Published online May 7, 2016. doi: 10.3748/wjg.v22.i17.4411
Peer-review started: December 11, 2015
First decision: January 13, 2016
Revised: January 26, 2016
Accepted: February 22, 2016
Article in press: February 22, 2016
Published online: May 7, 2016
Processing time: 140 Days and 13.1 Hours
Sub capsular hepatic haematoma is a rare complication after endoscopic retrograde cholangiopancreatography (ERCP). Exact pathological mechanism is still unclear and few reports are nowadays available in literature. We report the case of a 58-year-old woman with recurrent episodes of upper abdominal pain, nausea and vomiting. On the basis of laboratory exams, abdomen ultrasound and magnetic resonance imaging she was diagnosed with a common bile duct stone. Endoscopic biliary sphincterotomy was performed. On the following day the patient complaint severe abdominal pain with rebound and hemodynamic instability. A computed tomography scan reveal a 14 cm × 6 cm × 19 cm sub-capsular hepatic haematoma on the right lobe that was successfully managed via percutaneous embolization. Sub capsular liver haematoma is a rare life threatening complication after ERCP that should be managed according to patients’ haemodynamic and clinic.
Core tip: Hepatic hematoma is a rare and potentially life threatening complication after endoscopic retrograde cholangiopancreatography (ERCP). Despite its severity, only few cases are described in current literature. The paper describe the management of a huge right lobe hepatic hematoma following ERCP. An exhaustive literature analysis is made considering, signs and symptoms at presentation, time of presentation, diagnosis, and treatment. Awareness of this potential complication, high level of suspicion and prompt treatment are at the basis of better outcomes in such patients.
- Citation: Zappa MA, Aiolfi A, Antonini I, Musolino CD, Porta A. Subcapsular hepatic haematoma of the right lobe following endoscopic retrograde cholangiopancreatography: Case report and literature review. World J Gastroenterol 2016; 22(17): 4411-4415
- URL: https://www.wjgnet.com/1007-9327/full/v22/i17/4411.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i17.4411
Endoscopic retrograde cholangiopancreatography (ERCP) is a minimally invasive procedure for diagnosis and treatment of biliary and pancreatic disease. Complications occur in 2.5%-8% of cases with mortality rates ranging from 0.5%-1.0%[1]. Pancreatitis, cholangitis, perforation, and bleeding as a result of papillotomy are the most frequently described complications[2-3]. Sub capsular hepatic haematoma is a rare and potential life threatening condition[4]. We report the unusual case of a sub capsular hepatic haematoma after ERCP presenting with abdominal pain and hypotension.
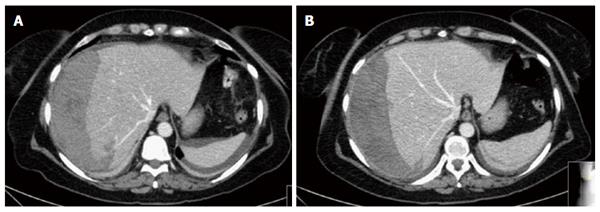
A 58-year-old woman with recurrent episodes of upper abdominal pain was diagnosed with common bile duct stone by abdomen ultrasound and magnetic resonance imaging. She was admitted for ERCP and sphincterotomy. A proper drainage of the common bile duct was performed without complications. 12 h after the procedure the patient complaint a sudden abdominal pain with tenderness and rebound in the upper right quadrant without fever. Laboratory tests revealed a normal white blood cell count (7.44 × 109/L) and haemoglobin level (13.3 g/dL) with a slightly increased C-reactive protein (14.3 mg/dL). Total bilirubin, transaminases and amylases were within normal limits. Abdomen plain film was normal without signs of pneumoperitoneum. On the basis of such symptoms the patient was closely monitored. On the following 12 h she gradually develops hypotension (95/50 mmHg) and tachycardia (115 bpm) with a progressive haemoglobin decrease (8.6 g/dL). Urgent abdomen computed tomography (CT) scan demonstrated a large subcapsular hepatic haematoma of the right hepatic lobe supported by three peripheral parenchymal lacerations with contextual active bleeding and compression of the right and middle hepatic vein (Figure 1). On the basis of laboratory, clinical, and hemodynamic parameters the patient was urgently managed with percutaneous embolization of some small peripheral vessels on the sixth and seventh segment.
The post procedural course was uneventful with restoration of normal haemoglobin levels after transfusion (12.9 g/dL). Six days after embolization an abdomen CT scan shows the stability of the hematoma and the patient was discharged home.
Sub capsular hepatic haematoma is a rare and potentially life threatening complication after ERCP. Probably underestimated, only few cases are nowadays reported in literature and the exact pathological mechanism is unclear (Table 1). Accidental puncture of a peripheral intrahepatic biliar tree with consensual laceration of a small parenchymal vessels by endoscopic guide wire, may explain the phenomenon[2-4].
| Ref. | Indication for ERCP | ERCP | Onset of symptoms | Symptoms | Diagnosis | Dimension | Treatment | Death |
| Ortega Deballon et al[5] | Common bile duct stone | NA | NA | Abdominal pain | NA | NA | Percutaneous drainage | No |
| Horn et al[6] | Pancreatic adenocarcinoma | Cytologic brushing over a 0.035-inch guidewire + biliary stent | 48 h | Abdominal pain/anemia | 48 h; CT scan | NA (right lobe) | Conservative | No |
| Chi et al[7] | Pancreatic cancer | Biliary stent placement over a guidewire | NA | Abdominal pain | NA | NA | Embolization | No |
| Ertuğrul et al[8] | Hilar cholangiocarcinoma | Biliary stent placement over a guidewire | 48 h | Abdominal pain/fever | 48 h, CT scan | 7.8 cm × 4.1 cm (right lobe) | Conservative | No |
| Priego et al[9] | Common bile duct stone | Spincterotomy over a guidewire | NA | Abdominal pain/hypotension/peritonism | NA, CT scan | 4.7 cm × 10 cm × 11 cm (right lobe) | Surgery (Haematoma evacuation) | No |
| Petit-Laurent et al[10] | Common bile duct stone | Spincterotomy over a guidewire | 48 h | Abdominal pain/fever | 48 h; US/CT scan | NA | Percutaneous drainage | No |
| Bhati et al[11] | Common bile duct stone | Spincterotomy over a guidewire | NA | Abdominal pain/hypotension | NA; CT scan | 10 cm × 13 cm (right lobe) | Percutaneous drainage | No |
| Mc Arthur et al[12] | Common bile duct stone | Spincterotomy over a 0.035-ich guidewire + biliary stent | 12 h | Abdominal pain/leucocytosis | 12 h; CT scan | 5 cm × 3 cm (right lobe) | Conservative | No |
| De La Serna-Higuera et al[13] | Common bile duct stone | Spincterotomy over a 0.035-ich guidewire | 48 h | Abdominal pain/leucocytosis | 72 h; abdomen US/ CT scan | 14 cm × 8 cm × 5 cm (right lobe) | Conservative | No |
| Cárdenas et al[14] | bile leak after liver transplantation | Spincterotomy over a guidewire + biliary plastic stent positioning | 24 h | Abdominal pain/anemia | NA, CT scan | NA | Conservative | No |
| Nari et al[15] | Acute biliary pancreatitis | NA | NA | Fever/Abdominal pain | NA; CT scan | NA (right lobe) | Conservative | No |
| Revuelto Rey et al[16] | Common bile duct stone | Spincterotomy | 6 h | Anemia | 6 hours; CT scan | 13 cm × 9 cm × 11 cm (right lobe) | Conservative | No |
| Baudet et al[17] | Common bile duct stone | Spincterotomy over a 0.035-ich guidewire | 24 h | Abdominal pain/anemia/fever/hypotension | 36 h; abdomen US/CT scan | 16 cm × 6 cm, 5 cm × 21 cm (right lobe S6-7-8) | Embolization/surgery (haematoma evacuation) | No |
| Pérez-Legaz et al[18] | Common bile duct stone | Spincterotomy | 2 h | Abdominal pain/anemia/hypotension/peritonism | 2 h; CT scan | 8 cm (S5-6) | Surgery (electrocoagulation) | No |
| Del Pozo et al[19] | Common bile duct stone | Spincterotomy over a 0.035-ich guidewire | 6 h | Abdominal pain | 5 d; CT scan | NA, Right lobe | Conservative | No |
| Orellana et al[4] | Periampullary tumor | Biopsies + biliary plastic stent | 4 h | Abdominal pain | 4 h, CT scan | 17 cm × 13 cm × 5 cm (right lobe) | Conservative | No |
| Biliary stent occlusion | Stent exchange | 2 h | Abdominal pain/hypotension | 2 h; CT scan | Hepatic hematoma covering the 50% of the total hepatic volume + hemoperitoneum | Embolization of the right epatic artery + peritoneal drainage under CT guidance under CT guidance | No | |
| Biliary stent disfunction in a patient affected by gallbladder cancer with consensual malignant biliary obstruction | Biliary plastic stent exchange | NA | Abdominal pain | NA, CT scan | Hepatic hematoma covering the 30% of the total hepatic volume | Conservative | No | |
| Fei et al[1] | Common bile duct stone | Spincterotomy over a 0.035-ich guidewire | 2 h | Fever | 6 d; CT scan | 13 cm × 6 cm (right lobe) | Percutaneous drainage | No |
| Klímová et al[20] | Wirsung stone | NA | 6 h | Abdomial pain/anemia/hypotension | NA | Right lobe | Embolization/surgery/percutaneous drainage | No |
| Zizzo et al[21] | Common bile duct stone | Spincterotomy over a 0.035-ich guidewire | 24 h | Abdominal pain/hypotension/anemia | 36 h; CT scan and angiography | 15 cm × 11 cm (right lobe) | Embolization | No |
| González-López et al[22] | Iatrogenic benign stenosis following laparoscopic cholecistecotmy | Spincterotomy + Pneumatic dilation + biliary stent positioning | 24 h | Abdominal pain/anemia/hypotension/peritonism | 72 h; CT scan | NA (right lobe) | Surgery (damage control and packing) | Yes |
| Present case 2015 | Common bile duct stone | Spincterotomy over a 0.035-ich guidewire | 12 h | Abdominal pain/hypotension/anemia | 24 h; CT scan | 14 cm × 6 cm × 19 cm (right lobe) | Embolization | No |
Sudden abdominal pain whenever associated with hypotension and tachycardia after ERCP should raise the suspicion of intrahepatic bleeding with Glisson’s capsule distension. Different symptoms are described in literature: abdominal pain (91%), anemia (39.1%), hypotension (39.1%), fever (21.7%) and peritonism (13%) (Table 1). Laboratory tests did not provide major indicators of the development of a sub capsular hepatic haematoma, except for a decrease in the haemoglobin level[1]. Imaging modalities (ultrasound and CT) are the gold standard for diagnosis and surveillance of this emergent complication[9,15].
In the present case symptoms and signs started 12 h after the procedure with an early diagnosis and prompt treatment. Aspecific symptoms with a late onset from ERCP may occur with consequent delayed diagnosis and treatment (range 2-144 h) (Table 1).
Different treatment modalities are proposed in literature based on haemodynamic and clinics. The role of imaging in the assessment dimension and of ab extrinsic compression on hepatic vein is an important detail that should kept in mind whenever approaching such patients.
In stable patients with a limited, peripheral and non-compressive haematoma, a conservative management with prophylactic antibiotics should be suggested. Serial haemoglobin controls and abdomen CT verification is advisable[19]. Percutaneous drainage under CT guide and US should be proposed in case of abscess formation and fever[1].
Whenever hemodynamic instability is present with active bleeding and contrast extravasation, an immediate radiological or surgical approach should be taken into account. Minimally invasive radiological selective peripheral vessels embolization shows high success rates[21]. Surgical management should be reserved in case of general condition deterioration, haemodynamic instability with signs of consensual peritoneal and free abdominal fluid[9]. Surgical approach consist in hematoma evacuation, local haemostasis with electrocoagulation or haemostatic devices, or packing in case of massive haemorrhage[22]. Literature data are in favour with a conservative treatment (43.5%), percutaneous embolization (26%), drainage (17.4%) and surgical management (13%) as a first line treatment. Failure of the first approach occur in 3 different cases (13%) without severe consequences (Table 1). Sudden rupture of the haematoma with consequent haemoperitoneum is a dreaded complications with high risk of mortality if misdiagnosed. González-López et al[22] report the case of a 30 years-old patient with Glisson’s capsule rupture and consequent haemoperitoneum with consequent hypotension and signs of peritonism. The patients was surgically managed with electrocautery and packing without success.
Sub capsular liver haematoma is a rare and potentially life threatening complication following ERCP. Conservative treatment will be sufficient in most hemodinamically stable patients with no signs of super infection or abscess formation. Selective embolization is adequate in case of peripheral small vessels bleeding determining hemodynamic instability. Surgical approach is advisable in case of rupture risk, signs of peritonism and free abdominal fluid. Serial follow up CT scan are essential for dimension monitoring. We recommend that for legal purposes this potential risk should be addressed in the preoperative informed consent.
A 58-year-old woman with recurrent episodes of upper abdominal pain was diagnosed with common bile duct stone by abdomen ultrasound and magnetic resonance imaging and admitted for endoscopic retrograde cholangiopancreatography (ERCP) and sphincterotomy.
Hemodynamic instability, hypotension, and tachycardia were consistent with a post-procedural bleeding.
Papillary bleeding after ERCP is one of the most common complications after the procedure. Splenic rupture, intrahepatic hematoma and visceral abdominal vessels rupture, related to instrumental looping with excessive traction, are exceptionally responsible for such situation.
Laboratory tests did not provide major indicators in development of sub capsular hepatic haematoma.
Abdominal ultrasound and computed tomography (CT) scan are necessary for differential diagnosis.
A large sub capsular hepatic haematoma of the right lobe with active bleeding was evident on CT scan.
On the basis of laboratory, clinical, and hemodynamic parameters the patient was urgently managed with percutaneous embolization of some small peripheral vessels.
Probably underestimated, hepatic hematoma following ERCP is an extremely rare complication with few cases reported in current literature.
Hepatic hematoma is a rare, potentially life threatening complication after ERCP. Awareness of such event is fundamental for early detection, diagnosis and treatment.
This report describe our experience in the management of a large hepatic hematoma after ERCP with an exhaustive literature review. Symptoms and signs at presentation, diagnosis, and management are reviewed in accordance to published literature. Limited number of literature reported cases is the major weakness of this study. Further studies are necessary to investigate the mechanism of injury and appropriate management of such complication.
P- Reviewer: Alimehmeti R, Djodjevic I S- Editor: Qi Y L- Editor: A E- Editor: Wang CH
| 1. | Fei BY, Li CH. Subcapsular hepatic haematoma after endoscopic retrograde cholangiopancreatography: an unusual case. World J Gastroenterol. 2013;19:1502-1504. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 30] [Cited by in RCA: 24] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 2. | Abdel Aziz AM, Lehman GA. Pancreatitis after endoscopic retrograde cholangio-pancreatography. World J Gastroenterol. 2007;13:2655-2668. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 34] [Cited by in RCA: 35] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 3. | Cotton PB, Garrow DA, Gallagher J, Romagnuolo J. Risk factors for complications after ERCP: a multivariate analysis of 11,497 procedures over 12 years. Gastrointest Endosc. 2009;70:80-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 449] [Cited by in RCA: 467] [Article Influence: 29.2] [Reference Citation Analysis (0)] |
| 4. | Orellana F, Irarrazaval J, Galindo J, Balbontin P, Manríquez L, Plass R, Araya R, Ríos H, Sáenz R. Subcapsular hepatic hematoma post ERCP: a rare or an underdiagnosed complication? Endoscopy. 2012;44 Suppl 2 UCTN:E108-E109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | Ortega Deballon P, Fernández Lobato R, García Septiem J, Nieves Vázquez MA, Martínez Santos C, Moreno Azcoita M. Liver hematoma following endoscopic retrograde cholangiopancreatography (ERCP). Surg Endosc. 2000;14:767. [PubMed] |
| 6. | Horn TL, Peña LR. Subcapsular hepatic hematoma after ERCP: case report and review. Gastrointest Endosc. 2004;59:594-596. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Chi KD, Waxman I. Subcapsular hepatic hematoma after guide wire injury during endoscopic retrograde cholangiopancreatography: management and review. Endoscopy. 2004;36:1019-1021. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 20] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Ertuğrul I, Parlak E, Ibiş M, Altiparmak E, Saşmaz N, Sahin B. An unusual complication of endoscopic retrograde cholangiopancreatography. Dig Dis Sci. 2006;51:1167-1168. [PubMed] |
| 9. | Priego P, Rodríguez G, Mena A, Losa N, Aguilera A, Ramiro C, Lisa E, Conde S, Fresneda V. Subcapsular liver hematoma after ERCP. Rev Esp Enferm Dig. 2007;99:53-54. [PubMed] |
| 10. | Petit-Laurent F, Scalone O, Penigaud M, Barbeys J. Subcapsular hepatic hematoma after endoscopic retrograde cholangiopancreatography: case report and literature review. Gastroenterol Clin Biol. 2007;31:750-752. [PubMed] |
| 11. | Bhati CS, Inston N, Wigmore SJ. Subcapsular intrahepatic hematoma: an unusual complication of ERCP. Endoscopy. 2007;39 Suppl 1:E150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 12. | McArthur KS, Mills PR. Subcapsular hepatic hematoma after ERCP. Gastrointest Endosc. 2008;67:379-380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 13. | De La Serna-Higuera C, Fuentes Coronel A, Rodríguez Gómez SJ, Martín Arribas MI. [Subcapsular hepatic hematoma secondary to the use of hydrophilic guidewires during endoscopic retrograde cholangiopancreatography]. Gastroenterol Hepatol. 2008;31:266-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 14. | Cárdenas A, Crespo G, Balderramo D, Bordas JP, Sendino O, Llach J. Subcapsular liver hematoma after Endoscopic Retrograde Cholangiopancreatography in a liver transplant recipient. Ann Hepatol. 2008;7:386-388. [PubMed] |
| 15. | Nari GA, Preciado Vargas J, Rosendo Ballesteros N. A rare complication of ERCP: sub-capsular liver haematoma. Cir Esp. 2009;85:261-262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 16. | Revuelto Rey J, Gordillo Escobar E, Batalha P. [Subcapsular hepatic hematoma after ERCP]. Med Intensiva. 2010;34:224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 17. | Baudet JS, Arguiñarena X, Redondo I, Tadeo E, Navazo L, Mendiz J, Montiel R. [Subcapsular hepatic hematoma: an uncommon complication of endoscopic retrograde cholangiopancreatography]. Gastroenterol Hepatol. 2011;34:79-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 18. | Pérez-Legaz J, Santos J, Ruiz-Tovar J, Moya-Forcén P, Armañanzas L, Gómez M, Oller I, Arroyo A, Calpena R. Subcapsular hepatic hematoma after ERCP (endoscopic retrograde cholangipancreatography). Rev Esp Enferm Dig. 2011;103:550-551. [PubMed] |
| 19. | Del Pozo D, Moral I, Poves E, Sanz C, Martín M. Subcapsular hepatic hematoma following ERCP: case report and review. Endoscopy. 2011;43 Suppl 2 UCTN:E164-E165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 20. | Klímová K, Suárez C, Asanza C, Peña A, Arregui E, Alonso A. Subcapsular hepatic hematoma after ERCP: a case report and revision of literature. Sci Res. 2014;3:161-166. [RCA] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 21. | Zizzo M, Lanaia A, Barbieri I, Zaghi C, Bonilauri S. Subcapsular Hepatic Hematoma After Endoscopic Retrograde Cholangiopancreatography: A Case Report and Review of Literature. Medicine (Baltimore). 2015;94:e1041. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 24] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 22. | González-López R, García-Cano E, Espinosa-González O, Cruz-Salgado Á, Montiel-Jarquin ÁJ, Hernández-Zamora V. Surgical treatment for liver haematoma following endoscopic retrograde cholangiopancreatography; An unusual case. Cir Cir. 2015;83:506-509. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |