Published online May 28, 2017. doi: 10.3748/wjg.v23.i20.3758
Peer-review started: November 21, 2016
First decision: February 10, 2017
Revised: March 10, 2017
Accepted: April 12, 2017
Article in press: April 12, 2017
Published online: May 28, 2017
Processing time: 190 Days and 0.9 Hours
Chronic abdominal and pelvic pain is a common condition that has significant impact on quality of life, and causes billions of dollars in direct and indirect costs. Emerging data suggest that transcranial direct current stimulation (tDCS), alone or in combination with transcutaneous electrical nerve stimulation (TENS), could be a promising therapeutic avenue to reduce chronic pain. The encouraging results coming from these studies prompted us to try combining TENS and tDCS in 4 of our patients who suffered from chronic abdominal/pelvic pain and to compare the effect with 5 other patients who received TENS alone. Pain intensity was assessed with a visual analog scale before, during and after the stimulation. We observed that there was a slight decrease in pain which was similar in both patient groups (TENS alone and TENS combined with tDCS). These observations suggest that combining TENS and tDCS in patients suffering from chronic pelvic and/or abdominal pain produces no additional benefit, compared to TENS alone. Future studies, looking at the effect of several/consecutive TENS and tDCS sessions should be conducted.
Core tip: Past studies have showed that combining transcutaneous electrical nerve stimulation (TENS) and transcranial direct current stimulation (tDCS) can be an effective strategy to relieve chronic pain. In this letter, we describe the observations made on nine patients suffering from chronic pelvic and/or abdominal pain. Combining TENS and tDCS produced negligible effect on pain. The reduction in pain noted after the application of TENS and tDCS was comparable to the reduction noted after the application of TENS only. These clinical observations question the added value of tDCS in patients suffering from chronic pelvic and abdominal pain.
- Citation: Harvey MP, Watier A, Dufort Rouleau É, Léonard G. Non-invasive stimulation techniques to relieve abdominal/pelvic pain: Is more always better? World J Gastroenterol 2017; 23(20): 3758-3760
- URL: https://www.wjgnet.com/1007-9327/full/v23/i20/3758.htm
- DOI: https://dx.doi.org/10.3748/wjg.v23.i20.3758
Chronic pelvic pain syndrome is quite prevalent and disabling, and should definitely receive more attention[1]. Abnormalities in the brain-gut axis play an important role in functional gastro-intestinal disorders, suggesting that brain modulation can be a part of the solution to relieve visceral pain, such as pelvic and abdominal pain[2]. Over the last few years, two studies looking into the usefulness of brain stimulation techniques to reduce chronic abdominal and pelvic pain syndromes were published. The first article, published by Fenton et al[3], looked into the safety and efficacy of transcranial direct current stimulation (tDCS) in patients suffering from refractory chronic pelvic pain. Then, a few years later, Schabrun et al[4] published a study in which they suggested that combining tDCS to transcutaneous electrical nerve stimulation (TENS) could be more effective to reduce pain than tDCS or TENS alone. TENS is a modality that is frequently used with our patients. Although the outcomes are generally good, some patients report no significant benefit following TENS application. The results reported by Schabrun et al[4] prompted us to try combining TENS and tDCS in our patients who suffered from chronic abdominal and/or pelvic pain and who failed standard pharmacological/surgical therapies.
Patients were randomly allocated to TENS alone (n = 5) or TENS combined with tDCS (n = 4) using a random numbers table with a ratio of 1: 1, based on their order of entry in the trial. All patients (mean age 43 ± 10 years old) were medicated for their pain (8 with opioids, 5 with cannabinoids, 5 with anticonvulsants, and 1 with tricyclic antidepressants; note that every patient had at least two medications). They were asked to keep their medication stable at least 1 mo before receiving the neurostimulation treatments. There was no difference between the 2 treatment groups regarding the age and medical diagnosis, although the proportion of women tended to be higher in the TENS-only group. For both groups, TENS was delivered using 2 pairs of rubber silicone electrodes connected to a digital Eclipse Plus apparatus (Empi, St. Paul, Minnesota). Two electrodes were placed on the lower lumbar or abdominal region and two other electrodes were placed over the right tibial nerve, in order to target the painful area (directly or via the associated dermatome)[5]. TENS frequency was set at 3 Hz and the pulse duration at 400 ms, and the intensity was adjusted to produce strong and painful sensations[5,6]. For the TENS + tDCS group, a 2 mA direct current was transferred to the patients, through the scalp, by a saline-soaked pair of surface sponge electrodes (5 cm × 7 cm) and delivered by a constant current stimulator, battery-driven, 1 × 1 tDCS device (Model 1300-A; Soterix Medical Inc, New York). Patients received anodal stimulation of the primary motor cortex (M1), as suggested by Fenton et al[3] and by Schabrun et al[4]. The anodal electrode was placed over M1, contralateral to the most painful site (C3 or C4 according to the electroencephalogram 10/20 system), and the cathodal electrode was placed on the supraorbital area contralateral to the anode[3,7]. Both TENS and tDCS were applied for 30 min. Patients who received TENS + tDCS received both stimulations simultaneously. Pain intensity was assessed 4 times during the patients’ visit (before, during, after and 15 min following the treatment) using a visual analog scale (VAS) of 10 cm ranges from “no pain” (0 cm) to “the worst imaginable pain” (10 cm). The study was approved by the local institutional ethics committee and written informed consent was obtained from all patients.
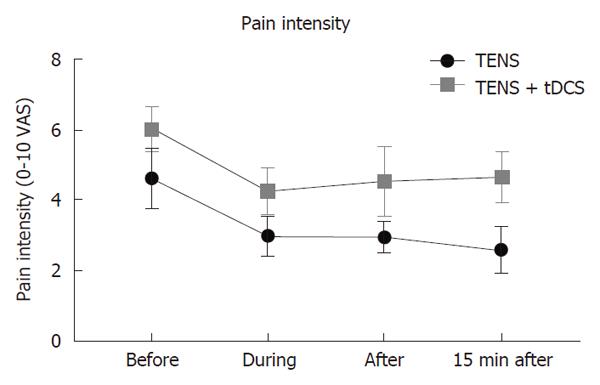
As can be seen in Figure 1, there was a slight decrease in pain during treatment; however the pain reduction was not clinically significant and was similar between both groups (average reduction of 1.6 in the TENS group and 1.8 in the TENS+tDCS group)[8]. Pain intensity continued to slightly decrease and barely reached clinical significance (2 points on VAS) 15 min after stimulation in the TENS group[8].
These results somewhat contrast with those of Schabrun et al[4] who observed a decrease 2.5 in the pain severity score after TENS alone and a decrease of 2.8 after combined TENS and tDCS, a change that was both statistically and clinically significant[8]. The inconsistencies between our observations and those of Schabrun et al[4] could be explained by the different populations studied (chronic low back pain vs chronic abdominal/pelvic pain). It is also important to mention that the beneficial effect of TENS+tDCS noted by Schabrun et al[4] was observed in a subsample of patients only (i.e., in individuals with more pronounced pain sensitization). Different results could have perhaps been obtained if we had included solely chronic abdominal/pelvic pain patients with increased pain sensitization. Furthermore, it should be noted that the effects noted in our patients were observed after one single session of neurostimulation. Providing chronic pain patients with only one tDCS session is perhaps not sufficient to drive important and long-lasting changes in symptoms. Finally, it should be pointed out that 8 of our 9 patients took opioids on a regular basis, a medication that is known to have a negative effect on the reaction to low frequency TENS[9].
In conclusion, our observations suggest that one session of TENS, alone or in combination with tDCS, can slightly reduce pain in patients suffering from chronic abdominal or pelvic pain. However, combining TENS with tDCS does not seem to provide any additional benefit. Contrary to TENS, which can be self-administered by patients at home during their everyday activities, tDCS must be administered by a healthcare professional. Future studies, looking at the effect of several/consecutive TENS and tDCS sessions should be conducted.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Canada
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Thota PN, Kraja B, Rubbini M S- Editor: Qi Y L- Editor: A E- Editor: Wang CH
| 1. | Chiarioni G, Asteria C, Whitehead WE. Chronic proctalgia and chronic pelvic pain syndromes: new etiologic insights and treatment options. World J Gastroenterol. 2011;17:4447-4455. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 62] [Cited by in RCA: 37] [Article Influence: 2.6] [Reference Citation Analysis (1)] |
| 2. | Sharma A, Lelic D, Brock C, Paine P, Aziz Q. New technologies to investigate the brain-gut axis. World J Gastroenterol. 2009;15:182-191. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 35] [Cited by in RCA: 32] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 3. | Fenton BW, Palmieri PA, Boggio P, Fanning J, Fregni F. A preliminary study of transcranial direct current stimulation for the treatment of refractory chronic pelvic pain. Brain Stimul. 2009;2:103-107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 77] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 4. | Schabrun SM, Jones E, Elgueta Cancino EL, Hodges PW. Targeting chronic recurrent low back pain from the top-down and the bottom-up: a combined transcranial direct current stimulation and peripheral electrical stimulation intervention. Brain Stimul. 2014;7:451-459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 108] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 5. | Istek A, Gungor Ugurlucan F, Yasa C, Gokyildiz S, Yalcin O. Randomized trial of long-term effects of percutaneous tibial nerve stimulation on chronic pelvic pain. Arch Gynecol Obstet. 2014;290:291-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 30] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 6. | Gokyildiz S, Kizilkaya Beji N, Yalcin O, Istek A. Effects of percutaneous tibial nerve stimulation therapy on chronic pelvic pain. Gynecol Obstet Invest. 2012;73:99-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 42] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 7. | Antal A, Terney D, Kühnl S, Paulus W. Anodal transcranial direct current stimulation of the motor cortex ameliorates chronic pain and reduces short intracortical inhibition. J Pain Symptom Manage. 2010;39:890-903. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 257] [Cited by in RCA: 236] [Article Influence: 15.7] [Reference Citation Analysis (0)] |
| 8. | Farrar JT, Portenoy RK, Berlin JA, Kinman JL, Strom BL. Defining the clinically important difference in pain outcome measures. Pain. 2000;88:287-294. [PubMed] |
| 9. | Léonard G, Cloutier C, Marchand S. Reduced analgesic effect of acupuncture-like TENS but not conventional TENS in opioid-treated patients. J Pain. 2011;12:213-221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 40] [Article Influence: 2.7] [Reference Citation Analysis (0)] |