |
| 13. | Andriulli A, Loperfido S, Napolitano G, Niro G, Valvano MR, Spirito F, Pilotto A, Forlano R. Incidence rates of post-ERCP complications: a systematic survey of prospective studies. Am J Gastroenterol. 2007;102:1781-1788. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 669] [Cited by in RCA: 771] [Article Influence: 42.8] [Reference Citation Analysis (0)] |
| 14. | Cotton PB, Garrow DA, Gallagher J, Romagnuolo J. Risk factors for complications after ERCP: a multivariate analysis of 11,497 procedures over 12 years. Gastrointest Endosc. 2009;70:80-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 449] [Cited by in RCA: 467] [Article Influence: 29.2] [Reference Citation Analysis (0)] |
| 15. | Salminen P, Laine S, Gullichsen R. Severe and fatal complications after ERCP: analysis of 2555 procedures in a single experienced center. Surg Endosc. 2008;22:1965-1970. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 54] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 16. | Testoni PA, Mariani A, Giussani A, Vailati C, Masci E, Macarri G, Ghezzo L, Familiari L, Giardullo N, Mutignani M, Lombardi G, Talamini G, Spadaccini A, Briglia R, Piazzi L; SEIFRED Group. Risk factors for post-ERCP pancreatitis in high- and low-volume centers and among expert and non-expert operators: a prospective multicenter study. Am J Gastroenterol. 2010;105:1753-1761. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 184] [Cited by in RCA: 200] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 17. | Olsson G, Arnelo U, Swahn F, Törnqvist B, Lundell L, Enochsson L. The H.O.U.S.E. classification: a novel endoscopic retrograde cholangiopancreatography (ERCP) complexity grading scale. BMC Gastroenterol. 2017;17:38. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 25] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 18. | Cotton PB, Eisen G, Romagnuolo J, Vargo J, Baron T, Tarnasky P, Schutz S, Jacobson B, Bott C, Petersen B. Grading the complexity of endoscopic procedures: results of an ASGE working party. Gastrointest Endosc. 2011;73:868-874. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 192] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 19. | Ragunath K, Thomas LA, Cheung WY, Duane PD, Richards DG. Objective evaluation of ERCP procedures: a simple grading scale for evaluating technical difficulty. Postgrad Med J. 2003;79:467-470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 31] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 20. | Freeman ML. Cannulation techniques for ERCP: one size does not fit all. Gastrointest Endosc. 2007;65:132-133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 21. | Freeman ML, Guda NM. ERCP cannulation: a review of reported techniques. Gastrointest Endosc. 2005;61:112-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 215] [Cited by in RCA: 224] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 22. | ASGE Standards of Practice Committee, Faulx AL, Lightdale JR, Acosta RD, Agrawal D, Bruining DH, Chandrasekhara V, Eloubeidi MA, Gurudu SR, Kelsey L, Khashab MA, Kothari S, Muthusamy VR, Qumseya BJ, Shaukat A, Wang A, Wani SB, Yang J, DeWitt JM. Guidelines for privileging, credentialing, and proctoring to perform GI endoscopy. Gastrointest Endosc. 2017;85:273-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 156] [Article Influence: 19.5] [Reference Citation Analysis (0)] |
| 23. | Wani S, Keswani R, Hall M, Han S, Ali MA, Brauer B, Carlin L, Chak A, Collins D, Cote GA, Diehl DL, DiMaio CJ, Dries A, El-Hajj I, Ellert S, Fairley K, Faulx A, Fujii-Lau L, Gaddam S, Gan SI, Gaspar JP, Gautamy C, Gordon S, Harris C, Hyder S, Jones R, Kim S, Komanduri S, Law R, Lee L, Mounzer R, Mullady D, Muthusamy VR, Olyaee M, Pfau P, Saligram S, Piraka C, Rastogi A, Rosenkranz L, Rzouq F, Saxena A, Shah RJ, Simon VC, Small A, Sreenarasimhaiah J, Walker A, Wang AY, Watson RR, Wilson RH, Yachimski P, Yang D, Edmundowicz S, Early DS. A Prospective Multicenter Study Evaluating Learning Curves and Competence in Endoscopic Ultrasound and Endoscopic Retrograde Cholangiopancreatography Among Advanced Endoscopy Trainees: The Rapid Assessment of Trainee Endoscopy Skills Study. Clin Gastroenterol Hepatol 2017; 15: 1758-1767. e11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 83] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 24. | Granato CM, Kaul V, Kothari T, Damania D, Kothari S. Career prospects and professional landscape after advanced endoscopy fellowship training: a survey assessing graduates from 2009 to 2013. Gastrointest Endosc. 