Published online Jul 21, 2017. doi: 10.3748/wjg.v23.i27.4968
Peer-review started: December 29, 2016
First decision: March 16, 2017
Revised: April 17, 2017
Accepted: June 9, 2017
Article in press: June 12, 2017
Published online: July 21, 2017
Processing time: 204 Days and 12.1 Hours
To obtain a reference range of morphological indices and establish a formula to accurately predict standard liver volume (SLV) in Chinese adults.
Computed tomography (CT)-estimated total liver volume (CTLV) was determined in 369 Chinese adults. Age, sex, body weight, body height, body mass index, and body surface area (BSA) were recorded using CT. Total splenic volume, portal venous diameter (PVD), splenic venous diameter (SVD), and portal venous cross-sectional area (PVCSA) were also measured by CT. Stepwise multiple linear regression analysis was performed to evaluate the impact of each parameter on CTLV and to develop a new SLV formula. The accuracy of the new formula was compared with the existing formulas in a validation group.
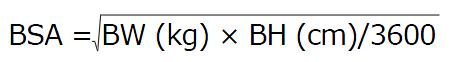
The average CTLV was 1205.41 ± 257.53 cm3 (range, 593.80-2250.10 cm3). The average of PVD, SVD and PVCSA was 9.34 ± 1.51 mm, 7.40 ± 1.31 mm and 173.22 ± 48.11 mm2, respectively. The CT-estimated splenic volume of healthy adults varied markedly (range, 46.60-2892.30 cm3). Sex, age, body height, body weight, body mass index, and BSA were significantly correlated with CTLV. BSA showed the strongest correlation (r = 0.546, P < 0.001), and was used to establish a new model for calculating SLV: SLV (cm3) = 758.259 × BSA (m2)-124.272 (R2 = 0.299, P < 0.001). This formula also predicted CTLV more accurately than the existing formulas, but overestimated CTLV in elderly subjects > 70 years of age, and underestimated liver volume when CTLV was > 1800 cm3.
Our new BSA-based formula is more accurate than other formulas in estimating SLV in Chinese adults.
Core tip: This was a prospective international phase II trial with 16 patients seeking to evaluate the effect of selenomethionine on acute toxicity in the setting of concurrent chemoradiaiton for locally advanced, inoperable non-small cell lung cancer. Selenium proved to be well tolerated and led to significantly reduced rates of myelosuppression.
- Citation: Feng LM, Wang PQ, Yu H, Chen RT, Wang J, Sheng X, Yuan ZL, Shi PM, Xie WF, Zeng X. New formula for predicting standard liver volume in Chinese adults. World J Gastroenterol 2017; 23(27): 4968-4977
- URL: https://www.wjgnet.com/1007-9327/full/v23/i27/4968.htm
- DOI: https://dx.doi.org/10.3748/wjg.v23.i27.4968
Liver volume, which can indirectly reflect liver function, is an important clinical indicator of liver disease. Changes in liver volume correlate with the prognosis and severity of liver cirrhosis, and a lower mean liver volume was observed in Child-Pugh C patients[1-3]. In liver transplantation, liver graft volume is one of the major factors determining outcome. A liver graft that is too large for the recipient will lead to poor perfusion, while a graft that is too small may cause postoperative small-for-size syndrome, primary non-function, and even severe liver failure[4-6]. Therefore, accurate estimation of total liver volume (TLV) is an important consideration for clinical condition assessment, pharmacological applications, and a variety of surgeries, especially liver transplantation.
Although liver volume can be measured by the water overflow method or calculated indirectly by liver weight[7], these methods are limited to autopsy or intraoperative use. Numerous other methods have been developed for noninvasive measurement of liver volume based on imaging, including ultrasonography[8], computed tomography (CT), and magnetic resonance imaging (MRI)[1,9,10]. CT volumetric analysis is the most frequently used among these methods. The development of helical CT, refinements in imaging techniques, and the availability of sophisticated software for three-dimensional reconstruction has improved the estimation deviation of liver volume to within 5%[11,12]. Thus, CT liver volumetry is considered the gold standard for measuring TLV. Measurement of liver volumes based on CT analysis is also used in liver resection[6,13-15] and transplantation[16,17]. However, the associated post-procedural image processing of CT volumetry is costly, time-consuming, and has not yet been successfully automated, which are obstacles in some clinical settings, particularly in developing countries.
Due to the large variability in liver size based on race, sex, body shape and body size, the difference in actual liver volume and standard liver volume (SLV) is considered more sensitive than TLV alone[1,8,18,19]. Therefore, it is important to establish SLV criteria for healthy individuals. Since DeLand et al[20] first presented their formula for calculating liver size, at least 15 other formulas have been proposed for estimating SLV. However, as yet, no single formula is statistically comparable with the TLV for the absolute volume and the percentage error reported by Pomposelli et al[18]. Furthermore, the SLV formulas derived from various ethnic groups may not be comparable with each other. Indeed, discrepancies have been observed between formulas for various Asian populations[18,19]. Thus, at present there are no formulas for assessing SLV that are generally accepted in Chinese or Western centers[18,19]. Other morphological indices, including total splenic volume (TSV), portal venous diameter (PVD), splenic venous diameter (SVD) and portal venous cross-sectional area (PVCSA), have been used as indirect measures of portal vein (PV) pressure. However, as for TLV, differences in race, sex, body shape and size, and measurement method can also affect these indices. The aim of this study was to obtain a reference range of TLV and other morphological indices for healthy Chinese adults, and to establish a new formula for assessing SLV in the Chinese population that is more accurate than current formulas.
