Published online Nov 21, 2019. doi: 10.3748/wjg.v25.i43.6430
Peer-review started: July 31, 2019
First decision: August 27, 2019
Revised: September 25, 2019
Accepted: November 7, 2019
Article in press: November 7, 2019
Published online: November 21, 2019
Processing time: 112 Days and 9.9 Hours
Segmental intrahepatic cholestasis caused by transjugular intrahepatic portosystemic shunt (TIPS) (SIC-T), is a rare complication of this technique and only referred by case reports. Thus, we conducted a systematic, retrospective analysis to provide evidence regarding prevalence and consequences of this TIPS-induced bile duct compression.
To assess prevalence and outcome of SIC-T in a large TIPS-cohort.
In this retrospective cohort study, we screened the institutional databases for all consecutive patients that were treated by TIPS-placement or TIPS-revision between January 2005 and August 2013. We analyzed radiologic images for signs of biliary congestion. Cases that were indicative of SIC-T were reviewed by two independent radiologists and additional patient data was collected. Descriptive statistics of patient demographics, indications for TIPS and procedural details were registered. Logistic regression analysis was performed to identify predictors for the development of SIC-T.
We analyzed 135 cirrhotic patients who underwent TIPS (mean age 55 years, 79% male gender). Etiology of cirrhosis was alcohol in most cases and indications for TIPS were mainly refractory ascites and recurrent variceal bleeding. TIPS revision was necessary in 31 patients. We identified 4 cases (2.9%) of SIC-T in direct proximity of the TIPS-stent. Diagnosis was confirmed by CT-scan, MRI or endoscopic retrograde cholangio pancreaticography (ERCP). In two patients TIPS was implanted via the right and in one through the medial hepatic vein. One patient received TIPS-prolongation by multiple revisions. Most patients were asymptomatic but one cholangitic abscess necessitated a transhepatic drain. Logistic regression analysis identified TIPS-placement other than from medial hepatic vein to right portal vein as risk factor (OR 21.0) for SIC-T.
SIC-T ads to (mostly late) complications in the interventional treatment of cirrhotic portal hypertensions and can lead to cholangitic abscesses. Patients, particularly with multiple interventions, should be screened for SIC-T.
Core tip: Segmental intrahepatic cholestasis (SIC-T) is a rare and mostly late complication of transjugular intrahepatic portosystemic shunt (TIPS). Detection of SIC-T is performed by a combination of clinical, radiological and laboratory analyses. In the majority of patients, SIC-T requires no intervention but can lead to cholangitic abscesses. SIC-T contributes to late complications of TIPS-procedure. TIPS placement other than from the medial hepatic vein is an important risk factor for SIC-T development. Patients with atypical TIPS placements should be screened for SIC-T.
- Citation: Bucher JN, Hollenbach M, Strocka S, Gaebelein G, Moche M, Kaiser T, Bartels M, Hoffmeister A. Segmental intrahepatic cholestasis as a technical complication of the transjugular intrahepatic porto-systemic shunt. World J Gastroenterol 2019; 25(43): 6430-6439
- URL: https://www.wjgnet.com/1007-9327/full/v25/i43/6430.htm
- DOI: https://dx.doi.org/10.3748/wjg.v25.i43.6430
Portal hypertension is a consequence of chronic liver disease and the main cause of morbidity and mortality in patients with cirrhosis[1]. Although conservative therapy is an effective method to reduce portal hypertension[2], the implantation of a transjugular intrahepatic portosystemic shunt (TIPS) is the treatment of choice in refractory ascites (RA) and recurrent or refractory variceal bleeding (RVB)[3]. Moreover, recent data indicate that the use of a pre-emptive TIPS in variceal bleeding should be performed in all patients with end-stage liver disease[4,5].
Despite its convincing efficacy in reducing portal hypertension, a procedure related rate of major complications varies between less than 5%[6] and up to 10%[7]. Aside from life threatening acute complications that occur in less than 2%, post-interventional hepatic encephalopathy (up to 53.9%)[8] and shunt-dysfunction (15-43.9%)[9] are more frequent after TIPS. Rare chronic complications are isolated hyperbilirubinemia[10], stent migration[11], biliary fistula[12], migration[13] and liver infarction[14]. However, the use of covered and small diameter TIPS was associated with significantly less rates of complication but comparable efficacy and is now the standard of therapy[15-17].
Another rare complications of TIPS is a segmental intrahepatic cholestasis induced by TIPS-related compression of bile ducts (SIC-T)[18]. In order to identify prevalence and consequences of SIC-T in a large cohort, we evaluated all consecutive patients who underwent TIPS implantation or TIPS-revision at our institution since 2005. Moreover, we aimed to analyze risk factors for the development of SIC-T in regression analysis and described the management of SIC-T.
The study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki and was approved by the ethical review board of the Medical Faculty of the University of Leipzig (230/19-ek, June 16th 2019). In 2013 we reported a case of a segmental intrahepatic cholestasis caused by intrahepatic bile duct compression as a consequence of the TIPS-stent[18]. Thus, all patients with TIPS were identified by screening our institutional databases. Then, all consecutive patients who were treated by TIPS-placement or revision with prolongation of formerly placed TIPS stents between January 2005 and August 2013 were included to this study. We identified 135 Patients (107 males, 28 female) that met the selection criteria. Medical records were evaluated for patient demographics including age, gender as well as etiology of cirrhosis and indication for TIPS. All patients received TIPS-implantations as recommended by current guidelines[2] and Polytetrafluorethylene-(PTFE)-covered TIPS [VIATORR® TIPS-Stents (W.L. Gore, United States)] were used in all cases. Databases were also analyzed for the used techniques (puncture from the medial, right or left hepatic vein to the right or left portal vein). Here, the implantation of TIPS from the right hepatic vein to the right portal vein was considered as typical TIPS placement as described before. Also, the route from the medial hepatic vein to the right portal vein demonstrates an equivalent alternative[19-21]. Revisions and indication for revision of TIPS were assessed and follow-up time with patient’s status at the end of follow-up was evaluated.
All patients had at least one radiological imaging (ultrasound, contrast-enhanced CT or MRI) of the liver at our institution after TIPS-placement/-prolongation. The radiological imaging was reviewed by one radiologist who screened patients with TIPS for biliary congestion. Imaging, that showed signs of biliary congestion, was reviewed by a second radiologist and the diagnosis of SIC-T was either excluded or confirmed. For the patients with SIC-T we reviewed the medical history and the laboratory parameters that were indicative of biliary congestion in between the date of SIC-T diagnosis and the last imaging without signs of SIC-T. MRI was performed with 1.5 Tesla Siemens Symphony (Siemens Healthcare, Germany). For intravenous contrast, we used Gadoxetic acid (Bayer Healthcare Pharmaceuticals, Germany).
Statistical analysis was performed with SPSS 20 (IBM, Armonk, NY, United States). Data is presented with median as well as mean with lower and upper range or presented as “n” with a percentage (%) to each corresponding group. Logistic regression analysis was used to evaluate possible predictor for SIC-T. A P value ≤ 0.05 was considered statistically significant with except in regression analysis (P value less than 0.01 due to multiple testing). All statistical analyses were reviewed by an institutional biomedical statistician.
Patients’ characteristics are presented in Table 1. Patients underwent 121 primary TIPS-placements and 30 TIPS-revisions (22.2%), of which in two patients multiple revisions per patient were performed (n = 4 and n = 2). Mean age was 54 years (19-84). The most frequent liver disease was alcoholic cirrhosis (84.3%) and the most frequent indications for TIPS-placement were RA (61.5%) and RVB (28.4%). In the majority of cases, the TIPS was placed from the medial hepatic vein to the right portal branch (79.3%). In 11.1% of the cases the TIPS was placed from the right hepatic vein to the right portal branch (together 90.4% typical TIPS placement) and in 2.2% an unconventional approach was performed for anatomical reasons. In 10 patients the anatomical route for TIPS-placement was not known because TIPS-placement was performed at another institution and follow-up was conducted by ultrasound. Indications for TIPS-revisions were hepatic encephalopathy because of high shunt-flow in 8 cases (26.7%) and RA because of low shunt flow or thrombosis in 8 and 14 cases (26.7% and 46.7% respectively). At the time of screening, the median retrospective follow-up after TIPS-placement per patient was 7 mo (mean/min/max = 19/0/148). Retrospective follow-up ended because of loss to clinical follow-up due to absence from our outpatient clinic or stop of retrospective follow up at the time of screening in 99 cases (73.3%), because of death with TIPS in 20 cases (14.8%) or because of consecutive liver transplantation in 17 cases (12.6%) (see Table 1). In 6 patients (4.4%) intrahepatic cholestasis was suspected in the initial screening because of tubular structures with fluid equivalent radiodensity converging in proximity to the TIPS stent. Two of these cases were identified as a hepatic vein obstruction by the reviewing radiologist while four cases of SIC-T (2.9%) were confirmed. Logistic regression analysis showed that TIPS-placement other than from the medial hepatic vein to the right portal branch was significantly associated with the occurrence of SIC-T (odds ratio 21.0, 95%CI: 0.7-5.4, P = 0.01). In contrast, age, male gender, RVB as TIPS indication or etiology of cirrhosis other than alcohol could not be identified as predictors for SIC-T (Tables 1-3). In addition, multivariate logistic regression failed to identify prediction parameters for SICT-T (data not shown).
| Characteristic | Value |
| Age1 | 55 (19, 54, 84) |
| Female | 28 (20.7) |
| Male | 107 (79.3) |
| Etiology of cirrhosis | |
| Alcoholic | 114 (84.4) |
| NASH | 7 (5.2) |
| BCS | 4 (3.0) |
| Kryptogenic | 3 (2.2) |
| HCV | 2 (1.5) |
| PBC | 1 (0.7) |
| Autoimmune | 1 (0.7) |
| Hemochromatosis | 1 (0.7) |
| HBV | 1 (0.7) |
| Toxic | 1 (0.7) |
| Indications for TIPS | |
| RA | 83 (61.5) |
| RVB | 38 (28.4) |
| HRS | 10 (7.5) |
| BCS | 3 (2.2) |
| Others | 1 (0.7) |
| Technique | |
| MHV-RPV | 107 (79.3) |
| RHV-RPV | 15 (11.1) |
| LHV-LPV | 2 (1.5) |
| MHV-LPV | 1 (0.7) |
| Unknown | 10 (7.4) |
| Time with TIPS2 | 7 (0, 19, 148) |
| Revision | |
| No revision | 105 (77.8) |
| 1 revision | 28 (20.7) |
| More than 1 revision | 2 (1.5) |
| Indications for revision | |
| Encephalopathy | 8 (26.7) |
| Low shunt flow | 8 (26.7) |
| Thrombosis | 14 (46.7) |
| End of follow-up | |
| Loss to follow-up | 99 (73.3) |
| Death with TIPS | 20 (14.8) |
| Consecutive LTx | 17 (12.6) |
| Patient | Age1 | Sex | Aetiolog-y of cirrhosis | Indicati-on for TIPS | TIPS-type | TIPS Localisa-tion | Congest-ed segment-s | SIC-T free intervall with TIPS2 | Time from last imaging without SIC-T suspi-cion2 | MELD before SIC-T diagno-sis | MELD at SIC-T diagno-sis | Relevant complica-tions |
| 1 | 51 | M | Alcoholic | RA & HRS | PTFE-covered | RHV-RPV | VII | 72 | 39 | 11 | 12 | None |
| 2 | 55 | M | Alcoholic | RA | PTFE-covered | RHV-RPV | VII | 83 | 26 | 19 | 16 | None |
| 3 | 49 | F | alcoholic | RA & HRS | PTFE-covered | MHV-RPV | V | 17 | < 1 | 18 | 22 | SBP |
| 4 | 44 | M | BCS | RA | PTFE-covered | Atypical | I | 0,4 | < 1 | 10 | 9 | Hepatic abscess |
| Variable | OR | Univariate 95%CI | P value |
| Age | 0.96 | -0.1 - 0.1 | 0.40 |
| Male gender | 0.78 | -2.6 - 2.1 | 0.83 |
| Other than alcoholic cirrhosis | 0.54 | -2.9 - 1.7 | 0.60 |
| RVB as TIPS indication | < 0.01 | -5654.8 - 5620.0 | 0.99 |
| TIPS placement other than MHV-RPV | 21.0 | 0.7 - 5.4 | 0.01 |
Patient 1 is a 59 year-old male with an alcoholic Child B cirrhosis, who received a TIPS from the right hepatic vein to the right portal branch for RA and hepatorenal syndrome (HRS). Lab values were unremarkable. One month after the procedure the patient was free of ascites and the renal function had returned to the patient’s baseline. No episode of hepatic encephalopathy occurred. A contrast enhanced abdominal CT scan for routine follow-up 6 years after TIPS-Placement incidentally showed the congestion of the intrahepatic bile ducts in segment VII. An MRI with liver specific, intravenous contrast and MRCP-sequence was performed to rule out hilar neoplasia and to clearly confirm the compression of the segmental bile duct by the TIPS-stent. It also showed a late contrast washout, that was highly suspicious for a hepatocellular carcinoma (HCC) in segment VIII unrelated to the biliopathy. Observational approach of the SIC-T was performed due to absence of cholangitis. The HCC was confirmed and treated by trans-arterial chemoembolisation and no episode of cholangitis or an attributable worsening of the cholestasis has occurred. After 2 years, a contrast enhanced CT-scan showed no signs of SIC-T. Unfortunately the patient developed bone metastases and had to be taken off the transplant waiting list.
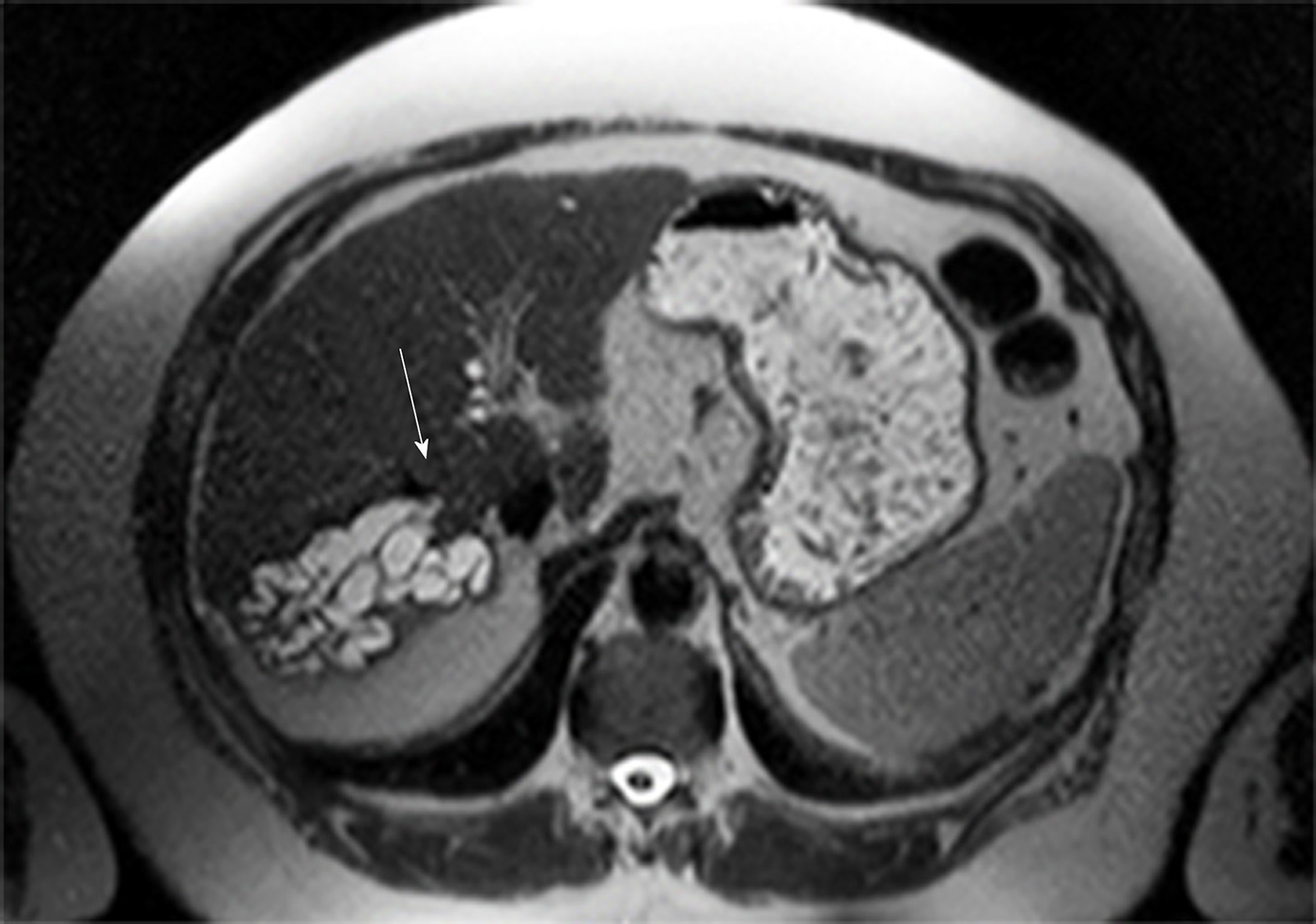
Patient 2 is a 63 year old male with alcoholic Child B cirrhosis, who received a TIPS from the right hepatic vein to the right portal vein for RA. Lab values were inconspicuous. Reduction of ascites was sufficient and no episode of hepatic encephalopathy was registered. Although initial follow-up ultrasound was inconspicuous, a new, hypoechoic structure of 50 mm × 75 mm appeared 5 years after TIPS-placement in the right liver lobe. A contrast enhanced CT-scan revealed a tubular, cystic congestion of the intrahepatic bile ducts selectively in liver segment VII. The liver parenchyma in this segment was completely extinct by congested ducts. Tumorous compression was ruled out by MRI with MRCP-sequence and the SIC-T was confirmed (see Figure 1). The patient negotiated complaints, thus an observational approach was conducted. In last follow-up, the patient was in a stable condition.
Patient 3 is a 50 year-old female with alcoholic Child C cirrhosis who received a TIPS from the medial hepatic vein to the right portal vein branch for RA and HRS. Initial ascites reduction and improvement of renal function were satisfying and hepatic encephalopathy was absent. One month after TIPS-placement, she was re-admitted with a relapse of ascites and spontaneous bacterial peritonitis (SBP). Relapse of alcoholic abuse was reported. The hydropic decompensation was caused by a low shunt flow due to a protrusion of the covered part of the portal TIPS-end that was diagnosed by TIPS-angiography. Multiple TIPS-revisions and a stent-in-TIPS procedure were performed to elongate the stent into the extrahepatic portal vein. A significant reduction of ascites and a sustained clinical stability was achieved. Follow-up ultrasound and CT-scan revealed a biliary congestion of the intrahepatic bile ducts in segment V converging and ending in direct proximity of the TIPS stent. By reason of elevated cholestasis parameters (sudden hyperbilirubinemia from 98 to 493 µmol/L), an endoscopic retrograde cholangio pancreaticography (ERCP) was attempted but endoscopic access to the compressed bile duct could not be achieved. Decompression and biliary drainage through percutaneous transhepatic biliary drainage was not performed because of ascites. Thus, conservative therapy with antibiotic prophylaxis was initiated because the initial clinical deterioration of patient 3 was rather attributable to the development of SBP and the relapsing alcohol abuse than to the SIC-T. The patient was discharged but unfortunately, the patient did not keep follow-up appointment due to continued alcohol abuse.
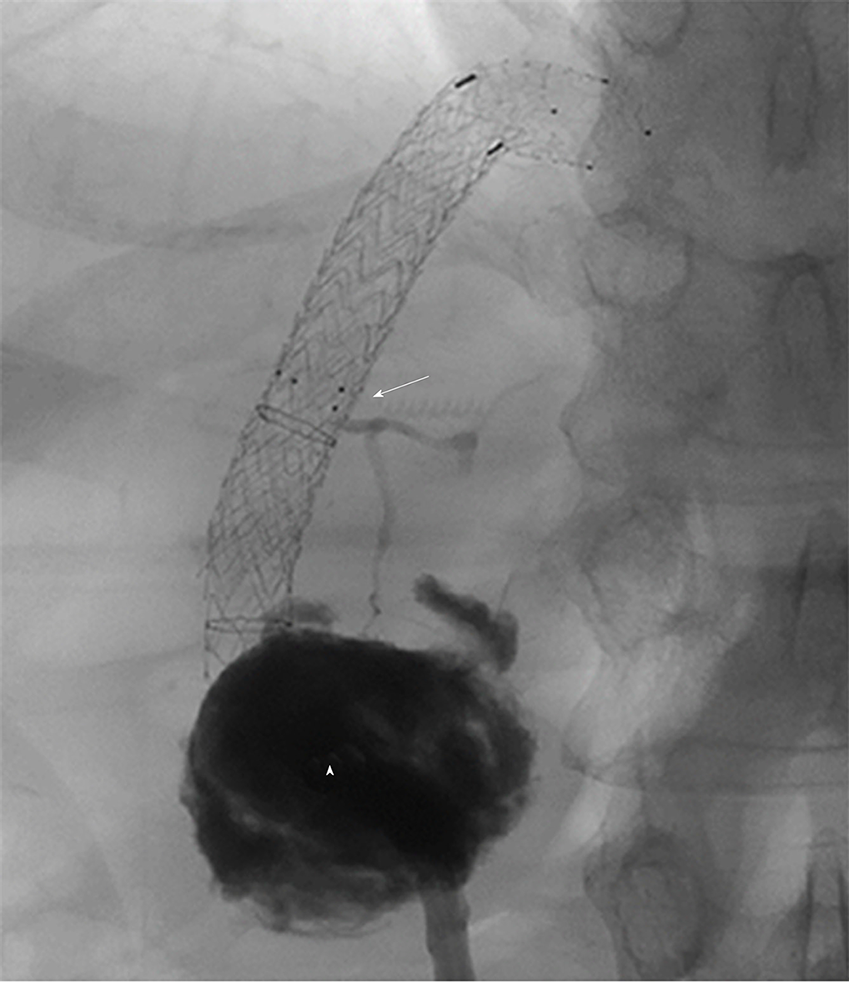
Patient 4 is a 44 year-old male with a Child B cirrhosis and Budd-Chiari syndrome. A first TIPS-attempt in another hospital for RA failed because of an atypical portal and hepatic venous anatomy. A single hepatic vein drained mainly the right liver lobe with multiple collaterals combined with an atypical portal-venous anatomy. A TIPS-placement was achieved through an atypical approach from the sole right hepatic vein into an atypically located portal branch. Ascites reduction was acceptable and the patient did not suffer from hepatic encephalopathy. Nevertheless, lab values showed increased inflammatory markers and a subtle but relevant peak in bilirubin (22.3 µmol/L), alkaline phosphatase (AP) and gamma-glutamyl transferase (gGT) (peak at 5.2 and 2.9 µkat/L). CT-scan indicated a segmental cholestasis and a cholangitic abscess in liver segment I that was treated with a percutaneous drain. Antibiotics were prescribed. An angiography of the drain showed a connection of the abscess with the segmental bile duct that appeared to be compressed by the TIPS-Stent (see Figure 2). A consecutively performed ERCP showed an abrupt ending of the segment I bile duct next to the TIPS-stent but internal stent-placement was not possible. Nevertheless, hilar neoplasia could be excluded. Lab values decreased at baseline levels after two weeks. Further follow-up was unremarkable.
Details of the patients with SIC-T can be found in Table 2. Additionally, all patients were instructed in detail about signs and symptoms of cholangitis and the necessity to urgently admit in our emergency room if these were present.
TIPS-placement is a well-established option to treat complications of portal hypertension secondary to cirrhosis[1]. Major complications related to the TIPS-procedure occur in 5 up to 10%[7] and minor complications in up to 53% of the cases. These can be stratified into acute complications through accidental damage of hepatic structures resulting in vascular occlusion, hemorrhage or bile-leak. Chronic complications result from the partial liver bypass or a progressive tissue proliferation that lead to stent occlusion[8,11,12]. In most cases chronic complications develop after an initial clinical improvement whereas acute challenges mostly present with immediate symptoms.
We described a segmental intrahepatic cholestasis as a new type of TIPS-related complication as case report before[18]. In our current study, we identified in our TIPS-cohort 4 cases of segmental intrahepatic cholestasis caused by the TIPS-stent (SIC-T), which can be assigned to the group of complications that result from damage of intrahepatic structures, yet in case of SIC-T without causing immediate symptoms in the majority of the patients. SIC-T can be defined as segmental cholestasis due to the mechanical obstruction of intrahepatic biliary branches by the stent graft after TIPS-procedure. This resulted in the significant congestion of the biliary system proximal to the obstructed intrahepatic bile duct in all identified cases.
In our retrospective analysis, SIC-T was detected with a relevant prevalence at our center (2.9%). Most cases could only be identified by a detailed review of the whole population that was treated with a TIPS or a TIPS-revision. Moreover, SIC-T was a late complication of TIPS (time from TIPS to SIC-T up to 83 mo). The reason for the delayed diagnosis could be explained on the one hand by the absence of distinct symptoms or conspicuous lab values in the majority of the cases (3 out of 4 cases; 75%) and on the other hand in the long period from TIPS-placement to development of SIC-T. Even in patients with regularly follow-up imaging, the interval from last inconspicuous imaging to diagnosis of SIC-T was up to 39 mo. However, one patient developed a cholangitic abscess immediate after onset of a symptomatic SIC-T and its severe clinical course. Remarkably, the TIPS-placement in this case was performed by an unconventional approach from one single hepatic vein to an atypically situated right portal branch because of anatomic variation. Consecutively, this results in a rather straight and central direction of the TIPS stent, which is suspected to have caused the interference with the segment I bile duct. In 3 out of 4 patients with SIC-T, TIPS-placement could not be performed out of the preferred medial hepatic vein. This finding was confirmed in the logistic regression analysis that identified TIPS-placement other than from medial hepatic vein as significant risk factor for SIC-T (OR 21.0). We are aware, that the preferred TIPS route in most centers is from the right hepatic vein to the right portal vein as described before[19,20] and is seen as the standard of procedure. Nevertheless, a TIPS placement from the medial hepatic vein to the right portal vein is an accepted alternative with equal results[21]. Moreover, our data also indicate that the MHV-RPV route might help to prevent the occurrence of SIC-T.
The pathophysiological etiology for the development of (late) SIC-T remains multifactorial and not elucidated yet. Three patients (1-3) had multiple unsuspicious imaging including contras-enhanced CT-scan between TIPS-placement and the detection of SIC-T. Thus, the biliopathy must have developed several months after TIPS-placement in the majority of the patients. Other factors that can lead to a segmental biliary congestion such as portal hypertensive biliopathy, cavernoma or tumor were ruled out by CT, MRI or ERCP. A combined interplay of a mechanical compression, ischemia through compression of the segmental artery or tissue encasement through a proliferative stimulus is assumable. Also, one could hypothesize that SIC-T will result from stent placement through the segmental bile duct. Before the use of covered stents, this would have resulted in a biliary fistula as previously described[12]. In this regard, again an atypical TIPS-placement is very likely to be associated with SIC-T. Moreover, other factors that could influence a TIPS-induced compression of the bile ducts or liver tissue, for instance the diameter of dilation or the length of the TIPS, but were not analyzed in our cohort. In addition, transient bacteremia during TIPS-implantation or pathologies of the bile duct system should also be considered to contribute to SIC-T.
However, our analysis showed some limitations. First this is a retrospective analysis and in the most patients with SIC-T no interventions was needed (but one cholangitic abscess). Moreover, statistical analysis was based on 4 cases with SIC-T that could have impacted the results as a consequence of a low patient number.
In conclusion, the unusual etiology of segmental intrahepatic cholestasis caused by intrahepatic bile duct compression due to TIPS-stent ads, with a remarkable prevalence of 2.9%, to the variety of TIPS-related complications. Furthermore, SIC-T could be relevant for the management of the affected patients and may lead to cholangitic abscesses. Therefore, we propose that TIPS-patients, in particular with TIPS-placement other than from the medial hepatic vein or multiple interventions, should be screened for SIC-T in their routine follow-ups.
Transjugular intrahepatic portosystemic shunt (TIPS) is an accepted and emerging intervention in ascites and variceal bleeding related to portal hypertension. Several complications have been described so far but a segmental intrahepatic cholestasis caused by TIPS (SIC-T) was only described as case report so far.
We aimed to perform a retrospective cohort analysis to obtain prevalence and consequences of SIC-T.
Our analysis aimed at prevalence, outcome and risk factors for development of SIC-T.
This is a monocentric restrospective cohort analysis. All TIPS patients between January 2005 and August 2013 were screened for signs of biliary congestion. Cases that were conspicuous for SIC-T were reviewed by two independent radiologists. Patients data and procedural details were registered. Logistic regression analysis was performed to identify predictors for the development of SIC-T.
Out of 135 cirrhotic TIPS patients we identified 4 cases (2.9%) of SIC-T in direct proximity of the TIPS-stent. Main indications for TIPS were refractory ascites and variceal bleeding. Most patients were asymptomatic but one patient suffered from a cholangitic abscess. Logistic regression analysis identified TIPS-placement other than from medial hepatic vein to right portal vein as risk factor (OR 21.0) for SIC-T.
SIC-T is a relatively rare and late complication of TIPS. Most patient do not require an intervention but severe infectious complications can occur. Patients with multiple interventions or atypical TIPS implantation should be screened for SIC-T.
Future studies analyzing safety and complications of TIPS should include SIC-T as possible late complication of TIPS.
We acknowledge support from Universität Leipzig within the program of Open Access Publishing.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Germany
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Gencdal G, Ruiz-Margáin A, Yang L S-Editor: Wang J L-Editor: A E-Editor: Ma YJ
| 1. | European Association for the Study of the Liver. EASL clinical practice guidelines on the management of ascites, spontaneous bacterial peritonitis, and hepatorenal syndrome in cirrhosis. J Hepatol. 2010;53:397-417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1125] [Cited by in RCA: 1129] [Article Influence: 75.3] [Reference Citation Analysis (0)] |
| 2. | Boyer TD, Haskal ZJ; American Association for the Study of Liver Diseases. The Role of Transjugular Intrahepatic Portosystemic Shunt (TIPS) in the Management of Portal Hypertension: update 2009. Hepatology. 2010;51:306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 390] [Cited by in RCA: 404] [Article Influence: 26.9] [Reference Citation Analysis (1)] |
| 3. | Fagiuoli S, Bruno R, Debernardi Venon W, Schepis F, Vizzutti F, Toniutto P, Senzolo M, Caraceni P, Salerno F, Angeli P, Cioni R, Vitale A, Grosso M, De Gasperi A, D'Amico G, Marzano A; AISF TIPS Special Conference. Consensus conference on TIPS management: Techniques, indications, contraindications. Dig Liver Dis. 2017;49:121-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 110] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 4. | Hernández-Gea V, Procopet Procopet B, Giráldez Á, Amitrano L, Villanueva C, Thabut D, Ibañez-Samaniego L, Silva-Junior G, Martinez J, Genescà J, Bureau C, Trebicka J, Llop E, Laleman W, Palazon JM, Castellote J, Rodrigues S, Gluud LL, Noronha Ferreira C, Barcelo R, Cañete N, Rodríguez M, Ferlitsch A, Mundi JL, Gronbaek H, Hernández-Guerra M, Sassatelli R, Dell'Era A, Senzolo M, Abraldes JG, Romero-Gómez M, Zipprich A, Casas M, Masnou H, Primignani M, Krag A, Nevens F, Calleja JL, Jansen C, Robic MA, Conejo I, Catalina MV, Albillos A, Rudler M, Alvarado E, Guardascione MA, Tantau M, Bosch J, Torres F, Garcia-Pagán JC;. International Variceal Bleeding Observational Study Group and Baveno Cooperation. Preemptive-TIPS Improves Outcome in High-Risk Variceal Bleeding: An Observational Study. Hepatology. 2019;69:282-293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 95] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 5. | García-Pagán JC, Caca K, Bureau C, Laleman W, Appenrodt B, Luca A, Abraldes JG, Nevens F, Vinel JP, Mössner J, Bosch J; Early TIPS (Transjugular Intrahepatic Portosystemic Shunt) Cooperative Study Group. Early use of TIPS in patients with cirrhosis and variceal bleeding. N Engl J Med. 2010;362:2370-2379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 826] [Cited by in RCA: 837] [Article Influence: 55.8] [Reference Citation Analysis (0)] |
| 6. | Bettinger D, Schultheiss M, Boettler T, Muljono M, Thimme R, Rössle M. Procedural and shunt-related complications and mortality of the transjugular intrahepatic portosystemic shunt (TIPSS). Aliment Pharmacol Ther. 2016;44:1051-1061. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 51] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 7. | Rodrigues SG, Sixt S, Abraldes JG, De Gottardi A, Klinger C, Bosch J, Baumgartner I, Berzigotti A. Systematic review with meta-analysis: portal vein recanalisation and transjugular intrahepatic portosystemic shunt for portal vein thrombosis. Aliment Pharmacol Ther. 2019;49:20-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 89] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 8. | Dissegna D, Sponza M, Falleti E, Fabris C, Vit A, Angeli P, Piano S, Cussigh A, Cmet S, Toniutto P. Morbidity and mortality after transjugular intrahepatic portosystemic shunt placement in patients with cirrhosis. Eur J Gastroenterol Hepatol. 2019;31:626-632. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 9. | Bureau C, Garcia Pagan JC, Layrargues GP, Metivier S, Bellot P, Perreault P, Otal P, Abraldes JG, Peron JM, Rousseau H, Bosch J, Vinel JP. Patency of stents covered with polytetrafluoroethylene in patients treated by transjugular intrahepatic portosystemic shunts: long-term results of a randomized multicentre study. Liver Int. 2007;27:742-747. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 220] [Cited by in RCA: 225] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 10. | Rouillard SS, Bass NM, Roberts JP, Doherty CA, Gee L, Bacchetti P, Somberg KA. Severe hyperbilirubinemia after creation of transjugular intrahepatic portosystemic shunts: natural history and predictors of outcome. Ann Intern Med. 1998;128:374-377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Silva RF, Arroyo PC, Duca WJ, Silva AA, Reis LF, Cabral CM, Sgnolf A, Domingues RB, Barao GT, Coelho DJ, Deberaldini M, Felício HC, Silva RC. Complications following transjugular intrahepatic portosystemic shunt: a retrospective analysis. Transplant Proc. 2004;36:926-928. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 12. | Freedman AM, Sanyal AJ, Tisnado J, Cole PE, Shiffman ML, Luketic VA, Purdum PP, Darcy MD, Posner MP. Complications of transjugular intrahepatic portosystemic shunt: a comprehensive review. Radiographics. 1993;13:1185-1210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 229] [Cited by in RCA: 207] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 13. | Paterno F, Khan A, Cavaness K, Asolati M, Campsen J, McKenna GJ, Onaca N, Ruiz R, Trotter J, Klintmalm GB. Malpositioned transjugular intrahepatic portosystemic shunt in the common hepatic duct leading to biliary obstruction and liver transplantation. Liver Transpl. 2011;17:344-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (1)] |
| 14. | Mayan H, Kantor R, Rimon U, Golubev N, Heyman Z, Goshen E, Shalmon B, Weiss P. Fatal liver infarction after transjugular intrahepatic portosystemic shunt procedure. Liver. 2001;21:361-364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 15. | Sauerbruch T, Mengel M, Dollinger M, Zipprich A, Rössle M, Panther E, Wiest R, Caca K, Hoffmeister A, Lutz H, Schoo R, Lorenzen H, Trebicka J, Appenrodt B, Schepke M, Fimmers R; German Study Group for Prophylaxis of Variceal Rebleeding. Prevention of Rebleeding From Esophageal Varices in Patients With Cirrhosis Receiving Small-Diameter Stents Versus Hemodynamically Controlled Medical Therapy. Gastroenterology. 2015;149:660-8.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 180] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 16. | Schepis F, Vizzutti F, Garcia-Tsao G, Marzocchi G, Rega L, De Maria N, Di Maira T, Gitto S, Caporali C, Colopi S, De Santis M, Arena U, Rampoldi A, Airoldi A, Cannavale A, Fanelli F, Mosconi C, Renzulli M, Agazzi R, Nani R, Quaretti P, Fiorina I, Moramarco L, Miraglia R, Luca A, Bruno R, Fagiuoli S, Golfieri R, Torricelli P, Di Benedetto F, Belli LS, Banchelli F, Laffi G, Marra F, Villa E. Under-dilated TIPS Associate With Efficacy and Reduced Encephalopathy in a Prospective, Non-randomized Study of Patients With Cirrhosis. Clin Gastroenterol Hepatol. 2018;16:1153-1162.e7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 98] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 17. | Li YH, Xu ZY, Wu HM, Yang LH, Xu Y, Wu XN, Wan YM. Long-term shunt patency and overall survival of transjugular intrahepatic portosystemic shunt placement using covered stents with bare stents versus covered stents alone. Clin Radiol. 2018;73:580-587. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 18. | Karlas T, Hoffmeister A, Fuchs J, Tröltzsch M, Keim V. Bile duct obstruction after transjugular intrahepatic portosystemic shunt implantation. Endoscopy. 2013;45 Suppl 2 UCTN:E47-E48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 19. | Rössle M, Haag K, Ochs A, Sellinger M, Nöldge G, Perarnau JM, Berger E, Blum U, Gabelmann A, Hauenstein K. The transjugular intrahepatic portosystemic stent-shunt procedure for variceal bleeding. N Engl J Med. 1994;330:165-171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 522] [Cited by in RCA: 474] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 20. | Rössle M, Ochs A, Gülberg V, Siegerstetter V, Holl J, Deibert P, Olschewski M, Reiser M, Gerbes AL. A comparison of paracentesis and transjugular intrahepatic portosystemic shunting in patients with ascites. N Engl J Med. 2000;342:1701-1707. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 421] [Cited by in RCA: 380] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 21. | Rössle M. TIPS: 25 years later. J Hepatol. 2013;59:1081-1093. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 230] [Cited by in RCA: 285] [Article Influence: 23.8] [Reference Citation Analysis (0)] |