Published online Mar 14, 2017. doi: 10.3748/wjg.v23.i10.1851
Peer-review started: September 28, 2016
First decision: October 20, 2016
Revised: November 10, 2016
Accepted: January 17, 2017
Article in press: January 17, 2017
Published online: March 14, 2017
Processing time: 172 Days and 4.1 Hours
To assess the feasibility and effectiveness of a novel application of percutaneous intraductal radiofrequency (RF) for the treatment of biliary stent obstruction.
We specifically report a retrospective study presenting the results of percutaneous intraductal RF in patients with biliary stent occlusion. A total of 43 cases involving biliary stent obstruction were treated by placing an EndoHPB catheter and percutaneous intraductal RF was performed to clean stents. The stent patency was evaluated by cholangiography and follow-up by contrast enhanced computed tomography or ultrasound after the removal of the drainage catheter.
Following the procedures, of the 43 patients, 40 survived and 3 died with a median survival of 80.5 (range: 30-243) d. One patient was lost to follow-up. One patient had the stent patent at the time of last follow-up. Two patients with stent blockage at 35 d and 44 d after procedure underwent percutaneous transhepatic drain insertion only. The levels of bilirubin before and after the procedure were 128 ± 65 μmol/L and 63 ± 29 μmol/L, respectively. There were no related complications (haemorrhage, bile duct perforation, bile leak or pancreatitis) and all patients’ stent patency was confirmed by cholangiography after the procedure, with a median patency time of 107 (range: 12-180) d.
This preliminary clinical study demonstrated that percutaneous intraductal RF is safe and effective for the treatment of biliary stent obstruction, increasing the duration of stent patency, although randomized controlled trials are needed to confirm the effectiveness of this approach.
Core tip: This study sought to assess the feasibility and effectiveness of a novel application of percutaneous radiofrequency ablation in the treatment of biliary stent obstruction. We report a retrospective study with the results of percutaneous intraductal radiofrequency ablation in patients with biliary stent occlusion.
- Citation: Xia N, Gong J, Lu J, Chen ZJ, Zhang LY, Wang ZM. Percutaneous intraductal radiofrequency ablation for treatment of biliary stent occlusion: A preliminary result. World J Gastroenterol 2017; 23(10): 1851-1856
- URL: https://www.wjgnet.com/1007-9327/full/v23/i10/1851.htm
- DOI: https://dx.doi.org/10.3748/wjg.v23.i10.1851
The use of biliary self-expanding metallic stents (SEMSs) is an effective method for treating malignant biliary obstruction. However, with excessive tumor growth, tumor ingrowth, epithelial hyperplasia, biological film deposition and biliary sludge formation, the patency time of SEMSs is approximately 120 d[1]. The current management approaches for occluded SEMSs include mechanical cleaning and the insertion of a second stent (a covered SEMS, uncovered SEMS or plastic stent) via an endoscopic or percutaneous approach[2].
Recently, numerous clinical reports have demonstrated the safety and efficacy of using a novel radiofrequency (RF) ablation (RFA) catheter for endoscopic palliative procedures[3,4]. There is a clinical need for an effective method of re-opening biliary stents that accounts for the limitations of an endoscope, particularly in cases involving hepatic hilar tumors or after gastrointestinal operations. Therefore, our research group investigated the treatment of biliary stent occlusion by percutaneous biliary RF.
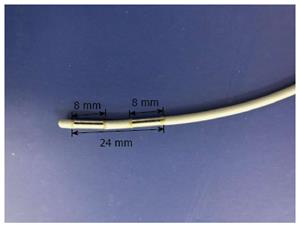
The Habib EndoHPB RF catheter for bipolar RFA (EMcision, United States) has a bipolar RF probe diameter of 8 Fr (2.6 mm), a length of 1.8 m, and a distance of 0.035 (COOK, United States) that allows to pass over a guide wire. The catheter has two ring electrodes separated by a distance of 8 mm and a leading edge that extends 5 mm beyond the distal electrode, and it can produce focal coagulation necrosis with a long diameter of more than 2.5 cm (Figure 1). This catheter can be used in the treatment of intraductal RF.