Patients who underwent CT examination between October 2014 and January 2016 in Shanghai Changzheng Hospital, Shanghai, China and who met the following criteria were included in the analysis. Eligibility criteria were as follows: (1) > 18 years of age; (2) normal liver function and no history of liver disease; and (3) either sex. Exclusion criteria were: (1) presence of hepatitis B or hepatitis C virus infection, alcoholic liver disease, non-alcoholic fatty liver disease, autoimmune liver disease, and hepatitis caused by other etiology; (2) liver cirrhosis or other liver diseases; (3) patients with confirmed or highly suspected diagnosis of primary or secondary liver cancer; (4) history of diseases affecting TLV or total spleen volume, such as cysts, hemangioma, and other benign lesions in the liver and spleen (1 cm in diameter, and 2 in number), hematologic diseases, connective tissue disorders, or history of severe infectious diseases; and (5) conditions with a hemodynamic effect on the PV, including PV thrombosis, embolism, or sponge appearance change.
A total of 244 subjects were included to establish a new formula. A further 125 subjects were included to validate the formula. For each subject, body weight (BW; kg) and body height (BH; m) were recorded at the time of CT examination. Body mass index (BMI) was calculated as: BMI = BW/BH2. Body surface area (BSA) was calculated using Mosteller’s formula[21] as follows:
Math 1
The study protocol was reviewed and approved by the Institutional Ethics Committee of Shanghai Changzheng Hospital, and all subjects provided signed informed consent.
Patients were examined using a multi-slice spiral CT scanner (Brilliance 256-slice spiral CT scanner; Philips Medical Systems, the Netherlands) with a collimating reconstruction thickness of 1 mm and an interval of 1 mm. Abdominal contrast-enhanced CT was completed by professional technicians in accordance with standard operating procedures. To improve the quality of examinations, patients were placed in the supine position and trained to hold their breath to reduce breathing and movement artifacts during scanning.
The morphological indices assessed included CT estimated TLV (CTLV), CT-based total splenic volume (CTSV), PVD, SVD, and PVCSA. These variables were measured on portal phase images by two medical students blinded to the clinical results under the supervision of an experienced radiologist using an image-analysis program (Phillips Intellispace Portal Workstation; Philips Medical Systems). CTLV and CTSV were obtained as a summation by manually tracing the boundaries on each transverse image, avoiding the large vessels, gallbladder, and fissures. PVD and PVCSA were measured at the midpoint between the portal bifurcations and the venous confluences, while SVD was detected at the point 1 cm proximal to the confluence of the PV and splenic vein.
In the validation group, CTLV was measured as above, and SLV was calculated using our new formula and seven other previously reported formulas. The detailed information of each formula is shown in Supplementary Table 1.
| Total, n = 244 | Male, n = 138 | Female, n = 106 | P value | |
| Age, yr | 48.8 ± 12.00 (18-88) | 49.4 ± 11.59 (18-81) | 48.0 ± 12.49 (18-88) | 0.355 |
| Body height, cm | 167.29 ± 7.14 (148-185) | 172.10 ± 4.95 (156-185) | 161.04 ± 4.04 (148-172) | < 0.001 |
| Body weight, kg | 65.41 ± 10.92 (38-96) | 70.86 ± 9.35 (49-96) | 58.32 ± 8.47 (38-80) | < 0.001 |
| BMI, kg/m2) | 23.29 ± 3.06 (15.63-35.16) | 23.91 ± 2.95 (17.16-35.16) | 22.47 ± 3.02 (15.63-30.04) | < 0.001 |
| BSA, m2 | 1.74 ± 0.17 (1.25-2.21) | 1.84 ± 0.13 (1.47-2.21) | 1.61 ± 0.13 (1.25-1.94) | < 0.001 |
| CTLV, cm3 | 1194.31 ± 238.25 (593.80-2250.10) | 1268.32 ± 228.09 (815.10-2250.10) | 1097.96 ± 216.60 (593.80-2005.80) | < 0.001 |
All analytical tests were performed using SPSS 21 (IBM SPSS, Chicago, IL, United States). Data are expressed as mean ± SD. The correlations between CTLV and age, sex (men = 1, women = 0), BW, BH, BSA, and BMI were analyzed by Pearson correlation analysis. Stepwise multiple linear regression analysis was performed to evaluate the impact of each parameter and to develop a new equation that more accurately predicted CTLV. CTLV was compared with SLV calculated by formulas using a t-test, with absolute volume and percentage error as (SLV - CTLV)/CTLV × 100. We used ± 10% and ± 15% as acceptable ranges for differences between estimated SLV and CTLV[18,22], and the proportions of the estimates within these acceptable ranges were determined for each SLV formula. All statistical analyses were two-tailed, and P values less than 0.05 were considered to indicate statistical significance.
A total of 244 healthy adults (138 men and 106 women) were enrolled to establish the new SLV formula. The mean age was 48.81 ± 12.00 years, with no differences in age between the sexes (48.81 ± 12.00 years vs 48.00 ± 12.49 years, respectively; P = 0.355). Anthropometric data, including BH, BW, BMI and BSA, are shown in Table 1. The mean BH and BW of men were larger than those of women (BH: 172.10 ± 4.95 vs 161.04 ± 4.04, respectively; BW: 70.86 ± 9.35 vs 58.32 ± 8.47, respectively; P < 0.001 for both). BMI and BSA were also significantly different between the sexes (Table 1). The average CTLV in all subjects was 1194.31 ± 238.25 cm3 (range, 593.80-2250.10 cm3). Eleven of 138 men and 26 of 206 women had a liver volume smaller than 80% of the mean volume (955.4 cm3), while 33 men and 7 women had a liver volume larger than 120% of the mean volume. As expected, there was a significant difference in CTLV between men and women (1268.32 ± 228.09 vs 1097.96 ± 216.60 cm3, respectively; P < 0.001), which may be related to the difference in body frame between men and women.
We also measured CTSV, PVD, SVD and PVCSA in Chinese adults using CT (Table 2). The average CTSV in healthy Chinese adults was 210.48 ± 224.07 cm3 (range, 46.60-2892.30 cm3), with large individual variations observed (Table 2). The mean PVD, SVD and PVCSA were 9.34 ± 1.51 mm, 7.40 ± 1.31 mm and 173.22 ± 48.11 mm2, respectively. Three of 213 subjects had a PV larger than 13 mm, the widely referenced upper limit. There were no differences in CTSV or SVD between men and women. Pearson correlation analysis showed that CTSV was not associated with anthropometric indices, including sex, BH, BW, BMI or BSA (Supplementary Table 2).
| Total, n = 244 | Male, n = 138 | Female, n = 106 | P value | |
| CTSV, in cm3 | 210.48 ± 224.07 (46.60-2892.30) | 213.91 ± 172.76 (46.60-1490.30) | 206.02 ± 277.87 (65.00-2892.30) | 0.786 |
| PVD, in mm | 9.34 ± 1.5 (5.60-16.25) | 9.84 ± 1.56 (6.10-16.25) | 8.27 ± 1.23 (5.60-12.95) | < 0.001 |
| SVD, in mm | 7.40 ± 1.31 (3.20-12.50) | 7.61 ± 2.95 (4.70-12.50) | 7.17 ± 3.02 (3.20-10.50) | 0.278 |
| PVCSA, mm2 | 173.22 ± 48.11 (92.22-451.00) | 189.63 ± 50.88 (101.91-451.00) | 153.74 ± 36.16 (92.22-253.34) | < 0.001 |
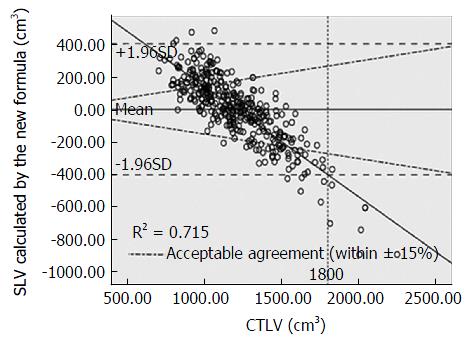
Pearson correlation analysis showed a negative correlation between TLV and age, and a positive correlation between TLV and sex, BH, BW, BMI and BSA (Table 3; correlation coefficients = -0.117, 0.355, 0.421, 0.534, 0.416 and 0.546, respectively). Of these factors, BSA had the strongest correlation (r = 0.546, P < 0.001), while age had the weakest correlation (r = -0.117, P = 0.067). Conversely, stepwise multiple linear regression analysis showed that BSA and age were the only two definite independent correlation factors for CTLV. Because of the small partial regression coefficient for age (-2.246/year), we considered that its effect on TLV was negligible, and we thus removed this factor from the new SLV formula. The final formula used to calculate SLV based on BSA was: SLV (cm3) = 758.259 × BSA (m2) - 124.272; R2 = 0.299, P < 0.001). The scatter plot is shown in Figure 1.
| Factor | r value | P value |
| Age | -0.117 | 0.067 |
| Sex | 0.355 | < 0.001 |
| BH | 0.421 | < 0.001 |
| BW | 0.534 | < 0.001 |
| BMI | 0.416 | < 0.001 |
| BSA | 0.546 | < 0.001 |
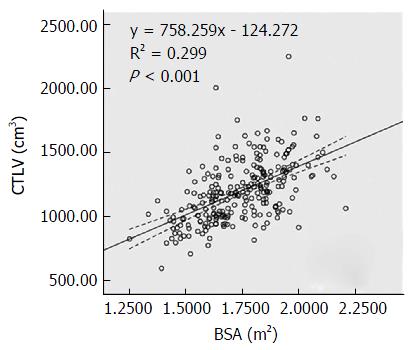
Based on the results of Pomposelli et al[18], John’s formula[23] showed a calculated SLV closest to CTLV, while Poovathumkadavil’s formula[19] showed the lowest percentage error. However, Urata’s formula[11] is the most frequently used worldwide. Therefore, we selected these three formulas plus four others established in the Chinese population[24-27] and compared these with our new formula in the validation group (n = 125). Although the root of the mean predicted residual sum of squares and the intra-class correlation were similar between all formulas, only Urata’s, Fu-Gui’s, and our new formula had a mean percentage error of SLV vs CTLV lower than ± 10%. Our new formula and Urata’s formula were the most accurate for assessing absolute volumes, which were very close to the CTLV. In contrast, the mean absolute values of difference calculated by the other six formulas were > 100 cm3. Indeed, our formula underestimated the mean SLV by < 10 cm3 compared with the mean CTLV, while the average deviation of Urata’s formula was 37 cm3 (Table 4). Nevertheless, there were no significant differences between the mean liver volume estimated by either of these formulas and the CTLV. Furthermore, the SLV derived from our formula showed almost perfect agreement with liver volume using Urata’s formula (R2 = 0.993, P < 0.001, Figure 2). Our new formula showed the highest proportion of estimated SLV with percentage errors compared with CTLV for both levels of agreement, which was greater than that for Urata’s formula (60.8% vs 57.6%, and 44.0% vs 20.8%, respectively, Table 5).
| Study | Mean SLV-TLV, in cm3 | Mean error, as % | P value | Root of the mean PRESS | ICC |
| Urata et al[11], 1995 | 37.45 | 6.95 | 0.066 | 225.72 | 0.668 |
| Johnson et al[23], 2005 | 232.94 | 22.92 | < 0.001 | 216.79 | 0.668 |
| Poovathumkadavil et al[19], 2010 | 169.96 | 10.82 | < 0.001 | 216.67 | 0.686 |
| Lin et al[24], 1998 | 271.54 | 25.74 | < 0.001 | 225.40 | 0.652 |
| Chan et al[25], 20061,2 | -165.31 | -10.82 | < 0.001 | 216.60 | 0.686 |
| Yuan et al[26], 20083 | 104.16 | 11.72 | < 0.001 | 216.03 | 0.672 |
| Fu-Gui et al[27], 2009 | -103.28 | -5.35 | < 0.001 | 218.85 | 0.686 |
| Our new SLV, 2016 | 8.10 | 4.17 | 0.680 | 219.43 | 0.679 |
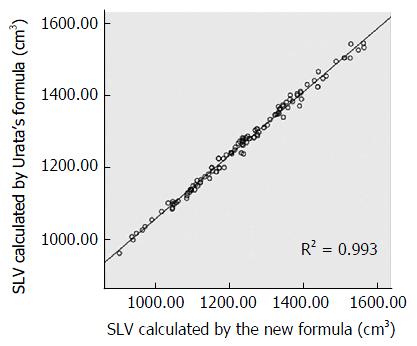
Our formula was the most accurate for estimating both absolute volume and the percentage error. However, the proportions of estimated SLV with percentage errors compared with CTLV within ± 10% and ± 15% agreement using our new formula were just 44.0% and 60.8%, respectively. We suspect that factors related to differences between CTLV and SLV may have limited the application of our formula. A total of 369 subjects (244 for formula establishment, 125 for validation) were enrolled to analyze the latent factors (Table 6). The new formula overestimated the CTLV of elderly subjects (age > 70 years) (P < 0.05, Table 6), with a decreased correlation between SLV and CTLV in this population (Figure 3). Scatter plots and fitted lines (Figure 4) showed that SLV also tended to underestimate liver volume when the CTLV was > 1800 cm3.
| Factor | n | TLV, in cm3 | SLV-TLV, in cm3 |
| Total | 369 | 1205.41 ± 257.53 | |
| Sex | |||
| Male | 219 | 1285.64 ± 252.27 | -1.82 ± 218.70 |
| Female | 150 | 1088.27 ± 217.76a | 9.40 ± 187.04 |
| Age, in yr | |||
| 18-30 | 14 | 1143.50 ± 192.33 | -16.51 ± 122.80 |
| 30-50 | 184 | 1217.30 ± 259.75 | -7.06 ± 210.37 |
| 50-70 | 158 | 1211.43 ± 263.84 | 4.52 ± 209.63 |
| > 70 | 13 | 1030.55 ± 118.18a | 140.69 ± 124.56a |
| BMI, in kg/m2 | |||
| < 18.5 | 19 | 973.94 ± 163.74 | 4.65 ± 138.26 |
| 18.5-24.9 | 250 | 1162.63 ± 231.54a | 12.70 ± 197.74 |
| ≥ 25 | 100 | 1356.33 ± 262.51a | -22.50 ± 235.32 |
Precise measurement of liver volume and correct assessment of SLV have important implications for estimating liver function and making strategic medical decisions for liver transplantation. Due to the marked effects of race and body indices on SLV, it is important to develop a method for SLV calculation that can be applied to particular demographic groups. In the present study, we determined morphological variables including CTLV, CTSV, PVD, SVD and PVCSA using CT in healthy adult Chinese subjects, and determined the medical reference ranges for Chinese men and women older than 18 years of age. We found a direct correlation between liver volume and various body indices, including sex, BH, BW, BMI and BSA. Based on Pearson’s correlation and stepwise multiple linear regression analyses, BSA was selected to establish a new formula for estimating SLV. In addition, we confirmed the precision of our formula for calculating SLV in healthy Chinese adults by comparing it with seven other reported formulas.
Previous studies have reported significant differences in TLV between Asian and Caucasian populations[5,23,28]. Kokudo et al[5] reported an average TLV of 1092 cm3 in Japanese populations and 1622 cm3 in Swiss populations, while TLV volumes in Chinese populations were reported to range from 1099.10-1220.1 cm3[24-27]. Thus, there seem to be notable racial differences, rather than geographical differences, in TLV. The mean TLV represented by CTLV in the present study was 1194.31 ± 238.25 cm3, providing further support for racial differences in liver volume. There are 56 different ethnic groups in China, although Han is the major population. As there were few other ethnic groups included in the present study, differences in TLV between distinct ethnic groups were not analyzed, and the accuracy of our formula in ethnic minorities remains unclear.
A number of body indices have been reported to impact liver volume, including sex, age, BH, BW, BMI and BSA. Of these factors, BSA is the most widely accepted parameter for determining SLV. BSA is widely used to normalize measurement of biological function with respect to variations in body size. Several formulas have been developed to calculate BSA, including Du Bois’s formula[29]: BSA (m2) = BW (kg) 0.425 × BH (cm) 0.725 × 0.007184. However, due to its convenience and accuracy in the Chinese population, we selected Mosteller’s formula[21] to estimate BSA. Since DeLand et al[20] first presented their formula for calculating liver size based on BSA, numerous studies have used BSA as an independent factor for liver size estimation[11,23,26]. As expected, BSA was also the best indicator for estimating liver volume in the present study, providing further support linking BSA with SLV.
BMI has also been used to adjust the influence of body size on biological function. Surprisingly, although many studies have reported that BMI can affect SLV, there are no SLV formulas based on BMI. This may relate to the even stronger association between BSA and TLV compared with that between BMI and TLV. Indeed, we found that BMI was positively correlated with CTLV in Pearson’s correlation analysis (coefficient of correlation = 0.416). However, this index was excluded from our new SLV formula by stepwise multiple linear regression analysis. In addition, Hashimoto et al[30] reported that TLV may be underestimated in thin individuals with a BMI < 18.5. In contrast, in the present study, we did not find this association when comparing differences between TLV and SLV calculated using our formula.
Similar to the findings by DeLand et al[20], we found a correlation between TLV and both BH and BW (correlation coefficient = 0.421 and 0.534, respectively). With increasing BH or BW, there was a gradual increase in CTLV. Although BSA based on BW and BH showed an excellent correlation with TLV, liver size was not predicted exactly by BW and/or BH. Thus, both BW and BH were eliminated in the SLV formula by stepwise multiple linear regression analysis, and SLV estimated by formulas based on BW/BH[19,24,25,27] were significantly different from the actual TLV.
Sex is another important factor that can affect liver size, with the majority of studies showing that men have a larger TLV than women[7,31]. In the present study, there was a weak correlation between sex and TLV. However, sex is not widely used in the formula for calculating SLV. For example, sex was included as a factor in the SLV formula in two studies, as women (particularly those < 50 years old) showed significantly smaller liver volume compared with males with the same BMI[25,31]. In contrast, Pomposelli et al[18] reported that sex did not improve the accuracy of SLV calculation. Similarly, in the present study, sex was not an independent correlation factor of CTLV by stepwise multiple linear regression analysis. These contrasting findings may be explained by the fact that the effect of sex on TLV is contained in that of BSA. DeLand et al[20] and Urata et al[11] reported that men and women have similar LV/BSA or liver weight/BSA ratios. Similarly, there were no differences in the LV/BSA ratio between men and women in the present study (691.10 ± 117.27 vs 673.90 ± 116.53, respectively; P = 0.166), while there was a difference in the LV/BW ratio with sex (P < 0.05).
Age is also an important consideration when assessing SLV. Hashimoto et al[30] reported that SLV estimated using their equation overestimated the TLV of older donors (≥ 50 years of age), while Pomposelli et al[18] found no benefit of adjusting for age in their SLV formula. In the present study, age was an independent predictor of SLV by multiple linear regression, with a similar coefficient to that of Kokudo et al[5]. To validate the precise impact of age on liver volumes, we used 8-year interval interpretation as a presentation for the liver volume measurement and established another new formula based on age stratification: SLVa = 857.088 × BSA - 21.228 × Age - 205.070 (aged between 18 and 26, value of Age was 1; aged between 27 and 34, value of Age was 2; and so on). Then we compared the difference of SLV, SLVa and TLV. Consistent with our expectation, the mean Error between SLVa and TLV was 3.63%, which was not significant different with the mean Error between SLV and TLV (4.17%, P = 0.283). Therefore, considering that the partial regression coefficient (-2.246/year) was very small, we considered that the effect of this variable in adults was negligible. Thus, age was excluded from our final formula, as reported by Vauthey et al[28]. However, it is still possible that age may have an effect on TLV in specific populations. In the present study, the correlation between TLV and SLV decreased in subjects > 70 years of age, and SLV was always overestimated in these individuals. Therefore, further studies are required to evaluate the validity of our new formula in a large elderly population.
At present, Urata’s formula[11] is the most frequently used for calculating SLV worldwide. Pomposelli et al[18] compared 16 different SLV formulas and found that Johnson’s formula[23] was the most accurate in terms of assessing absolute liver volume with a relatively low percentage error, while Poovathumkadavil’s formula[19] provided the lowest percentage error versus actual TLV. However, these formulas have not been validated in the Chinese population. To the best of our knowledge, there are four formulas based on the Chinese population established by Lin et al[24], Chan et al[25], Yuan et al[26], and Fu-Gui et al[27]. Nevertheless, these formulas have not gained general acceptance in Chinese or Western centers. In the present study, our new formula based on SLV was more accurate for assessing absolute liver volume compared with the other formulas, with the exception of Urata’s formula. Furthermore, our formula showed the strongest agreement with TLV. Thus, despite the limited adjusted R2 value, our formula is easily calculated and should be considered when assessing SLV in the Chinese population.
There are few reports on spleen volume and SVD in the normal population, with evidence of marked differences in those studies[32,33]. For example, spleen size determined by CT was relatively larger than that measured at postmortem, which may be explained by differences in the measurement methods or by removal of blood from the spleen during surgery. In the present study, CTSV varied markedly in various subjects (average CTSV = 210.48 ± 224.07 cm3), as reported in previous CT imaging studies[9,34]. Spleen volume was also reported to be related to age, BW, and BSA, although this correlation was not confirmed by other investigators or in the present study[29].
PVD and PVCSA were significantly enlarged in the high portal venous pressure group. PVD is regarded as an essential indicator of portal hypertension[35]. However, there are limited studies assessing PVCSA, as it is difficult to measure. PVD values in healthy adults were reported to range from 9.6-12.5 mm, with 13 mm accepted as the upper limit of PVD in many major medical textbooks. Nevertheless, Stamm et al[36] reported that PVD measured by CT was larger than this upper limit, which may be related to the different methods used to measure PVD. Many earlier studies detected PVD using ultrasonography, while Stamm et al[36] used CT imaging. However, in contrast to the findings of Stamm et al[36], we found that PVD was 9.34 ± 1.51 mm (range, 5.6-16.25 mm), with only 3 of 213 subjects having a PVD larger than 13 mm. Thus, further studies are required to compare ultrasound and CT for the measurement of PVD and PVCSA.
There are some limitations in the present study. In addition to TLV, the liver segmentation proposed by Couinaud is used in everyday clinical practice, which divided the liver into 8 operatively relevant segments based on the anatomy of the PV and hepatic vein[37]. Some studies that have reported the change of volume in different locations of liver could hint at some liver diseases[38]. Our further study will continue to propose the range of normal value of the volume of the 8 liver segments and investigate the correlation between the volume of different liver segments and body indices. When TLV was large, especially > 1800 cm3, the accuracy of our formula for SLV decreased. Liver steatosis may affect liver volume. Although we set very strict exclusion criteria, we did not obtain liver biopsy results, and our study may have included subjects with liver steatosis or mild fatty liver. Hwang et al[14] also reported that the calculated decrease in SLV was larger than the reduction in CTLV after body weight loss. Nevertheless, this formula has not been used in individuals with a short-term and rapid decrease in body weight. Our formula also used BSA as a major variable, which may be influenced considerably by the presence of ascites or edema. Hence, the application of our formula in patients with chronic liver disease and liver cirrhosis remains to be assessed.
In conclusion, by setting strict exclusion criteria, we obtained the TLV of healthy Chinese adults, and developed a new formula for estimating SLV based on BSA. This formula predicted the SLV in the Chinese population more accurately than other previously reported formulas.
Liver volume, which can indirectly reflect liver function, is an important clinical indicator of liver disease. Accurate estimation of total liver volume (TLV) is an important consideration for clinical condition assessment, pharmacological applications, and a variety of surgeries, especially liver transplantation. Computed tomography liver volumetry is considered the gold standard for measuring TLV. The standard liver volume (SLV) formulas derived from various ethnic groups may not be comparable with each other.
The multiple comparison of liver volumes obtained by different methods were very similar without statistically significant differences, However, the three methods achieved an efficiency of 27.63 min, 1.26 min and 1.18 min on average, respectively, compared with the manual volumetry, which took 43.98 min (Journal of Applied Clinical Medical Physics, 2016).
By setting strict exclusion criteria, the authors obtained the TLV of healthy Chinese adults, and developed a new formula for estimating SLV based on BSA. This formula predicted the SLV in the Chinese population more accurately than other previously reported formulas.
The authors were able to use the SLV formula to obtain the SLV of patients with liver cirrhosis, resulting in its normal state of the liver volume prediction, compared with the actual liver volume, from which the reserved liver function can be evaluated. The optimal size of liver resection for hepatectomy in patients with hepatocellular carcinoma is of great significance for the evaluation of donor liver volume in donor and recipient liver transplantation.
The current manuscript would like to create a SLV and vascular structure in Chinese adult. It’s an interesting and well-written paper.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Chiu KW S- Editor: Gong ZM L- Editor: Filipodia E- Editor: Zhang FF
| 1. | Saygili OB, Tarhan NC, Yildirim T, Serin E, Ozer B, Agildere AM. Value of computed tomography and magnetic resonance imaging for assessing severity of liver cirrhosis secondary to viral hepatitis. Eur J Radiol. 2005;54:400-407. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 34] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 2. | Chen XL, Chen TW, Zhang XM, Li ZL, Zeng NL, Li T, Wang D, Li J, Fang ZJ, Li H. Quantitative assessment of the presence and severity of cirrhosis in patients with hepatitis B using right liver lobe volume and spleen size measured at magnetic resonance imaging. PLoS One. 2014;9:e89973. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 3. | Caldwell SH, de Lange EE, Gaffey MJ, Sue M, Boyd JC, Dickson RC, Driscoll C, Stevenson WC, Ishitani MB, McCullough C. Accuracy and significance of pretransplant liver volume measured by magnetic resonance imaging. Liver Transpl Surg. 1996;2:438-442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 28] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Kawasaki S, Makuuchi M, Matsunami H, Hashikura Y, Ikegami T, Chisuwa H, Ikeno T, Noike T, Takayama T, Kawarazaki H. Preoperative measurement of segmental liver volume of donors for living related liver transplantation. Hepatology. 1993;18:1115-1120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 166] [Cited by in RCA: 150] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 5. | Kokudo T, Hasegawa K, Uldry E, Matsuyama Y, Kaneko J, Akamatsu N, Aoki T, Sakamoto Y, Demartines N, Sugawara Y. A new formula for calculating standard liver volume for living donor liver transplantation without using body weight. J Hepatol. 2015;63:848-854. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 36] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 6. | Schindl MJ, Redhead DN, Fearon KC, Garden OJ, Wigmore SJ; Edinburgh Liver Surgery and Transplantation Experimental Research Group (eLISTER). The value of residual liver volume as a predictor of hepatic dysfunction and infection after major liver resection. Gut. 2005;54:289-296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 430] [Cited by in RCA: 416] [Article Influence: 20.8] [Reference Citation Analysis (0)] |
| 7. | Yu HC, You H, Lee H, Jin ZW, Moon JI, Cho BH. Estimation of standard liver volume for liver transplantation in the Korean population. Liver Transpl. 2004;10:779-783. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 73] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 8. | Zoli M, Cordiani MR, Marchesini G, Abbati S, Bianchi G, Pisi E. Ultrasonographic follow-up of liver cirrhosis. J Clin Ultrasound. 1990;18:91-96. [PubMed] [DOI] [Full Text] |
| 9. | Henderson JM, Heymsfield SB, Horowitz J, Kutner MH. Measurement of liver and spleen volume by computed tomography. Assessment of reproducibility and changes found following a selective distal splenorenal shunt. Radiology. 1981;141:525-527. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 156] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 10. | Shimamoto D, Nishie A, Asayama Y, Ushijima Y, Takayama Y, Fujita N, Shirabe K, Hida T, Kubo Y, Honda H. MR Prediction of Liver Function and Pathology Using Gd-EOB-DTPA: Effect of Liver Volume Consideration. Biomed Res Int. 2015;2015:141853. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Urata K, Kawasaki S, Matsunami H, Hashikura Y, Ikegami T, Ishizone S, Momose Y, Komiyama A, Makuuchi M. Calculation of child and adult standard liver volume for liver transplantation. Hepatology. 1995;21:1317-1321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 712] [Cited by in RCA: 704] [Article Influence: 23.5] [Reference Citation Analysis (0)] |
| 12. | Heymsfield SB, Fulenwider T, Nordlinger B, Barlow R, Sones P, Kutner M. Accurate measurement of liver, kidney, and spleen volume and mass by computerized axial tomography. Ann Intern Med. 1979;90:185-187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 337] [Cited by in RCA: 313] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 13. | Pulitano C, Crawford M, Joseph D, Aldrighetti L, Sandroussi C. Preoperative assessment of postoperative liver function: the importance of residual liver volume. J Surg Oncol. 2014;110:445-450. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 51] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 14. | Hwang S, Ha TY, Song GW, Jung DH, Ahn CS, Moon DB, Kim KH, Lee YJ, Lee SG. Quantified Risk Assessment for Major Hepatectomy via the Indocyanine Green Clearance Rate and Liver Volumetry Combined with Standard Liver Volume. J Gastrointest Surg. 2015;19:1305-1314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 55] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 15. | Truant S, Boleslawski E, Sergent G, Leteurtre E, Duhamel A, Hebbar M, Pruvot FR. Liver function following extended hepatectomy can be accurately predicted using remnant liver volume to body weight ratio. World J Surg. 2015;39:1193-1201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 29] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 16. | Hirata Y, Sanada Y, Urahashi T, Ihara Y, Yamada N, Okada N, Tashiro M, Katano T, Otomo S, Ushijima K. Relationship Between Graft Liver Function and the Change of Graft Liver and Spleen Volumes After Technical Variant Liver Transplantation. Transplant Proc. 2016;48:1105-1109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 17. | Lim MC, Tan CH, Cai J, Zheng J, Kow AW. CT volumetry of the liver: where does it stand in clinical practice? Clin Radiol. 