Published online Nov 21, 2016. doi: 10.3748/wjg.v22.i43.9650
Peer-review started: June 24, 2016
First decision: August 8, 2016
Revised: August 17, 2016
Accepted: August 30, 2016
Article in press: August 30, 2016
Published online: November 21, 2016
Processing time: 148 Days and 23.6 Hours
Choroidal and skin metastasis of colon cancer is rare. In women, the frequency of cutaneous metastasis from colon cancer as the primary lesion in is 9% and skin metastasis occurs in 0.81% of all colorectal cancers. We report a patient with colonic adenocarcinoma who presented with visual disorder in her right eye and scalp pain as her initial symptoms. Contrast-enhance orbital magnetic resonance imaging with fat suppression revealed an infrabulbar mass, and skin biopsy of the posterior parietal scalp confirmed adenocarcinoma. These symptoms were diagnosed as being caused by choroidal and skin metastases of colonic adenocarcinoma. We started palliative chemotherapy with oral capecitabine (1000 mg/m2, twice a day, on days 1-14) every 3 wk, which was effective at shrinking the brain masses and improving the visual disorder. This is the first report that capecitabine is effective at reducing a choroidal and cutaneous metastatic lesion from right-sided colorectal cancer.
Core tip: This case report describes a rare choroidal and skin metastasis of colon cancer and demonstrates that capecitabine is effective at reducing a choroidal and skin metastatic lesion from right-sided colorectal cancer.
- Citation: Ha JY, Oh EH, Jung MK, Park SE, Kim JT, Hwang IG. Choroidal and skin metastases from colorectal cancer. World J Gastroenterol 2016; 22(43): 9650-9653
- URL: https://www.wjgnet.com/1007-9327/full/v22/i43/9650.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i43.9650
Choroidal and skin metastases from colorectal cancer are very rare, and it has never been reported in Korea. The uvea consists of the iris, ciliary body, and choroid. Uveal metastasis is reported in 4% of patients who have a primary cancer in the gastrointestinal tract. Metastasis has been found in the iris in 90 (9%), the ciliary body in 22 (2%), and the choroid in 838 (88%) of the 950 metastatic foci in the uvea[1]. Choroidal metastasis from colon cancer has only been reported in 14 cases in the literature, and the frequency of skin metastasis in colorectal carcinoma has been reported in only 2.3%-6% of cases. Here, we report a patient with colon cancer who presented with visual disturbance and a palpable mass in her scalp.
A 78-year-old woman visited our hospital in May 2013 complaining of epigastric pain and indigestion. To evaluate these problems, a biopsy was conducted by gastroduodenoscopy and colonoscopy, and colon cancer was diagnosed with no metastasis (cT2N1M0). Laparoscopic right colectomy was performed, and stage IIA (pT3N0M0) colon cancer was determined. The final pathological findings revealed no residual tumor cells in the colon and no metastasis in the lymph nodes (0/19).
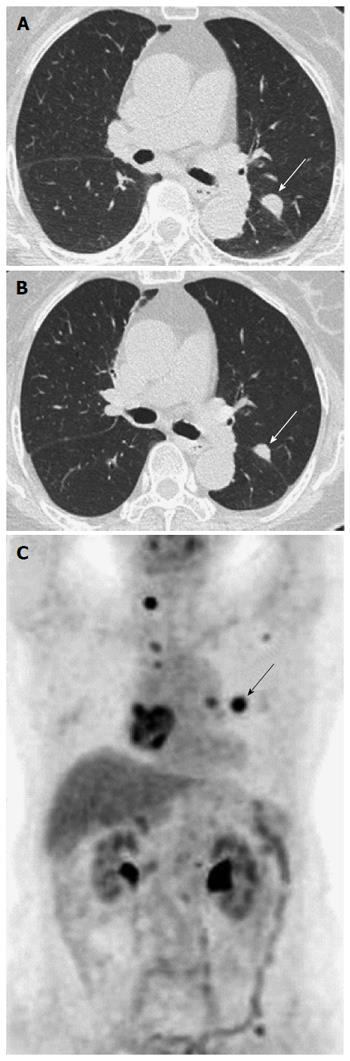
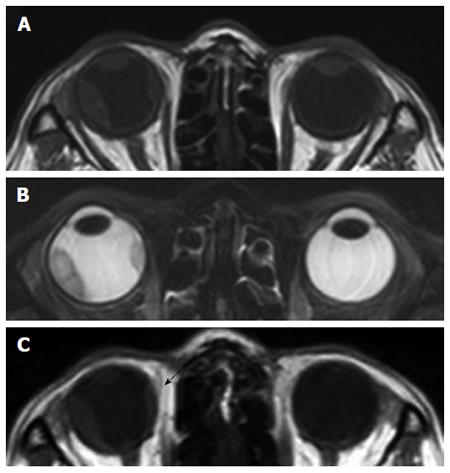
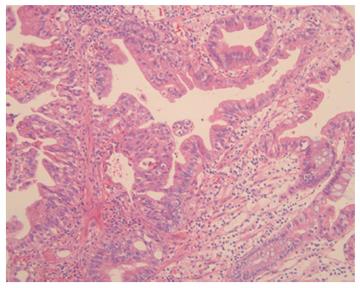
The patient received postoperative adjuvant chemotherapy with 5-fluorouracil plus leucovorin for 12 cycles. Six months after adjuvant chemotherapy, chest computed tomography (CT) revealed a 4-mm enhanced lung nodule that remained aggravated for 3 mo. Hematogenous lung metastasis was identified by 18F-fluorodeoxyglucose-positron emission tomography/computed tomography (Figure 1). At the same time, the patient complained about visual disturbances and multiple flesh-colored palpable masses on her scalp (Figure 2). Orbit CT and magnetic resonance imaging (MRI) revealed intraocular enhancing masses located nasally and temporally in the right eye, with a diagnosis of choroidal metastasis (Figure 3). Brain MRI was performed to evaluate the palpable mass in her scalp, obtaining enhancing lesions in the right parietal and posterior parietal scalp. Adenocarcinoma was confirmed by skin biopsy (Figure 4). Thus, we made a final diagnosis of stage IV colon cancer with multiple metastases (scalp, right choroid, and lung).
We started palliative chemotherapy with oral capecitabine (1000 mg/m2, twice a day, on days 1 -14) every 3 wk[2], which was effective at shrinking the brain masses and improving the visual disorder (Figure 3C). After 8 mo, the level of serum carcinoembryonic antigen was elevated from 2.83 ng/mL to 4.61 ng/mL. All the masses had increased in size, and disease progression was confirmed. Although second-line chemotherapy was administered, the disease was worsening. The patient consequently died.
Choroidal and skin metastases from colorectal cancer are a rare event. When it is present, the metastasis suggests dissemination of the disease and a poor prognosis. However, palliative chemotherapy can be an effective method of treatment for these metastases. The median survival time for patients with ocular metastasis due to cancer is 7.4 mo from the time of ocular operation[3].
The frequency of skin metastasis is relatively low and varies with gender according to the type of underlying malignancy. The most common origins of skin metastasis in women[4] are breast cancer, colon cancer, melanoma, ovarian cancer and lung cancer. In women, the frequency of colon cancer as the primary lesion in skin metastasis is 9%[5], and skin metastasis occurs in 0.81% of all colorectal cancer[6].
In this case, we could not pathologically diagnose the choroidal tumor of this patient as a metastatic tumor. Because the posterior choroid is particularly susceptible to the hematogenous dissemination of cancer cells due to its high vascularity, melanomas and metastatic tumors are typically the most common malignant choroid tumors[7]. Therefore, we need to differentiate between melanomas and metastatic tumors. MRI of the orbits demonstrated a well-circumscribed subretinal mass. The lesion was hypointense on the T1-weigthed image without enhancement of the mass and hyperintense on the T2-weighted image. The MRI findings were compatible with a metastatic tumor and not melanoma[8].
Regarding the treatment of choroidal metastasis, systemic chemotherapy[9], radiotherapy[10], chemoradiotherapy, and intravitreal bevacizumab therapy[11] have all been reported. However, the current literature has few recommendations on the appropriate treatment of choroidal metastasis from colorectal cancer. In our case, capecitabine was effective for the choroidal metastasis. And the patients with KRAS wild type, was not administered in anti-EGFR therapy (panitumumab, cetuximab) insurance issues in Korea.
In summary, choroidal or cutaneous metastasis of colon cancer is rare. We report a patient with colon adenocarcinoma who presented with both choroidal and cutaneous metastases of colon cancer as her initial symptoms. This is the first report that capecitabine is effective at reducing a choroidal and cutaneous metastatic lesion from colorectal cancer.
A 78-year-old woman with stage IIA colon cancer performed laparoscopic right colectomy and adjuvant chemotherapy 1 years ago, complained about visual disturbances and multiple flesh-colored palpable masses on her scalp.
The patient had impaired the visual field, and palpable mass on her scalp was non tenderness.
Metastatic colon cancer, Melanoma.
Serum carcinoembryonic antigen was elevated.
Chest computed tomography revealed a 4-mm enhanced lung nodule that remained aggravated and orbital magnetic resonance imaging (MRI) showed a right infrabulbar mass of 12 mm × 5 mm.
Adenocarcinoma from colon cancer.
Palliative chemotherapy with oral capecitabine (1000 mg/m2, twice a day, on days 1-14) every 3 wk.
Choroidal or cutaneous metastasis of colon cancer is rare. This is entity is commonly confused for melanoma and choroidal metastasis from colorectal cancer.
KRAS known as V-Ki-ras2 Kirsten rat sarcoma viral oncogene is a GTPase that in humans is encoded by the KRAS gene. KRAS mutation is predictive of a very poor response to anti-EGFR therapy (panitumumab, cetuximab) in colorectal cancer.
This is commonly confused for melanomas and metastatic tumors in orbit mass. MRI of the orbits demonstrated a well-circumscribed subretinal mass. The lesion was hypointense on the T1-weigthed image without enhancement of the mass and hyperintense on the T2-weighted image. It means not melanoma but metastatic colon cancer.
The authors describe differential diagnosis and treatment of choroidal and skin metastasis from colorectal cancer. Images of the choroidal finding (diagnosis ex juvantibus) are rare and of interest.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: South Korea
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Kleeff J, Lakatos PL, Sunakawa Y S- Editor: Yu J L- Editor: A E- Editor: Zhang FF
| 1. | Shields CL, Shields JA, Gross NE, Schwartz GP, Lally SE. Survey of 520 eyes with uveal metastases. Ophthalmology. 1997;104:1265-1276. [PubMed] |
| 2. | Tol J, Koopman M, Cats A, Rodenburg CJ, Creemers GJ, Schrama JG, Erdkamp FL, Vos AH, van Groeningen CJ, Sinnige HA. Chemotherapy, bevacizumab, and cetuximab in metastatic colorectal cancer. N Engl J Med. 2009;360:563-572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1000] [Cited by in RCA: 998] [Article Influence: 62.4] [Reference Citation Analysis (0)] |
| 3. | Ferry AP, Font RL. Carcinoma metastatic to the eye and orbit. I. A clinicopathologic study of 227 cases. Arch Ophthalmol. 1974;92:276-286. [PubMed] |
| 5. | Brownstein MH, Helwig EB. Patterns of cutaneous metastasis. Arch Dermatol. 1972;105:862-868. [PubMed] |
| 6. | Hu SC, Chen GS, Wu CS, Chai CY, Chen WT, Lan CC. Rates of cutaneous metastases from different internal malignancies: experience from a Taiwanese medical center. J Am Acad Dermatol. 2009;60:379-387. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 160] [Article Influence: 9.4] [Reference Citation Analysis (1)] |
| 7. | Tong KA, Osborn AG, Mamalis N, Harrie RP, Call NB. Ocular melanoma. AJNR Am J Neuroradiol. 1993;14:1359-1366. [PubMed] |
| 8. | Peyster RG, Augsburger JJ, Shields JA, Hershey BL, Eagle R, Haskin ME. Intraocular tumors: evaluation with MR imaging. Radiology. 1988;168:773-779. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 67] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 9. | Cole MD, Farah NB. The choroid--an unusual site for metastasis in patients with adenocarcinoma of the rectum--a case report. Eur J Surg Oncol. 1985;11:275-278. [PubMed] |
| 10. | Linares P, Castanon C, Vivas S, Diz P, Garcia-Palomo A, Llano C, Olcoz JL. Bilateral choroidal metastasis as the initial manifestation of a rectal cancer. J Gastroenterol Hepatol. 2004;19:726-727. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Lin CJ, Li KH, Hwang JF, Chen SN. The effect of intravitreal bevacizumab treatment on choroidal metastasis of colon adenocarcinoma--case report. Eye (Lond). 2010;24:1102-1103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 30] [Article Influence: 1.9] [Reference Citation Analysis (0)] |