Published online May 7, 2016. doi: 10.3748/wjg.v22.i17.4416
Peer-review started: December 24, 2015
First decision: January 13, 2016
Revised: January 22, 2016
Accepted: February 22, 2016
Article in press: February 22, 2016
Published online: May 7, 2016
Processing time: 128 Days and 7 Hours
An inverted Meckel’s diverticulum is a rare gastrointestinal congenital anomaly that is difficult to diagnose prior to surgery and presents with anemia, abdominal pain, or intussusception. Here, we report the case of 57-year-old men with an inverted Meckel’s diverticulum, who was preoperatively diagnosed using double-balloon enteroscopy. He had repeatedly experienced epigastric pain for 2 mo. Ultrasonography and computed tomography showed intestinal wall thickening in the pelvis. Double-balloon enteroscopy via the anal route was performed for further examination, which demonstrated an approximately 8-cm, sausage-shaped, submucosal tumor located approximately 80 cm proximal to the ileocecal valve. A small depressed erosion was observed at the tip of this lesion. Forceps biopsy revealed heterotopic gastric mucosa. Thus, the patient was diagnosed with an inverted Meckel’s diverticulum, and single-incision laparoscopic surgery was performed. This case suggests that an inverted Meckel’s diverticulum should be considered as a differential diagnosis for a submucosal tumor in the ileum. Balloon-assisted enteroscopy with forceps biopsy facilitate a precise diagnosis of this condition.
Core tip: An inverted Meckel’s diverticulum is a rare congenital anomaly of the gastrointestinal tract which is difficult to diagnose prior to surgery. This case report represents the utility of double-balloon enteroscopy for the precise preoperative diagnosis of an inverted Meckel’s diverticulum.
- Citation: Takagaki K, Osawa S, Ito T, Iwaizumi M, Hamaya Y, Tsukui H, Furuta T, Wada H, Baba S, Sugimoto K. Inverted Meckel’s diverticulum preoperatively diagnosed using double-balloon enteroscopy. World J Gastroenterol 2016; 22(17): 4416-4420
- URL: https://www.wjgnet.com/1007-9327/full/v22/i17/4416.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i17.4416
Meckel’s diverticulum is a common asymptomatic congenital, gastrointestinal anomaly that is a remnant of the omphalomesenteric duct[1]. The incidence of Meckel’s diverticulum was between 0.3%-4% in an autopsy series[1-3]. This anomaly may present as an inverted diverticulum causing anemia, abdominal pain, or intussusception[4]. Small bowel series and abdominal computed tomography (CT) scans have been used for the diagnosis of an inverted Meckel’s diverticulum. However, the preoperative diagnosis of an inverted Meckel’s diverticulum is difficult because the clinical and imaging features overlap with those of other etiologies or acute abdomen or gastrointestinal bleeding[5]. The final diagnosis is often made either intra-operatively or based on postoperative pathology reports. A recent advance in diagnostic methods involves balloon-assisted enteroscopy, which enables both the endoscopic observation of the entire small intestine as well as biopsy collection[6-8]. Here we report the rare case of a 57-year-old man with an inverted Meckel’s diverticulum that was preoperatively diagnosed using double-balloon enteroscopy.
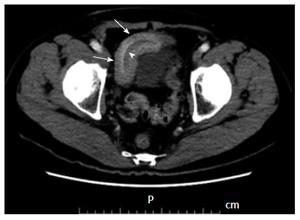
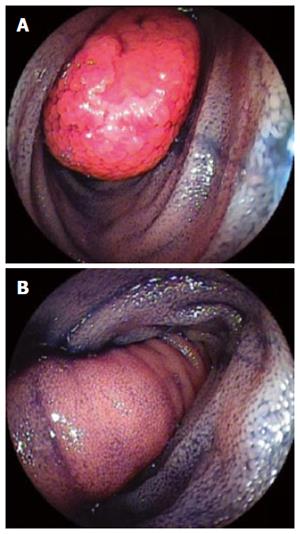
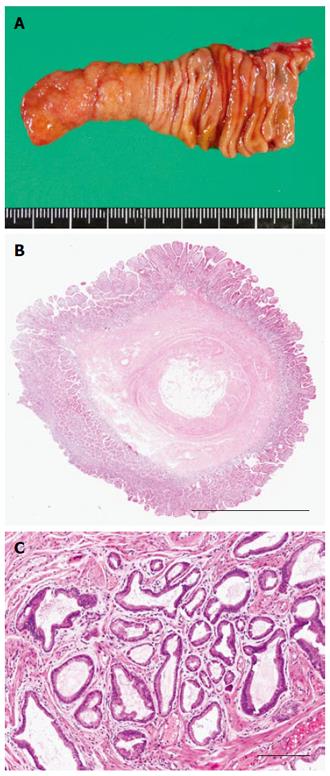
A 57-year-old man who had been repeatedly experiencing epigastric pain for 2 mo consulted at a clinic. He was then referred to another hospital due to a thickened intestinal wall observed on abdominal ultrasonography. His past medical history included depression and a gallbladder polyp treated by cholecystectomy. Physical examination and laboratory findings were unremarkable. An abdominal contrast-enhanced CT also showed a thickened small intestinal wall, with an elongated, intraluminal, fat-attenuating lesion in the lower abdomen (Figure 1). An upper gastrointestinal endoscopy and total colonoscopy were performed, but no abnormalities were found within the observed area. The patient was subsequently referred to our hospital for further examination. Retrograde double-balloon enteroscopy (DBE) was performed, which demonstrated an 8-cm, sausage-shaped, polypoid lesion that was located approximately 80 cm proximal to the ileocecal valve. A small depressed erosion was seen at the tip of the polypoid lesion, and intestinal villous mucosa was seen on the surface of the lesion (Figure 2). Using selective contrast-enhanced radiography with DBE, an elongated polypoid lesion was demonstrated in the ileum (Figure 3). Although Tc-99m pertechnetate scintigraphy was negative, a forceps biopsy from the tip of the depressed lesion revealed heterotopic gastric mucosa. The patient was diagnosed with an inverted Meckel’s diverticulum, and he underwent single-incision laparoscopic surgery 3 mo later. An excavation of the serosa was observed at the basal region of the polypoid lesion by laparoscopy. After a Hutchinson’s maneuver, segmental resection was performed. Pathological examination of the specimen revealed an 8.0 cm × 1.4 cm, sausage-shaped, polypoid lesion. Histological examination showed heterotopic gastric mucosa mimicking the pyloric glands at the tip of the lesion (Figure 4). The patient was discharged on post-operative day 6 without complications.
A Meckel’s diverticulum is usually an asymptomatic condition, and many cases are incidentally discovered during a radiographic evaluation or during surgery performed for other reasons[1]. This condition causes symptoms in 4%-30% of patients[9], and possible complications include hemorrhage, bowel obstruction with or without intussusception, diverticulitis, and inversion. According to a recent report, the most common complaint in an inverted Meckel’s diverticulum is bleeding (80%), followed by anemia (78%) and abdominal pain (68%)[4]. The radiological features of an inverted Meckel’s diverticulum are similar to that of a pedunculated intraluminal polyp, especially lipoma. Small bowel series reveal an elongated, smoothly margined, intraluminal mass that parallels the long axis of the intestine and frequently has a bulbous or club-sharped tip. Abdominal CT shows typical inverted cases as having a central core of fat attenuation[1].
This case seemed difficult to diagnose prior to surgery because the symptoms were mild and non-specific. Nevertheless, we could preoperatively diagnose the inverted Meckel’s diverticulum using DBE. Recently, the reports of Meckel’s diverticulum diagnosed using DBE are increasing[8]. DBE was developed by Yamamoto et al[6,7] in 2000 for the diagnosis and treatment of small intestinal disease. DBE is quite useful for diagnosis because it enables a biopsy of the entire small intestine[6]. Heterotopic gastric mucosa reportedly occurred in up to 50% of Meckel’s diverticulum and up to 80% of symptomatic patients[10]. Heterotopic pancreatic tissue was also found in 5%-16% of cases[1,11]. Meckel’s diverticulum is typically located on the antimesenteric side of the distal ileum, within 20-100 cm proximal to the ileocecal valve[1]. Therefore, retrograde DBE is particularly recommended to diagnose Meckel’s diverticulum[8,12].
The mechanism of inversion is not clearly understood. Levy et al[1] reported that 21% cases of Meckel’s diverticulum were found to be inverted in the lumen of the small intestine. One theory is that abnormal peristaltic movement in proximity to the Meckel’s diverticulum may cause it to invert[11,12]. Another theory is that because Meckel’s diverticulum is not fixed to the mesentery or the intestine, it increases the likelihood of an inversion[4]. The mesenteric fat of the Meckel’s diverticulum is pulled into the center of the diverticulum as it inverts in the small intestinal lumen. When the diverticulum is inverted, it may cause not only intestinal obstruction but also intussusception[1,4].
The preferred treatment for symptomatic Meckel’s diverticulum is surgery. Whenever an inverted Meckel’s diverticulum is diagnosed either pre-operatively or intra-operatively, the surgical procedure should be segmental resection. Laparoscopic resection is a safe and less invasive surgical procedure[1,4]. In this case, single-incision laparoscopic surgery was performed, which is a minimal access technique that can yield a reduction in scarring and consequently pain and suffering of the patients. Asymptomatic diverticula that are incidentally discovered remains controversial to date. The lifetime risk of developing complications is 4% up to the age of 20 years, 2% up to the age of 40 years, and 0% in the elderly population[1,4]. Therefore, preventive resection is recommended for patients younger than 40 years; for a diverticulum longer than 2 cm; diverticula with narrow necks, fibrous bands, or heterotopic gastric mucosa; or when the diverticula appears thickened and inflamed[4].
In the present case, an inverted Meckel’s diverticulum with heterotopic gastric mucosa was clearly viewed using double-balloon enteroscopy. Therefore, an inverted Meckel’s diverticulum should be considered as a differential diagnosis for a submucosal tumor in the ileum. Balloon-assisted enteroscopy combined with forceps biopsy enables a precise preoperative diagnosis.
A 57-year-old man had repeatedly experienced epigastric pain for 2 mo.
Physical examinations were unremarkable.
Intestinal submucosal tumors: especially lipoma.
All laboratory tests were within normal limits.
An abdominal contrast-enhanced computed tomography showed a thickened small intestinal wall, with an elongated, intraluminal, fat-attenuating lesion in the ileum, and retrograde double-balloon enteroscopy (DBE) demonstrated a sausage-shaped, polypoid lesion that was located approximately 80 cm proximal to the ileocecal valve. A small depressed erosion was seen at the tip of the polypoid lesion.
Histological examination showed that the diverticulum was composed of all layers of the intestinal wall, and heterotopic gastric mucosa was seen at the tip of the lesion.
Single-incision laparoscopic surgery was performed.
Although the reports of Meckel’s diverticulum diagnosed using DBE are increasing, those of inverted situation is rare. DBE is quite useful for diagnosis.
An inverted Meckel’s diverticulum is a condition where the Meckel’s diverticulum literally inverts intraluminally on itself.
An inverted Meckel’s diverticulum is a rare congenital anomaly of the gastrointestinal tract which is difficult to diagnose prior to surgery. This case report represents the utility of double-balloon enteroscopy with biopsy for the precise preoperative diagnosis of an inverted Meckel’s diverticulum.
The authors present a case report of inverted Meckel’s diverticulum diagnosed pre-operatively. The report is well written.
P- Reviewer: Pinho R S- Editor: Ma YJ L- Editor: A E- Editor: Liu XM
| 1. | Levy AD, Hobbs CM. From the archives of the AFIP. Meckel diverticulum: radiologic features with pathologic Correlation. Radiographics. 2004;24:565-587. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 191] [Cited by in RCA: 177] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 2. | Park JJ, Wolff BG, Tollefson MK, Walsh EE, Larson DR. Meckel diverticulum: the Mayo Clinic experience with 1476 patients (1950-2002). Ann Surg. 2005;241:529-533. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 347] [Cited by in RCA: 371] [Article Influence: 18.6] [Reference Citation Analysis (0)] |
| 3. | Sagar J, Kumar V, Shah DK. Meckel‘s diverticulum: a systematic review. J R Soc Med. 2006;99:501-505. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 4. | Rashid OM, Ku JK, Nagahashi M, Yamada A, Takabe K. Inverted Meckel’s diverticulum as a cause of occult lower gastrointestinal hemorrhage. World J Gastroenterol. 2012;18:6155-6159. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 24] [Cited by in RCA: 26] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 5. | Kopácová M, Vykouril L, Vacek Z, Tycová V, Bártová J, Rejchrt S, Bures J. Inverted Meckel’s diverticulum with ectopic pancreatic tissue as a source of severe gastrointestinal bleeding. J Gastrointest Surg. 2010;14:578-581. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 6. | Yamamoto H, Sugano K. A new method of enteroscopy--the double-balloon method. Can J Gastroenterol. 2003;17:273-274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 7. | Shinozaki S, Yamamoto H, Ohnishi H, Kita H, Yano T, Iwamoto M, Miyata T, Hayashi Y, Sunada K, Ido K. Endoscopic observation of Meckel’s diverticulum by double balloon endoscopy: report of five cases. J Gastroenterol Hepatol. 2008;23:e308-e311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Fukushima M, Kawanami C, Inoue S, Okada A, Imai Y, Inokuma T. A case series of Meckel’s diverticulum: usefulness of double-balloon enteroscopy for diagnosis. BMC Gastroenterol. 2014;14:155. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 32] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 9. | Heider R, Warshauer DM, Behrns KE. Inverted Meckel‘s diverticulum as a source of chronic gastrointestinal blood loss. Surgery. 2000;128:107-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Puligandla PS, Becker L, Driman D, Prokopiw I, Taves D, Davies ET. Inverted Meckel’s diverticulum presenting as chronic anemia: case report and literature review. Can J Surg. 2001;44:458-459. [PubMed] |
| 11. | Kim JH, Park SH, Ha HK. Case 156: Inverted Meckel diverticulum. Radiology. 2010;255:303-306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 12. | Blakeborough A, McWilliams RG, Raja U, Robinson PJ, Reynolds JV, Chapman AH. Pseudolipoma of inverted Meckel’s diverticulum: clinical, radiological and pathological correlation. Eur Radiol. 1997;7:900-904. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 23] [Article Influence: 0.8] [Reference Citation Analysis (0)] |