From July 2012 to March 2014, 43 patients with malignant biliary obstruction were recruited to this study. These patients underwent biliary stent (SEMSs, length 6-8 cm, diameter 1 cm, BARD, United States) treatment by percutaneous puncture (n = 24; stent patency range: 72-145 d) or endoscopic retrograde cholangiopancreatography (n = 19; stent patency range: 69-139 d). After treatment, the patients had fever, jaundice or symptoms of abdominal pain again (15-110 d). All patients underwent evaluation by CT or ultrasound to confirmed the proximal stent dilatation of the bile duct, an assessment of biliary stent occlusion, and dilatation of the intrahepatic bile duct, and routine preoperative examinations (routine blood parameters, liver function, renal function, and blood coagulation function). There were 24 cases of pancreatic carcinoma, 8 cases of bile duct carcinoma, 6 cases of hepatocellular carcinoma, and 5 cases of gallbladder cancer. The mean of patients’ ages was 62 (47-82) years, and the male:female ratio was 26:17. Severe coagulopathy, heart failure and cardiac pacemaker implantation were contraindications for the procedures of this study. All patients signed an informed consent form before undergoing these procedures, which were approved by the relevant ethics committee.
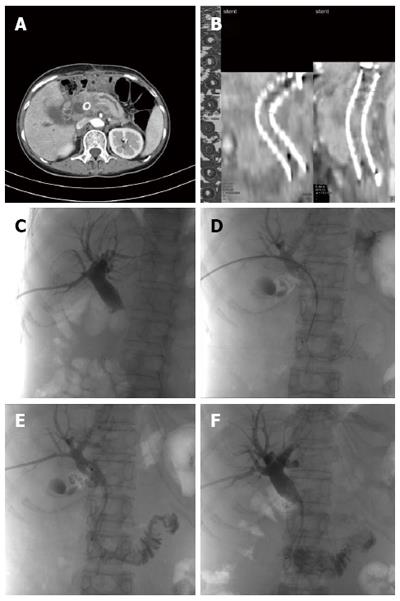
An Innova 3100 DSA (GE, United States) system was used for image-guided applications. A RITA 1500X RF generator (AngioDynamics, United States) was used for energy output. Under DSA guidance, contrast agent was injected into the bile duct, and the length of the stenosis was accurately determined by cholangiography. Using a guidewire technique, the catheter (C3 COOK, United States) was positioned in the area of the occlusion. In cases of complete biliary occlusion, it was necessary to form the guide wire into a loop using vascular catheters and a 5 Fr sheath (Terumo Japan) for support before passing the wire through the occlusion. If the 0.035 guide wire (Terumo Japan) remained unable to pass through the obstruction, the 0.018 guidewire (Boston, United States) was used. The location of the RF catheter was confirmed to avoid contact with the intestine. The RF generator was then connected using the following parameters: a frequency of 400 KHz, a power of 710 W, the mean ablation time of 90 s (range from 60 to 120 s), a stop time of 60 s, and a total output energy of 1200-3600 J (Figure 2). The ablation procedure was repeated 2 to 3 times across the length of the obstruction, and the catheter was removed simultaneously (Table 1).
| Ablation time (s) | 90 (62-150) |
| Ablation repeats | 3 (2-5) |
| Ablation energy (J) | 2474 (1200-3600) |
| Stenosis length (mm) | 35 (20-55) |
The RFA catheter was then withdrawn. A drainage tube was implanted, stent patency was confirmed by angiography, and the bile duct was flushed with 0.9% saline to avoid stents restenosis. The indwelling drainage tube was removed 2-3 d after the operation, after which biliary stent patency was reconfirmed by cholangiography and the tract was plugged.
All patients underwent routine blood tests, liver and kidney function assessments, and determinations of serum amylase and C-reactive protein (CRP). And relevant data were recorded. Biliary tract dilatation was determined by CT, and biliary stent stenosis measurements, the number of ablations, and the ablation power output were recorded. The indwelling biliary drainage tube was removed 2 d after the procedures, and the tract was plugged with a gelatin sponge to prevent bile leakage into the peritoneal cavity. During the first week of follow-up, the patients were subjected to liver function tests and determinations of serum amylase and CRP. At 2 or 3 wk of follow-up, the patients were examined either as outpatients or during hospitalization, and liver function and bilirubin concentration changes were recorded. Ultrasound or low-dose CT was also performed to evaluate biliary tract dilatation, and survival times were recorded. Additionally, stent patency was evaluated by ultrasound or CT scan, with continuous bilirubin increase or pneumobilia considered to indicate stent obstruction.
All study data were analyzed using SPSS 17.0 and GraphPad Prism 5 statistical software. The data are expressed as the median (range) or mean (± SD). Measurement and count data were evaluated using t-tests and χ2 tests, respectively. P < 0.05 was regarded as statistically significant.
All patients underwent successful intraductal RF in the stents, and cholangiography was performed to ensure stent patency after the procedure. The indwelling drainage tube was retained for 7 d after procedures in 2 cases, because of necrosis and cholestasis after procedure, and in the remaining 41 cases, the biliary drainage tube was removed 2 d after the procedure. Post-procedure cholangiography revealed stent patency. There were no cases requiring implanting another biliary stent or further percutaneous transhepatic drainage.
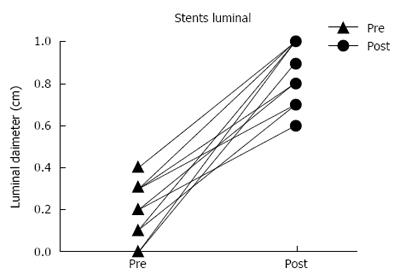
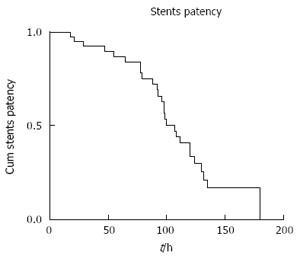
There were no procedure related complications per SIR reporting standards. And no cases of hemorrhage, bile duct perforation, bile leak, or pancreatitis were observed after the intraductal RF. Mild abdominal pain (n = 16) was the main symptom after procedure, and it can subside spontaneously in 36 h. One patient was lost to follow-up, and 3 patients with cachexia due to multiple organ failure died 1 mo after ablation. Intraoperative angiography indicated that the median length of the biliary stricture was 35 mm (range: 20-55 mm). The median number of intraductal RF was 3 times (range: 2-5 times), which was based on the location and degree of obstruction of the biliary stent. The median output power for the intraductal RF was 2474 J (range: 1200-3600 J), and cholangiography was used to measure the diameter of the biliary tract. The median diameter of the biliary stricture before and after procedure was 1 mm (range: 0-4 mm) vs 8.0 mm (range: 6.0-10.0 mm). The median stent patency duration was 107 d (range: 12-180 d). Figure 3 presents Kaplan-Meier curves that reveal stent patency trends. Figure 4 indicates pre- and post-procedure luminal diameters. The bilirubin levels before and after procedure were 63 ± 29 μmol/L vs 128 ± 65 μmol/L (P < 0.05). Table 2 showed details about hepatic function metrics changes before and after procedure.
| Parameters | Pre-ablation | Post-ablation (day 3) | Normal |
| Bilirubin (μmol/L) | 128 ± 65 | 63 ± 29 | 0-21 |
| ALP (IU/L) | 1240 ± 865 | 1032 ± 790 | 30-130 |
| ALT (IU/L) | 105 ± 58 | 79 ± 40 | < 40 |
| GGT (IU/L) | 747 ± 729 | 720 ± 625 | < 55 |
| LDH (IU/L) | 60 ± 84 | 311 ± 45 | 0-250 |
| AST (IU/L) | 98 ± 49 | 65 ± 34 | < 40 |
| CRP (mg/L) | 15 ± 8 | 12 ± 7 | 0-5 |
| Amylase (IU/L) | 80 ± 15 | 79 ± 12 | 0-90 |
Obviously, with lengthened patient survival times, SEMS occlusion has become a common clinical situation. Although organic polymer-packaged SEMSs or methods to coat stents with nickel titanium alloy or other alloys could potentially be used instead of stainless steel or covered stents to address the issue of stent restenosis, experimental data have not supported this possibility[5,6]. Rather, the data have indicated that these novel types of stents increase the incidence of pancreatitis and cholecystitis, leading to long-term inflammation and bile duct bleeding[7-9]. Khashab et al[10] tried to extend the stent patency time by changing the shape of the stent, but the results were not different from those for a conventional stent.
Once a stent is placed in the bile duct, an encrustation of amorphous material and bacteria (sludge) begins to accumulate on its surface. The major limitation to long-term biliary stenting is thus early stent occlusion, although early symptoms of stent obstruction are not typical. Pneumobilia in the intrahepatic biliary tree is present when there is reflux of gas from the bowel and can also be present after biliary stent occlusion. In this context, early improvement of biliary drainage is particularly important[11].
RF has been widely used to treat malignant solid tumors and has even become a standard treatment for certain inoperable tumors, such as liver cancer and lung cancer. Its safety and efficacy are well established. However, restricted to the traditional RF structure, the RF technology has never been used to treat malignant biliary obstruction. The use of this catheter risks indirect injury to adjacent organs and electrode-induced skin burns. In addition, the unpredictability of the electric current path reduces the ablation area. The use of RFA in the biliary tract is also limited due to the possibility of biliary fistulas and bile duct adhesion. A new bipolar catheter can avoid the aforementioned problems and has been demonstrated to be successful and safe for palliative therapy for malignant biliary occlusion[12].
Intraductal RF can delay tumor growth and retain the patency of SEMSs for a prolonged duration. In turn, the successful drainage leads to prolongation of survival time[13]. Khorsandi et al[14] subjected the EndoHPB catheter to extensive in vivo preclinical testing. A preliminary study using a pig model indicated that this catheter can be safely deployed in the context of SEMSs. In particular, intraductal RF treatment using this catheter causes the coagulative burning of intraductal tissues, but the heat associated with this burning will not damage surrounding tissue[15,16]. Another single published ex-vivo porcine study sought to systematically evaluate the effect of intraductal RF at various power settings (5, 10, 15 and 20 W) and durations of treatment (60, 90 and 120 s) on freshly resected porcine livers[17]. In practice, setting the output power to 10 W and ablation time for 90 s, it performed safe and efficient (Table 1). In the current study, none of patients exhibited pancreatitis or a biliary fistula due to heating.
An examination of endoscopic biliary RFA treatment in cases of malignant biliary obstruction and stent restenosis has confirmed the efficacy and safety of biliary RF technology[18]. Steel et al[3] specifically reported the endoscopic intraductal RF in 22 patients with malignant biliary obstruction. The examined cases included 10 patients with biliary SEMS restenosis (6 pancreatic cancer patients, 2 bile duct carcinoma patients, and 2 metastatic liver cancer patients) who underwent 13 intraductal RF treatments. The luminal diameter of the stenosis increased from a preoperative value of 1 mm to 5 mm after intraductal RF. The biliary stents remained open with a median patency duration of 119 d after procedures. Clinical research results have also demonstrated the effectiveness and safety of RF therapy for stent restenosis treatment in the biliary tract[19]. For patients with a history of gastrointestinal surgery, ERCP is considered a contraindication, but PTCD has no such limitation.
Intraductal RF via endoscopy has been used in the treatment of SEMS obstruction because of tumour ingrowth or overgrowth, which is a frequent complication. Mukund et al[19] specifically used intraductal RF to clear obstructed SEMSs. Both cases had extensive disease and showed radiological and biochemical evidence of improved drainage after intraductal RF application. However, the number of cases was too small to draw a definitive conclusion. Complication rates with both approaches appear to be comparable with those with the current standard ERC/PTD insertion and stenting in patients with malignant biliary disease[20,21].
Research has indicated that RF technology has potential clinical applications in treating stenosis of the biliary tract, and endoscopic RFA treatment in cases of malignant biliary obstruction and in-stent restenosis has confirmed the efficacy and safety of intraductal RF technology[22]. Furthermore, in the case of obstruction of a previously deployed metal stent, which cannot be removed, this intraductal RF approach can clear the occlusion and restore the biliary flow without the insertion of a new stent inside the obstructed stent, thereby saving the cost of a second stent[23]. Intraductal RF also has the advantageous characteristics of being a repeatable procedure by ERCP and PTCD. Moreover, for obstructive jaundice with a history of gastrointestinal surgery, it is difficult to reach the site of bile duct obstruction by endoscopy[24].
There were no major complications in our patients. The RF catheter can be easily introduced to the biliary tract and accurately positioned at the stricture lesion. However, the dispute is that how to apply intraductal RF for different stent locations (the hilum or ampulla) and how to choose an appropriate approach (percutaneous RFA or endoscopic RFA) to avoid injury to the bile duct and surrounding structures[21,25]. More clinical studies are required to guide clinical application.
The present study was a pilot feasibility study with obvious limitations. The number of patients enrolled was small. The follow-up duration may have been inadequate to demonstrate the long-term efficacy of this novel technique. Further studies are required to confirm our results.
The use of biliary self-expanding metallic stents is an effective method for treating malignant biliary obstruction. There is a clinical need for an effective method of re-opening biliary stents that accounts for the limitations of an endoscope, particularly in cases involving hepatic hilar tumors or after gastrointestinal operations. Therefore, our research group investigated the treatment of biliary stent occlusion by percutaneous biliary radiofrequency ablation (RFA).
To assess the feasibility and effectiveness of a novel application of percutaneous RF for the treatment of biliary stents obstruction, the authors specifically report a retrospective study presenting the results of percutaneous intraductal RF in patients with biliary stent occlusion.
This preliminary clinical study demonstrated that percutaneous intraductal RF is safe and effective for the treatment of biliary stent obstruction, increasing the duration of stent patency, although randomized controlled trials are needed to confirm the effectiveness of this approach.
In this manuscript, a total of 43 cases involving biliary obstruction caused by biliary stent stenosis were treated by placing an EndoHPB catheter into the stenosis and performing percutaneous transhepatic biliary RFA. The authors found that percutaneous internal biliary RFA is safe and effective for the treatment of biliary stent obstruction and increases the accumulation of stent patency time, although randomized controlled trials are needed to confirm the effectiveness of this approach.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Musquer N, Seo DW S- Editor: Yu J L- Editor: Wang TQ E- Editor: Wang CH
| 1. | Shepherd HA, Royle G, Ross AP, Diba A, Arthur M, Colin-Jones D. Endoscopic biliary endoprosthesis in the palliation of malignant obstruction of the distal common bile duct: a randomized trial. Br J Surg. 1988;75:1166-1168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 378] [Cited by in RCA: 337] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 2. | Ridtitid W, Rerknimitr R. Management of an occluded biliary metallic stent. World J Gastrointest Endosc. 2012;4:157-161. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 13] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 3. | Steel AW, Postgate AJ, Khorsandi S, Nicholls J, Jiao L, Vlavianos P, Habib N, Westaby D. Endoscopically applied radiofrequency ablation appears to be safe in the treatment of malignant biliary obstruction. Gastrointest Endosc. 2011;73:149-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 215] [Cited by in RCA: 225] [Article Influence: 16.1] [Reference Citation Analysis (0)] |
| 4. | Monga A, Gupta R, Ramchandani M, Rao GV, Santosh D, Reddy DN. Endoscopic radiofrequency ablation of cholangiocarcinoma: new palliative treatment modality (with videos). Gastrointest Endosc. 2011;74:935-937. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 46] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 5. | Andersen JR, Sørensen SM, Kruse A, Rokkjaer M, Matzen P. Randomised trial of endoscopic endoprosthesis versus operative bypass in malignant obstructive jaundice. Gut. 1989;30:1132-1135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 436] [Cited by in RCA: 393] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 6. | Elwir S, Sharzehi K, Veith J, Moyer MT, Dye C, McGarrity T, Mathew A. Biliary stenting in patients with malignant biliary obstruction: comparison of double layer, plastic and metal stents. Dig Dis Sci. 2013;58:2088-2092. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 7. | Loew BJ, Howell DA, Sanders MK, Desilets DJ, Kortan PP, May GR, Shah RJ, Chen YK, Parsons WG, Hawes RH. Comparative performance of uncoated, self-expanding metal biliary stents of different designs in 2 diameters: final results of an international multicenter, randomized, controlled trial. Gastrointest Endosc. 2009;70:445-453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 110] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 8. | Cariati A, Piromalli E. Prevention of biliary stent occlusion. Dig Dis Sci. 2012;57:1971; author reply 1971-1972. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 9. | Cui PJ, Yao J, Zhao YJ, Han HZ, Yang J. Biliary stenting with or without sphincterotomy for malignant biliary obstruction: a meta-analysis. World J Gastroenterol. 2014;20:14033-14039. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 31] [Cited by in RCA: 35] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 10. | Khashab MA, Hutfless S, Kim K, Lennon AM, Canto MI, Jagannath SB, Okolo PI, Shin EJ, Singh VK. A comparative evaluation of early stent occlusion among biliary conventional versus wing stents. Dig Dis Sci. 2012;57:1708-1716. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Thomas S, Patel RP, Oto A. Resolution of pneumobilia as a predictor of biliary stent occlusion. Clin Imaging. 2015;39:650-653. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Eum YO, Kim YT, Lee SH, Park SW, Hwang JH, Yoon WJ, Ryu JK, Yoon YB, Han JK, Yoon CJ. Stent patency using competing risk model in unresectable pancreatic cancers inserted with biliary self-expandable metallic stent. Dig Endosc. 2013;25:67-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Sugiyama G, Okabe Y, Ishida Y, Saitou F, Kawahara R, Ishikawa H, Horiuchi H, Kinoshita H, Tsuruta O, Sata M. Evaluation of endoscopic biliary stenting for obstructive jaundice caused by hepatocellular carcinoma. World J Gastroenterol. 2014;20:6968-6973. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 7] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 14. | Khorsandi SE, Zacharoulis D, Vavra P, Navarra G, Kysela P, Habib N. The modern use of radiofrequency energy in surgery, endoscopy and interventional radiology. Eur Surg. 2008;40:204-210. [RCA] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 15. | Ortner MA. Photodynamic therapy for cholangiocarcinoma: overview and new developments. Curr Opin Gastroenterol. 2009;25:472-476. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 38] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 16. | Itoi T, Isayama H, Sofuni A, Itokawa F, Tamura M, Watanabe Y, Moriyasu F, Kahaleh M, Habib N, Nagao T. Evaluation of effects of a novel endoscopically applied radiofrequency ablation biliary catheter using an ex-vivo pig liver. J Hepatobiliary Pancreat Sci. 2012;19:543-547. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 58] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 17. | Branovan DI, Fridman M, Krasko O, Lushchik M, Drozd V, Shiglik N, Danilova L, Demidchik Y. Bipolar radiofrequency ablation for thyroid nodules with effective induction of sufficiently large lesions without danger to surrounding structures (ex vivo morphological evaluation). Pathology. 2016;48 Suppl 1:S119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 18. | Wadsworth CA, Westaby D, Khan SA. Endoscopic radiofrequency ablation for cholangiocarcinoma. Curr Opin Gastroenterol. 2013;29:305-311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 39] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 19. | Mukund A, Arora A, Rajesh S, Bothra P, Patidar Y. Endobiliary radiofrequency ablation for reopening of occluded biliary stents: a promising technique. J Vasc Interv Radiol. 2013;24:142-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 20. | Mulier S, Ruers T, Jamart J, Michel L, Marchal G, Ni Y. Radiofrequency ablation versus resection for resectable colorectal liver metastases: time for a randomized trial? An update. Dig Surg. 2008;25:445-460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 102] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 21. | Kobayashi N, Watanabe S, Hosono K, Kubota K, Nakajima A, Kaneko T, Sugimori K, Tokuhisa M, Goto A, Mori R. Endoscopic inside stent placement is suitable as a bridging treatment for preoperative biliary tract cancer. BMC Gastroenterol. 2015;15:8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 22. | Kogure H, Isayama H, Nakai Y, Tsujino T, Matsubara S, Yashima Y, Ito Y, Hamada T, Takahara N, Miyabayashi K. High single-session success rate of endoscopic bilateral stent-in-stent placement with modified large cell Niti-S stents for malignant hilar biliary obstruction. Dig Endosc. 2014;26:93-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 48] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 23. | Wu TT, Li WM, Li HC, Ao GK, Zheng F, Lin H. Percutaneous Intraductal Radiofrequency Ablation for Extrahepatic Distal Cholangiocarcinoma: A Method for Prolonging Stent Patency and Achieving Better Functional Status and Quality of Life. Cardiovasc Intervent Radiol. 2017;40:260-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 36] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 24. | Alvarez-Sánchez MV, Napoléon B. Review of endoscopic radiofrequency in biliopancreatic tumours with emphasis on clinical benefits, controversies and safety. World J Gastroenterol. 2016;22:8257-8270. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 39] [Cited by in RCA: 35] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 25. | Kato H, Tsutsumi K, Harada R, Okada H, Yamamoto K. Endoscopic bilateral deployment of multiple metallic stents for malignant hilar biliary strictures. Dig Endosc. 2013;25 Suppl 2:75-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |