Published online Feb 28, 2016. doi: 10.3748/wjg.v22.i8.2611
Peer-review started: September 29, 2015
First decision: November 5, 2015
Revised: November 30, 2015
Accepted: December 12, 2015
Article in press: December 14, 2015
Published online: February 28, 2016
Processing time: 150 Days and 1 Hours
AIM: To describe the disease and psychosocial outcomes of an inflammatory bowel disease (IBD) transition cohort and their perspectives.
METHODS: Patients with IBD, aged > 18 years, who had moved from paediatric to adult care within 10 years were identified through IBD databases at three tertiary hospitals. Participants were surveyed regarding demographic and disease specific data and their perspectives on the transition process. Survey response data were compared to contemporaneously recorded information in paediatric service case notes. Data were compared to a similar age cohort who had never received paediatric IBD care and therefore who had not undergone a transition process.
RESULTS: There were 81 returned surveys from 46 transition and 35 non-transition patients. No statistically significant differences were found in disease burden, disease outcomes or adult roles and responsibilities between cohorts. Despite a high prevalence of mood disturbance (35%), there was a very low usage (5%) of psychological services in both cohorts. In the transition cohort, knowledge of their transition plan was reported by only 25/46 patients and the majority (54%) felt they were not strongly prepared. A high rate (78%) of discussion about work/study plans was recorded prior to transition, but a near complete absence of discussion regarding sex (8%), and other adult issues was recorded. Both cohorts agreed that their preferred method of future transition practices (of the options offered) was a shared clinic appointment with all key stakeholders.
CONCLUSION: Transition did not appear to adversely affect disease or psychosocial outcomes. Current transition care processes could be optimised, with better psychosocial preparation and agreed transition plans.
Core tip: Limited data exists regarding psychosocial and disease outcomes for inflammatory bowel disease patients following transition from paediatric to adult care and their perspectives on the process. Our study obtained this data through questionnaires and compared it to a matched cohort to see if the transition process itself influenced outcomes. We found that transition programs did not appear to adversely affect disease or psychosocial outcomes; however, patients have poor knowledge of their transition plan many are not strongly prepared. Current transition care practices could be optimised and this data contributes to a foundation on which future transition practices can be designed.
- Citation: Bennett AL, Moore D, Bampton PA, Bryant RV, Andrews JM. Outcomes and patients’ perspectives of transition from paediatric to adult care in inflammatory bowel disease. World J Gastroenterol 2016; 22(8): 2611-2620
- URL: https://www.wjgnet.com/1007-9327/full/v22/i8/2611.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i8.2611
In adolescents with chronic diseases, movement from paediatric to adult services is inevitable and is increasingly recognised as an essential element of holistic care[1-3]. A successful transition in young people with chronic conditions differs from simple handover of care and should aim to maximise the young person’s quality of life[4], with the ultimate goal of facilitating the development of successful self-management[5].
The topic of transition care has received significant attention in the literature[6-9] with considerable debate around the most effective way to achieve a smooth transition. A general consensus exists however; that whatever solution is adopted it should encompass a comprehensive programme that reflects and encourages the patient’s physical, psychological and social development, rather than merely providing a physical transfer from paediatric to adult care[10]. Implementation of an effective transition program has been shown to improve patient health and life outcomes in patients with liver transplant[11], diabetes mellitus[12] and juvenile arthritis[13] and facilitate self-reliance[14]. Conversely, if done poorly, adverse effects on health[15-17] and health service use[12] in other diseases have been reported. There is currently only extremely scant outcome data in inflammatory bowel disease (IBD).
In Australia, transition practises for IBD are highly variable and often involve a physical transfer of the patient rather than a coordinated, comprehensive and supportive process. This is despite a recent survey of adult and paediatric gastroenterologists, reporting that this is important[18].
Previous IBD transition care literature has highlighted multiple barriers to effective transition, with several studies obtaining perspectives from paediatric and adult gastroenterologists’ and IBD nurses[18-21]. From this growing body of literature practical recommendations for transitioning IBD patients have been promulgated[22,23]. However, as yet, these proposals lack actual outcome data and have omitted patient perspectives. Thus it is not yet clear whether these recommendations would improve health outcomes. Therefore outcome and patient perspective data are needed to critically appraise current practices and inform the development of interventions intended to improve transition outcomes.
The aims of this study were to thus to present such factual data and specifically to describe the disease and psychosocial outcomes and personal perspectives of a cohort of young adults with IBD who had recently moved from paediatric to adult care (transition cohort). The outcomes of this group are also compared to a cohort of patients with IBD with similar demographics and disease duration whose care had been solely in the adult realm (non-transition cohort).
This cross-sectional study was conducted in three parts. Firstly, a cohort of IBD patients diagnosed in paediatric services who had moved to adult care was identified and surveyed. Secondly, the case records of these transition patients were examined to verify their histories and to review clinician recorded data on transition plans and doctor-patient discussions. Finally, a non-transition cohort of young adults with IBD was surveyed for comparison.
In 2013 an IBD database established and maintained at the sole public paediatric gastroenterology service in South Australia (SA), Women’s and Children’s Hospital (WCH), was interrogated to identify people with IBD who had turned 18 (mandatory timing of transfer of care to adult services) since 2003. Patients diagnosed prior to age 18 on the Royal Adelaide Hospital (RAH) and Flinders Medical Centre (FMC) IBD databases were also identified. Potential participants were invited to participate by completing the questionnaire by return mail. The questionnaire (Appendix 1) included items relating to demographics, disease specific quantitative data, patient perspectives regarding their personal transition experience and perceived barriers.
During this period in SA, transition of adolescent IBD patients to adult healthcare services occurred via a letter of referral and if appropriate, telephone handover. Only since 2013, has IBD and hospital information been sent to the patient and a telephone introductory call by an adult IBD service nurse made.
In this transition cohort, survey response data were compared to contemporaneously recorded information in paediatric service case notes. Data regarding the planned transition process to adult care, availability of choice of location of adult care, timing of transition, psychosocial discussions during the transition period and disease characteristics at diagnosis were reviewed. Medication recommendations, current medication use, disease complications and surgery following transition to adult care were not reviewed nor confirmed in medical records.
A comparative cohort who had not undergone transition to adult care was investigated to see whether the transition process itself might have influenced physical/disease and psychosocial outcomes. This cohort was chosen out of a convenience sample of young patients diagnosed before 18, but never cared for in a paediatric setting. This results from the fact that in SA, from age 14, parents have a choice as to who (paediatric or adult specialist) cares for their child. IBD databases at the RAH and FMC were interrogated to derive a cohort which matched (as closely as possible) the original transition group cohort for age, gender, diagnosis and disease duration. Potential participants were invited to participate by completing the same questionnaire as the transition cohort with exemption of the section relating to personal transition experiences. Given that patients in this cohort did not undergo the transition process, medical records for this group were not reviewed.
Questionnaires were posted out accompanied by a letter of invitation, information sheet, consent form and opt-out form. Both the transition and non-transition cohorts had reminder letters at 2 wk and 2 mo except for “return to senders” and opt-out candidates. All completed surveys were de-identified.
The study was approved by the Human Research Ethics Committees of the WCH, RAH and FMC. All participating patients completed a consent form.
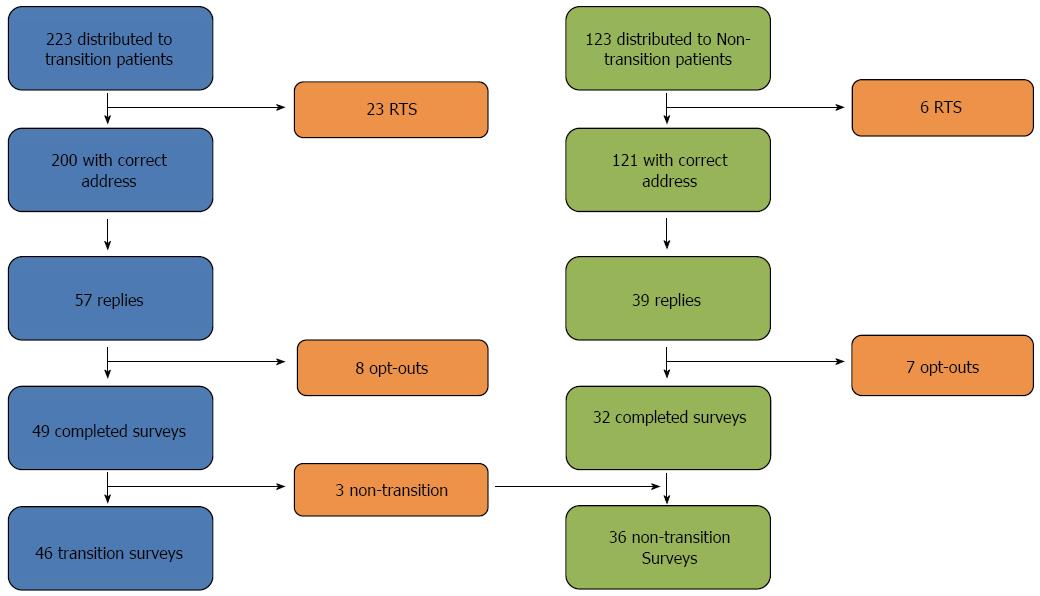
Two hundred and twenty three transition patients who appeared to have received paediatric IBD care were criteria invited to participate. Twenty-three patients were uncontactable (post marked “return-to-sender”), 49 completed surveys and 8 opted out requesting no further contact (response rate 49/200 = 24.5%). Three of the respondents were subsequently found to have received all care in the adult setting and were re-allocated to the non-transition cohort, leaving 46 transition respondents. Of 127 non-transition patients invited, 32 completed surveys, 7 opted-out and 6 “return-to-senders” were received (response rate 32/121 = 26%). The 3 surveys earlier excluded from the transition cohort were included in the non-transition cohort, resulting in 35 respondents (Figure 1). Not all respondents answered all questions. Data are presented as a percentage of those answering each item. The response rate did not differ between transition and non-transition cohorts (24.5% vs 26%, P = 0.69), and non-responders did not differ from responders in either cohort in terms of age, gender or postcode (as a proxy measure of socioeconomic status).
