Published online Jun 21, 2017. doi: 10.3748/wjg.v23.i23.4303
Peer-review started: October 10, 2016
First decision: December 19, 2016
Revised: March 21, 2017
Accepted: May 19, 2017
Article in press: May 19, 2017
Published online: June 21, 2017
Processing time: 257 Days and 10.6 Hours
To evaluate if any association existed between the extent of hepatic necrosis in initial liver biopsies and patient survival.
Thirty-seven patients with fulminant liver failure, whose liver biopsy exhibited substantial necrosis, were identified and included in the study. The histological and clinical data was then analyzed in order to assess the relationship between the extent of necrosis and patient survival, with and without liver transplantation. The patients were grouped based on the etiology of hepatic necrosis. Each of the etiology groups were then further stratified according to whether or not they had received a liver transplant post-index biopsy, and whether or not the patient survived.
The core tissue length ranged from 5 to 44 mm with an average of 23 mm. Causes of necrosis included 14 autoimmune hepatitis, 10 drug induced liver injury (DILI), 9 hepatitis virus infection, and 4 unknown origin. Among them, 11 showed submassive (26%-75% of the parenchymal volume) and 26 massive (76%-100%) necrosis. Transplant-free survival was worse in patients with a higher extent of necrosis (40%, 71.4% and 100% in groups with necrosis of 76%-100%, 51%-75% and 26%-50%, respectively). Additionally, transplant-free survival rates were 66.7%, 57.1%, and 25.0% in groups of autoimmune hepatitis, DILI, and viral hepatitis, respectively. Even after liver transplantation, the survival rate in patients as a result of viral hepatitis remained the lowest (80%, 100%, and 40% in groups of autoimmune hepatitis, DILI, and viral hepatitis, respectively).
Adequate liver biopsy with more than 75% necrosis is associated with significant transplant-free mortality that is critical in predicting survival.
Core tip: Fulminant liver failure is clinically characterized by an abrupt onset of jaundice and liver dysfunction with subsequent development of encephalopathy and coagulopathy in patients with or without preexisting liver disease. Liver biopsy may play a role in predicting patient survival, and may also potentially play a role in optimizing the utilization of resources in the setting of fulminant liver failure.
- Citation: Ndekwe P, Ghabril MS, Zang Y, Mann SA, Cummings OW, Lin J. Substantial hepatic necrosis is prognostic in fulminant liver failure. World J Gastroenterol 2017; 23(23): 4303-4310
- URL: https://www.wjgnet.com/1007-9327/full/v23/i23/4303.htm
- DOI: https://dx.doi.org/10.3748/wjg.v23.i23.4303
Fulminant liver failure is clinically characterized by an abrupt onset of jaundice and liver dysfunction with subsequent development of encephalopathy and coagulopathy in patients with or without preexisting liver disease[1-6]. Common etiologies for fulminant liver failure include viral hepatitis, autoimmune hepatitis, and drug induced liver injury (DILI)[7,8]. Other precipitating events comprise alcoholic liver disease, ischemia, portal vein thrombosis, and infection[9-11]. In some cases, a precipitating factor is never identified[9-11]. Regardless of the etiology, fulminant liver failure is typically associated with high morbidity and mortality[1]. In the clinical setting, the grade of encephalopathy has a strong association with prognosis[12]. Other prognostic indicators encompass coagulation factors (INR or Factor V levels), serum bilirubin, transaminases, creatinine, arterial pH, and serum lactate[12]. Additionally, computed tomographic assessment of liver atrophy is said to be of prognostic value[13]. As such, multiple prognostic models (e.g., Clichy, King’s College), based mainly on laboratory values and clinical findings, have been used to rapidly assess the need for transplantation[4,9-12].
Liver biopsy is the gold standard for evaluating hepatic diseases. However, these fulminant liver failure models do not directly taken into account the histopathological findings obtained via liver biopsy. Submassive or massive liver necrosis is the worst histological finding that is seen in association with fulminant liver failure, although it is not seen in every biopsy. In fulminant liver failure, the prognosis for those with significant hepatic necrosis is generally thought to be poor. And yet, the extent of necrosis in a biopsy, and its importance in predicting patient outcomes, is less well defined in the literature[7,14]. One study even casts doubt on the value of hepatic necrosis as a prognostic indicator[7].