2014;69:887-895. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 93] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 18. | Pomposelli JJ, Tongyoo A, Wald C, Pomfret EA. Variability of standard liver volume estimation versus software-assisted total liver volume measurement. Liver Transpl. 2012;18:1083-1092. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 34] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 19. | Poovathumkadavil A, Leung KF, Al Ghamdi HM, Othman Iel H, Meshikhes AW. Standard formula for liver volume in Middle Eastern Arabic adults. Transplant Proc. 2010;42:3600-3605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 24] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 20. | DeLand FH, North WA. Relationship between liver size and body size. Radiology. 1968;91:1195-1198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 117] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 21. | Mosteller RD. Simplified calculation of body-surface area. N Engl J Med. 1987;317:1098. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1521] [Cited by in RCA: 2012] [Article Influence: 52.9] [Reference Citation Analysis (0)] |
| 22. | Yoshizumi T, Taketomi A, Kayashima H, Yonemura Y, Harada N, Ijichi H, Soejima Y, Nishizaki T, Maehara Y. Estimation of standard liver volume for Japanese adults. Transplant Proc. 2008;40:1456-1460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 23. | Johnson TN, Tucker GT, Tanner MS, Rostami-Hodjegan A. Changes in liver volume from birth to adulthood: a meta-analysis. Liver Transpl. 2005;11:1481-1493. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 237] [Cited by in RCA: 237] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 24. | Lin XZ, Sun YN, Liu YH, Sheu BS, Cheng BN, Chen CY, Tsai HM, Shen CL. Liver volume in patients with or without chronic liver diseases. Hepatogastroenterology. 1998;45:1069-1074. [PubMed] |
| 25. | Chan SC, Liu CL, Lo CM, Lam BK, Lee EW, Wong Y, Fan ST. Estimating liver weight of adults by body weight and gender. World J Gastroenterol. 2006;12:2217-2222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in CrossRef: 55] [Cited by in RCA: 67] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 26. | Yuan D, Lu T, Wei YG, Li B, Yan LN, Zeng Y, Wen TF, Zhao JC. Estimation of standard liver volume for liver transplantation in the Chinese population. Transplant Proc. 2008;40:3536-3540. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 48] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 27. | Fu-Gui L, Lu-Nan Y, Bo L, Yong Z, Tian-Fu W, Ming-Qing X, Wen-Tao W, Zhe-Yu C. Estimation of standard liver volume in Chinese adult living donors. Transplant Proc. 2009;41:4052-4056. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 42] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 28. | Vauthey JN, Abdalla EK, Doherty DA, Gertsch P, Fenstermacher MJ, Loyer EM, Lerut J, Materne R, Wang X, Encarnacion A. Body surface area and body weight predict total liver volume in Western adults. Liver Transpl. 2002;8:233-240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 443] [Cited by in RCA: 464] [Article Influence: 20.2] [Reference Citation Analysis (0)] |
| 29. | Du Bois D, Du Bois EF. A formula to estimate the approximate surface area if height and weight be known. 1916. Nutrition. 1989;5:303-311; discussion 312-313. [PubMed] |
| 30. | Hashimoto T, Sugawara Y, Tamura S, Hasegawa K, Kishi Y, Kokudo N, Makuuchi M. Estimation of standard liver volume in Japanese living liver donors. J Gastroenterol Hepatol. 2006;21:1710-1713. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 52] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 31. | Choukèr A, Martignoni A, Dugas M, Eisenmenger W, Schauer R, Kaufmann I, Schelling G, Löhe F, Jauch KW, Peter K. Estimation of liver size for liver transplantation: the impact of age and gender. Liver Transpl. 2004;10:678-685. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 87] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 32. | Kaneko J, Sugawara Y, Matsui Y, Makuuchi M. Spleen size of live donors for liver transplantation. Surg Radiol Anat. 2008;30:515-518. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 17] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 33. | Loftus WK, Chow LT, Metreweli C. Sonographic measurement of splenic length: correlation with measurement at autopsy. J Clin Ultrasound. 1999;27:71-74. [PubMed] [DOI] [Full Text] |
| 34. | Prassopoulos P, Daskalogiannaki M, Raissaki M, Hatjidakis A, Gourtsoyiannis N. Determination of normal splenic volume on computed tomography in relation to age, gender and body habitus. Eur Radiol. 1997;7:246-248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 177] [Cited by in RCA: 204] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 35. | Zhang QW, Wang Y, Wang J, Zhao HB, Yu H, Liu SY, Zeng X, Chen Q, Hu ZQ, Guo WY. A non-invasive magnetic resonance imaging-based model predicts portal venous pressure. J Dig Dis. 2016;17:175-185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 36. | Stamm ER, Meier JM, Pokharel SS, Clark T, Glueck DH, Lind KE, Roberts KM. Normal main portal vein diameter measured on CT is larger than the widely referenced upper limit of 13 mm. Abdom Radiol (NY). 2016;41:1931-1936. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 17] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 37. | Couinaud C. Surgical anatomy of the liver revisited. Paris, France: Couinaud; 1989; . |
| 38. | Torres WE, Whitmire LF, Gedgaudas-McClees K, Bernardino ME. Computed tomography of hepatic morphologic changes in cirrhosis of the liver. J Comput Assist Tomogr. 1986;10:47-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 88] [Article Influence: 2.3] [Reference Citation Analysis (0)] |