Published online Jun 7, 2016. doi: 10.3748/wjg.v22.i21.5132
Peer-review started: January 10, 2016
First decision: February 18, 2016
Revised: February 24, 2016
Accepted: March 18, 2016
Article in press: March 18, 2016
Published online: June 7, 2016
Processing time: 141 Days and 18.2 Hours
We report a successful endoscopic ultrasonography-guided drainage of a huge infected multilocular walled-off necrosis (WON) that was treated by a modified single transluminal gateway transcystic multiple drainage (SGTMD) technique. After placing a wide-caliber fully covered metal stent, follow-up computed tomography revealed an undrained subcavity of WON. A large fistula that was created by the wide-caliber metal stent enabled the insertion of a forward-viewing upper endoscope directly into the main cavity, and the narrow connection route within the main cavity to the subcavity was identified with a direct view, leading to the successful drainage of the subcavity. This modified SGTMD technique appears to be useful for seeking connection routes between subcavities of WON in some cases.
Core tip: Walled-off necrosis (WON) remains difficult to endoscopically manage because of insufficient drainage of solid necrotic tissues. Here, we present a case of successful drainage of a huge WON via a modified single transluminal gateway transcystic multiple drainage technique. After placing a wide-caliber covered metal stent, follow-up computed tomography revealed an undrained subcavity of WON. A large fistula created by the metal stent enabled the insertion of an upper endoscope directly into the main cavity, and the narrow connection route within the main cavity to the subcavity was identified with a direct view, leading to the successful drainage of the subcavity.
- Citation: Minaga K, Kitano M, Imai H, Yamao K, Kamata K, Miyata T, Matsuda T, Omoto S, Kadosaka K, Yoshikawa T, Kudo M. Modified single transluminal gateway transcystic multiple drainage technique for a huge infected walled-off pancreatic necrosis: A case report. World J Gastroenterol 2016; 22(21): 5132-5136
- URL: https://www.wjgnet.com/1007-9327/full/v22/i21/5132.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i21.5132
Endoscopic ultrasonography (EUS)-guided drainage for pancreatic fluid collection (PFC) is increasingly used as a minimally invasive alternative to surgical and percutaneous drainage[1-3]. However, walled-off necrosis (WON) remains difficult to endoscopically manage because of insufficient drainage of solid necrotic tissues. Various techniques, such as the use of wide-caliber metal stents[4,5], direct endoscopic necrosectomy[6,7] and multiple transluminal gateway technique[8] are reportedly useful for managing WON. However, responses to these advanced techniques remain unsatisfactory in some cases. Recently, a single transluminal gateway transcystic multiple drainage (SGTMD) was developed for treating complicated multilocular WON[9]. Here, we present a case of successful endoscopic drainage of a huge infected multilocular WON via a modified SGTMD technique.
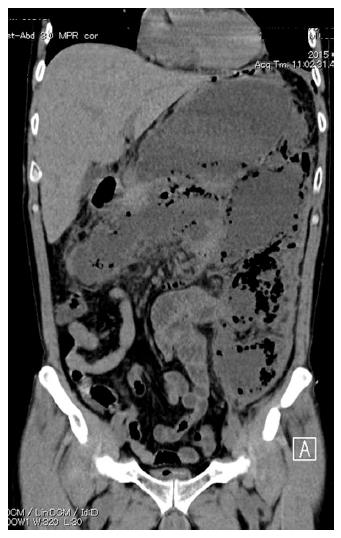
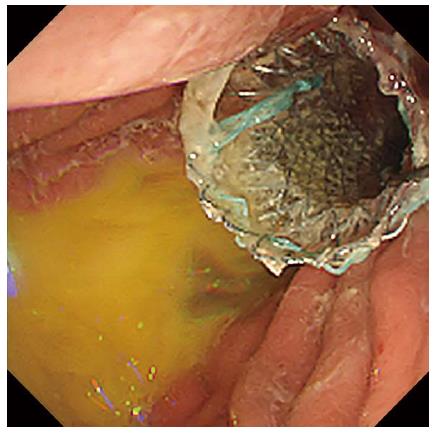
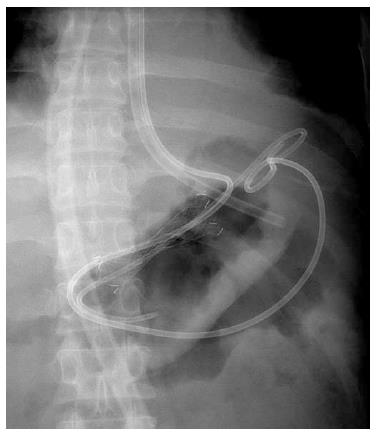
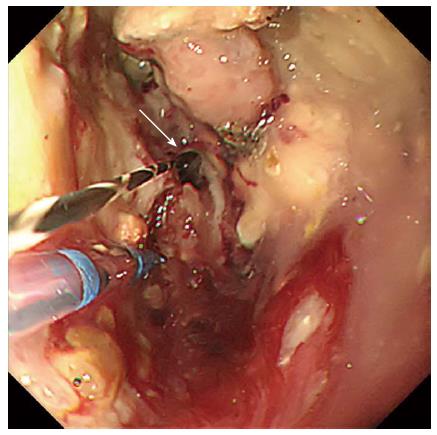
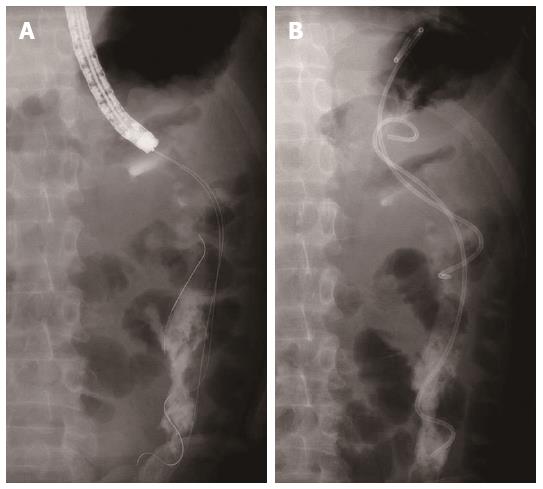
A 49-year-old male presented with upper abdominal pain and high fever of 7 d duration. He was diagnosed with alcohol-induced severe acute pancreatitis 1 mo before and was discharged 6 d after admission from a neighbouring general hospital. His computed tomography (CT) severity index[10] was 6. He was re-admitted to our hospital with the above-mentioned chief complaints. Laboratory tests revealed elevated C-reactive protein (CRP) and procalcitonin levels (27.8 mg/dL and 6.17 ng/mL, respectively). Elevated levels of kidney function parameters were also noted (blood urea nitrogen level, 77 mg/dL; serum creatinine level, 3.14 mg/dL). An abdominal CT revealed a huge multilocular WON measuring 31 cm × 16 cm, which spread from the pancreas to pelvis (Figure 1). Clinically, infection of the necrosis was assumed. Doripenem was intravenously introduced; however, his clinical symptoms and elevated inflammatory reaction persisted. As the main cavity of WON was close to the gastric lumen, we decided to puncture WON under EUS guidance. EUS-guided transluminal drainage was performed; a wide-caliber fully covered TTS Niti-S esophageal stent (internal diameter, 16 mm; maximum flange diameter, 24 mm; length, 40 mm; Taewoong Medical, Seoul, South Korea) was placed (Figure 2). Through the metal stent, a 7-Fr double-pigtail plastic stent (length, 80 mm) and a 7-Fr nasocystic catheter were inserted (Figure 3). During the procedure, approximately 2.4 L of purulent fluid were suctioned. A follow-up abdominal CT obtained 1 wk after the procedure demonstrated a significant reduction in the size of the main cavity; however, the undrained subcavity remained, which was mainly located in the left anterior pararenal space and extended to the left pelvis (Figure 4). Additional drainage targeting the subcavity was required because high fever continued after the procedure. Because the subcavity was not adjacent to the stomach or duodenum, additional EUS-guided puncture was difficult. CT suggested communication between the subcavity and main cavity; therefore, a SGTMD procedure was considered. Repeated attempts to determine the connection route within the main cavity to the subcavity using an ERCP catheter and 0.025-inch guidewire were unsuccessful. The metal stent was removed, and a large fistula that was created by the metal stent enabled the insertion of a forward-viewing upper endoscope directly into the main cavity. After the endoscope was advanced into the cavity, a narrow connection route was identified (Figure 5). Contrast medium was injected into the connection. Having confirmed the detection of the subcavity, the guidewire was inserted into the cavity and two 7-Fr double-pigtail plastic stents (lengths, 120 and 80 mm, respectively) were deployed (Figure 6). No procedure-related complications were observed. After additional endoscopic management, high fever resolved over the course of a few days and CRP levels significantly decreased. CT revealed that the subcavity of WON was well drained. The patient completely recovered and was discharged after 3 wk of hospitalization. Follow-up CT obtained 1 month after discharge revealed that WON had mostly collapsed (Figure 7) and the patient remained symptom free.
Over the last decade, techniques for pancreatic fluid collection have shifted toward minimally invasive approaches. Since first reported in 1992 by Grimm et al[1] EUS-guided transluminal drainage for pancreatic fluid collection has played a pivotal role and spread worldwide as a minimally invasive alternative to surgical and percutaneous drainage[1-3]. However, the clinical response rate of the conventional single transluminal gateway technique deploying single or multiple stenting for treating WON is not satisfactory (described as 45%-63%)[8,11]. Recently, various techniques, such as the use of wide-caliber metal stents[4,5], direct endoscopic necrosectomy[6,7] and multiple transluminal gateway technique[8] have improved the clinical success rate of endoscopic management of WON. However, response to these advanced techniques remains unsatisfactory in some cases. Mukai et al[9] recently described a novel SGTMD procedure for complicated multilocular WON and reported successful drainage in five cases using this technique. When subcavities are located far from the gastrointestinal lumen, percutaneous approach would have been used conventionally. Mukai et al[9] hypothesized that the multilocular cavity may have originally been unilocular and separated into subcavities with tiny, narrow connections during the process of treatment and collapse. They used an ERCP catheter and soft guidewire to locate tiny, narrow connections. In this case, we repeatedly attempted to identify the connection using an ERCP catheter and soft guidewire through the metal stent under fluoroscopic guidance, but the guidewire curled up in the main cavity and failed to locate a connection route. Instead, we inserted the upper endoscope into the cavity through the large fistula, which enabled the narrow connection route to be directly observed. The guidewire was easily and safely advanced into the subcavity, and successful drainage of the subcavity was achieved. This is a modified technique of the previously described SGTMD. In addition to SGTMD, having a direct view to identify the connection route may lead to a higher success rate in some cases.
In this case, the pig-tail stents have been left in place during 6 mo follow-up. This is because the previous studies revealed that stent retrieval was associated with higher PFC recurrence rates[12,13].
In conclusion, we presented a case of successful endoscopic drainage of a huge infected multilocular WON by a modified SGTMD technique with direct endoscope insertion into the cavity. This modified SGTMD technique appears to be useful in seeking connection routes between the subcavities of WON and might avoid the requirement for a more invasive drainage procedure, such as endoscopic or surgical necrosectomy.
One month after being diagnosed with alcohol-induced severe acute pancreatitis, a 49-year-old male presented with upper abdominal pain and high fever of 7 d duration.
The patient had upper abdominal pain and high fever.
Pancreatic pseudocyst.
The laboratory findings showed elevated C-reactive protein, procalcitonin levels and renal dysfunction.
Abdominal computed tomography demonstrated a huge multilocular WON measuring 31 cm × 16 cm, which spread from the pancreas to pelvis.
Pathological examination was not performed in this case.
Endoscopic drainage with a modified single transluminal gateway transcystic multiple drainage (SGTMD) technique was performed.
WON remains difficult to endoscopically manage because of insufficient drainage of solid necrotic tissues. Various techniques, such as the use of wide-caliber metal stents, direct endoscopic necrosectomy, multiple transluminal gateway technique and SGTMD technique were developed for treating WON.
Modified SGTMD is a novel alternative technique for drainage of WON which means a single transluminal gateway transcystic multiple drainage with direct endoscope insertion into the cavity.
Modified SGTMD technique appears to be useful in seeking connection routes between the subcavities of WON and might avoid the requirement for a more invasive drainage procedure, such as endoscopic or surgical necrosectomy.
This case report is interesting and well documented.
P- Reviewer: Wronski M S- Editor: Qi Y L- Editor: A E- Editor: Zhang DN
| 1. | Grimm H, Binmoeller KF, Soehendra N. Endosonography-guided drainage of a pancreatic pseudocyst. Gastrointest Endosc. 1992;38:170-171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 194] [Cited by in RCA: 160] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 2. | Park DH, Lee SS, Moon SH, Choi SY, Jung SW, Seo DW, Lee SK, Kim MH. Endoscopic ultrasound-guided versus conventional transmural drainage for pancreatic pseudocysts: a prospective randomized trial. Endoscopy. 2009;41:842-848. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 237] [Cited by in RCA: 217] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 3. | Talreja JP, Shami VM, Ku J, Morris TD, Ellen K, Kahaleh M. Transenteric drainage of pancreatic-fluid collections with fully covered self-expanding metallic stents (with video). Gastrointest Endosc. 2008;68:1199-1203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 123] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 4. | Bapaye A, Itoi T, Kongkam P, Dubale N, Mukai S. New fully covered large-bore wide-flare removable metal stent for drainage of pancreatic fluid collections: results of a multicenter study. Dig Endosc. 2015;27:499-504. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 38] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 5. | Attam R, Trikudanathan G, Arain M, Nemoto Y, Glessing B, Mallery S, Freeman ML. Endoscopic transluminal drainage and necrosectomy by using a novel, through-the-scope, fully covered, large-bore esophageal metal stent: preliminary experience in 10 patients. Gastrointest Endosc. 2014;80:312-318. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 23] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 6. | Seifert H, Wehrmann T, Schmitt T, Zeuzem S, Caspary WF. Retroperitoneal endoscopic debridement for infected peripancreatic necrosis. Lancet. 2000;356:653-655. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 250] [Cited by in RCA: 209] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 7. | Yasuda I, Nakashima M, Iwai T, Isayama H, Itoi T, Hisai H, Inoue H, Kato H, Kanno A, Kubota K. Japanese multicenter experience of endoscopic necrosectomy for infected walled-off pancreatic necrosis: The JENIPaN study. Endoscopy. 2013;45:627-634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 95] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 8. | Varadarajulu S, Phadnis MA, Christein JD, Wilcox CM. Multiple transluminal gateway technique for EUS-guided drainage of symptomatic walled-off pancreatic necrosis. Gastrointest Endosc. 2011;74:74-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 216] [Cited by in RCA: 189] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 9. | Mukai S, Itoi T, Sofuni A, Itokawa F, Kurihara T, Tsuchiya T, Ishii K, Tsuji S, Ikeuchi N, Tanaka R. Novel single transluminal gateway transcystic multiple drainages after EUS-guided drainage for complicated multilocular walled-off necrosis (with videos). Gastrointest Endosc. 2014;79:531-535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 10. | Balthazar EJ, Robinson DL, Megibow AJ, Ranson JH. Acute pancreatitis: value of CT in establishing prognosis. Radiology. 1990;174:331-336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1076] [Cited by in RCA: 960] [Article Influence: 27.4] [Reference Citation Analysis (1)] |
| 11. | Gardner TB, Chahal P, Papachristou GI, Vege SS, Petersen BT, Gostout CJ, Topazian MD, Takahashi N, Sarr MG, Baron TH. A comparison of direct endoscopic necrosectomy with transmural endoscopic drainage for the treatment of walled-off pancreatic necrosis. Gastrointest Endosc. 2009;69:1085-1094. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 150] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 12. | Arvanitakis M, Delhaye M, Bali MA, Matos C, De Maertelaer V, Le Moine O, Devière J. Pancreatic-fluid collections: a randomized controlled trial regarding stent removal after endoscopic transmural drainage. Gastrointest Endosc. 2007;65:609-619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 198] [Cited by in RCA: 184] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 13. | Bang JY, Wilcox CM, Trevino J, Ramesh J, Peter S, Hasan M, Hawes RH, Varadarajulu S. Factors impacting treatment outcomes in the endoscopic management of walled-off pancreatic necrosis. J Gastroenterol Hepatol. 2013;28:1725-1732. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 67] [Article Influence: 5.6] [Reference Citation Analysis (0)] |