In this study, we aimed to evaluate if there is any association between the degree of hepatocellular necrosis and patient survival. Additionally, we attempted to identify any relationship between the underlying etiology of necrosis and survival. Lastly, we evaluated the outcomes of liver transplantation following a histopathological diagnosis of significant hepatic necrosis.
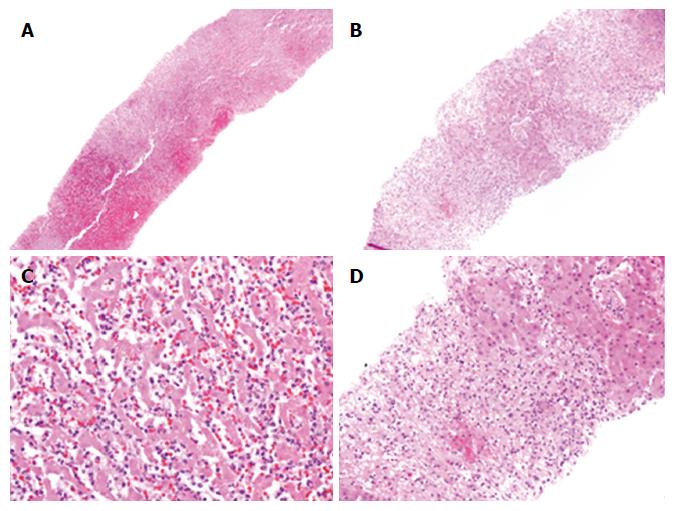
A search of our institution’s pathology database was performed in order to retrospectively identify native liver biopsies with a diagnosis of either submassive or massive hepatic necrosis. Thirty-seven liver biopsies, originally performed from 2004 to 2013, were identified. The biopsies were distributed among 37 individual patients who were clinically diagnosed with fulminant liver failure. Hepatic necrosis is defined as death of hepatocytes, which maybe single cell, multiple cells in piecemeal, focal, multifocal, submassive or massive (Figure 1). Submassive hepatic necrosis is defined as necrosis involving 26%-75% of the parenchymal volume, while massive necrosis involves more than 75%. The percentage of hepatic necrosis is determined based on the total amount of necrotic hepatic tissue present vs the amount of total parenchyma. Hematoxylin and eosin (H&E) slides for each of the individual biopsies were reviewed by an experienced pathologist (Lin J) to assess the percentage of necrosis and other pathologic features.
A review of each individual patient’s electronic medical chart was performed and relevant clinical data was obtained. Collected data included age, gender, etiology of hepatic necrosis, presence of hepatic encephalopathy, whether or not the patient received treatment related to the underlying disease, whether or not liver transplantation was performed after the index liver biopsy, and survival time. Additional clinical information included patient INR values, presence of a bacterial infection, and whether or not ascites was present.
The histological and clinical data was then analyzed in order to assess the relationship between the extent of necrosis and patient survival, with or without liver transplantation. Patients were sorted into three groups based on the percentage of necrosis present within the biopsy (26%-50%, 51%-75%, and 76%-100%). Each of the three percentage groups was then further stratified according to whether or not they had subsequently received a liver transplant.
A separate analysis of all data was then performed in order to assess the relationship between the etiology of hepatic necrosis and patient prognosis, with or without liver transplantation. The patients were grouped based on etiology of hepatic necrosis. Etiologies included autoimmune hepatitis, DILI, viral hepatitis, and unknown. An unknown etiology was defined as any case in which there was no clearly identified cause following an extensive clinical workup. Each of the etiology groups were then further stratified according to whether or not they had received a liver transplant post-index biopsy, and whether or not the patient survived.
Statistical analysis methodologies included Fisher’s exact test and χ2 test. P values of < 0.05 were considered statistically significant. All statistics were performed by an experienced statistician (Zang Y).
The patients within the study ranged in age from 18 to 75 years old with a mean age of 41 years. Two patients were less than 20 years old; 10 were in the 21-30 year old age group, 4 in the 31-40 age group, 7 in the 41-50 age group, 6 in the 51-60 age group, 5 in the 61-70 age group, and 3 patients were older than 70. Fourteen (37.8%) were male and 23 (62.2%) were female.
Tissue adequacy for pathologic assessment was evaluated. Of 37 liver biopsies, the core tissue length ranged from 5 mm to 44 mm with an average of 23 mm. Twenty-three biopsies (62%) were in the length of > 20 mm, 11 (30%) in the range of 10-20 mm , and 3 (8%) < 10 mm.
Causes of submassive or massive liver necrosis included autoimmune hepatitis in 14 patients, DILI in 10 (9 due to acetaminophen and 1 due to clopidogrel), hepatitis virus infection in 9 patients (1 hepatitis A, 5 hepatitis B, 2 hepatitis C, and 1 with both hepatitis B and C), and unknown origin in 4. All patients within the study underwent biopsy with a clinical diagnosis of fulminant liver failure. Survival times for all 37 patients ranged from less than 1 mo to 127 mo according to the last visit record for each patient. The mean survival time was 41 mo.
As shown in Table 1, the single patient with 26-50% necrosis had an INR of 1.34, and no clinical evidence of bacterial infection or ascites. Only 1 of the 10 patients with 51%-75% necrosis had ascites. The mean INR for the patients within this group was 2.19, with individual values ranging from 0.95 to 4.52. None of the patients within this group had evidence of a bacterial infection. Three of the 26 patients with 76%-100% hepatic necrosis had a bacterial infection. The mean INR for patients in this group was 2.64, with individual values ranging from 1.10-5.91. Five of these patients had ascites.
| Extent of necrosis | Patients (n = 37) | Ascites | Bacterial infection | INR mean and range |
| 26%-50% | 1 | 0 (0) | 0 (0) | 1.34 (1.34) |
| 51%-75% | 10 | 1 (10) | 0 (0) | 2.19 (0.95-4.52) |
| 76%-100% | 26 | 5 (19.2) | 3 (11.5) | 2.64 (1.10-5.91) |
Statistical analysis using Fisher exact test demonstrated that there was no significant association between the presence of ascites and extent of necrosis (P = 0.71). Additionally, Fisher’s exact test showed no significant association between the presence of bacterial infection and extent of necrosis (P = 0.58). Analysis of variance showed that there was no significant association between mean INR level and extent of necrosis (P = 0.45).
As shown in Table 2, one patient had 26%-50% hepatic necrosis at the time of biopsy. Ten patients had 51%-75% and 26 patients had 76%-100% necrosis. No bridging fibrosis or cirrhosis was appreciated in any of them. The patient within the 26%-50% group did not receive a transplant and is currently still living well with a followup of 86 mo. Out of the 10 patients with 51%-75% necrosis, 3 received a liver transplant and are still alive (100%) with a mean followup of 86 mo (range, 66-103 mo). Within this group, 5 of the 7 who did not receive a transplant are currently still living (71.4%) with a mean followup of 72 mo (range, 21-127 mo) and 2 died (both < 1 mo after the index liver biopsy). Within the 76%-100% necrosis group, 11 underwent liver transplantation; of these, 7 are still alive (63.6%) and 4 died. Of the 15 transplant-free patients within this group, 6 survived (40%) with a mean followup of 65 mo (range, 28-122 mo) and 9 died (mean, 3 mo; range, 1-14 mo after the index biopsy).
| Extent of necrosis | Patients (n = 37) | Received transplant (n = 14) | Transplant free (n = 23) | ||
| Died | Survived | Died | Survived | ||
| 26%-50% | 1 | NA | NA | NA | 1 (100) |
| 51%-75% | 10 | NA | 3 (100) | 2 (28.6) | 5 (71.4) |
| 76%-100% | 26 | 4 (36.4) | 7 (63.6) | 9 (60.0) | 6 (40.0) |
In summary, transplant-free survival appeared worse in patients with a higher extent of necrosis (40%, 71.4% and 100% in groups with necrosis of 76%-100%, 51%-75% and 26%-50%, respectively). Although higher-extent hepatic necrosis appeared to be associated with worse prognosis, statistically there was no significance between the submassive and the massive necrosis groups (P > 0.05).
Liver transplantation improved patient survival. The patients who received liver transplantation appeared to have somewhat better survival rates compared with non-transplanted patients (100% vs 71.4% and 63.6% vs 40.0% in 51%-75% and 76%-100% necrosis groups, respectively). However, statistical analysis using Fisher’s exact test showed no significant difference in the survival rates of patients within the transplanted and non-transplanted groups, probably due to a small sample size.
Further analysis based upon the etiology of substantial hepatic necrosis, transplantation status, and survival was shown in Table 3. For the 10 cases of drug induced hepatic necrosis, only 3 were transplanted and all of them survived (100%). Four of the 7 who did not receive a transplant survived (57.1%). Overall survival rates for DILI group were not statistically different, depending on transplantation status (P = 0.475).
| Etiology | Patients (n = 37) | Received transplant (n = 14) | Transplant free (n = 23) | ||
| Died | Survived | Died | Survived | ||
| DILI | 10 | NA | 3 (100) | 3 (42.9) | 4 (57.1) |
| AIH | 14 | 1 (20.0) | 4 (80.0) | 3 (33.3) | 6 (66.7) |
| Viral hepatitis | 9 | 3 (60.0) | 2 (40.0) | 3 (75.0) | 1 (25.0) |
| Unknown | 4 | NA | 1 (100) | 2 (66.7) | 1 (33.3) |
Of the 14 cases due to autoimmune hepatitis, 5 underwent liver transplantation and 4 patients survived (80.0%). Six of the 9 patients with autoimmune hepatitis who did not receive transplant survived (66.7%).Overall survival rates were not significantly different, depending on transplantation status (P = 1).
Five patients within the viral hepatitis group underwent transplantation and only 2 survived (40.0%). In comparison, only 1 of the 4 viral hepatitis patients survived without transplantation (25.0%). Although the overall survival rate was higher in the transplant group, there was no statistical significance (P = 1).
For the 4 cases of unknown hepatic necrosis, only 1 patient was transplanted. This patient survived. One of the 3 who did not receive a transplant survived. Overall survival rates for the unknown group with or without transplantation were 100% and 33.3%, respectively. Although transplant group had higher survival rate, there was no statistical significance (P = 1).
In summary, transplant-free survival rates were 66.7%, 57.1%, and 25.0% in groups of autoimmune hepatitis, DILI, and viral hepatitis, respectively. Although the survival rates appeared different among the various etiology groups, a statistically significant difference only existed between autoimmune hepatitis and viral hepatitis groups (P = 0.048). Even after liver transplantation, the survival rate in patients as a result of viral hepatitis remained the lowest when compared with the other groups, although no statistical significance has been reached between DILI and viral hepatitis (P = 0.058 or 0.090), or between DILI and autoimmune hepatitis (P = 0.116 or 0.408) in the setting of transplant or transplant-free, respectively.
As demonstrated in Table 4, the patient within 26%-50% necrosis group did not have encephalopathy; nor did any of the patients within 51%-75% group. Five patients within 76%-100% group had encephalopathy (19.2%). Thus, it appears that a higher extent of liver necrosis is possibly associated with encephalopathy. Further analysis of the patients who had encephalopathy revealed that the sole surviving patient (10%) within this group underwent liver transplantation, with a followup time of 92 mo. This finding was statistically significant when compared to the transplant-free group (57.1%, P < 0.05).
| Extent of necrosis | Patient number (n = 37) | Encephalopathy | |
| Present (n = 5) | Absent (n = 32) | ||
| 26%-50% | 1 | 0 | 1 (100) |
| 51%-75% | 10 | 0 | 10 (100) |
| 76%-100% | 26 | 5 (19.2) | 21 (80.8) |
Of the 21 patients in 76%-100% necrosis group without encephalopathy, 10 underwent transplantation, and the survival rate was statistically significant (60.0%) when compared to the survival rate of 54.5% in those who did not undergo transplantation (P < 0.05). Encephalopathy is an important prognostic predictor. The survival rate for transplant-free patients with encephalopathy was much lower compared with the group without encephalopathy (0% vs 54.5%; P < 0.05).
Studies addressing the prognostic value of liver biopsies with substantial necrosis are rare, and the conclusions are not well defined in the literature[14,15]. Hanau and colleagues questioned the value of hepatic necrosis in predicting clinical outcome, because about 50% of the biopsies in their study showed minimal bridging necrosis[7]. In their 1995 study, patients were selected based solely on their clinical characteristics (e.g., signs and symptoms of fulminant liver failure with elevated liver function tests).In contrast, we selected and stratified our study cohorts based on the extent of necrosis in the liver biopsies. Although Hanau’s study included 38 cases, only 12 liver biopsies demonstrated either > 90% (3) or 10%-90% (9) necrosis. Additionally, Hanau and colleagues found that only one of seven (14.3%) patients whose liver biopsy demonstrated ≥ 70% necrosis survived without transplantation, keeping in line with our finding. In another study in 1993, Donaldson and colleagues found that only 2 of 19 patients (10.5%) with > 70% necrosis survived without transplantation[14]. These findings indicate that the percentage of hepatic necrosis may be an important prognosticator for patient survival. As noted, our transplant-free survival rates are much higher with 71.4% and 40% for 51%-75% and > 75% necrosis, respectively. A possible explanation for the difference in transplant-free survival might be related to the different therapeutic options utilized in the respective study cohorts. It seems likely that some more effective non-transplant related treatments were available for the patients in our study; as the two aforementioned studies took place more than two decades ago. Since then, it appears that no report has been added in the literature in the regard of prognostic value of liver biopsy in an advantaged era of liver transplantation for the past 20 years. To the best of our knowledge, our study is the largest ever to address whether or not there is an association between substantial hepatic necrosis and prognosis (11 with 26%-75% and 26 with > 75% necrosis)[7,14]. Despite a difference in approaches between our study, the Donaldson study, and the Hanau study, a similar trend seems to be present; as the degree of hepatic necrosis increases, the transplant-free survival rate declines. However, the statistical significance of this trend is still not readily apparent, and more studies are certainly warranted.
Adequacy is an important matter to consider, given the well-known fact that necrosis is often heterogeneously distributed throughout the liver[7]. The mean core tissue length of 23 mm in our study and 21 mm in Donaldson’s[14] study are both adequate. Specimen adequacy is not mentioned in Hanau’s study[7]. Inadequate biopsy specimens, localized liver necrosis[7], and a prolonged interval between the time of symptoms and biopsy, are the most common causes of a discrepancy between the extent of necrosis in a liver biopsy when compared to hepatectomy specimens from the same patient (our unpublished data). Therefore, if a liver biopsy is going to be obtained, it is best obtained from a patient where diffuse hepatic necrosis is suspected; provided that the biopsy will be adequate and is taken as soon as possible following the onset of symptoms. Localized liver necrosis due to ischemia or other injury can be feasibly monitored by CT/MRI imaging, and the interpretation of the biopsy should be considered as a local event.
Importantly, our study has indicated that there may be association between etiology and patient survival in the setting of submassive or massive necrosis, which has not been discussed in the prior reports[7,14,15]. In our study, survival was the worst in those with hepatotropic viral hepatitis as the underlying etiology, regardless of the status of liver transplantation. Patients with autoimmune hepatitis induced hepatic necrosis had the best transplant-free survival and those with DILI had the best survival after transplantation. It is not entirely clear why different causes may lead to different survival from our study. One might speculate that differences in patient age, availability of effective therapeutic options, or preexisting co-morbidities might play a role in prognosis. In our study, the median age for those with massive hepatic necrosis was 49, 43, 48, and 44 years in autoimmune hepatitis, DILI, viral hepatitis, and unknown groups, respectively (Supplement 1). This finding demonstrates a lack of correlation between age and prognosis in the setting of substantial hepatic necrosis, although age has been suggested as playing a role in Hanau’s study[7]. In our study, the autoimmune hepatitis group had the greatest median age, and yet had the best overall survival . It is likely that effective therapeutic agents in autoimmune hepatitis might play a role in explaining why transplant-free survival is better when compared with other etiologies. However, due to the small number of cases in each of the substratified groups, no definitive conclusions can be drawn and further investigation seems warranted.
Bacterial infections and ascites were present more frequently in patients with a higher extent of hepatic necrosis. Mean INR for the patients with higher percentages of hepatic necrosis were also higher than in patients with a smaller percentage of necrosis. However none of these trends were found to be statistically significant. It is likely that a larger study may be able to identify a statistically significant association between these individual parameters.
Hepatic encephalopathy is present more frequently in the patients with massive necrosis. However, the incidence seems low in our study (19.2%). The relatively low incidence of encephalopathy might reflect the characteristics of the study cohort in our institution. The lack of a clear statistically significant association between extent of necrosis and encephalopathy is likely due to the relatively low number of patients in our study. In patients with hepatic encephalopathy and massive necrosis, the prognosis is extremely miserable. The only patient with encephalopathy who survived received a liver transplant. This finding suggests that encephalopathy due to hepatic necrosis may be associated with increased mortality. It also suggests that liver transplantation may be useful in this setting[16-20].
In conclusion, accurate histopathological evaluation in patients with fulminant liver failure is useful. However, more research with a larger number of patients is required to truly identify any significant associations between the extent of hepatic necrosis and prognosis. The significance of liver biopsy is not limited to identifying or confirming the etiology; it is also a valuable tool in the assessment of prognosis and management decisions in regard to liver transplantation. As demonstrated, the percentage of liver necrosis in an adequate liver biopsy is a prognostic indicator of survival. More than 75% hepatic necrosis is associated with substantial transplant-free mortality, thus massive hepatic necrosis is worth considering as an indicator for liver transplantation. Importantly, survival is associated with etiology with the worst in those with hepatotropic viral hepatitis even after liver transplantation. Taken together, assessing the extent of hepatic necrosis and its underlying etiology can aid in screening candidates who may benefit most from liver transplantation, a lifesaving but expensive and high risk procedure. Early identification of transplant candidates is critical in optimizing the utilization of resources.
Patients with fulminant hepatic failure often receive liver biopsies as part of the clinical work-up. In many instances, extensive hepatic necrosis is identified. The significance of extensive hepatic necrosis within a liver biopsy, as it relates to patient prognosis or treatment decisions, has not been well described.
To our knowledge, no new studies addressing the significance of biopsy proven hepatic necrosis as it relates to patient prognosis have been published for over twenty years. The objective of our study was to identify what associations if any exist between hepatic necrosis, patient clinical characteristics, and survival.
This study shows trends suggesting that the extent of hepatic necrosis is associated with poorer patient survival. Further, we noticed a trend that patients who undergo liver transplantation tend to have a longer survival time. Additionally, higher extents of hepatic necrosis typically showed trends with clinical factors such as higher mean INR, and increased frequency of ascites or bacterial infections. While these trends all seemed to be present within our study, no statistical significance was identified, likely due to the small size of our study (in spite of us having the largest number of cases to date).
The trends evident within our study may provide future investigators with a starting point for their inquiries into how hepatic necrosis may play a role in patient management.
Fulminant liver failure is clinically characterized by an abrupt onset of jaundice and liver dysfunction with subsequent development of encephalopathy and coagulopathy in patients with or without preexisting liver disease. Hepatic necrosis is defined as death of hepatocytes, which maybe single cell, multiple cells in piecemeal, focal, multifocal, submassive or massive. Submassive hepatic necrosis is defined as necrosis involving 26%-75% of the parenchymal volume, while massive necrosis involves more than 75%.
This paper evaluated if any association existed between the extent of hepatic necrosis and patient survival through observing the data resulted from 37 patients with fulminant liver failure, whose liver biopsy exhibited substantial necrosis. It was found that transplant-free survival was worse in patients with a higher extent of necrosis (40%, 71.4% and 100% in groups with necrosis of 76%-100%, 51%-75% and 26%-50%, respectively). So, the author concluded that adequate liver biopsy with more than 75% necrosis is associated with significant transplant-free mortality that is critical in predicting survival. This study has some scientific and clinic significances.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Gong ZJ S- Editor: Gong ZM L- Editor: A E- Editor: Zhang FF
| 1. | Shakil AO, Kramer D, Mazariegos GV, Fung JJ, Rakela J. Acute liver failure: clinical features, outcome analysis, and applicability of prognostic criteria. Liver Transpl. 2000;6:163-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 51] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 2. | Singhal A, Vadlamudi S, Stokes K, Cassidy FP, Corn A, Shrago SS, Wright HI, Kohli V. Liver histology as predictor of outcome in patients with acute liver failure. Transpl Int. 2012;25:658-662. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 3. | Sugawara K, Nakayama N, Mochida S. Acute liver failure in Japan: definition, classification, and prediction of the outcome. J Gastroenterol. 2012;47:849-861. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 108] [Cited by in RCA: 109] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 4. | Arroyo V, Moreau R, Jalan R, Ginès P; EASL-CLIF Consortium CANONIC Study. Acute-on-chronic liver failure: A new syndrome that will re-classify cirrhosis. J Hepatol. 2015;62:S131-S143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 298] [Cited by in RCA: 306] [Article Influence: 30.6] [Reference Citation Analysis (0)] |
