Published online Sep 14, 2020. doi: 10.3748/wjg.v26.i34.5207
Peer-review started: May 28, 2020
First decision: June 12, 2020
Revised: June 29, 2020
Accepted: August 21, 2020
Article in press: August 21, 2020
Published online: September 14, 2020
Processing time: 103 Days and 14.5 Hours
Pancreatic duct stones can lead to significant abdominal pain for patients. Per oral pancreatoscopy (POP)-guided intracorporal lithotripsy is being increasingly used for the management of main pancreatic duct calculi (PDC) in chronic pancreatitis. POP uses two techniques: Electrohydraulic lithotripsy (EHL) and laser lithotripsy (LL). Data on the safety and efficacy are limited for this procedure. We performed a systematic review and meta-analysis with a primary aim to calculate the pooled technical and clinical success rates of POP. The secondary aim was to assess pooled rates of technical success, clinical success for the two individual techniques, and adverse event rates.
To perform a systematic review and meta-analysis of POP, EHL and LL for management of PDC in chronic pancreatitis.
We conducted a comprehensive search of multiple electronic databases and conference proceedings including PubMed, EMBASE, Cochrane, Google Scholar and Web of Science databases (from 1999 to October 2019) to identify studies with patient age greater than 17 and any gender that reported on outcomes of POP, EHL and LL. The primary outcome assessed involved the pooled technical success and clinical success rate of POP. The secondary outcome included the pooled technical success and clinical success rate for EHL and LL. We also assessed the pooled rate of adverse events for POP, EHL and LL including a subgroup analysis for the rate of adverse event subtypes for POP: Hemorrhage, post-endoscopic retrograde cholangiopancreatography pancreatitis (PEP), perforation, abdominal pain, fever and infections. Technical success was defined as the rate of clearing pancreatic duct stones and clinical success as the improvement in pain. Random-effects model was used for analysis. Heterogeneity between study-specific estimates was calculated using the Cochran Q statistical test and I2 statistics. Publication bias was ascertained, qualitatively by visual inspection of funnel plot and quantitatively by the Egger test.
A total of 16 studies including 383 patients met the inclusion criteria. The technical success rate of POP was 76.4% (95%CI: 65.9-84.5; I2 = 64%) and clinical success rate was 76.8% (95%CI: 65.2-85.4; I2 = 66%). The technical success rate of EHL was 70.3% (95%CI: 57.8-80.3; I2 = 36%) and clinical success rate of EHL was 66.5% (95%CI: 55.2-76.2; I2 = 19%). The technical success rate of LL was 89.3% (95%CI: 70.5-96.7; I2 = 70%) and clinical success rate of LL was 88.2% (95%CI: 66.4-96.6; I2 = 77%). The incidence of pooled adverse events for POP was 14.9% (95%CI: 9.2-23.2; I2 = 49%), for EHL was 11.2% (95%CI: 5.9-20.3; I2 = 15%) and for LL was 13.1% (95%CI: 6.3-25.4; I2 = 31%). Subgroup analysis of adverse events showed rates of PEP at 7% (95%CI: 3.5-13.6; I2 = 38%), fever at 3.7% (95%CI: 2-6.9; I2 = 0), abdominal pain at 4.7% (95%CI: 2.7-7.8; I2 = 0), perforation at 4.3% (95%CI: 2.1-8.4; I2 = 0), hemorrhage at 3.4% (95%CI: 1.7-6.6; I2 = 0) and no mortality. There was evidence of publication bias based on funnel plot analysis and Egger’s test.
Our study highlights the high technical and clinical success rates for POP, EHL and LL. POP-guided lithotripsy could be a viable option for management of chronic pancreatitis with PDC.
Core Tip: Current management for symptomatic pancreatic duct stones is extracorporeal shock wave lithotripsy (ESWL) or endoscopic retrograde cholangiopancreatography (ERCP) followed by surgery if the former is unsuccessful. Sparse data exists regarding safety and efficacy of per oral pancreatoscopy (POP)- guided lithotripsy. This is the first systematic review and meta-analysis evaluating safety and efficacy of POP using electrohydraulic lithotripsy and laser lithotripsy. The POP procedure is of interest compared to current standard of care due to the ability to directly visualize pancreatic duct calculi, perform lithotripsy and extract the stones in the same session. ESWL and ERCP require multiple sessions and have low technical success.
- Citation: Saghir SM, Mashiana HS, Mohan BP, Dhindsa BS, Dhaliwal A, Chandan S, Bhogal N, Bhat I, Singh S, Adler DG. Efficacy of pancreatoscopy for pancreatic duct stones: A systematic review and meta-analysis. World J Gastroenterol 2020; 26(34): 5207-5219
- URL: https://www.wjgnet.com/1007-9327/full/v26/i34/5207.htm
- DOI: https://dx.doi.org/10.3748/wjg.v26.i34.5207
Pancreatic duct (PD) stones are a common complication of chronic pancreatitis (CP), which can lead to obstruction of the PD and cause chronic abdominal pain and exocrine pancreatic insufficiency[1]. PD stones may be present in as many as 50%-90% of CP patients[1,2]. The cause of the pain is multifactorial, but is thought to be secondary to elevated pancreatic ductal pressures, elevated interstitial pancreatic pressure, ischemia, fibrosis, and inflammation-related injury to the nerves innervating the pancreas[1]. Relieving PD obstruction is an important aspect in treatment of patients with painful chronic pancreatitis.
Current management of symptomatic PD stones includes medical therapy such as pancreatic enzyme replacement therapy (PERT), extracorporeal shock wave lithotripsy (ESWL) with or without endoscopic retrograde cholangiopancreatography (ERCP), ERCP with pancreatic sphincterotomy and either balloon or basket retrieval with stent placement, peroral pancreatoscopy and/or surgery[1,2]. According to the 2018 European Society of Gastrointestinal Endoscopy (ESGE) and the 2017 United European Gastroenterology (UEG) guidelines, ESWL is the first line approach for patients with painful PD stones who have failed in medical therapy and who have stones greater than 5 mm[3,4]. ERCP is recommended for stones less than 5 mm[4]. The American College of Gastroenterology (ACG) 2020 guidelines recommend ERCP/interventional endoscopic ultrasound (EUS) for PD stone management[5]. If these modalities are unsuccessful, pancreatic surgery should be considered[6,7].
Per oral pancreatoscopy (POP)-guided lithotripsy is being increasingly used for the management of main pancreatic duct calculi (PDC) in the setting of CP[2,8]. Previously two operators were required to do this procedure and imaging quality was poor, but with the advent of newer technology, POP by single operator is now widely available[9]. POP uses two techniques: Electrohydraulic lithotripsy (EHL) and laser lithotripsy (LL). EHL technique uses a charge generator and bipolar probe to create a spark to produce a vapor plasma. The vapor plasma becomes a cavitation bubble that oscillates around the tip of the probe, which leads to stone fragmentation by absorption of rebounding shockwaves from the vapor. LL technique uses laser light at a specific wavelength to induce fragmentation[1]. Both techniques simply fragment stones into smaller pieces that still need to be removed via balloon and basket retrieval devices.
Information about the safety profile of POP and ESWL is limited. We performed a systematic review and meta-analysis on POP to assess the two techniques with regards to stone fragmentation, safety, and efficacy.
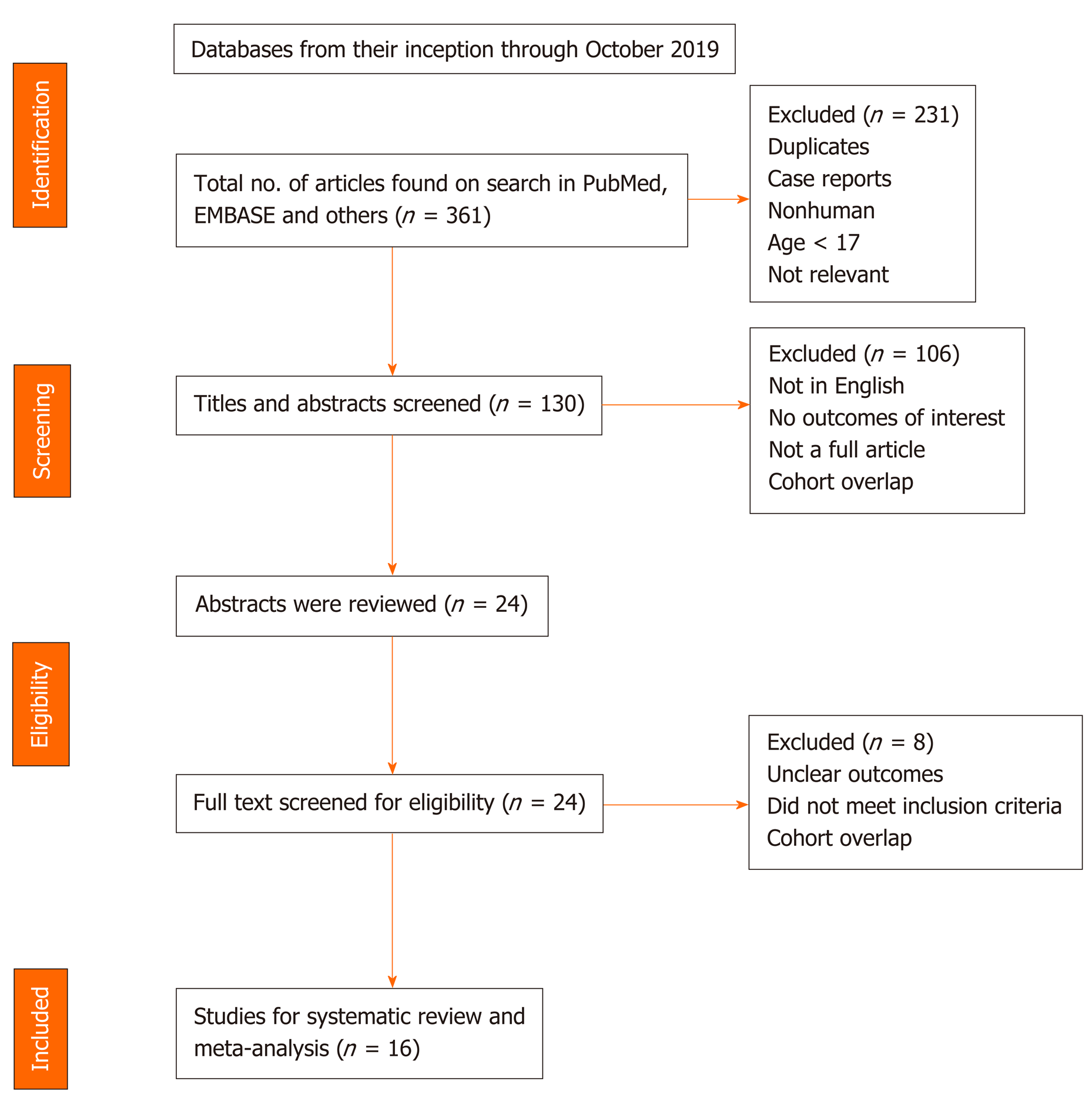
We conducted a comprehensive search of multiple electronic databases and conference proceedings including PubMed, EMBASE, Cochrane, Google Scholar, and Web of Science databases (from 1999 to October 2019). We identified studies reporting on outcomes of POP-guided intracorporal lithotripsy and followed the Preferred Reporting items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines[10]. The schematic diagram of study selection as per PRISMA guidelines is illustrated in Figure 1.
Literature search keywords included a combination of “per-oral”, “pancrea-toscopy”, “pancreatoscope”, “POP”, “electrohydraulic”, “EHL”, “laser”, “lithotripsy”, “LL”, “pancreas”, “calculi”, “stones”, “chronic” and “pancreatitis”. The literature retrieved was restricted to studies done on humans and published in English. Two authors (BD, HS) independently evaluated titles and abstracts obtained from the literature search and discarded any studies that were irrelevant to our topic, based on predetermined inclusion and exclusion criteria. We then reviewed the complete versions of the articles of interest to determine if they contained relevant context. Any article with discrepancies was reviewed by a third author (SS).
Additional relevant articles were discovered from the bibliographic sections from the articles of interest.
In this meta-analysis, studies that discussed the use of POP, EHL, and LL in patients with pancreatic duct stones were included. We included relevant studies for the data analysis regardless of their geographical location, inpatient/outpatient setting, or abstract/manuscript status.
The exclusion criteria included the following: (1) Alternative therapies for management of pancreatic duct stones other than POP; (2) Use of POP for indications other than for pancreatic duct stones; (3) Studies of the pediatric population (age < 17 years); and (4) Studies published in languages other than English.
In instances where there were multiple articles from the same cohort or overlapping cohorts, we used the ones that were the most relevant, comprehensive and/or recent.
Information regarding study-related outcomes from the individual studies was extracted onto a standardized form by three authors (BD, HM, SMS).
The collected data was evaluated akin to single group cohort studies and thus, we used the Newcastle-Ottawa scale to assess the quality of these studies[11]. Details of the scale is provided in Supplementary Table 1.
| Ref. | Year | Type of study | Center | Mean age (yr) | No. of patients | Males | Females | ||
| Total | EHL | LL | Total | Total | |||||
| Howell et al[29] | 1999 | Prospective | Single | 62.5 | 6 | 6 | 0 | 5 | 1 |
| Hirai et al[28] | 2004 | Prospective | Single | 51.2 | 17 | 0 | 17 | 9 | 8 |
| Brauer et al[30] | 2007 | Prospective | Single | 54 | 27 | 27 | 0 | 12 | 15 |
| Chen et al[8] | 2008 | Prospective | Single | -- | 10 | 10 | 0 | -- | -- |
| Fishman et al[9] | 2009 | Retrospective | Multi | -- | 6 | 6 | 0 | -- | -- |
| Maydeo et al[27] | 2011 | Prospective | Single | -- | 4 | 0 | 4 | -- | -- |
| Shah et al[26] | 2012 | Retrospective | Multi | 51 | 28 | 0 | 28 | -- | -- |
| Alatawi et al[31] | 2013 | Prospective | Single | 53.8 | 5 | 0 | 5 | 4 | 1 |
| Ito et al[23] | 2014 | Prospective | Single | -- | 8 | 8 | 0 | -- | -- |
| Malachias et al[24] | 2017 | Retrospective | Single | -- | 19 | 0 | 19 | 13 | 6 |
| Bekkali et al[7] | 2017 | Retrospective | Single | 45 | 6 | 6 | 0 | 3 | 3 |
| Canena et al[20] | 2019 | Prospective | Multi | -- | 3 | 2 | 1 | 3 | 0 |
| Gerges et al[21] | 2019 | Retrospective | Multi | 62.4 | 20 | 2 | 18 | 11 | 9 |
| Brewer Gutierrez et al[2] | 2019 | Retrospective | Multi | 54.7 | 109 | 59 | 50 | 77 | 32 |
| Ogura et al[25] | 2019 | Prospective | Single | 55 | 21 | 21 | 0 | 15 | 6 |
| Han et al[22] | 2019 | Retrospective | Single | -- | 94 | -- | -- | -- | -- |
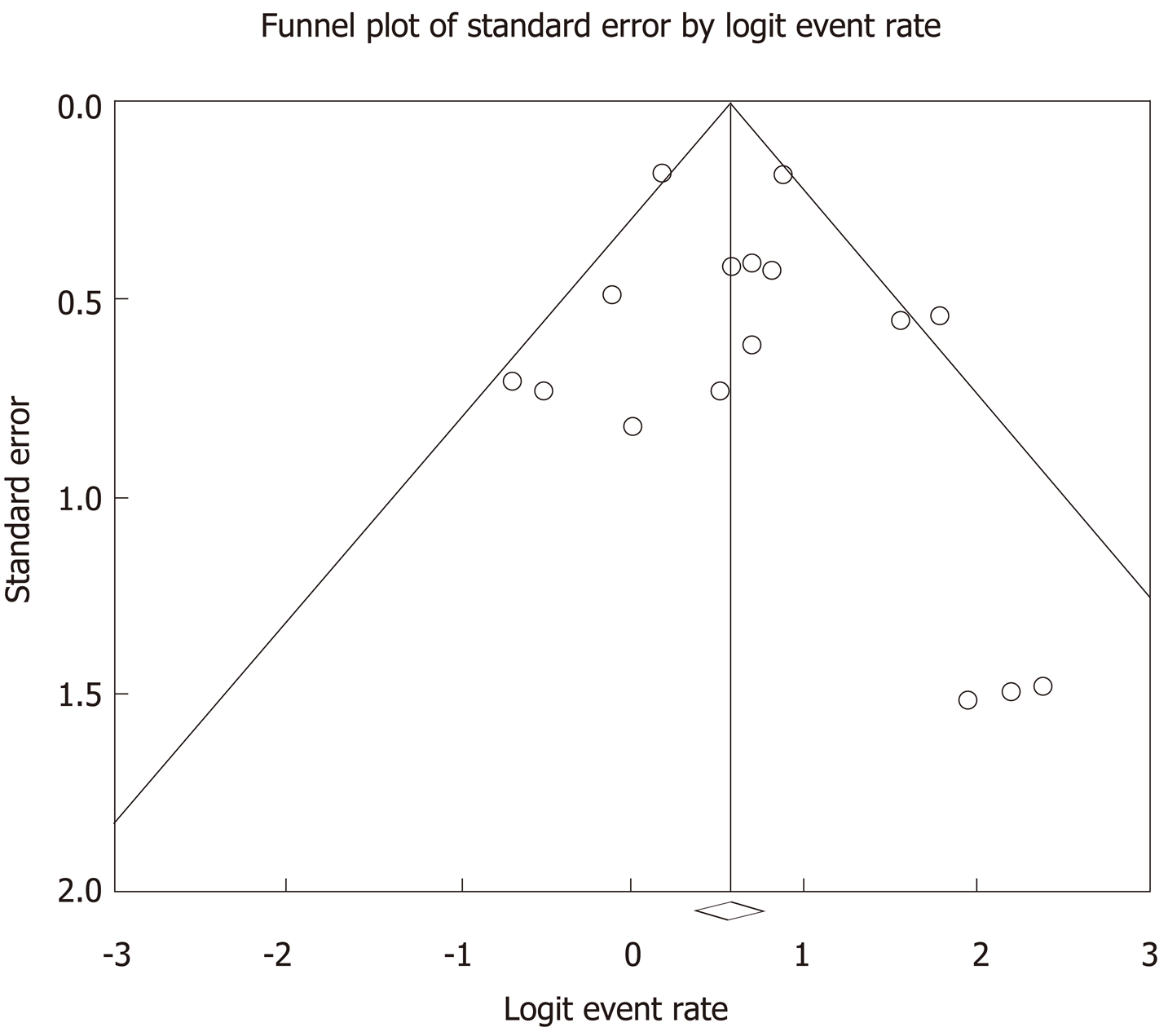
The pooled estimates were calculated with meta-analysis techniques as per DerSimonian and Laird using the random-effects model[12]. A continuity correction of 0.5 was added to the number of incident cases if incidence of an outcome was zero before statistical analysis[13]. Heterogeneity was evaluated via Cochrane Q statistical test for heterogeneity and the I2 statistics[14,15]. I2 values of < 30%, 30% to 60%, 61% to 75%, and > 75% were indicative of low, moderate, substantial, and significant heterogeneity, respectively[16]. Publication bias was determined quantitatively via the Egger test and qualitatively via visual inspection of the funnel plot[17]. With the presence of publication bias, we used the fail-safe N test and the Duval and Tweedie’s “Trim and Fill” test to determine the impact of the bias[18]. Impact was described in three levels based on similarities between the reported results and of those estimated as if there were no bias. Impact was classified as minimal if versions of both results were valued to be same, modest if there was substantial change in effect size, but the conclusion remained the same, or severe if the final conclusion of the analysis was subject to change by the bias[19].
All of our analyses were executed using comprehensive meta-analysis software, version 3 (BioStat, Englewood, NJ, United States).
Primary outcomes: (1) Pooled technical success rate of POP-guided lithotripsy; and (2) Pooled clinical success rate of POP-guided lithotripsy.
Secondary outcomes: (1) Pooled technical success rate: EHL and LL; (2) Pooled clinical success rate: EHL and LL; (3) Pooled rate of adverse events (AE): POP, EHL and LL; and (4) Pooled rate of AE subtypes for POP: Hemorrhage, post-ERCP pancreatitis (PEP), perforation, abdominal pain, fever and infections.
Our initial search yielded 361 results. There was a total of 16 studies that reported on POP lithotripsy procedures. Ten of these studies reported outcomes on POP using EHL[2,7-9,20,21,23,25,29,30] and 8 studies reported outcomes on POP using LL[2,20,21,24,26-28,31].
Ten of the 16 studies reported gender differences, with 65% of the population being male. The mean age reported in 9 of the 16 studies on POP was 54.4 years. The patient demographics are shown in Table 1.
Nine studies were prospective, and the rest were retrospective. Eleven studies were from a single center and the remainder from multicenters. Twelve studies were in full text and 4 studies were in abstract form. There were no population-based studies. The clinical outcomes from all studies were adequately documented.
A total of 383 patients underwent 464 POP procedures. One hundred and forty-seven patients underwent 265 EHL procedures. One hundred and forty-two patients underwent 199 LL procedures.
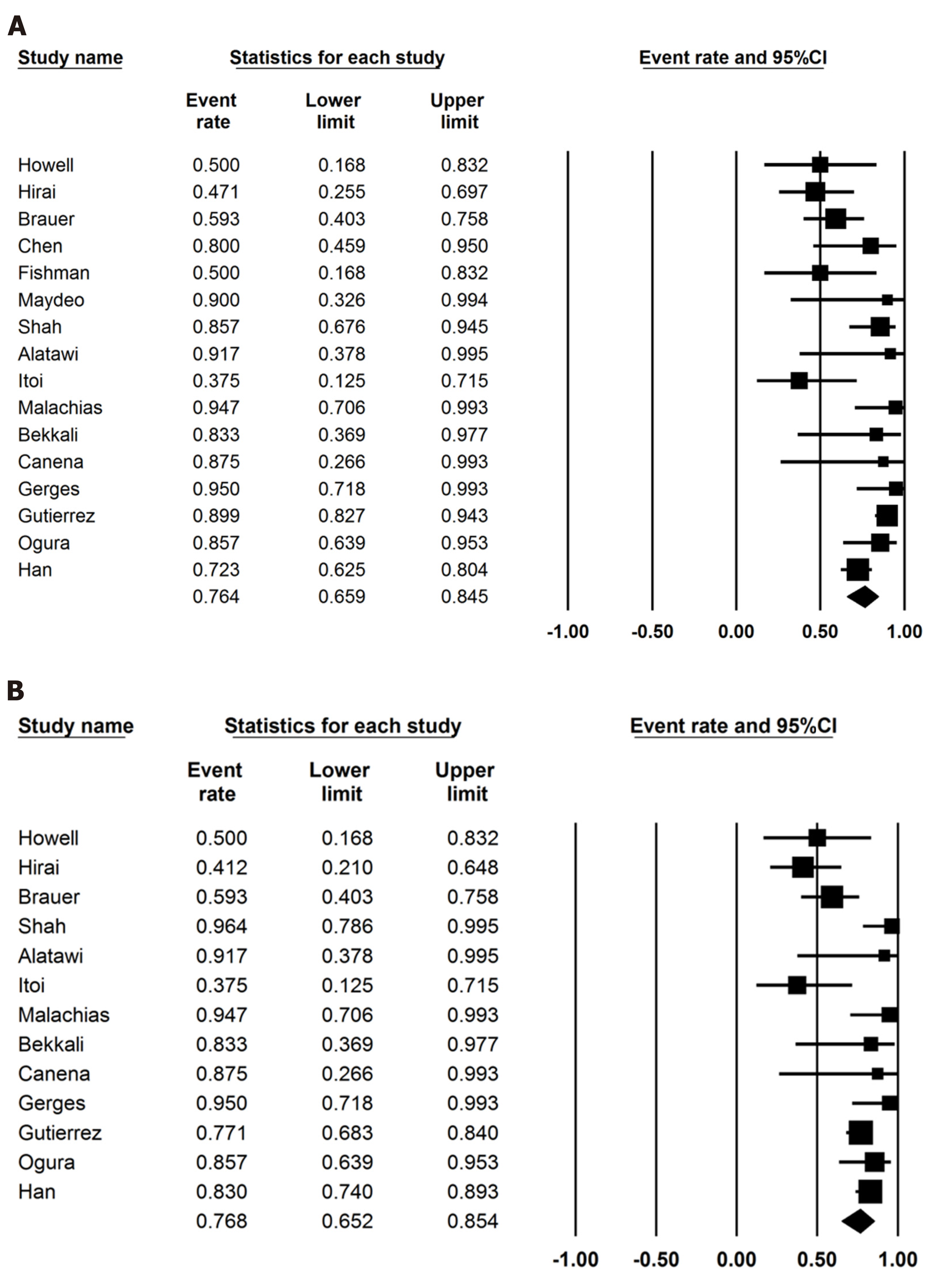
The pooled technical success rate of POP was 76.4% (95%CI: 65.9-84.5; I2 = 64%) and the pooled clinical success rate of POP was 76.8% (95%CI: 65.2-85.4; I2 = 66%). Figure 2 shows the forest plots for technical and clinical success of POP, respectively.
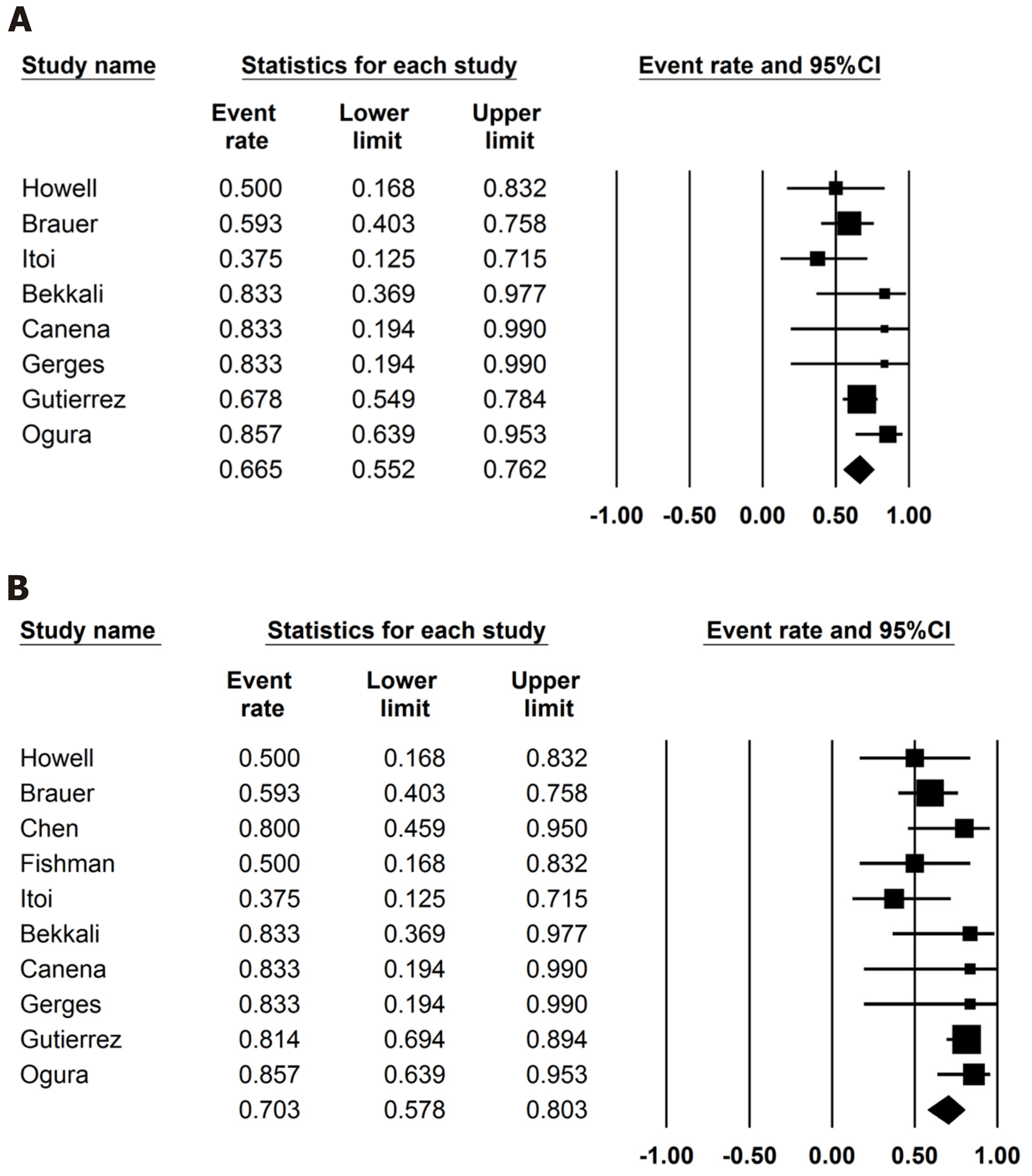
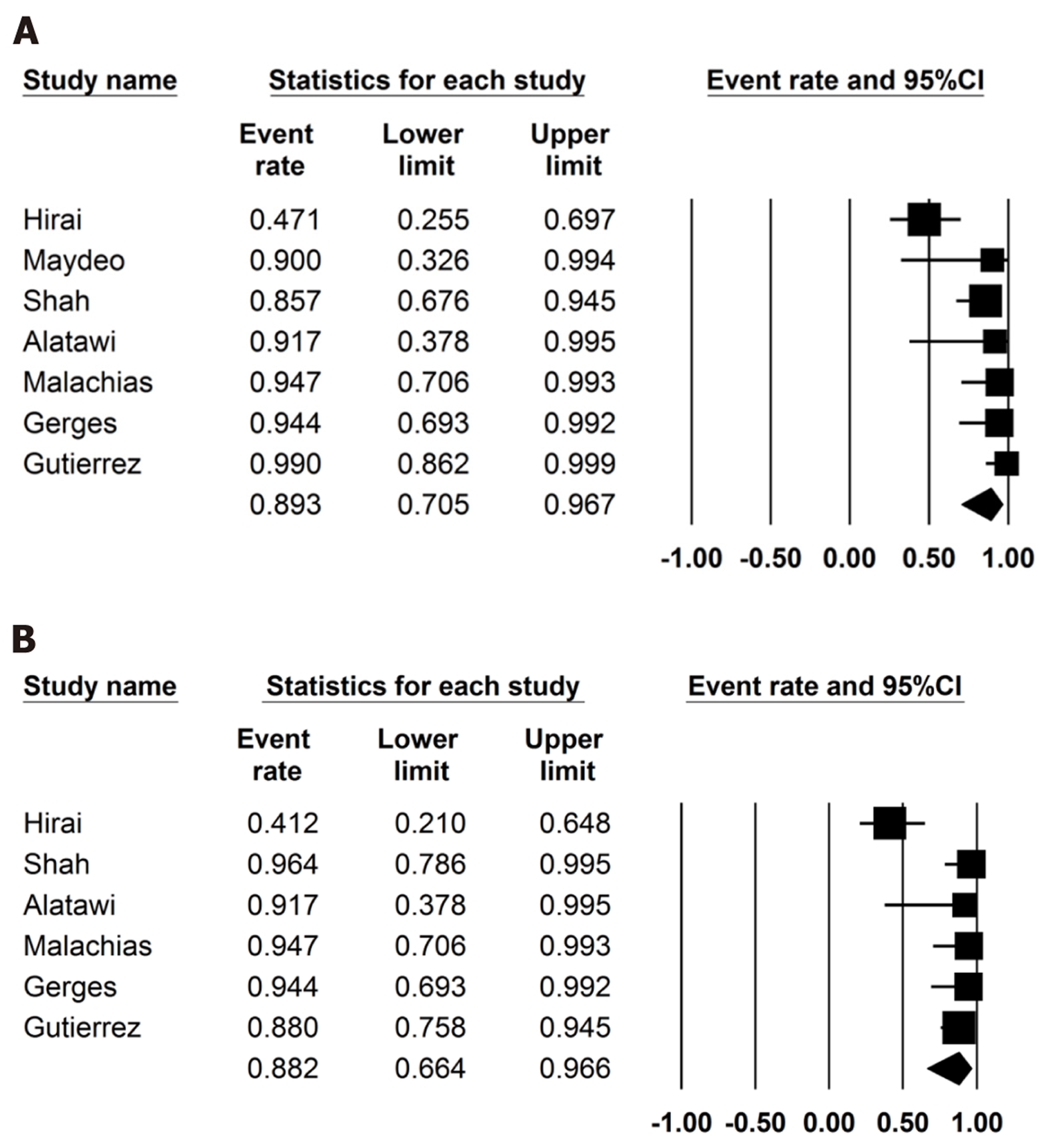
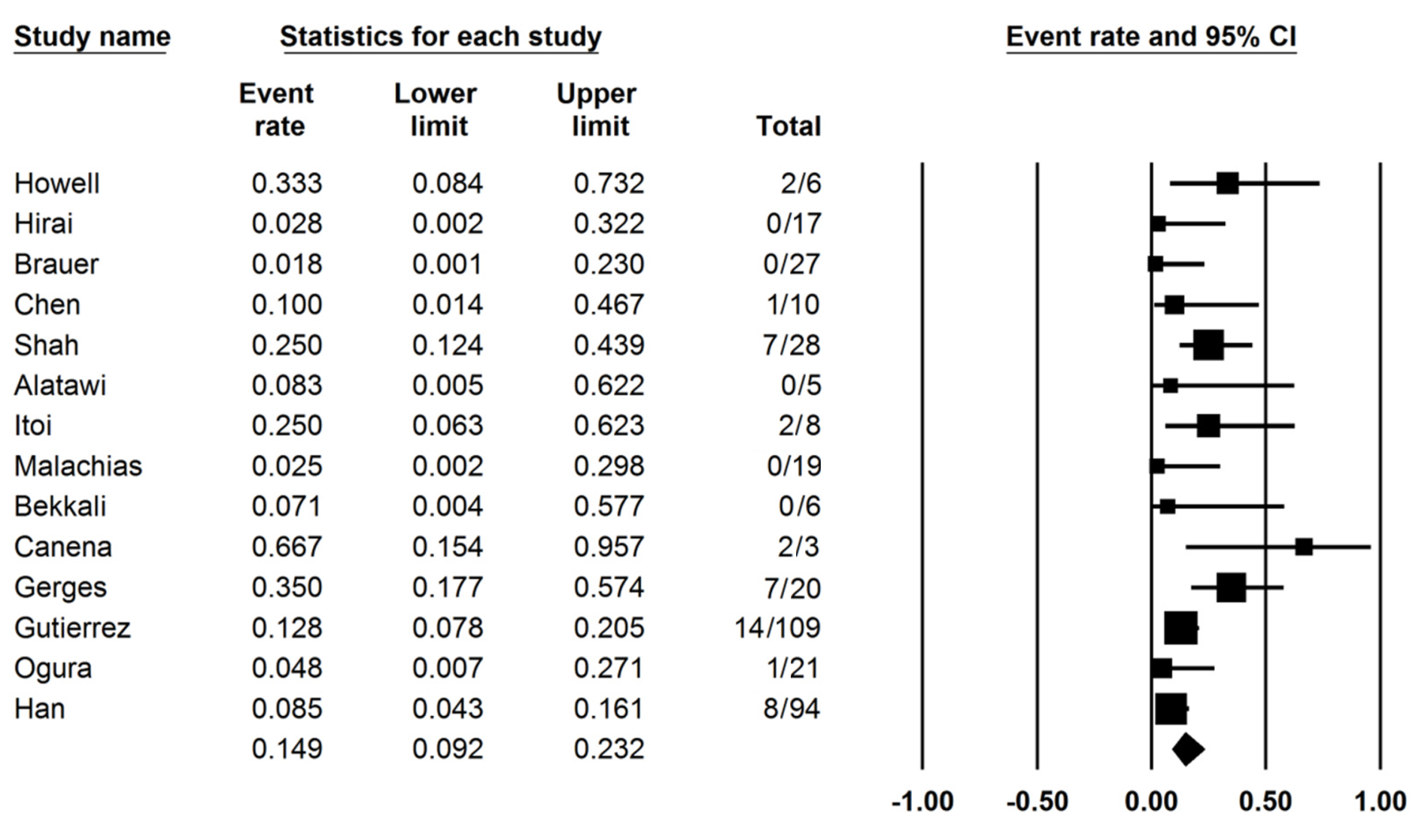
The pooled technical success rate of EHL was 70.3% (95%CI: 57.8-80.3; I2 = 36%) and the pooled technical success rate for LL was 89.3% (95%CI: 70.5-96.7; I2 = 70%). The pooled clinical success rate of EHL was 66.5% (95%CI: 55.2-76.2; I2 = 19%) and of LL was 88.2% (95%CI: 66.4-96.6; I2 = 77%). The pooled rates of technical success, clinical success, AE of POP, EHL and LL are presented in Table 2. The pooled POP AE rate was 14.9% (95%CI: 9.2-23.2; I2 = 49%), the pooled POP EHL AE rate was 11.2% (95%CI: 5.9-20.3; I2 = 15%) and the pooled POP LL AE rate was 13.1% (95%CI: 6.3-25.4; I2 = 31%). The subgroup analysis for POP AE were as follows: post-ERCP pancreatitis (PEP), 7% (95%CI: 3.5-13.6; I2 = 38%); fever, 3.7% (95%CI: 2-6.9; I2 = 0); abdominal pain, 4.7% (95%CI: 2.7-7.8; I2 = 0); perforation, 4.3% (95%CI: 2.1-8.4; I2 = 0); hemorrhage, 3.4% (95%CI: 1.7-6.6; I2 = 0) and no mortality. The AE in all procedures is shown in Table 3. Figure 3-5 show technical and clinical success of EHL, technical and clinical success of LL, and total adverse events, respectively.
| POP (%) | EHL (%) | LL (%) | |
| Technical success | 76.4 (95%CI: 65.9-84.5; I2 = 64%) | 70.3 (95%CI: 57.8-80.3; I2 = 36%) | 89.3 (95%CI: 70.5-96.7; I2 = 70%) |
| Clinical success | 76.8 (95%CI: 65.2-85.4; I2 = 66%) | 66.5 (95%CI: 55.2-76.2; I2 = 19%) | 88.2 (95%CI: 66.4-96.6; I2 = 77%) |
| All adverse events | 14.9 (95%CI: 9.2-23.2; I2 = 49%) | 11.2 (95%CI: 5.9-20.3; I2 = 15%) | 13.1 (95%CI: 6.3-25.4; I2 = 31%) |
| PEP | 7.0 (95%CI: 3.5-13.6; I2 = 38%) | -- | -- |
| Fever | 3.7 (95%CI: 2-6.9; I2 = 0) | -- | -- |
| Abdominal pain | 4.7 (95%CI: 2.7-7.8; I2 = 0) | -- | -- |
| Perforation | 4.3 (95%CI: 2.1-8.4; I2 = 0) | -- | -- |
| Hemorrhage | 3.4 (95%CI: 1.7-6.6; I2 = 0) | -- | -- |
| Ref. | Total | PEP | Perforation | Bleeding | Fever | Abd pain | EHL | LL |
| Howell et al[29] | 2 | 0 | 1 | 0 | 0 | 1 | 2 | 0 |
| Hirai et al[28] | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Brauer et al[30] | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Chen et al[8] | 1 | -- | -- | -- | -- | -- | 1 | -- |
| Fishman et al[9] | -- | -- | -- | -- | -- | -- | -- | -- |
| Maydeo et al[27] | -- | -- | -- | -- | -- | -- | -- | -- |
| Shah et al[26] | 7 | -- | -- | -- | -- | -- | 0 | 7 |
| Alatawi et al[31] | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Ito et al[23] | 2 | 1 | 1 | 0 | 0 | 0 | 2 | 0 |
| Malachias et al[24] | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Bekkali et al[7] | 0 | 0 | 0 | 0 | 0 | 0 | 0 | -- |
| Canena et al[20] | 2 | 1 | 0 | 0 | 1 | 0 | -- | -- |
| Gerges et al[21] | 7 | 5 | 1 | 1 | 0 | 0 | -- | -- |
| Brewer Gutierrez et al[2] | 14 | 5 | 1 | 2 | 3 | 3 | 5 | 6 |
| Ogura et al[25] | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 0 |
| Han et al[22] | 8 | 1 | 0 | 0 | 1 | 5 | 7 | 1 |
Sensitivity analysis: We excluded one study at a time and explored its effect on the main summary evaluation to determine if any one study had a dominant effect on the meta-analysis. We concluded that there was no significant effect on the outcome or heterogeneity.
The subgroup analysis of technical and clinical success by geographical location (United States, Japan and Europe), publication type (manuscript/abstract), study center (single/multicenter), and study type (retrospective/prospective) did not reveal major differences.
Heterogeneity: Based on prediction interval and I2 analysis for heterogeneity, we assessed dispersion of the calculated rates. With I2 we can determine what proportion in terms of dispersion is true vs chance[32]. The technical success of POP, clinical success of POP and technical success of LL showed substantial heterogeneity. The technical success in EHL, POP AE, POP LL AE, and PEP showed moderate heterogeneity. Clinical success in EHL, POP EHL AE and remaining subgroup analysis of AE had low heterogeneity. Clinical success for LL had significant heterogeneity.
Based on the results of the funnel plot and Eggers regression test, there was publication bias. Further assessment using the fail-safe N test and the Duval and Tweedie’s “Trim and Fill” test did not affect the final pooled outcomes. Figure 6 shows the funnel plot.
Our study demonstrates that the technical success rate of POP was 76.4% and the clinical success rate was 76.8%. Eight out of 16 studies performed ESWL[2,21-23,26,29,30] and all studies attempted standard ERCP prior to POP. This highlights that POP-guided lithotripsy can be utilized when patients fail in the first-line therapy.
The overall technical success ranged from 37.5%-95% and this variability could be secondary to the type of POP procedure used and the experience of the individual operator. On indirect comparative analysis between EHL and LL, we found that LL had higher overall rates of technical and clinical success. This may be secondary to the ability of LL to fragment denser stones (i.e., Hounsfield index > 2000 HU) as compared to EHL[2]. Although EHL is more widely available as compared to LL, LL tends to be much more expensive and requires special precautions compared with EHL. On subgroup analysis, studies with more than 20 patients showed higher technical success as compared to studies with less than 20 patients. This indicates that operator expertise may have influence on technical success.
Multiple stones, strictures, impacted stones, difficulty in cannulating PD due to angulation, poor visibility, equipment failure, or stones greater than 17 mm are other factors that may lead to lower technical success of POP[2,7,9,22-24,28-30]. Gutierrez et al[2] reported that presence of 3 or more stones was an independent risk factor for technical failure of POP (P < 0.04). Conversely, Han et al[22] reported that increased stone burden lead to higher technical success as these patients had higher chances of having smaller stones as compared to larger stones, which led to easier clearance.
Only Gerges et al[21] reported data regarding quality of life via questionnaires for pre- and post-procedure pain improvement based on a numeric rating scale decreased from mean of 5.4 ± 1.6 to 2.8 ± 1.8 (P < 0.01). Improvement in quality of life was reported by 89% of the patients in this study, which is comparable to ESWL[21,33].
The overall pooled AE rate of POP was comparable to ESWL ranging from 7% to 15%[34-37]. On subgroup analysis, the pooled AE rate of EHL and LL was similar at 11.2% and 13.1%, respectively. PEP was the most common AE and was comparable to ESWL at 7%[4,33,35].
Several limitations exist in our meta-analysis. Most of our studies were performed in tertiary care referral centers, so they may not be reflective of outcomes seen with less experienced operators. Also, POP does not reflect the skill of an average endoscopist. Our analysis contains studies that are retrospective in nature, which contribute to selection bias. No studies included data to compare POP as a first-line therapy with POP as a second-line therapy. Less than 5% of patients underwent POP as a first-line procedure and the individual outcomes were not mentioned in these studies. Nevertheless, this study contains the best available literature thus far with respect to POP. More studies are warranted to evaluate the technical and clinical success of EHL and LL. Clinical success is best defined universally with questionnaires, scores or scales to assess improvement of pain and quality of life, but not all studies provided this data.
In summary, POP-guided lithotripsy is a viable option for management of patients with chronic pancreatitis and symptomatic PD stones. We found LL technique to have a higher technical and clinical success rate with comparable AE rates. Optimal techniques for POP should be selected based on the clinical situation, device availability, and local center expertise. Further randomized controlled trials are needed for head to head comparison of the two techniques and evaluate if POP can be a potential first-line therapy in these cases.
Painful chronic calcifying pancreatitis management involves pancreatic enzyme replacement therapy, extracorporeal shock wave lithotripsy (ESWL) with or without endoscopic retrograde cholangiopancreatography (ERCP), ERCP with pancreatic sphincterotomy and either balloon or basket retrieval with stent placement, peroral pancreatoscopy (POP) and/or surgery. POP utilizes two different methods for pancreatic stone lithotripsy, which are electrohydraulic lithotripsy (EHL) or laser lithotripsy (LL).
There are limited data regarding the safety and efficacy of POP for symptomatic pancreatic calculi.
We aimed to assess the safety and efficacy of both POP techniques in regard to stone fragmentation. Primary outcomes assessed involved technical and clinical success of POP. Secondary outcomes included technical and clinical success for EHL and LL, and adverse events (AE) for POP, EHL and LL.
We conducted a comprehensive search of multiple electronic databases and conference proceedings including PubMed, EMBASE, Cochrane, Google Scholar and Web of Science databases. Statistical analysis was conducted via comprehensive meta-analysis software.
POP-guided lithotripsy was successful in patients who had failed in the first-line therapy. On indirect comparative analysis, LL was found to have higher technical and clinical success than EHL. POP AE was comparable to ESWL. The AE for EHL and LL was similar on indirect comparison. PEP was the most common AE and was comparable to ESWL.
POP-guided lithotripsy is a viable option for management of patients with chronic pancreatitis and symptomatic PD stones. We found LL technique to have a higher technical and clinical success rate with comparable AE rates.
Further randomized controlled trials are needed for head to head comparison of the two techniques and evaluate if POP can be a potential first line therapy in these cases.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Tierney J S-Editor: Ma YJ L-Editor: MedE-Ma P-Editor: Zhang YL
| 1. | Gerges C, Pullmann D, Schneider M, Siersema P, van Geenen E, Neuhaus H, Beyna T. Pancreatoscopy in endoscopic treatment of pancreatic duct stones: a systematic review. Minerva Chir. 2019;74:334-347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 2. | Brewer Gutierrez OI, Raijman I, Shah RJ, Elmunzer BJ, Webster GJM, Pleskow D, Sherman S, Sturgess RP, Sejpal DV, Ko C, Maurano A, Adler DG, Mullady DK, Strand DS, DiMaio CJ, Piraka C, Sharahia R, Dbouk MH, Han S, Spiceland CM, Bekkali NLH, Gabr M, Bick B, Dwyer LK, Han D, Buxbaum J, Zulli C, Cosgrove N, Wang AY, Carr-Locke D, Kerdsirichairat T, Aridi HD, Moran R, Shah S, Yang J, Sanaei O, Parsa N, Kumbhari V, Singh VK, Khashab MA. Safety and efficacy of digital single-operator pancreatoscopy for obstructing pancreatic ductal stones. Endosc Int Open. 2019;7:E896-E903. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 37] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 3. | Dominguez-Munoz JE, Drewes AM, Lindkvist B, Ewald N, Czakó L, Rosendahl J, Löhr JM; HaPanEU/UEG Working Group. Recommendations from the United European Gastroenterology evidence-based guidelines for the diagnosis and therapy of chronic pancreatitis. Pancreatology. 2018;18:847-854. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 109] [Article Influence: 15.6] [Reference Citation Analysis (0)] |
| 4. | Dumonceau JM, Delhaye M, Tringali A, Arvanitakis M, Sanchez-Yague A, Vaysse T, Aithal GP, Anderloni A, Bruno M, Cantú P, Devière J, Domínguez-Muñoz JE, Lekkerkerker S, Poley JW, Ramchandani M, Reddy N, van Hooft JE. Endoscopic treatment of chronic pancreatitis: European Society of Gastrointestinal Endoscopy (ESGE) Guideline - Updated August 2018. Endoscopy. 2019;51:179-193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 168] [Cited by in RCA: 246] [Article Influence: 41.0] [Reference Citation Analysis (0)] |
| 5. | Gardner TB, Adler DG, Forsmark CE, Sauer BG, Taylor JR, Whitcomb DC. ACG Clinical Guideline: Chronic Pancreatitis. Am J Gastroenterol. 2020;115:322-339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 202] [Article Influence: 40.4] [Reference Citation Analysis (0)] |
| 6. | Attwell AR, Brauer BC, Chen YK, Yen RD, Fukami N, Shah RJ. Endoscopic retrograde cholangiopancreatography with per oral pancreatoscopy for calcific chronic pancreatitis using endoscope and catheter-based pancreatoscopes: a 10-year single-center experience. Pancreas. 2014;43:268-274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 42] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 7. | Bekkali NL, Murray S, Johnson GJ, Bandula S, Amin Z, Chapman MH, Pereira SP, Webster GJ. Pancreatoscopy-Directed Electrohydraulic Lithotripsy for Pancreatic Ductal Stones in Painful Chronic Pancreatitis Using SpyGlass. Pancreas. 2017;46:528-530. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 36] [Article Influence: 4.5] [Reference Citation Analysis (1)] |
| 8. | Chen YK, Tarnasky PR, Raijman I, Pleskow D, Shah RJ, Fortajada EL. Peroral Pancreatoscopy (PP) for Pancreatic Stone Therapy and Investigation of Susptected Pancreatic Lesions-First Human Experience Using the Spyglass Direct Visualization System (SDVS). Gastrointest Endosc. 2008;AB108. [DOI] [Full Text] |
| 9. | Fishman DS, Tarnasky PR, Patel SN, Raijman I. Management of pancreaticobiliary disease using a new intra-ductal endoscope: the Texas experience. World J Gastroenterol. 2009;15:1353-1358. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 70] [Cited by in RCA: 63] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 10. | Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151:264-269, W64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21613] [Cited by in RCA: 18149] [Article Influence: 1134.3] [Reference Citation Analysis (0)] |
| 11. | Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603-605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8858] [Cited by in RCA: 12599] [Article Influence: 839.9] [Reference Citation Analysis (0)] |
| 12. | DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26739] [Cited by in RCA: 30375] [Article Influence: 778.8] [Reference Citation Analysis (0)] |
| 13. | Sutton AJ, Abrams KR, Jones DR, Jones DR, Sheldon TA, Song F. Methods for meta-analysis in medical research. Chichester: Wiley, 2000. |
| 14. | Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557-560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39087] [Cited by in RCA: 46396] [Article Influence: 2108.9] [Reference Citation Analysis (3)] |
| 15. | Kanwal F, White D. "Systematic Reviews and Meta-analyses" in Clinical Gastroenterology and Hepatology. Clin Gastroenterol Hepatol. 2012;10:1184-1186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 94] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 16. | Guyatt GH, Oxman AD, Kunz R, Woodcock J, Brozek J, Helfand M, Alonso-Coello P, Glasziou P, Jaeschke R, Akl EA, Norris S, Vist G, Dahm P, Shukla VK, Higgins J, Falck-Ytter Y, Schünemann HJ; GRADE Working Group. GRADE guidelines: 7. Rating the quality of evidence--inconsistency. J Clin Epidemiol. 2011;64:1294-1302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1294] [Cited by in RCA: 1713] [Article Influence: 122.4] [Reference Citation Analysis (0)] |
| 17. | Easterbrook PJ, Berlin JA, Gopalan R, Matthews DR. Publication bias in clinical research. Lancet. 1991;337:867-872. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2020] [Cited by in RCA: 2003] [Article Influence: 58.9] [Reference Citation Analysis (0)] |
| 18. | Duval S, Tweedie R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56:455-463. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7948] [Cited by in RCA: 9059] [Article Influence: 362.4] [Reference Citation Analysis (0)] |
| 19. | Rothstein HR, Sutton AJ, Borenstein M. Publication bias in meta-analysis: prevention, assessment and adjustments. Chichester: Wiley, 2005: 1-7. |
| 20. | Canena J, Lopes L, Fernandes J, Alexandrino G, Lourenço L, Libânio D, Horta D, Giestas S, Reis J. Outcomes of Single-Operator Cholangioscopy-Guided Lithotripsy in Patients with Difficult Biliary and Pancreatic Stones. GE Port J Gastroenterol. 2019;26:105-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 21. | Gerges C, Pullmann D, Bahin F, Schneider M, Siersema PD, Neuhaus H, van Geenen EM, Beyna T. SpyGlass DS-guided lithotripsy for pancreatic duct stones in symptomatic treatment-refractory chronic calcifying pancreatitis. Endosc Int Open. 2019;7:E99-E103. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 22. | Han S, Shah RJ, Brauer BC, Edmundowicz SA, Hammad HT, Wagh MS, Wani S, Attwell AR. A Comparison of Endoscopic Retrograde Pancreatography With or Without Pancreatoscopy for Removal of Pancreatic Duct Stones. Pancreas. 2019;48:690-697. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 23. | Ito K, Igarashi Y, Okano N, Mimura T, Kishimoto Y, Hara S, Takuma K. Efficacy of combined endoscopic lithotomy and extracorporeal shock wave lithotripsy, and additional electrohydraulic lithotripsy using the SpyGlass direct visualization system or X-ray guided EHL as needed, for pancreatic lithiasis. Biomed Res Int. 2014;2014:732781. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 24. | Malachias A, Kypraios D, Theodoropoulos L, Hatzinicolaou S-L, Stavrinides S, Saribegioglou N, Dimitroulopoulos D, Tsamakidis K, Korkolis D, Xinopoulos D. Sa1498 Pancreatoscopy-Guided Laser Lithotripsy for Difficult Pancreatic Duct Stones. A Single Center Experience. Gastrointest Endosc 2016; 83: AB274. [DOI] [Full Text] |
| 25. | Ogura T, Okuda A, Imanishi M, Miyano A, Amano M, Nishioka N, Kamiyama R, Higuchi K. Electrohydraulic Lithotripsy for Pancreatic Duct Stones Under Digital Single-Operator Pancreatoscopy (with Video). Dig Dis Sci. 2019;64:1377-1382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 26. | Shah RJ, Attwell AR, Raijman I, Kahaleh M, Patel S. 577 Per Oral Pancreatoscopy With Intraductal Holmium Laser Lithotripsy for Treatment of Main Pancreatic Duct Calculi: A Multi-Center US Experience. Gastrointest Endosc 2012; 75: AB154. [DOI] [Full Text] |
| 27. | Maydeo A, Kwek BE, Bhandari S, Bapat M, Dhir V. Single-operator cholangioscopy-guided laser lithotripsy in patients with difficult biliary and pancreatic ductal stones (with videos). Gastrointest Endosc. 2011;74:1308-1314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 93] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 28. | Hirai T, Goto H, Hirooka Y, Itoh A, Hashimoto S, Niwa Y, Hayakawa T. Pilot study of pancreatoscopic lithotripsy using a 5-fr instrument: selected patients may benefit. Endoscopy. 2004;36:212-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 29. | Howell DA, Dy RM, Hanson BL, Nezhad SF, Broaddus SB. Endoscopic treatment of pancreatic duct stones using a 10F pancreatoscope and electrohydraulic lithotripsy. Gastrointest Endosc. 1999;50:829-833. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 62] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 30. | Brauer BC, Jing T, Chen YK, Shah RJ. ERCP with pancreatoscopy and electrohydraulic lithotripsy (EHL) for calcific pancreatitis. Gastrointest Endosc. 2007;AB241. [DOI] [Full Text] |
| 31. | Alatawi A, Leblanc S, Vienne A, Pratico CA, Gaudric M, Duchmann JC, Boyer J, Mangialavori L, Chaussade S, Prat F. Pancreatoscopy-guided intracorporeal laser lithotripsy for difficult pancreatic duct stones: a case series with prospective follow-up (with video). Gastrointest Endosc. 2013;78:179-183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 32. | Mohan BP, Adler DG. Heterogeneity in systematic review and meta-analysis: how to read between the numbers. Gastrointest Endosc. 2019;89:902-903. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 102] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 33. | Moole H, Jaeger A, Bechtold ML, Forcione D, Taneja D, Puli SR. Success of Extracorporeal Shock Wave Lithotripsy in Chronic Calcific Pancreatitis Management: A Meta-Analysis and Systematic Review. Pancreas. 2016;45:651-658. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 47] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 34. | Inui K, Tazuma S, Yamaguchi T, Ohara H, Tsuji T, Miyagawa H, Igarashi Y, Nakamura Y, Atomi Y. Treatment of pancreatic stones with extracorporeal shock wave lithotripsy: results of a multicenter survey. Pancreas. 2005;30:26-30. [PubMed] |
| 35. | Li BR, Liao Z, Du TT, Ye B, Zou WB, Chen H, Ji JT, Zheng ZH, Hao JF, Jiang YY, Hu LH, Li ZS. Risk factors for complications of pancreatic extracorporeal shock wave lithotripsy. Endoscopy. 2014;46:1092-1100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 75] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 36. | Haraldsson S, Roug S, Nøjgaard C, Novovic S, Gluud LL, Feldager E, Schmidt PN. Extracorporeal shock wave lithotripsy for pancreatic duct stones: an observational study. Scand J Gastroenterol. 2018;53:1399-1403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 37. | Li BR, Liao Z, Du TT, Ye B, Chen H, Ji JT, Zheng ZH, Hao JF, Ning SB, Wang D, Lin JH, Hu LH, Li ZS. Extracorporeal shock wave lithotripsy is a safe and effective treatment for pancreatic stones coexisting with pancreatic pseudocysts. Gastrointest Endosc. 2016;84:69-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 43] [Article Influence: 4.8] [Reference Citation Analysis (0)] |