Amongst transition respondents (n = 46), 31 (67%) had Crohn’s disease (CD), 14 (30%) had ulcerative colitis (UC) and one (2%) had IBD-Unclassified. Compared to case notes data, correct knowledge of disease was found in 100% of patients, however, correct knowledge of disease extent was found in only 18 of 31 patients (58%) with CD and 8/14 (57%) with UC. In the non-transition cohort (n = 35), 22 (63%) had CD and 13 (37%) had UC. Correct knowledge of disease extent was not assessed as case notes for this cohort were not reviewed. Cohorts were matched for age (P = 0.26) and gender (P = 0.51), but a highly statistically significant difference was found between cohorts for disease duration (P < 0.000005). No significant differences were found between cohorts for location of residence or socio-economic status based upon post-code. Demographic details for both cohorts are outlined in Tables 1 and 2.
| IBD transition patients (n = 46) | IBD non-transition patients (n = 35) | P value | |
| Type of IBD | |||
| Crohn’s disease | 31 (67) | 22 (63) | 0.81 |
| Ulcerative colitis | 14 (30) | 13 (37) | 0.64 |
| Indeterminate | 1 (2) | 0 (0) | 1.00 |
| Gender | |||
| Male | 24 (52) | 13 (37) | 0.26 |
| Female | 22 (48) | 22 (63) | 0.26 |
| Current age (yr) | |||
| 18-23 | 26 (57) | 17 (49) | 0.51 |
| 23-28 | 20 (43) | 18 (51) | 0.51 |
| Mean age at diagnosis (yr) | 14 | 17 | < 0.000005 |
| Disease duration (yr) | 10.7 | 5.1 | < 0.000005 |
| Current location of care | |||
| Public | 22 (52) | 21 (70) | 0.15 |
| Private | 18 (43) | 8 (27) | 0.21 |
| Both | 2 (5) | 1 (3) | 1.00 |
| As a child | Current | As a child | Current | |
| ASGC classification1 (Postcode based) | ||||
| RA1 - Major cities | 28 (64) | 34 (76) | 20 (67) | 17 (57) |
| RA2 - Inner regional | 9 (20) | 8 (18) | 4 (13) | 6 (20) |
| RA3 - Outer regional | 4 (9) | 2 (4) | 2 (7) | 6 (20) |
| RA4 - Remote | 3 (7) | 0 (0) | 3 (10) | 1 (3) |
| RA5 - Very remote | 0 (0) | 1 (2) | 1 (3) | 0 (0) |
| SEIFA classification (IRSAD)2 (Quintiles) | ||||
| 1 | 8 (18.5) | 3 (7.0) | 7 (23.3) | 6 (20.0) |
| 2 | 9 (21.0) | 11 (25.5) | 3 (10.0) | 4 (13.3) |
| 3 | 15 (35.0) | 11 (25.5) | 10 (33.3) | 10 (33.3) |
| 4 | 6 (14.0) | 8 (19.0) | 6 (20.0) | 4 (13.3) |
| 5 | 5 (11.5) | 10 (23.0) | 4 (13.3) | 6 (20.0) |
No significant difference was found between cohorts for occurrence of IBD complications (defined as perforation, bowel obstruction or stricture), perianal disease, surgery or hospitalisation since diagnosis (Table 3).
| Transition cohort | Non-transition cohort | P value | |
| Medication (self-reported) | |||
| 5-aminosalicylic acid | 19 (41) | 14 (41) | 1.00 |
| Sulfasalazine | |||
| Mesalazine | |||
| Immunomodulator | 30 (65) | 25 (71) | 0.63 |
| Azathioprine/6 | 27 | 24 | |
| Mercaptopurine | |||
| Methotrexate | 3 | 1 | |
| Biologic therapy (anti-TNF) | 8 (17) | 9 (26) | 0.42 |
| Infliximab | 6 | 5 | |
| Adalimumab | 2 | 4 | |
| Non-compliance | 3 (7) | 4 (11) | 0.46 |
| Perianal disease | 9 (20) | 8 (24) | 0.79 |
| Complications (Perforation, bowel obstruction, stricture) | 12 (26) | 5 (14) | 0.27 |
| Surgery (Resection +/- stoma, fistula with seton) | 15 (33) (9 prior to transition) | 10 (29) | 0.81 |
| Number of hospital admissions per patient (median) | |||
| During paediatric care | 3.2 | N/A | |
| During adult care | 1.5 | 2.1 | 0.67 |
| Number of flares requiring steroids per patient (median) | |||
| Since transition | 0.5 | N/A | |
| During last year | 0.5 | 1 | 0.31 |
| Extra intestinal manifestations of IBD (Arthropathy/Cutaneous/Ocular/Hepatobiliary/Metabolic bone disease)1 | 6 (14) | 8 (24) | 0.37 |
| IBD symptoms | |||
| Physical | 39 (85) | 33 (94) | 0.29 |
| Psychological | 16 (35) | 16 (46) | 0.36 |
| Social | 29 (63) | 26 (76) | 0.23 |
| MDT utilisation | |||
| General Practitioner | 34 (74) | 25 (69) | 0.80 |
| Psychologist | 2 (4) | 3 (8) | 0.65 |
| Dietician | 9 (20) | 7 (19) | 1.00 |
| Colorectal surgeon | 12 (26) | 11 (31) | 0.80 |
| IBD nurse | 11 (24) | 19 (25) | 0.01 |
| Relationship status | |||
| Single | 22 (48) | 17 (49) | 1.00 |
| In a relationship | 20 (43) | 12 (34) | 0.49 |
| Married | 4 (9) | 6 (17) | 0.32 |
| Divorced | 0 (0) | 0 (0) | 1.00 |
| Education (level completed) | |||
| Primary | 43 (100) | 35 (100) | 1.00 |
| Secondary | 38 (88) | 27 (77) | 0.23 |
| Tertiary | 19 (41) | 5 (14) | 0.01 |
| TAFE (Technical and further education) | 8 (17) | 12 (34) | 0.12 |
| Apprenticeship/trade | 6 (13) | 7 (20) | 0.54 |
| Employment | |||
| Currently employed | 35 (76) | 21 (60) | 0.15 |
| Full-time employment | 21 (60) | 11 (52) | 0.59 |
| Average hours worked/week | 29.8 | 34.2 |
Similar rates of self-reported medication use for most classes of drugs, non-compliance and side effects were found in both cohorts (Table 3). Self-reported medication recommendations compared to actual use was not confirmed given the retrospective nature of the study and the lack of a universal prescription tracking database.
The majority of respondents were regularly reviewed by a gastroenterologist [42/46 (91%), transition patients and 30/35 (86%), non-transition patients]. Among transition patients reviewed 15% were reviewed 3 monthly or more often, 60% 6 monthly and 25% annually. This compared with 38%, 48% and 14% respectively in the non-transition group. Twelve out of 22 (55%) transition patients, all of whom were public patients, reported contacting their IBD nurse as an option if a problem arose and 12 public patients felt adequately supported. Of note, these were not entirely the same 12 who reported contacting the IBD nurses. This compared with approximately the same proportion [12/29 (41%)] non-transition patients contacting their IBD nurse yet almost all [30/31 (97%)] feeling adequately supported.
Utilisation of members of other the multi-disciplinary team was generally low in both cohorts, except for their general practitioners (Table 3). The percentage of physical, psychological and social side effects relating to IBD is outlined in Table 3. The most frequent patient-reported symptoms listed in descending order of frequency included; fatigue, weight loss and diarrhoea; mood disturbance and reduced social interactions and interruptions to work/school.
No significant differences were seen in the rate of achievement of adult roles and responsibilities (marital status, education level and employment) between patients who transitioned compared to non-transition patients (Table 3).
Details regarding personal transition experience are outlined in Table 4. Thirty seven (of 46) transition patient medical records were available for review to compare with self-reported plans. In the majority (29/37, 78%) of case notes reviewed, there was evidence of discussion regarding future study/employment; however, documentation of any sexual or psychological discussions was found in only 3 and 7 patients’ files respectively.
| Age at first discussion of transition (yr) | |
| Median | 18 (Range: 16-18) |
| Mean | 17 |
| Age at transition (yr) | |
| Median | 18 (Range: 16-19) |
| Mean | 18 |
| Knowledge of transition plan by patient | 16 (36) |
| Case note documentation of transition plan | 32 (86) |
| Patient prepared for transition | |
| Not prepared | 10 (23) |
| Slightly prepared | 15 (34) |
| Strongly prepared | 19 (43) |
| Transition felt to be structured | 26 (63) |
| Part of transition decision making process | 25 (58) |
| Patient reported choice of transition plan | 1 (3) |
Positive feedback regarding what was done well at the time of transition was given by 24 patients (52%) and predominantly centred on provision of information and communication. Conversely, when asked what was done poorly at the time of transition 10/26 (38%) reported ‘Nothing’ and 3 (12%) reported “the handover”. The majority of respondents (37/44, 84%) were currently continuing with the same adult gastroenterologist as initially directed to after transition with no difference observed between those directed to either the public or private medical setting.
The majority (44/46, 96%) of the transition cohort felt that a structured transition plan was important. Non-transition patients also endorsed this statement (32/35, 91%). The transition cohort identified the task of establishing a new relationship with a practitioner; lack of communication and patients’ own lack of understanding of their disease as potential barriers to successful transition. Similar responses were proposed by the non-transition group. Aspects suggested by respondents as ways of improving the transition process are outline in Table 4. The majority of transition respondents thought that the timing of transition should be “age 18 years” compared with the non-transition cohort who nominated “patient readiness”. If timing of transition were to be solely based upon age, the transition group identified “age 17-18” whereas the non-transition group said “depended”. When respondents were asked if the timing of transition should be different for males and females, both cohorts replied that it would depend on the scenario. Both cohorts agreed that their preferred method of future transition practices (of the options offered) was that “at the time of transfer there is a single clinic appointment attended by the patient, caregiver, nurse coordinator, paediatric and adult gastroenterologist”.
This is the first study to simultaneously describe and compare outcome data and patients’ perspectives with regard to transition, in a cohort of paediatric onset IBD patients who have since moved on to adult care.
Approximately 25% of IBD patients are diagnosed under the age of 16 years[24] with data to suggest that onset in this period can have a more active disease course than in adults[25]. Our data suggests that despite active disease in paediatric years (frequent flares and hospital admissions), the cohort appears to have better disease control after entering adult care. This is represented by an apparent reduction in hospital admissions after leaving paediatric care with a comparable figure to the non-transition cohort. In addition, transition did not appear to significantly affect the rate of complications, surgery requirements, hospitalisation or perianal disease, which may seem surprising given the longer disease duration in the transition cohort.
Medication use was similar with self-reported non-compliance being low in both cohorts (7% transition, 11% non-transition). This is lower than 35% observed by López San Román et al[26] however; it is important to highlight that in reality, when objective measures of adherence were used, it is found that nearly 50% of patients do not take medications as prescribed[27].
The majority of the transition patients in our cohort appear to be coping well, as assessed by educational activity, employment and partnership rates. These findings are similar to the comparison non-transition cohort and more reassuringly also to Australian Bureau of Statistic population data[28,29] (based upon similar age categories). The only other paper to our knowledge examining these outcomes in young IBD patients found lower rates of further education and employment (50%)[30], and thus our data is reassuring.
Turunen et al[31] found that the quality of life of the patients with paediatric onset of IBD was decreased in early adulthood when compared to population-based controls. Our data supports this notion with a significant proportion (35%) reporting mood disturbance but despite this, psychological services are underutilised, with only 5% of those with mood disturbances accessing specific care. Whilst this data is comparable to that of the non-transition cohort suggesting that the transition process itself may not be the sole influence, it is concerning as it represents a lost opportunity to optimise their outcomes entering adult life.
Adult providers have identified a lack of medical knowledge in young patients with IBD transferred from the paediatric clinics[32], which may impair the success of transition. Pleasingly, 100% of patients in both the reported cohorts were able to correctly indicate their diagnosis. However, only 58% of the transition cohort correctly reported their extent of disease. This ignorance of an important aspect of their disease is in keeping with previous data trends[32,33]. It is concerning given the potential practical ramifications of preventing effective self-assessment and management. Provision of written information to adolescents, such as an IBD passport[34], may alleviate this knowledge gap.
A further area of significant concern is the rare documentation of any discussion regarding sexuality and reproduction on notes review of transitioning patients (in 3/34 notes only). Many young people are sexually active before age 18[35], and the lack of early discussion misses an opportunity to inform them accurately about how their IBD and especially any immunosuppressant therapy may or may not affect sexual function, sexually transmitted infections, fertility and pregnancy. This is an area where there is known to be poor knowledge amongst patients and primary care doctors[36-39], which can be helped by brief education[40]. Whilst paediatric gastroenterologists may not feel equipped or comfortable to do this, if they do not start the discussion in may be left until they are sexually active and it may be too late. These issues may have been discussed but not documented, highlighting the need for a transition checklist so that they are indeed addressed perhaps with specific assistance for paediatricians who may not be comfortable with these discussions.
Currently less than half of transition respondents feel that the process they experienced was adequate, with 23% not feeling prepared and 42% not feeling part of the decision making process. Whilst approximately half of respondents recalled knowledge of a “transition plan”, medical records indicate that this was documented in nearly all patients. This suggests that although the idea of transition was discussed 1 year on average prior to actual transition (recorded in notes) it may not be long enough or involve sufficient discussion/documentation to prepare/engage the patient. Future programs may need to involve distribution of written information or use of on-line resources, rather than a simple note in the file, as something to look at away from the doctor’s office.
Our cohort identified aspects of their transition experience that were done well and poorly, pleasingly, these were similar to key concepts of successful transition highlighted in a recent overview of the topic[10], suggesting clinicians have a good idea of how/where to make changes.
Adolescents with IBD have been highlighted as a group where there are significant barriers to transition to adult care[7]. The barriers identified by patients in our study, in addition to poor patient knowledge, concur with results from a small study of surveyed IBD patients in Spain[41]. Findings differ however, to a medical position paper based upon recommendations of the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition. Barriers discussed related to the reluctance of the patient, their family and medical providers for transition and the lack of a clear and consistent route to follow by medical practitioners[42]. Further survey data obtained from the perspectives of adult and paediatric gastroenterologists and nurses highlights suboptimal training for adult gastroenterologists[43], lack of entities such as resources, and clinician time[20,43], and lack of self-advocacy[42] as the main barriers. Perspectives on this topic are diverse and vary according to the cohort surveyed, with a paucity of viewpoints from patient cohorts in published literature. Our study has shown that patient perspectives differ to those aired by healthcare professionals and are vital, as without them we risk designing a system which suits medical professionals and not patients. Regardless of the origin, barriers identified can potentially lead to sub-optimal outcomes, which have been observed in existing chronic illness programme descriptions[31]. Being aware of all barriers is essential to any proposed system re-design to ensure what is done, is practical and acceptable to all stakeholders.
Currently, changes in transition practices are being recommended[7,43,44] without knowing what is actually happening to this cohort and what their preferences are. When specifically asked what they would prefer as a transition practice the majority of our transition cohort agreed that a period of overlapping care with a single clinic appointment attended by the patient, caregiver, nurse coordinator, paediatric and adult gastroenterologist would be the most appropriate. This technique has been shown to be beneficial for increasing IBD patients “readiness” for transfer[45], and among diabetic patients in improving disease control and increasing rates of follow up[2].
Despite the uniqueness of the data collected we recognise the limitations of our study. The foremost is the response rate (about 25%) in both cohorts. These response rates are similar for other young adult cohorts without incentive[46,47], and whilst one cannot regard the data as conclusive, one can certainly draw inferences and make suggestions based on this data in conjunction with the scant existing literature. Moreover the data are likely to be representative as there does not appear to be either a strong positive or negative responder bias as no difference in SES, age or gender was found between responders and non-responders. Secondly although the cohorts were matched for age and disease, there was a statistically significant difference in disease duration, despite rigorous attempts to match for this, which may have led to differences in disease outcomes. Responders did not differ in age, gender or postcode from non-responders so this is somewhat reassuring that there is not a large source of bias. Whilst these limitations exist we feel that our methodology is the most appropriate, as we are documenting outcomes of an existing process before changing it, so any alterations address deficiencies and are in line with patients’ wishes.
Whilst recent transition practice did not appear to adversely affect disease or psychosocial outcomes, current processes could be optimised, with better psychosocial preparation, greater awareness of mood disturbance, more effective provision of psychological care and explicitly documented and shared transition plans. These new data which include young patients’ perspectives are an important missing piece that contributes to a foundation on which future transition practices can be designed to optimise the process and improve outcomes.
We thank Rammy Abu-Assi, Rachel Grafton, Julie Hughes and Sarah Clark for assistance in the distribution of questionnaires.
Transitioning of adolescent patients with inflammatory bowel disease (IBD), a chronic, lifelong condition, is inevitable and an important aspect of their holistic care. Effective transition programs have been shown to improve patient health and life outcomes in other chronic diseases and conversely, if done poorly, adverse effects on health and health service use have been reported. Whilst transition practices are highly variable worldwide, a successful transition in young people with chronic conditions should aim to maximise the young person’s quality of life, with the ultimate goal of facilitating the development of successful self-management.
Previous IBD literature has highlighted multiple barriers to effective transition with practical recommendations being made. However, these proposals lack actual outcome data and patient perspectives and thus it is not yet clear whether these recommendations would improve health outcomes. This study simultaneously describes and compares outcome data and patients’ perspectives with regard to transition and provides important information in a field where IBD data is minimal.
This study is the first of its kind to present disease outcome data and patient perspectives in an IBD transition cohort. The authors found that whilst recent transition practices did not appear to adversely affect disease or psychosocial outcomes, current processes could be optimised, with better psychosocial preparation, greater awareness of mood disturbance, more effective provision of psychological care and explicitly documented and shared transition plans.
These new disease and psychosocial outcome data in addition to young patients’ perspectives are an important missing piece that contributes to a foundation on which future transition practices can be designed to optimise the process and improve outcomes.
The main concept of transition care is that it should encompass a comprehensive programme that reflects and encourages the patient’s physical, psychological and social development, rather than merely providing a physical transfer from paediatric to adult care.
This is a retrospective study, a survey, on an important aspect in IBD, transition care. In this cross-sectional study, the authors provide well documented outcomes of transition from paediatric to adult care in a large group of patients with IBD.
P- Reviewer: Desai DC, Yuksel I S- Editor: Ma YJ L- Editor: A E- Editor: Zhang DN
| 1. | Kennedy A, Sloman F, Douglass JA, Sawyer SM. Young people with chronic illness: the approach to transition. Intern Med J. 2007;37:555-560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 108] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 2. | Crowley R, Wolfe I, Lock K, McKee M. Improving the transition between paediatric and adult healthcare: a systematic review. Arch Dis Child. 2011;96:548-553. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 512] [Cited by in RCA: 455] [Article Influence: 32.5] [Reference Citation Analysis (0)] |
| 3. | Blum RW, Garell D, Hodgman CH, Jorissen TW, Okinow NA, Orr DP, Slap GB. Transition from child-centered to adult health-care systems for adolescents with chronic conditions. A position paper of the Society for Adolescent Medicine. J Adolesc Health. 1993;14:570-576. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 968] [Cited by in RCA: 1016] [Article Influence: 31.8] [Reference Citation Analysis (0)] |
| 4. | Cutler A, Brodie L. Transition care for young people – what should we be doing? The Australian Health Consumer 2004-2005.3.16-17. Available from: https://www.chf.org.au/pdfs/ahc/ahc-2004-3-transition-care-young-people.pdf. |
| 5. | American Academy of Pediatrics; American Academy of Family Physicians; American College of Physicians-American Society of Internal Medicine. A consensus statement on health care transitions for young adults with special health care needs. Pediatrics. 2002;110:1304-1306. [PubMed] |
| 6. | Goodhand J, Hedin CR, Croft NM, Lindsay JO. Adolescents with IBD: the importance of structured transition care. J Crohns Colitis. 2011;5:509-519. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 95] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 7. | Hait E, Arnold JH, Fishman LN. Educate, communicate, anticipate-practical recommendations for transitioning adolescents with IBD to adult health care. Inflamm Bowel Dis. 2006;12:70-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 77] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 8. | While A, Forbes A, Ullman R, Lewis S, Mathes L, Griffiths P. Good practices that address continuity during transition from child to adult care: synthesis of the evidence. Child Care Health Dev. 2004;30:439-452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 125] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 9. | McDonagh JE. Growing up and moving on: transition from pediatric to adult care. Pediatr Transplant. 2005;9:364-372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 119] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 10. | Bryant RV, Trott MJ, Bennett A, Bampton PA, Moore DJ, Andrews JM. Transition of care in inflammatory bowel disease: mind the gap! Theory, practice and recommendations for an Australian context. Intern Med J. 2013;43:1171-1176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Nakhla M, Daneman D, To T, Paradis G, Guttmann A. Transition to adult care for youths with diabetes mellitus: findings from a Universal Health Care System. Pediatrics. 2009;124:e1134-e1141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 209] [Cited by in RCA: 225] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 12. | McDonagh JE, Southwood TR, Shaw KL. The impact of a coordinated transitional care programme on adolescents with juvenile idiopathic arthritis. Rheumatology (Oxford). 2007;46:161-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 167] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 13. | Rosen DS, Blum RW, Britto M, Sawyer SM, Siegel DM. Transition to adult health care for adolescents and young adults with chronic conditions: position paper of the Society for Adolescent Medicine. J Adolesc Health. 2003;33:309-311. [PubMed] |
| 14. | Dodge JA, Lewis PA, Stanton M, Wilsher J. Cystic fibrosis mortality and survival in the UK: 1947-2003. Eur Respir J. 2007;29:522-526. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 415] [Cited by in RCA: 396] [Article Influence: 22.0] [Reference Citation Analysis (0)] |
| 15. | Kipps S, Bahu T, Ong K, Ackland FM, Brown RS, Fox CT, Griffin NK, Knight AH, Mann NP, Neil HA. Current methods of transfer of young people with Type 1 diabetes to adult services. Diabet Med. 2002;19:649-654. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 233] [Cited by in RCA: 227] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 16. | Annunziato RA, Emre S, Shneider B, Barton C, Dugan CA, Shemesh E. Adherence and medical outcomes in pediatric liver transplant recipients who transition to adult services. Pediatr Transplant. 2007;11:608-614. [PubMed] |
| 17. | Yeung E, Kay J, Roosevelt GE, Brandon M, Yetman AT. Lapse of care as a predictor for morbidity in adults with congenital heart disease. Int J Cardiol. 2008;125:62-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 225] [Cited by in RCA: 259] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 18. | Wright EK, Williams J, Andrews JM, Day AS, Gearry RB, Bampton P, Moore D, Lemberg D, Ravikumaran R, Wilson J. Perspectives of paediatric and adult gastroenterologists on transfer and transition care of adolescents with inflammatory bowel disease. Intern Med J. 2014;44:490-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 48] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 19. | Sebastian S, Jenkins H, Arnott I, Croft N, Ahmad T, McCartney S. Barriers to transition care in inflammatory bowel disease: A survey of adult and paediatric gastroenterologists in the UK. Gut. 2011;60:A215-A216. [DOI] [Full Text] |
| 20. | Houston Y, Lindsay J, McCartney S, Croft N, Ahmad T, Russell R, Jenkins H, Arnott I, Sebastian S. Barriers to transition care in inflammatory bowel disease: A survey of inflammatory bowel disease nurses. [Abstract] In: Nurses presentations: Nurses poster presentations. ECCO 2011; Available from: https://www.ecco-ibd.eu/index.php/publications/congress-abstract-s/abstracts-2011/item/406.html. |
| 21. | Philpott JR. Transitional care in inflammatory bowel disease. Gastroenterol Hepatol (N Y). 2011;7:26-32. [PubMed] |
| 22. | Australian Government Department of Health. ASGC Remoteness areas. Available from: http://www.doctorconnect.gov.au/internet/otd/publishing.nsf/Content/locator. Published 2006. |
| 23. | Australian Bureau of Statistics. 2033.0.55.001 - Census of Population and Housing: Socio-Economic Indexes for Areas (SEIFA). Data cube only. Available from: http://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/2033.0.55.0012011?. |
| 24. | Sawczenko A, Sandhu BK. Presenting features of inflammatory bowel disease in Great Britain and Ireland. Arch Dis Child. 2003;88:995-1000. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 317] [Cited by in RCA: 297] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 25. | Van Limbergen J, Russell RK, Drummond HE, Aldhous MC, Round NK, Nimmo ER, Smith L, Gillett PM, McGrogan P, Weaver LT. Definition of phenotypic characteristics of childhood-onset inflammatory bowel disease. Gastroenterology. 2008;135:1114-1122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 759] [Cited by in RCA: 702] [Article Influence: 41.3] [Reference Citation Analysis (1)] |
| 26. | López San Román A, Bermejo F, Carrera E, Pérez-Abad M, Boixeda D. Adherence to treatment in inflammatory bowel disease. Rev Esp Enferm Dig. 2005;97:249-257. [PubMed] |
| 27. | Shale MJ, Riley SA. Studies of compliance with delayed-release mesalazine therapy in patients with inflammatory bowel disease. Aliment Pharmacol Ther. 2003;18:191-198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 192] [Cited by in RCA: 196] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 28. | Australian Bureau of Statistics. Year Book Australia: Education and Training: Higher Education. (cat. no. 1301.0). Available from: http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/by Subject/1301.0~2012~Main Features~Higher education~107. |
| 29. | Australian Bureau of statistics. Young people in employment. Available from: http://www.abs.gov.au/AUSSTATS/abs@.nsf/2f762f95845417aeca25706c00834efa/40070b718b1c9acfca256e9e0028808c!OpenDocument. |
| 30. | Cole R, Ashok D, Kumar , Razack A, Azaz A, Sebastian S. OC-052 Comparative evaluation of outcomes in adolescents with IBD on transfer from paediatric to adult health care services: a case for structured transition. [abstract] In: BSG transition symposium. Digestive Disorders Federation Meeting 17-20 June 2012. Gut. 2012;61:A23. [DOI] [Full Text] |
| 31. | Turunen P, Ashorn M, Auvinen A, Iltanen S, Huhtala H, Kolho KL. Long-term health outcomes in pediatric inflammatory bowel disease: a population-based study. Inflamm Bowel Dis. 2009;15:56-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 79] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 32. | Hait EJ, Barendse RM, Arnold JH, Valim C, Sands BE, Korzenik JR, Fishman LN. Transition of adolescents with inflammatory bowel disease from pediatric to adult care: a survey of adult gastroenterologists. J Pediatr Gastroenterol Nutr. 2009;48:61-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 119] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 33. | Fishman LN, Barendse RM, Hait E, Burdick C, Arnold J. Self-management of older adolescents with inflammatory bowel disease: a pilot study of behavior and knowledge as prelude to transition. Clin Pediatr (Phila). 2010;49:1129-1133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 76] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 34. | Muhammad R, Law TL, Limdi JK. The IBD passport: bridging another gap in quality of care? J Crohns Colitis. 2012;6:261-262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 35. | Smith A, Agius P, Dyson S, Mitchell A, Pitts M. Secondary Students and Sexual Health 2002 - Summary - Results of the 3rd National Survey of Australian Secondary Students, HIV/AIDS and Sexual Health. Available from: http://www.latrobe.edu.au/arcshs/downloads/arcshs-research-publications/secondary_students_and_sexual_health_2002_summary.pdf. |
| 36. | Mountifield RE, Prosser R, Bampton P, Muller K, Andrews JM. Pregnancy and IBD treatment: this challenging interplay from a patients’ perspective. J Crohns Colitis. 2010;4:176-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 65] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 37. | Mountifield R, Bampton P, Prosser R, Muller K, Andrews JM. Fear and fertility in inflammatory bowel disease: a mismatch of perception and reality affects family planning decisions. Inflamm Bowel Dis. 2009;15:720-725. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 176] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 38. | Selinger CP, Eaden J, Selby W, Jones DB, Katelaris P, Chapman G, McDonald C, McLaughlin J, Leong RW, Lal S. Patients’ knowledge of pregnancy-related issues in inflammatory bowel disease and validation of a novel assessment tool (‘CCPKnow’). Aliment Pharmacol Ther. 2012;36:57-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 80] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 39. | Rhodes R, Smith Z, Adams J, Stoner J, Ali T. Assessment of Physicians’ Perceived Risk of Inflammatory Bowel Disease Medications in Pregnant Patients. Gastroenterol Hepatol. 2014;10:803-808. |
| 40. | Mountifield R, Andrews JM, Bampton P. It IS worth the effort: Patient knowledge of reproductive aspects of inflammatory bowel disease improves dramatically after a single group education session. J Crohns Colitis. 2014;8:796-801. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 44] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 41. | Rao N, Ashok D, Azaz A, Sebastian S. Ready to go and Let go: Perspectives on transition and transfer from paediatric to adult health care: A paired pilot survey of adolescent IBD patients and their parents. [abstract] In: Adolescent and young people. Digestive Disorders Federation Meeting 17-20 June 2012. Gut. 2012;61:A240. [DOI] [Full Text] |
| 42. | Baldassano R, Ferry G, Griffiths A, Mack D, Markowitz J, Winter H. Transition of the patient with inflammatory bowel disease from pediatric to adult care: recommendations of the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition. J Pediatr Gastroenterol Nutr. 2002;34:245-248. [PubMed] |
| 43. | Sebastian S, Jenkins H, McCartney S, Ahmad T, Arnott I, Croft N, Russell R, Lindsay JO. The requirements and barriers to successful transition of adolescents with inflammatory bowel disease: differing perceptions from a survey of adult and paediatric gastroenterologists. J Crohns Colitis. 2012;6:830-844. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 99] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 44. | Leung Y, Heyman MB, Mahadevan U. Transitioning the adolescent inflammatory bowel disease patient: guidelines for the adult and pediatric gastroenterologist. Inflamm Bowel Dis. 2011;17:2169-2173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 78] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 45. | Dabadie A, Troadec F, Heresbach D, Siproudhis L, Pagenault M, Bretagne JF. Transition of patients with inflammatory bowel disease from pediatric to adult care. Gastroenterol Clin Biol. 2008;32:451-459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 61] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 46. | Dabadie A; PeoplePulse. Survey response rates. Available from: http://www.peoplepulse.com.au/Survey-Response-Rates.htm. |
| 47. | Zagorsky J, Rhoton P. The effects of promised monetary incentives on attrition in a long-term panel survey. Public Opin Q. 2008;72:502-513. |