Published online Oct 21, 2019. doi: 10.3748/wjg.v25.i39.6016
Peer-review started: August 24, 2019
First decision: September 10, 2019
Revised: September 17, 2019
Accepted: September 27, 2019
Article in press: September 27, 2019
Published online: October 21, 2019
Processing time: 58 Days and 9.1 Hours
Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS) has been adopted by liver surgeons in recent years. However, high morbidity and mortality rates have limited the promotion of this technique. Some recent studies have suggested that ALPPS with a partial split can effectively induce the growth of future liver remnant (FLR) similar to a complete split with better postoperative safety profiles. However, some others have suggested that ALPPS can induce more rapid and adequate FLR growth, but with the same postoperative morbidity and mortality rates as in partial split of the liver parenchyma in ALPPS (p-ALPPS).
To perform a systematic review and meta-analysis on ALPPS and p-ALPPS.
A systematic literature search of PubMed, Embase, the Cochrane Library, and ClinicalTrials.gov was performed for articles published until June 2019. Studies comparing the outcomes of p-ALPPS and ALPPS for a small FLR in consecutive patients were included. Our main endpoints were the morbidity, mortality, and FLR hypertrophy rates. We performed a subgroup analysis to evaluate patients with and without liver cirrhosis. We assessed pooled data using a random-effects model.
Four studies met the inclusion criteria. Four studies reported data on morbidity and mortality, and two studies reported the FLR hypertrophy rate and one study involved patients with cirrhosis. In the non-cirrhotic group, p-ALPPS-treated patients had significantly lower morbidity and mortality rates than ALPPS-treated patients [odds ratio (OR) = 0.2; 95% confidence interval (CI): 0.07–0.57; P = 0.003 and OR = 0.16; 95%CI: 0.03-0.9; P = 0.04]. No significant difference in the FLR hypertrophy rate was observed between the two groups (P > 0.05). The total effects indicated no difference in the FLR hypertrophy rate or perioperative morbidity and mortality rates between the ALPPS and p-ALPPS groups. In contrast, ALPPS seemed to have a better outcome in the cirrhotic group.
The findings of our study suggest that p-ALPPS is safer than ALPPS in patients without cirrhosis and exhibits the same rate of FLR hypertrophy.
Core tip: Several studies have reported the comparison of complete and partial associating liver partition and portal vein ligation for staged hepatectomy (ALPPS). This meta-analysis, including all of these studies published to date, found that the partial ALPPS is safer than ALPPS in patients without cirrhosis and exhibits the same rate of future liver remnant hypertrophy. However, as the sample size is not large, more randomized controlled trials should be carried out.
- Citation: Huang HC, Bian J, Bai Y, Lu X, Xu YY, Sang XT, Zhao HT. Complete or partial split in associating liver partition and portal vein ligation for staged hepatectomy: A systematic review and meta-analysis. World J Gastroenterol 2019; 25(39): 6016-6024
- URL: https://www.wjgnet.com/1007-9327/full/v25/i39/6016.htm
- DOI: https://dx.doi.org/10.3748/wjg.v25.i39.6016
In 2012, Schnizbauer et al[1] introduced a new surgical strategy termed associating liver partition and portal vein ligation for staged hepatectomy (ALPPS) for patients with an insufficient future liver remnant (FLR) after major hepatectomy. This technique involves ligation of the portal vein and a complete split of the liver parenchyma, which can considerably accelerate FLR hypertrophy and markedly reduce the time interval between stages. However, the surgery-related morbidity and mortality rates are high. A published analysis of the international ALPPS registry, which includes 202 patients, revealed an in-hospital mortality rate of 9% and a severe complication (grade ≥ 3b)[2] rate of 28%[3]. Postoperative adverse events were evaluated according to the Clavien–Dindo classification of surgical complications[2]. A major complication was defined as a grade ≥ 3a complication. The morbidity and mortality rates can reflect the safety of this surgical strategy, and the FLR hypertrophy rate can reflect the effectiveness. Recent evidence has demonstrated that a partial split (defined as 50%–80% of the complete transection surface) of the liver parenchyma in ALPPS (p-ALPPS) results in the same rate of FLR hypertrophy as a complete split but with lower postoperative morbidity and mortality rates[4]. However, some evidence has also indicated that p-ALPPS does not have a comparable FLR hypertrophy rate and is associated with the same morbidity and mortality rates as in ALPPS[5]. Therefore, we performed a systematic review and meta-analysis of split completeness and its impact on the FLR hypertrophy, morbidity, and mortality rates in patients with a small FLR.
This systematic review and meta-analysis is reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement[6] and was registered at the International Prospective Register of Systematic Reviews (number CRD42017057798). We performed a systematic search of PubMed, Embase, the Cochrane Library, and Clinical Trials.gov for relevant studies performed until June 2019. We applied no language restrictions. The search terms used for PubMed were: ((ALPPS[All Fields] OR (associating[All Fields] AND (“liver”[MeSH Terms] OR “liver”[All Fields]) AND partition[All Fields] AND (“portal vein”[MeSH Terms] OR (“portal”[All Fields] AND “vein”[All Fields]) OR “portal vein”[All Fields]) AND (“ligation”[MeSH Terms] OR “ligation”[All Fields]) AND staged[All Fields] AND (“hepatectomy”[MeSH Terms] OR “hepatectomy”[All Fields]))) OR partial-ALPPS[All Fields]) OR (staged[All Fields] AND (“hepatectomy”[MeSH Terms] OR “hepatectomy”[All Fields])). We considered all potentially eligible studies for review. The studies in the reference list were also assessed for eligibility.
Two authors performed the literature search and study inclusion independently. Inconsistent results were resolved by a group discussion including a third author. The inclusion criterion was direct comparison between p-ALPPS and ALPPS for patients with a small FLR.
Year of publication, number of patients treated, and dichotomous data from the two treatments, such as morbidity and mortality, were extracted from each included study. We also extracted the FLR hypertrophy rate from each study as continuous data.
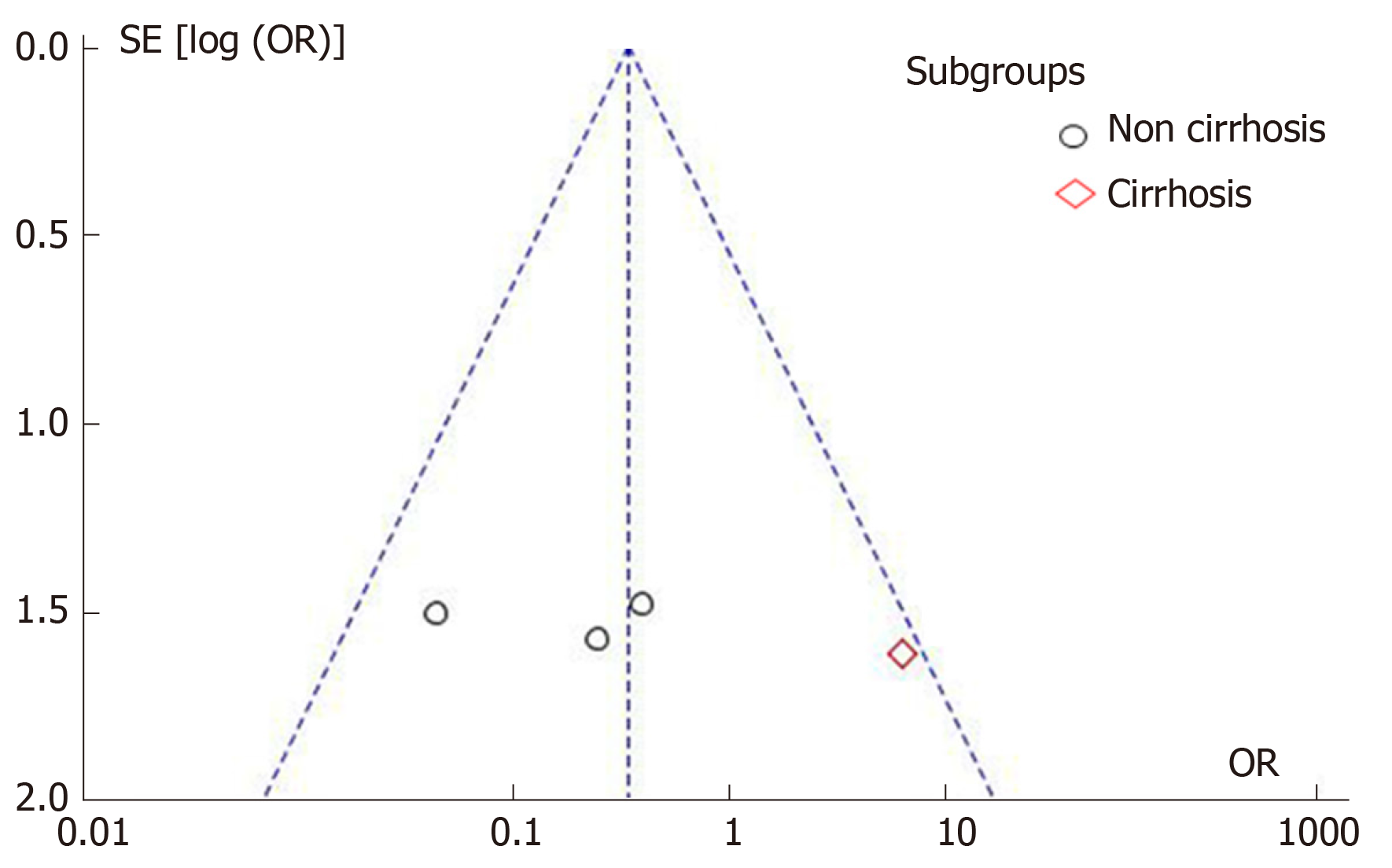
The Newcastle-Ottawa scale was used to assess the quality of retrospective studies; if the study was scored > 6, it was graded as I and when the score was ≤ 5, it was graded as II[7]. Funnel plots were used to evaluate the risk of publication bias.
We examined the effect of p-ALPPS vs ALPPS in patients with a small FLR and total patients in each study. Heterogeneity among the included studies was evaluated by I2 statistic and Chi-square test[8]. A random-effects model was applied when P < 0.10 or I2 > 50%[9]. All statistical tests were two-sided, and a P value < 0.05 was considered significant. Publication bias was evaluated by funnel plots. Statistical analyses were performed using Review Manager 5.2 (The Cochrane Collaboration, Copenhagen, Denmark).
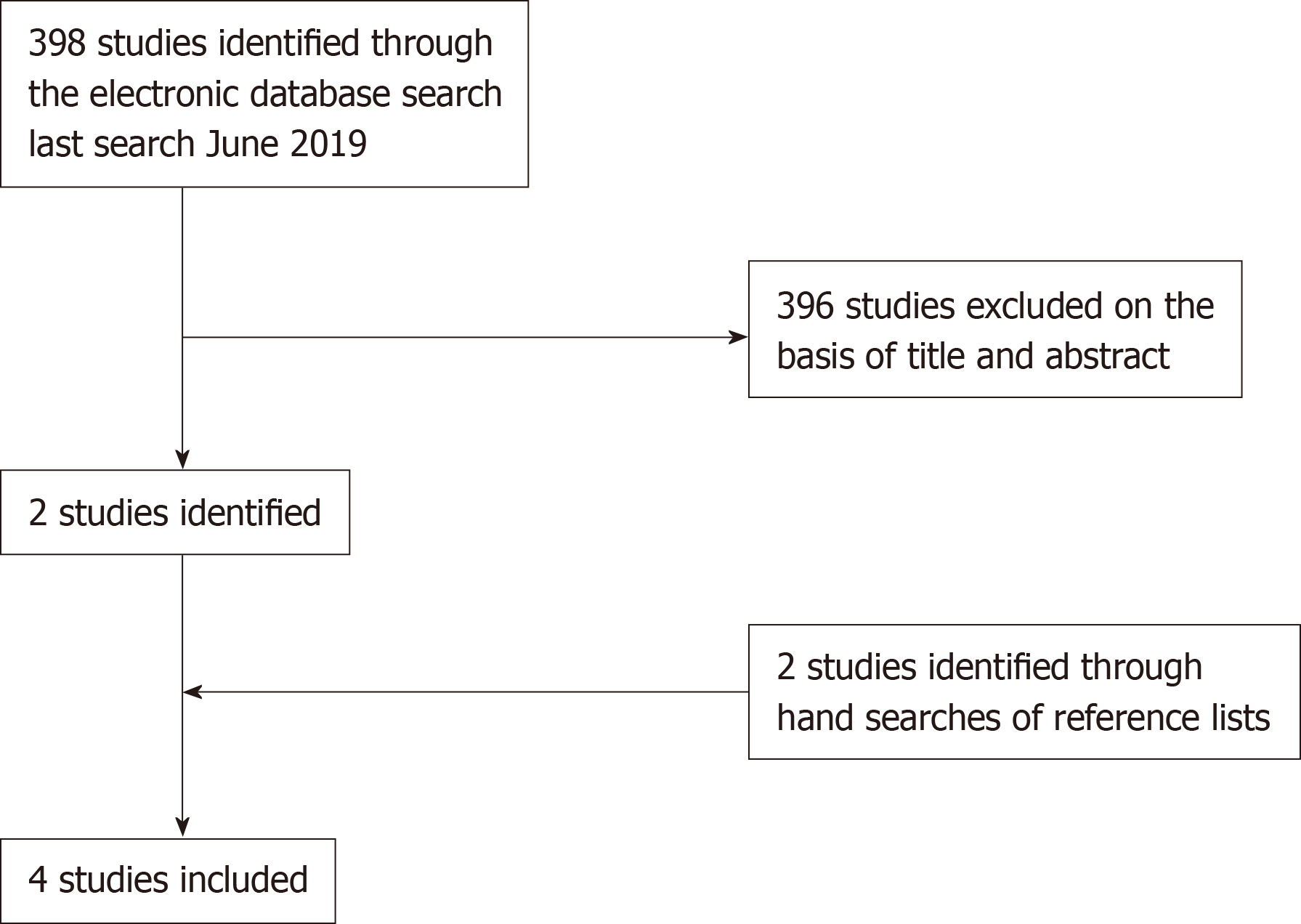
We identified 398 studies, of which 4 (with data for 124 patients)[4,5,10,11] were included in the meta-analysis (Figure 1).
The characteristics of the included studies are listed in Table 1. All four included studies were grade I according to the Newcastle–Ottawa scale[7]. Patient information in the two treatment groups is presented in Table 2. Four studies reported data on morbidity and mortality, and two studies reported the FLR hypertrophy rate (Table 2).
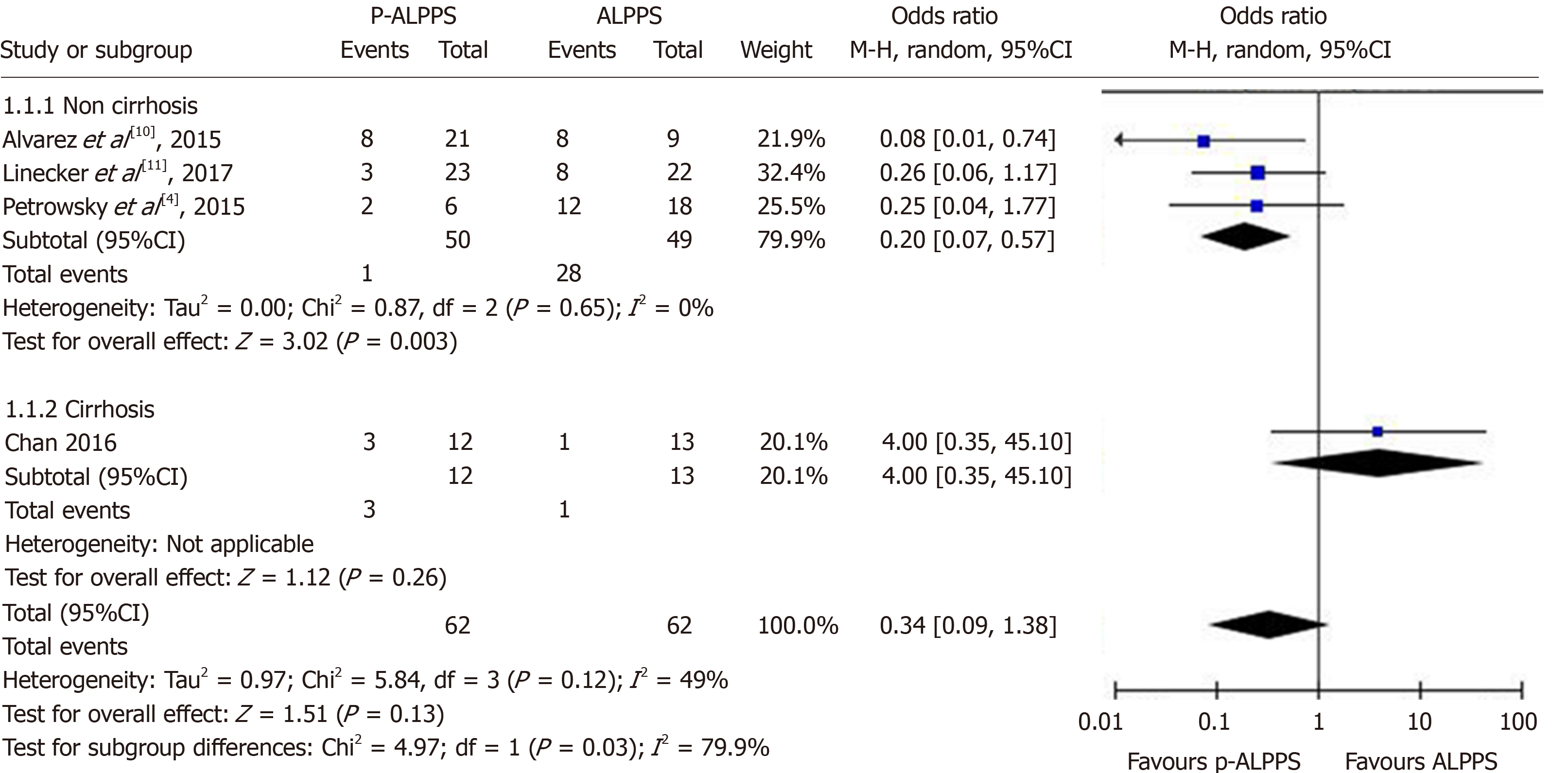
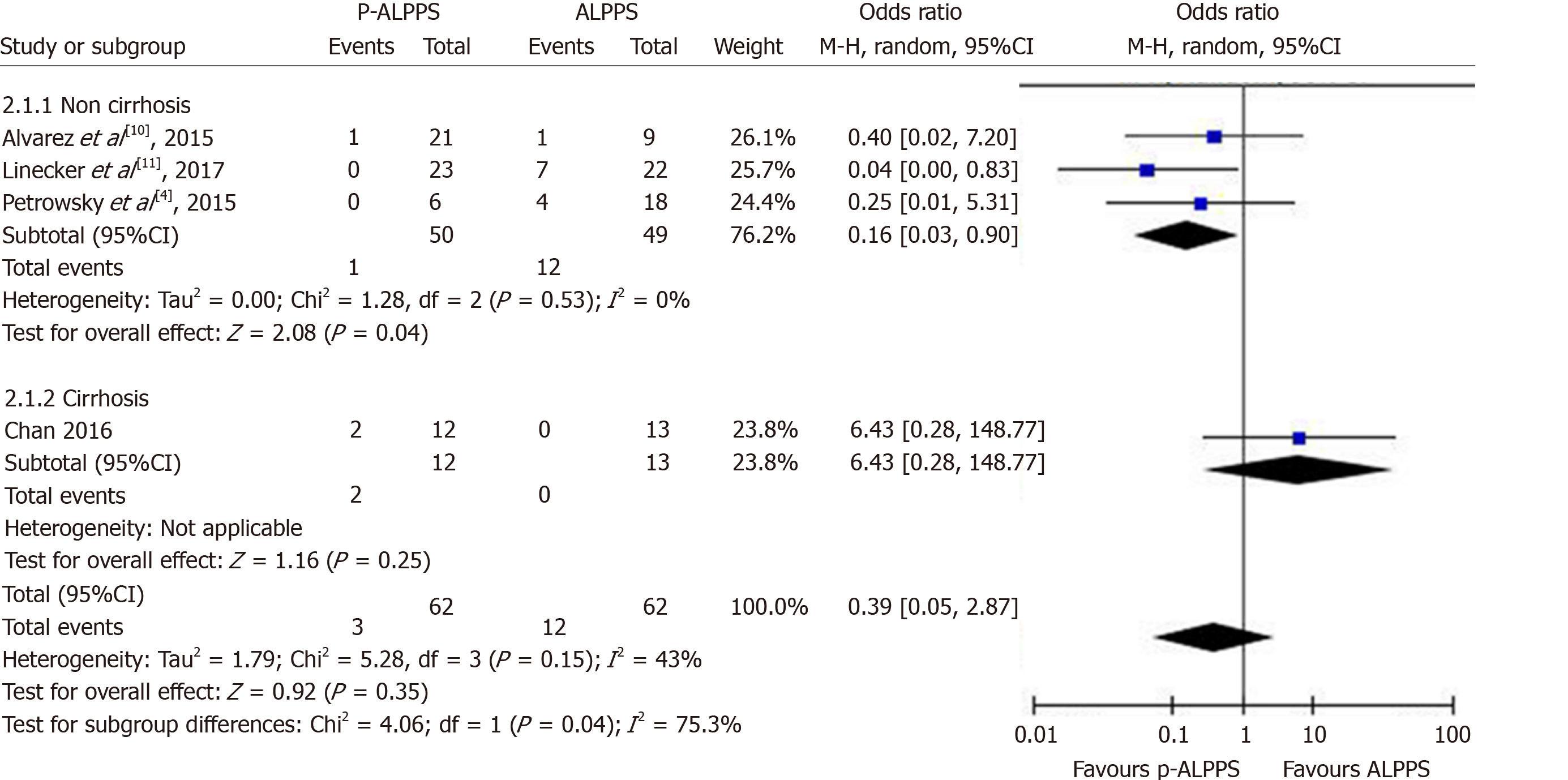
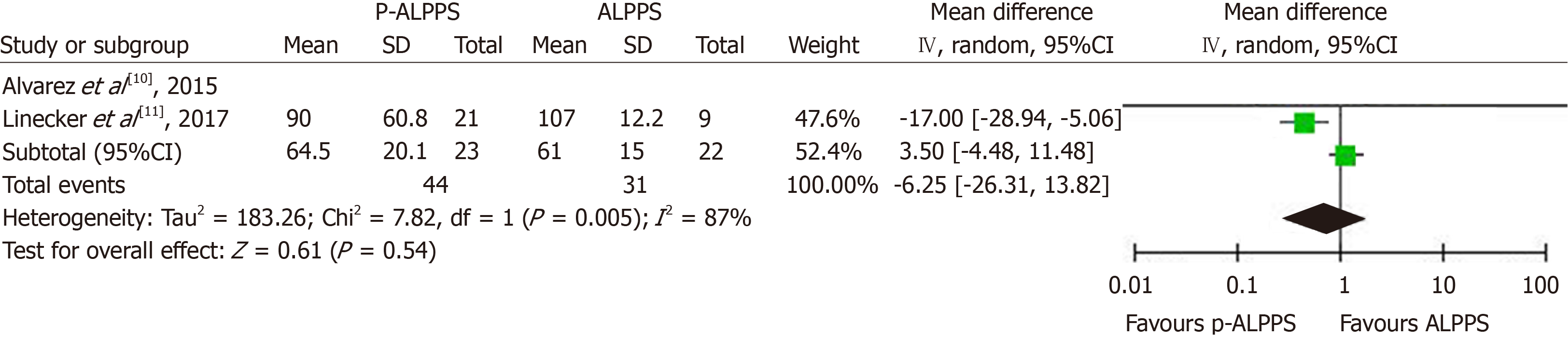
Meta-analysis was performed in the p-ALPPS and ALPPS groups. In non-cirrhotic patients, as shown in Figure 2, a significant difference was found in the morbidity rate between the two groups [odds ratio (OR) = 0.2; 95% confidence interval (CI): 0.07–0.57; P = 0.003]. As shown in Figure 3, a significant difference was observed in the mortality rate between the two groups (OR = 0.16; 95%CI: 0.03–0.9; P = 0.04). The FLR hypertrophy rate was not significantly different between the two groups (OR = − 6.25; 95%: CI: − 26.31-13.82; P = 0.54) (Figure 4).
The total effects indicated no difference in the FLR hypertrophy rate or perioperative morbidity and mortality rates between the two groups. However, the number of patients with cirrhosis was too small and only one study was involved. Therefore, the results should be interpreted with caution. Publication bias was evaluated by a funnel plot(Figure 5).
Our results show that compared with ALPPS, p-ALPPS can achieve lower surgery-related morbidity and mortality rates and exhibits the same FLR hypertrophy rate in non-cirrhotic patients. In cirrhotic patients, ALPPS seems to offer a better outcome with respect to FLR hypertrophy with no increase in morbidity or mortality. However, only one study focused on patients with cirrhosis. Therefore, the results should be interpreted with caution, and more studies are needed.
Before the introduction of ALPPS, some other strategies were applied to induce liver hypertrophy in patients with a small FLR. The most common methods were portal vein embolization (PVE) and portal vein ligation (PVL) for staged hepatectomy. PVE was first described in 1990 by Makuuchi et al[12]. In this technique, embolism of the ipsilateral portal blood flow induces rapid proliferation of the FLR. PVL was primarily used in patients with colorectal cancer liver metastases and could reportedly trigger a similar or better regenerative response than PVE[13,14]. PVE and PVL are now commonly applied in two-staged hepatectomy to improve the R0 resection rate[15-17]. Although PVE or PVL can effectively stimulate the growth of FLR, the second step of surgery is not always successful[18,19]. The main reasons include disease progression during the waiting period and insufficient liver hypertrophy. However, rapid and adequate FLR hypertrophy is the most prominent advantage of ALPPS. Although ALPPS is associated with greater FLR hypertrophy and a higher rate of completion of stage 2 than the two-staged hepatectomy, these advantages may be obtained at the cost of greater morbidity and mortality[20,21].
These disadvantages triggered the development and improvement of the ALPPS procedure. Many techniques have been proposed to reduce the postoperative morbidity and mortality rates since the introduction of this new surgical strategy[22-25]. These techniques include p-ALPPS, radiofrequency-assisted liver partition with portal vein ligation (RALPP), laparoscopic microwave ablation and portal vein ligation for staged hepatectomy, associating liver tourniquet and portal vein ligation for staged hepatectomy (ALTPS), and sequential ALTPS[26].
Most of these techniques reduced the perioperative morbidity and mortality rates by avoiding a physical split of the liver parenchyma. RALPP uses radiofrequency ablation during the laparoscopic first stage to produce a line of avascular necrosis along the future line of transection[27]. This technique ceases blood flow from the FLR to the diseased hemiliver while inducing FLR hypertrophy. The RALPP has better outcome of FLR hypertrophy than PVE and same outcome as by ALPPS, but has lower morbidity and mortality rates than ALPPS. Microwave ablation is used to treat hepatic tumors with electromagnetic microwaves to produce coagulative necrosis[28]. ALTPS using a tourniquet to ensure parenchymal compression and cessation of blood flow across the future line of transection has been described in three studies[29-31].
All of these modifications were developed to improve the safety of ALPPS. However, most of them are still in the initial stage with sporadic case reports and lack of comparison with ALPPS (with the exception of p-ALPPS, which has been addressed in many studies with some inconsistent results).
p-ALPPS is defined as ALPPS with a partial split of the liver parenchyma involving 50% to 80% of the complete transection surface. However, the exact amount of liver parenchyma that needs to be transected to trigger enough regeneration of the FLR remains unclear. Some authors have suggested extending the transection up to the middle hepatic vein[10], which means more transection may be performed than actually needed. Other surgeons have suggested at least a 50% transection based on intraoperative estimation[4]. In this case, however, the FLR hypertrophy rate may be too low. According to experimental and clinical data, p-ALPPS with a median partial transection of 61% can trigger FLR hypertrophy comparable with that of ALPPS with a complete split[10,11]. Based on the studies evaluated in the current analysis, the waiting period before the second step and the completion rate of the second step were not significantly different between p-ALPPS and ALPPS. Additionally, there is no evidence indicating that p-ALPPS is associated with a higher rate of disease progression during the waiting period.
The mechanism of FLR hypertrophy in ALPPS or p-ALPPS remains unclear. This hypertrophy might be related to redistribution of the portal blood flow between the diseased segment/s and the FLR. A recent study indicated that accelerated regeneration in ALPPS was not solely related to parenchymal transection and discontinuation of the blood supply between the two parts of the liver, but was mostly due to an “inflammatory-like reaction” leading to enhanced hepatocyte growth. The interleukin-6 level in the plasma and the interleukin-6 and tumor necrosis factor-α levels in the liver tissue reportedly increase after the first step[32], significantly facilitating the proliferation of the liver. In other words, the degree of liver parenchymal partitioning may not be the key factor in FLR hypertrophy. The similar FLR hypertrophy rate between ALPPS and p-ALPPS in the present study also seems to support these mechanisms. However, further studies are needed to determine whether there is a difference in inflammatory mediators between ALPPS and p-ALPPS.
This study has several limitations. Because of the small number of studies, especially studies involving patients with cirrhosis, this meta-analysis might have included an insufficient number of cases, leading to biased results. In addition, although a subgroup analysis was performed, the included studies may have still had publication bias as shown by the funnel plot. The retrospective nature of the studies contributes to this bias. Finally, further outcomes of this new technology should be followed up, but all included studies represent the latest research to date and thus lack long-term follow-up data.
Although our findings clearly support the use of p-ALPPS in non-cirrhotic patients with a small FLR, further studies are needed to fully evaluate the application of this treatment in practice.
Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS) has been adopted by liver surgeons. However, ALPPS with a partial split has been proposed recent years. Conflicting results have been reported between the ALPPS and partial split of the liver parenchyma in ALPPS (p-ALPPS). This systematic review and meta-analysis evaluated the difference in the future liver remnant (FLR) hypertrophy rate, postoperative morbidity and mortality rates between the ALPPS and p-ALPPS.
The FLR hypertrophy rate and safety between ALPPS and p-ALPPS are controversial.
To compare the currently reported results between ALPPS and p-ALPPS to confirm which is better for patients.
We systematically reviewed literatures on the ALPPS and p-ALPPS, and included relevant studies for meta-analysis.
The total effects indicated no difference in the FLR hypertrophy rate or perioperative morbidity and mortality rates between the ALPPS and p-ALPPS groups. However, p-ALPPS is safer than ALPPS in patients without cirrhosis and exhibits the same rate of FLR hypertrophy.
In non-cirrhotic patients, p-ALPPS resulted in the same FLR hypertrophy rate compared with the ALPPS, and is safer than ALPPS.
More studies to compare ALPPS with p-ALPPS in cirrhosis patients should be carried out.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: China
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Chandrakesan P, Shao L, Wittkopf N S-Editor: Tang JZ L-Editor: Ma JY E-Editor: Ma YJ
| 1. | Schnitzbauer AA, Lang SA, Goessmann H, Nadalin S, Baumgart J, Farkas SA, Fichtner-Feigl S, Lorf T, Goralcyk A, Hörbelt R, Kroemer A, Loss M, Rümmele P, Scherer MN, Padberg W, Königsrainer A, Lang H, Obed A, Schlitt HJ. Right portal vein ligation combined with in situ splitting induces rapid left lateral liver lobe hypertrophy enabling 2-staged extended right hepatic resection in small-for-size settings. Ann Surg. 2012;255:405-414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 837] [Cited by in RCA: 934] [Article Influence: 71.8] [Reference Citation Analysis (0)] |
| 2. | Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, de Santibañes E, Pekolj J, Slankamenac K, Bassi C, Graf R, Vonlanthen R, Padbury R, Cameron JL, Makuuchi M. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250:187-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6210] [Cited by in RCA: 8640] [Article Influence: 540.0] [Reference Citation Analysis (0)] |
| 3. | Schadde E, Ardiles V, Robles-Campos R, Malago M, Machado M, Hernandez-Alejandro R, Soubrane O, Schnitzbauer AA, Raptis D, Tschuor C, Petrowsky H, De Santibanes E, Clavien PA; ALPPS Registry Group. Early survival and safety of ALPPS: first report of the International ALPPS Registry. Ann Surg. 2014;260:829-836. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 352] [Cited by in RCA: 348] [Article Influence: 31.6] [Reference Citation Analysis (0)] |
| 4. | Petrowsky H, Györi G, de Oliveira M, Lesurtel M, Clavien PA. Is partial-ALPPS safer than ALPPS? A single-center experience. Ann Surg. 2015;261:e90-e92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 135] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 5. | Chan ACY, Chok K, Dai JWC, Lo CM. Impact of split completeness on future liver remnant hypertrophy in associating liver partition and portal vein ligation for staged hepatectomy (ALPPS) in hepatocellular carcinoma: Complete-ALPPS vs partial-ALPPS. Surgery. 2017;161:357-364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 45] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 6. | Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151:264-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21613] [Cited by in RCA: 18176] [Article Influence: 1136.0] [Reference Citation Analysis (0)] |
| 7. | Wells GA, Shea B, O’connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa: Ottawa Hospital Research Institute; 2014; Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.. |
| 8. | Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. Bmj. 2003;327:557-560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39087] [Cited by in RCA: 46560] [Article Influence: 2116.4] [Reference Citation Analysis (3)] |
| 9. | DerSimonian R, Laird N. Meta-analysis in clinical trials revisited. Contemp Clin Trials. 2015;45:139-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1231] [Cited by in RCA: 1927] [Article Influence: 192.7] [Reference Citation Analysis (0)] |
| 10. | Alvarez FA, Ardiles V, de Santibañes M, Pekolj J, de Santibañes E. Associating liver partition and portal vein ligation for staged hepatectomy offers high oncological feasibility with adequate patient safety: a prospective study at a single center. Ann Surg. 2015;261:723-732. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 106] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 11. | Linecker M, Kambakamba P, Reiner CS, Linh Nguyen-Kim TD, Stavrou GA, Jenner RM, Oldhafer KJ, Björnsson B, Schlegel A, Györi G, Schneider MA, Lesurtel M, Clavien PA, Petrowsky H. How much liver needs to be transected in ALPPS? A translational study investigating the concept of less invasiveness. Surgery. 2017;161:453-464. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 46] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 12. | Makuuchi M, Thai BL, Takayasu K, Takayama T, Kosuge T, Gunvén P, Yamazaki S, Hasegawa H, Ozaki H. Preoperative portal embolization to increase safety of major hepatectomy for hilar bile duct carcinoma: a preliminary report. Surgery. 1990;107:521-527. [PubMed] |
| 13. | Furrer K, Tian Y, Pfammatter T, Jochum W, El-Badry AM, Graf R, Clavien PA. Selective portal vein embolization and ligation trigger different regenerative responses in the rat liver. Hepatology. 2008;47:1615-1623. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 69] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 14. | Aussilhou B, Lesurtel M, Sauvanet A, Farges O, Dokmak S, Goasguen N, Sibert A, Vilgrain V, Belghiti J. Right portal vein ligation is as efficient as portal vein embolization to induce hypertrophy of the left liver remnant. J Gastrointest Surg. 2008;12:297-303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 122] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 15. | Clavien PA, Petrowsky H, DeOliveira ML, Graf R. Strategies for safer liver surgery and partial liver transplantation. N Engl J Med. 2007;356:1545-1559. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 724] [Cited by in RCA: 733] [Article Influence: 40.7] [Reference Citation Analysis (1)] |
| 16. | Brouquet A, Abdalla EK, Kopetz S, Garrett CR, Overman MJ, Eng C, Andreou A, Loyer EM, Madoff DC, Curley SA, Vauthey JN. High survival rate after two-stage resection of advanced colorectal liver metastases: response-based selection and complete resection define outcome. J Clin Oncol. 2011;29:1083-1090. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 276] [Cited by in RCA: 303] [Article Influence: 21.6] [Reference Citation Analysis (0)] |
| 17. | Song T. Recent advances in surgical treatment of hepatocellular carcinoma. Drug Discov Ther. 2015;9:319-330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 31] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 18. | Capussotti L, Muratore A, Baracchi F, Lelong B, Ferrero A, Regge D, Delpero JR. Portal vein ligation as an efficient method of increasing the future liver remnant volume in the surgical treatment of colorectal metastases. Arch Surg. 2008;143:978-982. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 119] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 19. | Turrini O, Ewald J, Viret F, Sarran A, Goncalves A, Delpero JR. Two-stage hepatectomy: who will not jump over the second hurdle? Eur J Surg Oncol. 2012;38:266-273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 38] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 20. | Eshmuminov D, Raptis DA, Linecker M, Wirsching A, Lesurtel M, Clavien PA. Meta-analysis of associating liver partition with portal vein ligation and portal vein occlusion for two-stage hepatectomy. Br J Surg. 2016;103:1768-1782. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 109] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 21. | Sparrelid E, van Gulik TM. Tumor progression in two-stage liver resections-is the shorter inter-stage period in associated liver partition and portal vein ligation for staged hepatectomy (ALPPS) of benefit to the patient? Hepatobiliary Surg Nutr. 2019;8:316-317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 22. | Lang H, de Santibañes E, Schlitt HJ, Malagó M, van Gulik T, Machado MA, Jovine E, Heinrich S, Ettorre GM, Chan A, Hernandez-Alejandro R, Robles Campos R, Sandström P, Linecker M, Clavien PA. 10th Anniversary of ALPPS-Lessons Learned and quo Vadis. Ann Surg. 2019;269:114-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 73] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 23. | Lau WY. Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS) and its further developments in the last decade. Hepatobiliary Surg Nutr. 2019;8:258-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 24. | Tanaka K. Modified ALPPS procedures: more safety through less invasive surgery. Langenbecks Arch Surg. 2017;402:563-574. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 25. | Soggiu F, Giovinazzo F, Straiton J, Turri G, Phillips J, Al-Kari B, Ahmed I, Habib M. Monosegment ALPPS hepatectomy preserving segment 4 for colorectal liver metastases: literature review and our experience. Hepatobiliary Surg Nutr. 2018;7:105-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 26. | Edmondson MJ, Sodergren MH, Pucher PH, Darzi A, Li J, Petrowsky H, Campos RR, Serrablo A, Jiao LR. Variations and adaptations of associated liver partition and portal vein ligation for staged hepatectomy (ALPPS): Many routes to the summit. Surgery. 2016;159:1058-1072. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 32] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 27. | Gall TM, Sodergren MH, Frampton AE, Fan R, Spalding DR, Habib NA, Pai M, Jackson JE, Tait P, Jiao LR. Radio-frequency-assisted Liver Partition with Portal vein ligation (RALPP) for liver regeneration. Ann Surg. 2015;261:e45-e46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 68] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 28. | Boutros C, Somasundar P, Garrean S, Saied A, Espat NJ. Microwave coagulation therapy for hepatic tumors: review of the literature and critical analysis. Surg Oncol. 2010;19:e22-e32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 94] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 29. | Robles Campos R, Brusadin R, López Conesa A, Parrilla Paricio P. Staged liver resection for perihilar liver tumors using a tourniquet in the umbilical fissure and sequential portal vein embolization on the fourth postoperative day (a modified ALTPS). Cir Esp. 2014;92:682-686. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 30. | Robles R, Parrilla P, López-Conesa A, Brusadin R, de la Peña J, Fuster M, García-López JA, Hernández E. Tourniquet modification of the associating liver partition and portal ligation for staged hepatectomy procedure. Br J Surg. 2014;101:1129-1134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 104] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 31. | Cai X, Peng S, Duan L, Wang Y, Yu H, Li Z. Completely laparoscopic ALPPS using round-the-liver ligation to replace parenchymal transection for a patient with multiple right liver cancers complicated with liver cirrhosis. J Laparoendosc Adv Surg Tech A. 2014;24:883-886. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 34] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 32. | Schlegel A, Lesurtel M, Melloul E, Limani P, Tschuor C, Graf R, Humar B, Clavien PA. ALPPS: from human to mice highlighting accelerated and novel mechanisms of liver regeneration. Ann Surg. 2014;260:839-846. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 143] [Article Influence: 14.3] [Reference Citation Analysis (0)] |