Published online Feb 21, 2015. doi: 10.3748/wjg.v21.i7.2178
Peer-review started: June 30, 2014
First decision: July 21, 2014
Revised: August 5, 2014
Accepted: September 18, 2014
Article in press: September 19, 2014
Published online: February 21, 2015
Processing time: 226 Days and 19.3 Hours
AIM: To assess the accuracy of polyp size using an endoscopic lesion measurement system (ELMS).
METHODS: The accuracy of polyp size assessment was compared among measurements acquired by visual estimation, disposable graduated biopsy forceps (DGBF; used as a “scale-plate”) and the ELMS.
RESULTS: There were 192 polyps from 166 cases included in this study. The mean diameter of the post polypectomy measurement was 0.85 ± 0.53 cm (range: 0.2-3.0 cm). The mean diameter by visual estimation was 1.10 ± 0.53 cm, which was significantly different compared to the actual size of the polyp (P < 0.001). The mean diameters obtained using DGBF (0.87 ± 0.54 cm) and ELMS (0.85 ± 0.53 cm) did not significantly differ from the actual size of the polyp. The difference between the measurements from the ELMS and DGBF was not significant.
CONCLUSION: Unlike visual estimations at colonoscopy, endoscopic graduated biopsy forceps and the endoscopic lesion measurement system are accurate methods to estimate polyp size.
Core tip: In this study, we established an endoscopic lesion measurement system (ELMS) to measure polyp size during endoscopy. We measured 192 polyps from 162 patients and found that the accuracy of visual estimation for colonic polyp size is low. The accuracy of estimating polyp size was distinctly increased when measured by disposable graduated biopsy forceps and ELMS. In particular, the accuracy of estimation by ELMS was higher than the clinician’s estimation and DGBF for polyps > 1 cm.
- Citation: Leng Q, Jin HY. Measurement system that improves the accuracy of polyp size determined at colonoscopy. World J Gastroenterol 2015; 21(7): 2178-2182
- URL: https://www.wjgnet.com/1007-9327/full/v21/i7/2178.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i7.2178
Tumor size determined at colonoscopy is associated with the treatment plan developed for the tumor. However, there are currently no standard criteria used for measuring the size of a tumor identified at colonoscopy. Many clinicians evaluate the size of a tumor based on their experience. Sometimes, this type of assessment has been inconsistent with the actual size of the tumor[1]. Morales et al[2] used open biopsy forceps to evaluate the diameter of colon polyps at colonoscopy, and three quarters of the results were inconsistent with the actual results. Eichenseer et al[3] compared the estimated size of 10-25-mm polyps determined at endoscopy by 15 different endoscopists, with the histopathology of post-fixation polyp measurements; the results showed that the mean size variation was 73.6% (range: 13%-127%). The size of approximately 62.6% (range: 0%-91%) of the polyps was incorrectly estimated, overestimated in many cases, which could lead to inappropriate advice concerning the treatment plan. Liu et al[4] developed disposable graduated biopsy forceps (DGBF) that could increase the accuracy of polyp size estimation. However, there continues to be variability, especially for visual estimation of polyps larger than 2 cm. To estimate the size of polyps at colonoscopy more accurately, we designed an endoscopic lesion measurement system (ELMS) using DGBF as a “scale-plate” and assessed its accuracy in a clinical setting.
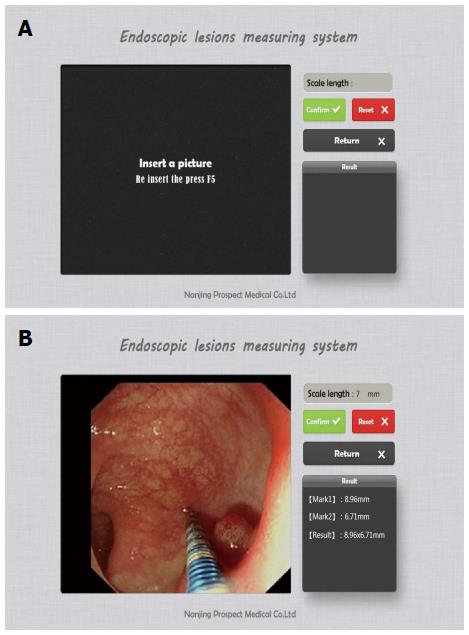
DGBF were used as a “scale-plate” to design the ELMS. When a polyp was observed at colonoscopy, DGBF parallel to the lesion were pressed onto it and a picture was taken. The image was viewed using the ELMS. First, the length was defined using an endwise graduation scale; then, the endwise diameter of a lesion was measured with the given length as a scale plate. Second, the diameter of the biopsy forceps was used as a scale plate to measure the size of a polyp. According to the results of the up arc of the circumference divided by the length of the arc, if the lesion occupied a quarter of the enteric cavity, then the actual diameter of the polyp was considered to be 1.1 times the measurement. When the lesion occupied one third of the enteric cavity, the size of the polyp was considered to be 1.2 times that of the measurement; the size of the polyp was estimated to be 1.6 times that of the measurement when it occupied half of the enteric cavity (Figure 1).
Patients with colon polyps were enrolled from the National Center of Colorectal Surgery, Nanjing University of Traditional Chinese Medicine. First, when the clinician observed a polyp or tumor, the width of the largest diameter of the tumor was determined; then, a graduated biopsy forceps was inserted and used to measure the width of the largest diameter of the tumor from the vertical view, and a picture was obtained according to the ELMS protocol. Next, the ELMS was used to measure the size of the lesion. Finally, the “gold standard” for the width of the largest diameter of the tumor was accurately measured using vernier calipers after the tumor was excised by surgery or endoscopy. A correct measurement was considered when the variation between the evaluation size and actual size was < 10%. The estimated accuracy rate was equal to the number of polyps accurately evaluated divided by the total number of polyps observed. Five endoscopists with experience from over 2000 colonoscopy cases were involved in this study.
The ethics committee of the Third Affiliated Hospital of Nanjing University of Traditional Chinese Medicine approved this study.
Data were analyzed using SPSS 17.0 software for Windows (SPSS Inc., Chicago, IL, United States). A paired Student’s t-test was used to compare the ratio of the estimated size by the endoscopists, the DGBF or the ELMS, to the actual size measured by vernier calipers. Analysis of variance was used to compare the differences among the four groups. Data are presented as mean ± SD; P < 0.05 was considered to be statistically significant.
From August 2013 to March 2014, 166 patients (110 male, 56 female; mean age: 58.7 ± 11.2 years, range: 28-84 years) were included in this study with 192 colorectal polyps: rectal (n = 69), sigmoid (n = 64), descending (n = 16), transverse (n = 15), and ascending (cecum; n = 28) colon polyps. Five of the patients underwent laparoscopic colectomy, and the remainder had endoscopic mucosal resection. The pathologic results of all resected lesions included tubular adenomas (n = 117), villous adenomas (n = 27; one of which was mucosal cancer), tubulovillous adenomas (n = 46), and neuroendocrine tumors (carcinoid; n = 2).
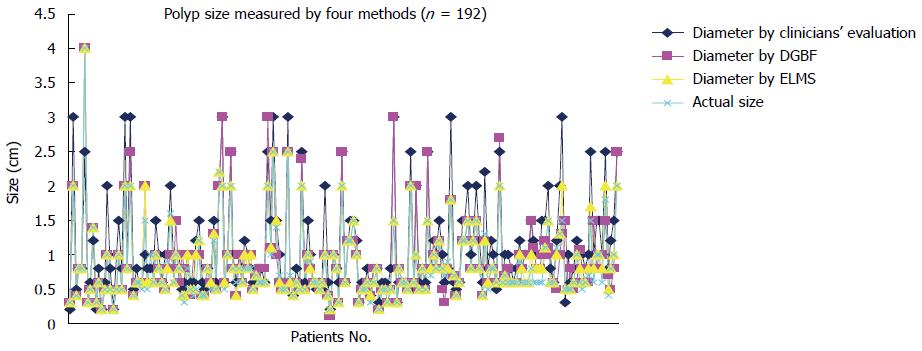
The mean largest diameter of the resected polyps measured by vernier calipers was 0.85 ± 0.53 cm (range: 0.2-3.0 cm), of which 134 were < 1 cm, 43 were 1-2 cm, and 15 were > 2 cm. Measurements of all polyps using all methods are depicted in Figure 2. Measurements taken using DGBF and the ELMS differed significantly from clinicians’ evaluations (Ps < 0.001), but not from the vernier calipers (Table 1).
| Method | Size (cm) | P | ||
| VC | CE | DGBF | ||
| VC | 0.85 ± 0.69 | - | - | - |
| CE | 1.10 ± 0.53 | < 0.001 | - | - |
| DGBF | 0.87 ± 0.54 | 0.134 | < 0.001 | - |
| ELMS | 0.85 ± 0.53 | 0.289 | < 0.001 | 0.027 |
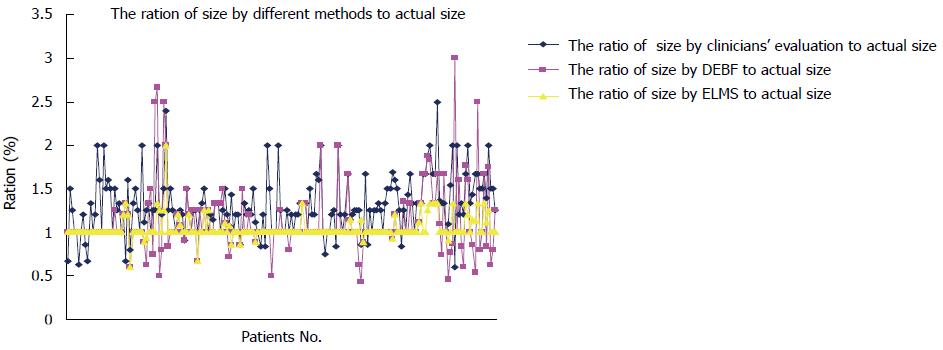
The ratios of the estimated sizes compared to vernier calipers are presented in Figure 3. Consistent with the mean diameters, the ratios obtained by DGBF and the ELMS differed significantly from those obtained using the clinicians’ evaluations (Ps < 0.001), but not from each other (Table 2).
| Ratio | Size (cm) | P | |
| DGBF:VC | ELMS:VC | ||
| CE:VC | 1.30 ± 0.33 | < 0.001 | < 0.001 |
| DGBF:VC | 1.11 ± 0.37 | - | 0.021 |
| ELMS:VC | 1.04 ± 0.13 | - | - |
For polyps less than 1 cm, only 20.6% (28/134) were accurately estimated by the clinicians’ evaluations, whereas significantly larger proportions were accurately assessed by DGBF and the ELMS (Ps < 0.001) (Table 3). Similar results were found with polyps 1-2 cm in diameter. In contrast, none of the polyps larger than 2 cm were accurately measured by the clinicians’ evaluations. However, significantly more polyps were accurately estimated by DGBF and the ELMS (Ps < 0.05).
| Polyp size | Method | Rate of accurate estimation | P | |
| CE | DGBF | |||
| < 1 cm | CE | 20.6% (28/134) | - | - |
| DGBF | 61.2% (82/134) | < 0.001 | - | |
| ELMS | 75.4% (101/134) | < 0.001 | 0.001 | |
| 1-2 cm | CE | 14.0% (6/43) | ||
| DGBF | 48.8 % (21/43) | < 0.001 | ||
| ELMS | 74.4% (32/43) | < 0.001 | 0.003 | |
| > 2 cm | CE | 0.0% (0/15) | ||
| DGBF | 40.0% (6/15) | 0.008 | ||
| ELMS | 80.0% (12/15) | 0.046 | 0.212 | |
The size of a polyp determined at colonoscopy is crucial for assessing its type and selecting a treatment plan[5-7]. Data presented here demonstrate that clinicians’ evaluations do not accurately estimate the actual size, consistent with previous findings[3,4]. As a result, inappropriate advice might be given for follow-up. Gopalswamy et al[8] compared the accuracy of a linear probe, visual estimation and forceps for estimating polyp size during colonoscopy and found that the measurement using a linear probe was most consistent with the actual polyp size. However, the linear probe requires special software for estimation, which adds to examination time and cost. The open biopsy forceps method was found to be the least accurate method. Using DGBF can increase the accuracy of estimation of polyp size, though the results can be inaccurate due to visual deviation, especially for the transverse diameter of the side of the developing tumor. In order to reduce visual deviation, we developed a system that uses this method as a “scale-plate” to increase the measurement accuracy.
In this study, the average largest diameter of the resected polyps measured by the endoscopists was significantly larger than the actual size. However, measurements taken with DGBE or the ELMS did not differ, demonstrating the increased estimation accuracy, which was consistent with the report by Liu et al[4]. The accuracy rate of DGBE was lower than that by ELMS, though a 25% error rate was still evident for polyps < 1 cm. The reasons for this may be that, first, a reduced visual deviation of these polyps increased the accuracy of the biopsy forceps. Second, many of the polyps < 1 cm were a protruding type. Due to the potential deviation of visual angle when taking pictures, the measurement deviation was more than 10%, which would be judged to be inaccurate whereas deviation of < 1 mm would not affect the choice of treatment. Notably, none of the polyps > 2 cm were accurately estimated by endosocopists’ visual estimations, suggesting increased visual deviation. Thus, the accuracy of the ELMS tended to increase with the diameter, though the number of large polyps was insufficient for statistical comparison. Future studies will include a larger number of polyps > 2 cm to address this. this study only estimated the largest diameters and did not compare the transverse or endwise diameters of the lesions, which will also be investigated in future studies.
In conclusion, the accuracy of estimating polyp size diameter at colonoscopy that relied on endoscopists’ experience was low. This accuracy can significantly be increased using DGBF and the ELMS.
Many thanks to Ping Liu, Xiu Zhang, and Huiping Lin for help with the acquisition of data, and to Dr. Hang Yao, Dr. Kunlan Wu, and Dr. Jinhao Zhang for assisting with the analysis and interpretation of data.
Determination of tumor size via colonoscopy is related to the nature and treatment of the tumor. However, there are still no standardized criteria for this, and many clinicians evaluate the size based on their experience, which is often inconsistent with the actual size of the tumor. The authors developed disposable graduated biopsy forceps (DGBF) to increase the accuracy of estimating the size of the polyps, as there is still visual variations, especially for polyps > 2 cm in diameter. To estimate the size of polyps via colonoscopy more accurately, the authors designed an endoscopic lesion measurement system (ELMS) using DGBF as a “scale-plate” and evaluated its use in the clinic.
The accuracy of estimating polyp size was compared among different methods by visual estimation, DGBF and ELMS.
In this study, the authors established an ELMS to measure the endoscopic polyp size. The authors found that the accuracy of visual estimation for polyp size is low. Use of the DGBF and ELMS significantly increased the accuracy of size estimation. The accuracy of estimation by ELMS tend to be higher with increasing polyp size.
This system is very easy to learn and provides objective estimation of polyp size under endoscopy. It can be used in clinical practice and does not increase the medical cost.
An ELMS can improve the accuracy of endoscopic polyp size measurement. The investigators have compared a new technique versus standard to grade endoscopic polyp size. They find significant differences between the old and new methods. This is potentially a compelling study. However, there must be some improvements.
P- Reviewer: Amornyotin S, Ciaccio EJ, Mentes O S- Editor: Qi Y L- Editor: AmEditor E- Editor: Zhang DN
| 1. | Wang HM, Huang CM, Zheng CH, Li P, Xie JW, Wang JB, Lin JX, Lu J. Tumor size as a prognostic factor in patients with advanced gastric cancer in the lower third of the stomach. World J Gastroenterol. 2012;18:5470-5475. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 35] [Cited by in RCA: 39] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 2. | Morales TG, Sampliner RE, Garewal HS, Fennerty MB, Aickin M. The difference in colon polyp size before and after removal. Gastrointest Endosc. 1996;43:25-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 81] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 3. | Eichenseer PJ, Dhanekula R, Jakate S, Mobarhan S, Melson JE. Endoscopic mis-sizing of polyps changes colorectal cancer surveillance recommendations. Dis Colon Rectum. 2013;56:315-321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 55] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 4. | Liu P, Zhang X, Lin HP, Jin HJ, Leng Q, Zhang JH, Zhang Y, Yao H, Wu KL. [Study on accuracy of endoscopic polyp size measurement by disposable graduated biopsy forceps]. Zhonghua Wei Chang Wai Ke Zazhi. 2013;16:1142-1145. [PubMed] |
| 5. | Tseng MY, Lin JC, Huang TY, Shih YL, Chu HC, Chang WK, Hsieh TY, Chen PJ. Endoscopic submucosal dissection for early colorectal neoplasms: clinical experience in a tertiary medical center in taiwan. Gastroenterol Res Pract. 2013;2013:891565. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 6. | Toyonaga T, Man-i M, Chinzei R, Takada N, Iwata Y, Morita Y, Sanuki T, Yoshida M, Fujita T, Kutsumi H. Endoscopic treatment for early stage colorectal tumors: the comparison between EMR with small incision, simplified ESD, and ESD using the standard flush knife and the ball tipped flush knife. Acta Chir Iugosl. 2010;57:41-46. [PubMed] |
| 7. | Horiuchi Y, Chino A, Matsuo Y, Kishihara T, Uragami N, Fujimoto Y, Ueno M, Tamegai Y, Hoshino E, Igarashi M. Diagnosis of laterally spreading tumors (LST) in the rectum and selection of treatment: characteristics of each of the subclassifications of LST in the rectum. Dig Endosc. 2013;25:608-614. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Gopalswamy N, Shenoy VN, Choudhry U, Markert RJ, Peace N, Bhutani MS, Barde CJ. Is in vivo measurement of size of polyps during colonoscopy accurate? Gastrointest Endosc. 1997;46:497-502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 134] [Article Influence: 4.8] [Reference Citation Analysis (0)] |