| 5. | Wlodzimirow K, Abu-Hanna A, Chamuleau RA. Acute-on-chronic liver failure - its definition remains unclear. J Hepatol. 2013;59:190-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Wlodzimirow KA, Eslami S, Abu-Hanna A, Nieuwoudt M, Chamuleau RA. A systematic review on prognostic indicators of acute on chronic liver failure and their predictive value for mortality. Liver Int. 2013;33:40-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 125] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 7. | Hanau C, Munoz SJ, Rubin R. Histopathological heterogeneity in fulminant hepatic failure. Hepatology. 1995;21:345-351. [PubMed] |
| 8. | Kessler WR, Cummings OW, Eckert G, Chalasani N, Lumeng L, Kwo PY. Fulminant hepatic failure as the initial presentation of acute autoimmune hepatitis. Clin Gastroenterol Hepatol. 2004;2:625-631. [PubMed] |
| 9. | Jalan R, Gines P, Olson JC, Mookerjee RP, Moreau R, Garcia-Tsao G, Arroyo V, Kamath PS. Acute-on chronic liver failure. J Hepatol. 2012;57:1336-1348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 447] [Cited by in RCA: 457] [Article Influence: 35.2] [Reference Citation Analysis (1)] |
| 10. | Jalan R, Gines P, Olson JC, Mookerjee RP, Moreau R, Garcia-Tsao G, Arroyo V, Kamath PS. Reply to: “Acute-on-chronic liver failure - its definition remains unclear”. J Hepatol. 2013;59:191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Jalan R, Mookerjee RP. Acute-on-chronic liver failure: an early biopsy is essential? Gut. 2010;59:1455-1456. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 12. | O’Grady J. Modern management of acute liver failure. Clin Liver Dis. 2007;11:291-303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 31] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 13. | Yamagishi Y, Saito H, Tada S, Horie Y, Kato S, Ishii H, Shimojima N, Haga J, Shimazu M, Kitajima M. Value of computed tomography-derived estimated liver volume/standard liver volume ratio for predicting the prognosis of adult fulminant hepatic failure in Japan. J Gastroenterol Hepatol. 2005;20:1843-1849. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 14. | Donaldson BW, Gopinath R, Wanless IR, Phillips MJ, Cameron R, Roberts EA, Greig PD, Levy G, Blendis LM. The role of transjugular liver biopsy in fulminant liver failure: relation to other prognostic indicators. Hepatology. 1993;18:1370-1376. [PubMed] |
| 15. | Kirsch R, Yap J, Roberts EA, Cutz E. Clinicopathologic spectrum of massive and submassive hepatic necrosis in infants and children. Hum Pathol. 2009;40:516-526. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 16. | Chan AC, Fan ST, Lo CM, Liu CL, Chan SC, Ng KK, Yong BH, Chiu A, Lam BK. Liver transplantation for acute-on-chronic liver failure. Hepatol Int. 2009;3:571-581. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 112] [Cited by in RCA: 104] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 17. | Duan BW, Lu SC, Wang ML, Liu JN, Chi P, Lai W, Wu JS, Guo QL, Lin DD, Liu Y. Liver transplantation in acute-on-chronic liver failure patients with high model for end-stage liver disease (MELD) scores: a single center experience of 100 consecutive cases. J Surg Res. 2013;183:936-943. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 52] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 18. | Farmer DG, Anselmo DM, Ghobrial RM, Yersiz H, McDiarmid SV, Cao C, Weaver M, Figueroa J, Khan K, Vargas J. Liver transplantation for fulminant hepatic failure: experience with more than 200 patients over a 17-year period. Ann Surg. 2003;237:666-675; discussion 675-676. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 112] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 19. | Gotthardt D, Riediger C, Weiss KH, Encke J, Schemmer P, Schmidt J, Sauer P. Fulminant hepatic failure: etiology and indications for liver transplantation. Nephrol Dial Transplant. 2007;22 Suppl 8:viii5-viii8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 54] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 20. | Ostapowicz G, Fontana RJ, Schiødt FV, Larson A, Davern TJ, Han SH, McCashland TM, Shakil AO, Hay JE, Hynan L. Results of a prospective study of acute liver failure at 17 tertiary care centers in the United States. Ann Intern Med. 2002;137:947-954. [PubMed] |