2016;84:266-271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 25. | Coté GA, Imler TD, Xu H, Teal E, French DD, Imperiale TF, Rosenman MB, Wilson J, Hui SL, Sherman S. Lower provider volume is associated with higher failure rates for endoscopic retrograde cholangiopancreatography. Med Care. 2013;51:1040-1047. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 65] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 26. | Haraldsson E, Kylänpää L, Grönroos J, Saarela A, Toth E, Qvigstad G, Hult M, Lindström O, Laine S, Karjula H, Hauge T, Sadik R, Arnelo U. Macroscopic appearance of the major duodenal papilla influences bile duct cannulation: a prospective multicenter study by the Scandinavian Association for Digestive Endoscopy Study Group for ERCP. Gastrointest Endosc. 2019;90:957-963. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 62] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 27. | Nguyen TT, Kim M, Lee DY. A hybrid contact model for cannulation simulation of ERCP. Stud Health Technol Inform. 2014;196:304-306. [PubMed] |
| 28. | Artifon EL, Ramirez ME, Ardengh JC, Sartor MC, Favaro GM, Belmonte E, Lobo J, Coelho D, Pereira-Lima J, Lopez CV, Matuguma SE, Furuya CK Jr, Pisani J, Cheng S, Buch MA, Franzini T, Vilela TF, Pessoa R, Bonin E, Lera M, Nakadomari TS, Kashiwagui LY, Gerber MT, Mascarenhas R. Ex vivo and simulator models teaching therapeutic ERCP and EUS: description of SOBED's first course. Rev Gastroenterol Peru. 2016;36:231-241. [PubMed] |
| 29. | Leung JW, Wang D, Hu B, Lim B, Leung FW. A head-to-head hands-on comparison of ERCP mechanical simulator (EMS) and Ex-vivo Porcine Stomach Model (PSM). J Interv Gastroenterol. 2011;1:108-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 30. | Liao WC, Leung JW, Wang HP, Chang WH, Chu CH, Lin JT, Wilson RE, Lim BS, Leung FW. Coached practice using ERCP mechanical simulator improves trainees' ERCP performance: a randomized controlled trial. Endoscopy. 2013;45:799-805. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 31] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 31. | Lim BS, Leung JW, Lee J, Yen D, Beckett L, Tancredi D, Leung FW. Effect of ERCP mechanical simulator (EMS) practice on trainees' ERCP performance in the early learning period: US multicenter randomized controlled trial. Am J Gastroenterol. 2011;106:300-306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 47] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 32. | Sahakian AB, Laine L, Jamidar PA, Siddiqui UD, Duffy A, Ciarleglio MM, Deng Y, Nagar A, Aslanian HR. Can a Computerized Simulator Assess Skill Level and Improvement in Performance of ERCP? Dig Dis Sci. 2016;61:722-730. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 33. | Barakat MT, Girotra M, Huang RJ, Choudhary A, Thosani NC, Kothari S, Sethi S, Banerjee S. Goff Septotomy Is a Safe and Effective Salvage Biliary Access Technique Following Failed Cannulation at ERCP. Dig Dis Sci. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 34. | Karaahmet F, Kekilli M. The presence of periampullary diverticulum increased the complications of endoscopic retrograde cholangiopancreatography. Eur J Gastroenterol Hepatol. 2018;30:1009-1012. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 35. | Han SY, Kim DU, Lee MW, Park YJ, Baek DH, Kim GH, Song GA. Acute distal common bile duct angle is risk factor for post-endoscopic retrograde cholangiopancreatography pancreatitis in beginner endoscopist. World J Clin Cases. 2020;8:20-28. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |