Published online Feb 21, 2015. doi: 10.3748/wjg.v21.i7.2047
Peer-review started: June 23, 2014
First decision: June 23, 2014
Revised: August 6, 2014
Accepted: November 18, 2014
Article in press: November 19, 2014
Published online: February 21, 2015
Processing time: 233 Days and 10.4 Hours
AIM: To investigate the possible mechanism of how glucose promotes invasion and metastasis of colon cancer cells.
METHODS: CT-26 rat colorectal cancer cells were cultured in different concentrations of glucose environments (10, 20, and 30 mmol/L). Wound healing assay and transwell chamber invasion assay were utilized to test the migration and invasion, respectively. In order to understand the role of signal transducer and activator of transcription 3 (STAT3) in the process, STAT3 inhibitors, including Stattic (an STAT3 specific inhibitor) and small interfering RNA targeting STAT3, were used to block STAT3 function to evaluate their impact on CT-26 cell motion. To verify whether STAT3 and matrix metalloproteinase-9 (MMP-9) protein expression is associated with glucose-induced cell movement, Western blot was used to compare the differences in the expression of MMP-9 and STAT3 in cells incubated with and without STAT3 inhibitors in high glucose condition.
RESULTS: In both wound healing and invasion assays, the migration and invasion of CT-26 cells increased gradually with the increase in glucose concentration. However, the glucose-induced migration and invasion were obviously inhibited by STAT3 inhibitors (P < 0.05). Similarly, in Western blot assessment, both MMP-9 and STAT3 expression increased under a high glucose environment and the highest expression was achieved when 30 mmol/L glucose was used. However, in cells treated with 30 mmol/L mannitol, either MMP-9 or STAT3 expression did not increase (P > 0.05). When STAT3 inhibitors were added in the 30 mM glucose group, not only STAT3 but also MMP-9 expression decreased significantly (P < 0.05).
CONCLUSION: Our study provides evidence that glucose can promote both migration and invasion of CT-26 cells, and that the STAT3-induced MMP-9 signal pathway is involved in this process.
Core tip: It has been known from several epidemiological reports that colorectal cancer patients with comorbid diabetes have poor outcomes. The high glucose status in diabetes patients may play an important role in this process, but the possible mechanism is unclear. Our study reveals that glucose can promote colorectal cell migration and invasion, and the signal transducer and activator of transcription 3 induced matrix metalloproteinase-9 expression is involved in this process.
- Citation: Lin CY, Lee CH, Huang CC, Lee ST, Guo HR, Su SB. Impact of high glucose on metastasis of colon cancer cells. World J Gastroenterol 2015; 21(7): 2047-2057
- URL: https://www.wjgnet.com/1007-9327/full/v21/i7/2047.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i7.2047
Colorectal cancer is the third most common cancer in both sexes worldwide[1]. The prognosis of colorectal cancer is related to its clinical stage. According to the American Joint Committee on Cancer staging system, the five-year survival rate is less than 60% in patients with colorectal cancer with lymph node metastasis (stage III) , and less than 10% in those with distal metastasis (stage IV)[2]. Therefore, understanding and avoiding the metastasis of colorectal cancer cells is important for prolonging patient survival.
Metastasis is a complex multistep process. The malignant cells must separate from the original cell clump, pass through the tightly bound extracellular matrix (ECM) barrier, and then migrate to distant organs[3]. One critical step in the process is that malignant cells dissolve basement membranes and ECM. The matrix metalloproteinases (MMPs), a large multigene family of zinc-dependent endopeptidases, have been thought to mediate and control the process[4]. MMP-9 is known as an important enzyme that degrades ECM and mediates angiogenesis in tumor cells[5]. The concentration of MMP-9 in patients with colorectal cancer is positively correlated with the depth of intestinal invasion, lymph node metastasis, and distant metastasis[6]. Therefore, MMP-9 is considered an important factor associated with tumor invasion and metastasis in colorectal cancer, and can serve as a potential prognostic factor for colorectal cancer[7].
Janus kinase-signal transducer and activator of transcription (JAK-STAT) is a signaling pathway that receives extracellular signals and transfers the message directly in the nucleus of the target gene without going through a second messenger[8]. JAK-STAT is involved primarily in immune regulation, cell growth, and differentiation[9]. There are several different types of STAT, and STAT3 is involved in the early embryonic development of animal cells, inflammation, and growth regulation, among other functions[10]. In colorectal cancer, the activation of STAT3 is associated with the increased incidence of lymph node involvement, distant organ metastasis, and poor survival[11,12].
Many epidemiological studies have also pointed out that patients with diabetes, regardless of gender, have a higher risk of colorectal cancer[13,14] . At the same time, patients with colorectal cancer with comorbid diabetes have poor outcomes[15,16]. It is still unclear whether the high blood sugar in patients with diabetes promotes the invasion of colorectal cancer cells and the detailed mechanism of this process is not well elucidated. The association of glucose with cancer cell migration has been investigated in some cancers. An in vitro breast cancer study pointed that high glucose can increase breast cancer MCF-7 cell motility via zinc and its associated transporters[17]; another study using pancreatic cancer cells has also found that glucose stimulates glucose metabolism and promotes cell migration via hypoxia-inducible factor-1α[18]. Therefore, the high glucose in diabetic patients may be one of possible factors to promote cancer cell movement. Here, we explored whether a high glucose environment increases the migration and invasion of colon cancer cells and the possible role of STAT3 and MMP-9 in the process.
STAT3 specific inhibitor (Stattic) was purchased from Abcam (Cambridge, MA, United States); small interfering RNA (siRNA) (siGENOME SMARTpool) for SATA3 from Thermo Fisher Scientific (Waltham, MA, United States); siRNA transfection reagent (TransIT-TKO) from Mirus Bio (Pittsburgh, PA, United States); and antibodies against STAT3, MMP-9, and actin from Millipore (Millicell; Bedford, MA, United States).
The rat colon cancer cell line CT-26 was bought from the Culture Collection and Research Center of the Food Industry Institute (Hsinchu City, Taiwan) and maintained in RPMI-1640 (Hyclone, Logan, UT, United States) supplemented with 10% (v/v) fetal bovine serum (FBS), 100 IU/mL penicillin and 100 μg/mL streptomycin, sodium pyruvate (0.11 mg/mL), and 1% (v/v) non-essential amino acids at 37 °C in a 5% CO2-95% air atmosphere with high humidity.
Proteins were extracted from tissue homogenates and cell lysates using an ice-cold radioimmunoprecipitation assay buffer supplemented with phosphatase and protease inhibitors (50 mmol/L sodium vanadate, 0.5 mmol/L phenylmethylsulphonyl fluoride, 2 mg/mL aprotinin, and 0.5 mg/mL leupeptin). Protein concentrations were determined using a Bio-Rad protein assay (Bio-Rad Hercules, CA, United States). Total proteins (30 μg) were separated using SDS-PAGE (sodium dodecyl sulfate polyacrylamide gel electrophoresis) (10% acrylamide gel) (Mini-Protein II system; Bio-Rad, Richmond, CA). Proteins were transferred to expanded polyvinylidene difluoride membranes (PerkinElmer, Waltham, MA, United States) using a Western blotting system (Trans-Blot Turbo Transfer System; Bio-Rad). After the transfer, the membranes were washed with phosphate buffer saline and blocked for 1 h at room temperature with 5% (w/v) skimmed milk powder in PBS. Blots were incubated overnight at 4 °C for the primary antibody reactions to bind the target proteins: nuclear STAT3, cytoplasmic STAT3, and MMP-9. The blots were incubated with goat polyclonal antibody (1:1000) to bind actin, which was the internal control. After the primary antibody had been removed, the blots were extensively washed with PBS/Tween 20 and then incubated for 2 h at room temperature with the appropriate peroxidase-conjugated secondary antibody diluted in PBS/Tween 20. The blots were developed using autoradiography with an enhanced chemiluminescence Western blotting system (Amersham International, Buckinghamshire, United Kingdom). The immune blots were quantified using a laser densitometer (Avegene Life Science, Taipei, Taiwan).
Duplexed RNA oligonucleotides for rat STAT3 (Stealth RNA interference) (siGENOME SMARTpool) were synthesized by Thermo Fisher Scientific. CT-26 cells were transfected with 50 nmol/L of STAT3 siRNAs (siRNA-STAT3) or scrambled siRNA using a transfection reagent (TransIT-TKO; Mirus Bio, Madison, WI, United States), incubated for 48 h after transfection, and then used for further investigation.
The in vitro invasion assays were done using a transwell chamber with a 12-mm diameter and a polycarbonate membrane with 8-μm pores (Corning Costar, Cambridge, MA, United States) coated with Matrigel[19,20]. Cells were trypsinized and suspended at a final concentration of 106 cells/mL in serum-free RPMI-1640 medium. Various concentrations of glucose (10, 20, and 30 mmol/L) were added to the cells 24 h before they were seeded. The cell suspension was added to the upper chamber of the transwell chamber. The bottom chamber contained medium with 5% FBS. After they had been incubated for 24 h at 37 °C under a 5% CO2 and 95% air atmosphere, all of the non-invaded cells were removed; the invaded cells were fixed with 4% paraformaldehyde and stained with hematoxylin. Images were collected using a fluorescence microscope (IX70; Olympus America, Center Valley, PA, United States) fitted with a camera and MagnaFire 2.1 software (both from Olympus America). Six fields were counted for each assay.
To study the wound-fill rate in vitro, we used an in vitro wound-healing model, which has been well-described and successfully used by other investigators[21-23]. Briefly, CT-26 cells were grown until confluence and 3-mm-wide wounds in the cell monolayers were created using a sterile instrument in a standardized manner. The wounded cell monolayers were grown in various concentrations of glucose (10, 20 and 30 mmol/L) for 24 h. The gaps in the monolayers were documented using inverse microscopy (IX70) and digital photography. The widths of the gaps were then measured and analyzed using MagnaFire 2.1.
Data are expressed as mean ± SE. Repeated measures analysis of variance was used to analyze the changes in gene and protein expression as well as other parameters. Significance was set at P < 0.05.
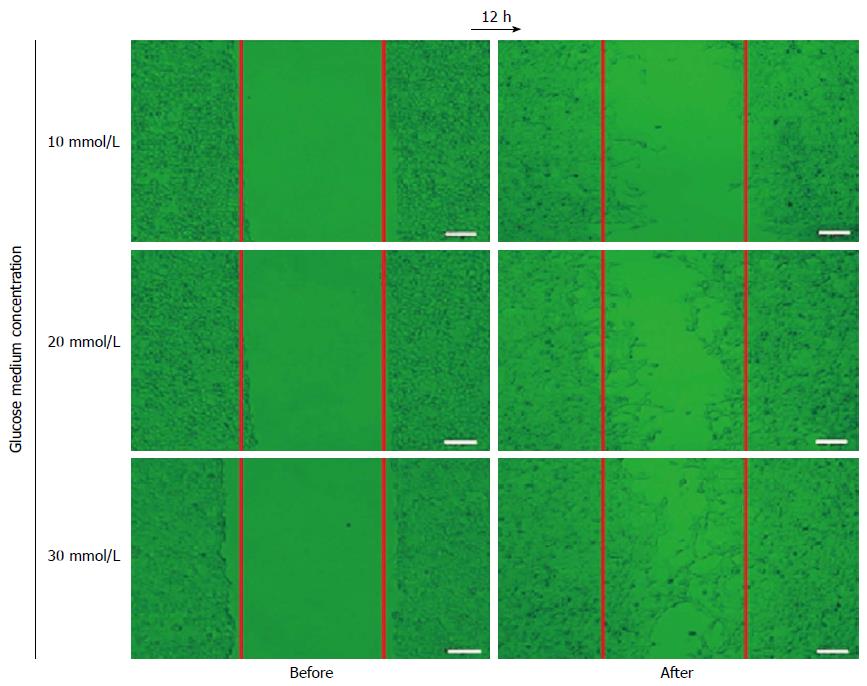
A 3-mm wide wound gap was created on the confluent monolayer of CT-26 cells in a Petri dish. The CT-26 cells were then incubated with 3 different concentrations of glucose (10, 20 or 30 mmol/L) for 12 h. The higher the concentration of glucose was, the more CT-26 migrated cells into the gap (Figure 1).
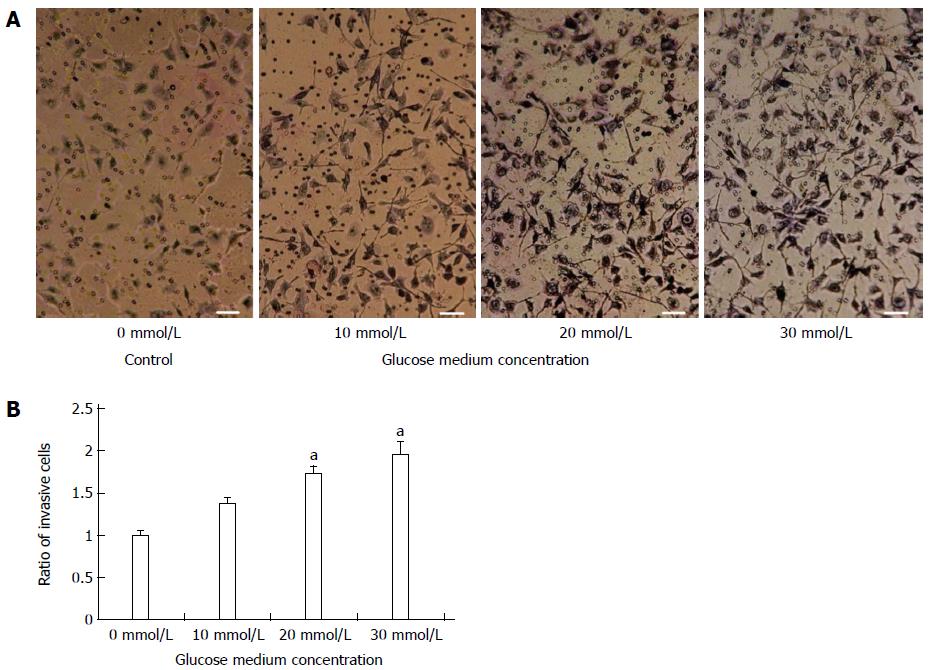
The suspended CT-26 cells were incubated with different concentrations of glucose (10, 20 or 30 mmol/L). The cell suspension was then transferred to the upper chamber of a transwell chamber. After 24 h, the noninvasive CT-26 cells were removed. The higher the glucose concentration was, the more CT cells penetrated through the basement membrane. All differences between glucose-treated and control cells were significant (P < 0.05 for all) (Figure 2A, B). The number of invasive CT-26 cells was about twice as high in the 30-mmol/L culture than in the 0-mmol/L culture (Figure 2B).
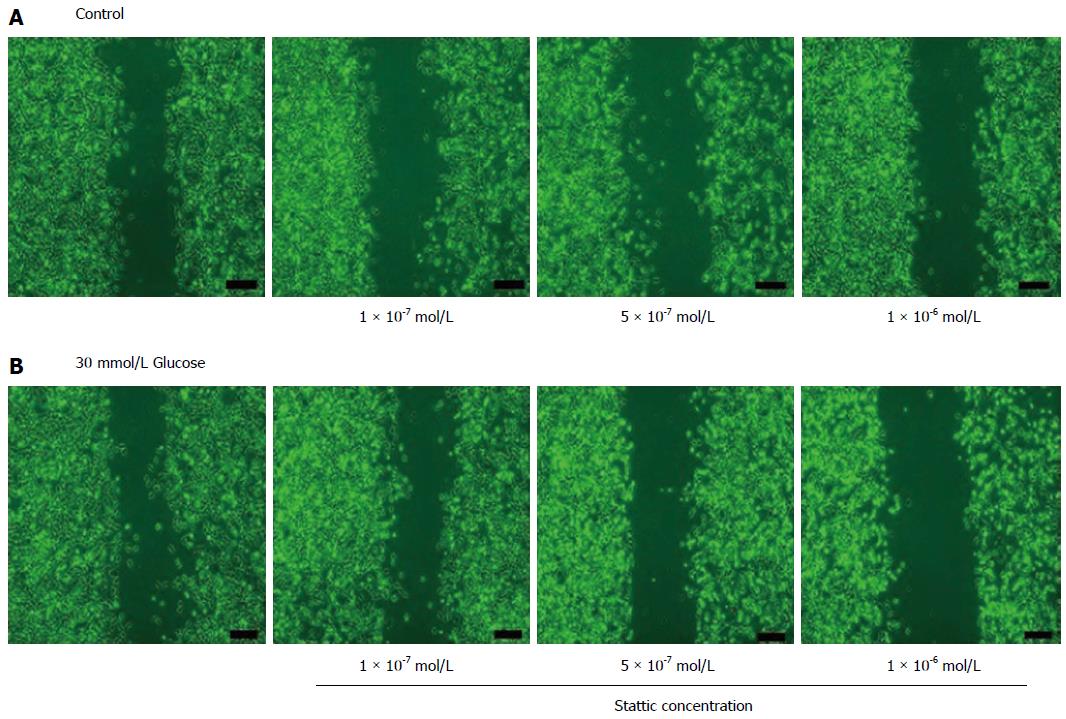
To determine whether STAT3 signaling is involved in the CT-26 cell migration, Stattic was added both to the glucose-free (0 mmol/L control group) and to the 30-mmol/L glucose-cultured group. A wound-healing analysis was then performed. In the glucose-free control group, migration was not significantly affected by different Stattic concentrations (as indicated) (Figure 3A). However, in the 30-mmol/L glucose group, the number of the migrated cells was reduced gradually with increasing concentrations of Stattic (Figure 3B).
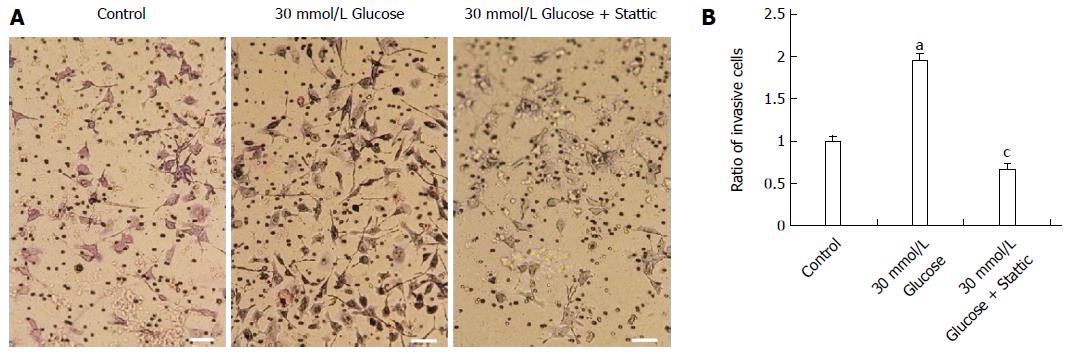
To determine whether STAT3 signaling is involved in CT-26 cell invasion, we added Stattic (1 × 10-6 mol/L) to 30-mmol/L glucose-cultured CT-26 cells. Compared with glucose-free control cells, the invasion of CT-26 cells was markedly higher in the group incubated with 30 mmol/L of glucose; however, in the group incubated with 30 mmol/L of glucose plus Stattic, the invasion of CT-26 cells was almost totally blocked (Figure 4).
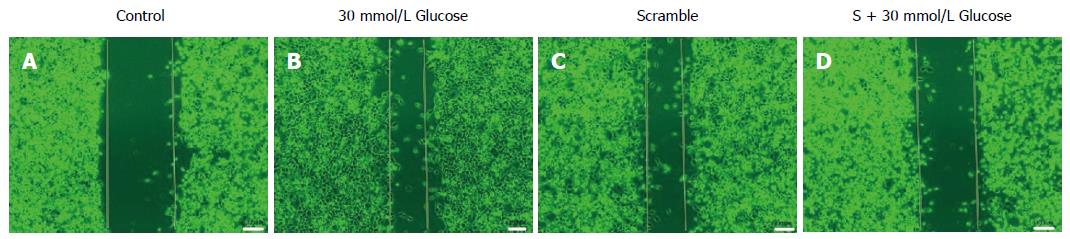
We used 50 nmol/L siRNA to test the effect of STAT3 on CT-26 cell migration. In the glucose-free control group, migration was negligible (Figure 5A); in the 30-mmol/L glucose and scramble (scrambled oligonucleotides) groups, CT-26 cells clearly moved into the wound gap (Figure 5B, C). In the group incubated with 30 mmol/L of glucose plus 50 nmol/L siRNA, CT-26 cell migration was substantially inhibited (Figure 5D).
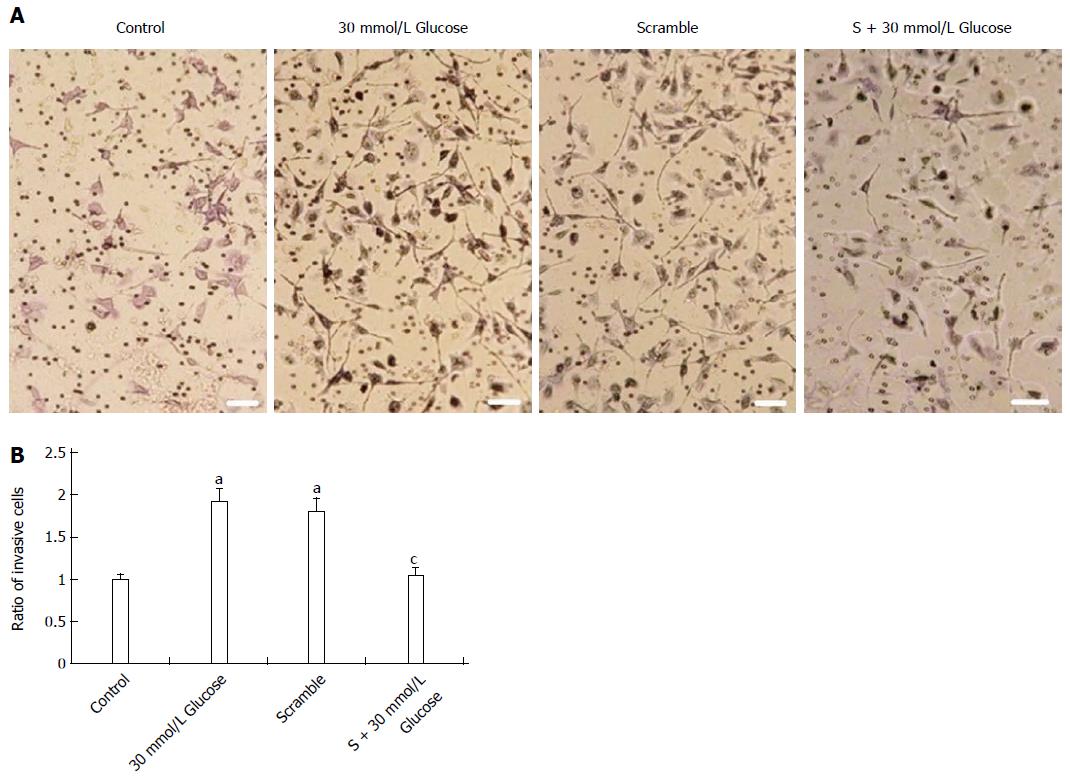
We also used 50 nmol/L siRNA to explore the effect of STAT3 on CT-26 cell invasion. In the 30-mmol/L glucose and scramble groups, invasion was about twice as high as in the glucose-free control group (P < 0.05 compared with control group) (Figure 6A), but in the 50 nmol/L siRNA + 30 mmol/L glucose group, invasion was almost totally inhibited (P < 0.05 compared with the 30-mmol/L glucose group) (Figure 6B).
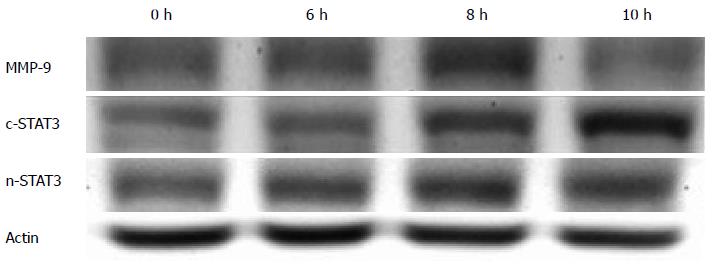
CT-26 cells were incubated in a 30-mmol/L glucose environment, and then, using Western blot with actin protein as an internal control, we detected the timeline of STAT3 and MMP-9 activation (Figure 7). MMP-9 and nuclear STAT3 expression peaked at 8 h, and cytoplasmic STAT3 peaked at 10 h.
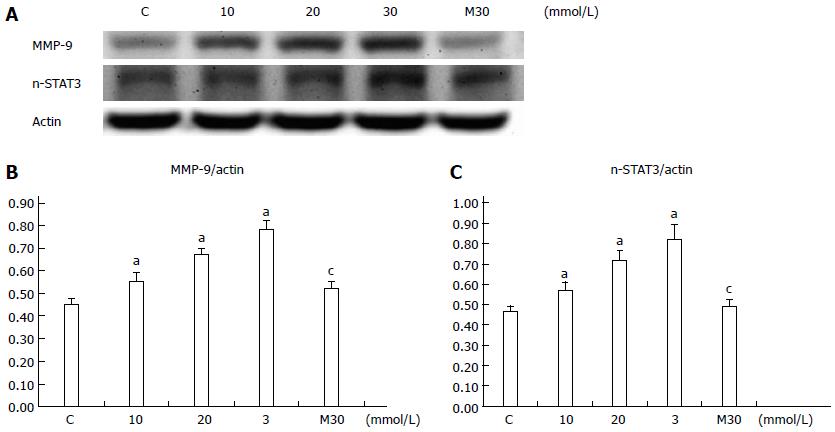
We then explored the relationship between glucose and the activation of STAT3 and MMP-9. Because nuclear STAT3 and MMP-9 peaked within 8 h, we incubated CT-26 cells with different concentrations of glucose [0 (control), 10, 20 and 30 mmol/L] for 8 h. The higher the glucose concentration, the higher the levels of expression of nuclear STAT3 and MMP-9 (P < 0.05 for all) (Figure 8A, B and C). To exclude the effect of the glucose concentration on the activation of STAT3 and MMP-9, we also tested the effect of 30 mmol/L mannitol on their expression and activation. There was no significant difference between the 30 mmol/L mannitol group (M30) and the control group (P > 0.05 compared with the control group) (Figure 8B, C).
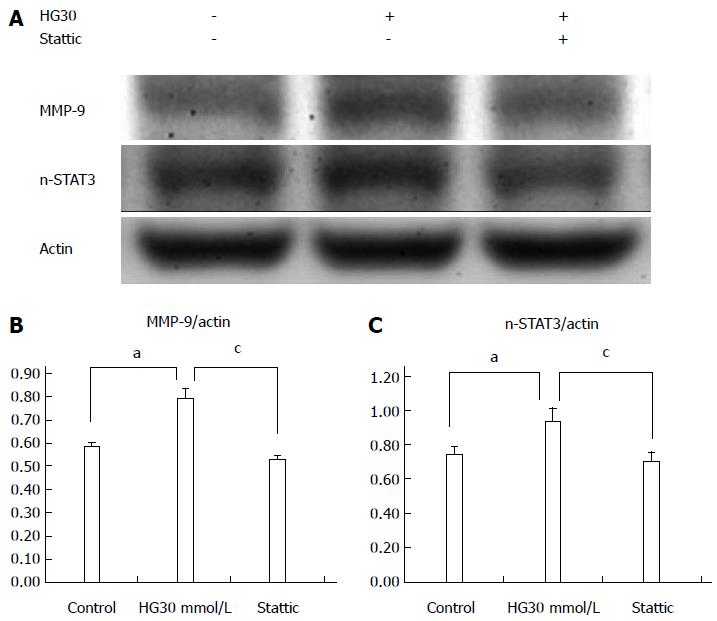
To see whether there is a correlation between STAT3 and MMP-9 in a high-glucose environment, Stattic was added, and then STAT3 and MMP-9 protein expression was analyzed using Western blot (Figure 9A). In the 30 mmol/L glucose group without Stattic, both MMP-9 and STAT3 were activated (P < 0.05 compared with the control group). However, after Stattic was added, both STAT3 and MMP-9 expression was slightly lower (Figure 9A) than in the glucose-free control (P < 0.05 compared with the 30 mmol/L glucose group) (Figure 9B, C).
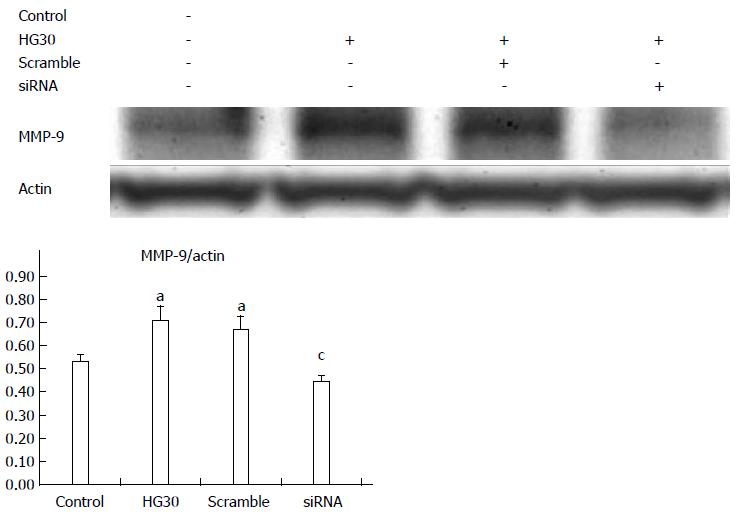
SiRNA (50 nmol/L) was used to evaluate the association between STAT3 and MMP-9 expression in a high-glucose environment. In both the 30 mmol/L glucose (HG30) group and in the scramble group, MMP-9 expression was significantly (P < 0.05) higher than that in the control and siRNA groups. In the siRNA group, MMP-9 expression was slightly but significantly (P < 0.05) lower than that in the glucose-free group (Figure 10 A, B).
We found that glucose promoted CT-26 cell migration and invasion and that both were directly glucose dose-dependent. When STAT3 inhibitor, Stattic or siRNA, was added to a high-glucose environment, both glucose induced CT-26 cell migration and invasion were inhibited. This indicated that the STAT3 signaling pathway is associated with regulating the effect of glucose on CT-26 cell migration and invasion.
In developing and developed countries, diabetes and cancer have become major health problems. Studies began to report an association between diabetes and cancer in 1959[24]. Since then, epidemiological studies claim that diabetes is one risk factor of cancers and indicates a poor prognosis.
The possible reasons for the correlation between DM and cancers might come from their shared risk factors. Those risks included the unchangeable factors such as aging, sex, and race; the modifiable life style and behavioral factors such as obesity, physical activity, diet, alcohol, and smoking. Nevertheless, whether diminishing these factors is expected to simultaneously reduce the DM and cancer risk is still debatable. Taking overweight as an example, weight loss has been shown to be helpful in reducing DM incidence. However, it is still unclear whether it can also reduce the incidence of cancers. Because of the lack of large and rigorous research data, there is still lack of sufficient evidence to prove its efficacy[25].
In addition to these common risk factors for both DM and cancers, the abnormal metabolism of DM itself also seems to contribute the occurrence of cancers. Diabetes is caused by a series of glucose metabolism dysfunctions and ultimately leads to an abnormal increase in blood sugar. Its causes and characteristics include the following: the insulin resistance of cells leads to insulinemia, insufficient insulin secretion, excessive or inappropriate glucagon secretion, abnormal hepatic glucose metabolism and gluconeogenesis, abnormal growth hormone secretion, and so on.
The abnormalities in the regulation of glucose metabolism may lead to the proliferation and growth of abnormal cells and, finally, to oncogenesis[26,27]. Nevertheless, the possible biologic links between diabetes and cancer are still incompletely understood.
The biophysiological factors that may contribute to the development of colorectal cancer in patients with diabetes include diabetes-related obesity, high insulinemia, high blood C-petite, high blood insulin-like factor-1, high blood leptin, low blood insulin growth factor binding protein-3, and low blood adiponectin[28,29]. However, the possible mechanisms by which diabetes affects the invasion and metastasis of colorectal cancer cells are not well studied and remain unclear.
Among the mechanisms of abnormal glucose metabolism in diabetes, overactive gluconeogenesis is one that causes high blood glucose[30,31]; however, its exact mechanism is not well understood. Some studies using cell culture and mouse liver tissue have pointed out that blood insulin resistance interacts with IL-6 and STAT3 signaling pathways to regulate gluconeogenesis-related gene activation and inhibition[32-34]. The STAT3 pathway as part of abnormal glucose metabolism is found not only in liver gluconeogenesis; some studies report that STAT3 is also related to the proliferation and differentiation of other types of tissue in a high-glucose diabetic environment. For example, renal glomerular mesangial cells are stimulated and undergo proliferation through the STAT3 signaling pathway, ultimately leading to diabetes nephropathy[35]. In addition, a study using in vitro differentiated myocytes, which were derived from human skeletal muscle satellite cells of obese patients with type II diabetes, reported that after they had been treated with IL-6, the phosphorylation of STAT3 increased in myocytes, thereby affecting the abnormal reaction of muscle tissue to insulin and hyperglycemia[36]. Therefore, the STAT3 signaling pathway seems to be involved in diabetes-related abnormal physiological conditions such as hyperglycemia, nephropathy, and muscle-tissue glucose utilization. In colorectal cancer, the abnormal activation of STAT3 may also influence and promote the invasion of colorectal cancer cells. As a result, the glucose-induced overactive STAT3 pathway may contribute to the poor prognosis of patients with comorbid colorectal cancer and diabetes mellitus.
Distant organ metastasis is one of most important causes of cancer death. In colorectal cancer, MMP-9 is known as an important factor involved in colorectal cell metastasis. Therefore, influencing and controlling the activation of the MMP gene will be important for cancer cell metastasis and invasion. The relationship between STAT3 activation and MMP-9 expression has been reported in different tissue types and cancer cells. A study using human mammary epithelial cells found that sustained activation of STAT3 immortalized mammary epithelial cells into cancerous cells, and that this carcinogenic mechanism required MMP-9 activation and expression. Tyrosine phosphorylated STAT3 has also been strongly positively correlated with MMP-9 expression[37], and when the STAT3-induced MMP-9 pathway was inhibited, breast cancer cell invasion and metastasis were also inhibited[38]. Another report on human skin squamous cell carcinoma found that inhibiting the STAT3 activity in transfected cancer cells also inhibited the expression of MMP-9 and the invasion of the transfected cells[39]. Moreover, STAT3 activation and MMP-9 expression are also associated in myeloid cells and fibroblast cells[40,41]. We also found a correlation between STAT3 activation and MMP-9 expression in colorectal cancer cells in a high-glucose environment.
Although our study provides evidence that glucose promotes the migration and invasion of CT-26 cells, and that the STAT3-induced MMP-9 signal pathway is involved in this process, there are some limitation and unanswered questions in our study. First, in order that cells could be presented both vertical and horizontal motions to evaluate the effects of invasion and migration, we used stuck-type rat CT-26 cells but not human colon cells in our study. Whether the effect is also active in human cell lines needs further investigation. Second, in clinical tumor niche, the production of MMP-9 could be derived from the tumor itself, surrounding stromal cells or inflammatory polymorphonuclear leukocytes[42]. So, the function and interaction of MMP-9 from different origin may play diverse effects in tumor cells. In our study, the MMP-9 is produced by CT-26 tumor cell only, so, we could only evaluate the effect of MMP-9 induced by STAT3 in colon cells itself. The interactions of STAT3 with MMP-9 which comes from extra-tumor cells need further study. Third, although MMP-9 expression is related with colorectal cancer with liver metastasis, a clinical study pointed out that the non-expression of MMP-9 in Duke B stage colorectal cancer patients is a poor predictor factor for survival[43]. Because MMP-9 plays multi-faceted role in different phases of the tumorigenic process, the expression of MMP-9 from tumor cells needs further studies to elucidate the final clinical outcomes. Therefore, in the future, we need more studies using human colon cells, as well as animal experiments to improve the deficiencies in our study and clarify the above controversies.
We thank Bill Franke for his invaluable advice and editorial assistance.
Both colorectal cancer (CRC) and diabetes mellitus (DM) are common diseases worldwide, and CRC patients combined with DM have poor prognosis compared with those without DM. It is essential to understand the contribution of DM to CRC metastasis although the mechanism is still not well elucidated. Studies on the mechanism were performed in order to provide further management and improve the prognosis for those patients.
Cancer cell metastasis is a complex process that involves a series of dysregulated signal pathways and related molecules. So, it is a hot research topic to identify the associated biological factors and their interaction in the process.
The sophisticated interaction between glucose and colorectal cancer has not well been understood. In this study, the authors employed a colorectal cell model to identify that signal transducer and activator of transcription 3 (STAT3) and matrix metalloproteinases 9 (MMP-9) signal pathway is involved in the process.
Identifying the glucose induced STAT3 and MMP-9 pathway as being associated with increasing colorectal cell motility could improve our understanding of the mechanism of DM and CRC, and provide a therapeutic idea for treatment of CRC combined with DM.
STAT3 is a subgroup of STAT. It is involved in the early embryonic development of animal cells, inflammation, and growth regulators. MMP-9 is one of zinc-dependent endopeptidases. MMPs are capable of degrading all kinds of extracellular matrix proteins and mediating associated molecules in the process.
The work is very interesting and well done. The laboratory results may have important clinical implications. For this reason in the discussion the authors could give more space to explain their work and to provide food for thought for clinical applications.
P- Reviewer: Amedei A, Fabozzi M, Kapischke M S- Editor: Ma YJ L- Editor: Wang TQ E- Editor: Liu XM
| 1. | Siegel R, Ward E, Brawley O, Jemal A. Cancer statistics, 2011: the impact of eliminating socioeconomic and racial disparities on premature cancer deaths. CA Cancer J Clin. 2011;61:212-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3032] [Cited by in RCA: 3123] [Article Influence: 223.1] [Reference Citation Analysis (0)] |
| 2. | O’Connell JB, Maggard MA, Ko CY. Colon cancer survival rates with the new American Joint Committee on Cancer sixth edition staging. J Natl Cancer Inst. 2004;96:1420-1425. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1063] [Cited by in RCA: 1162] [Article Influence: 55.3] [Reference Citation Analysis (0)] |
| 3. | Deryugina EI, Quigley JP. Matrix metalloproteinases and tumor metastasis. Cancer Metastasis Rev. 2006;25:9-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1413] [Cited by in RCA: 1502] [Article Influence: 79.1] [Reference Citation Analysis (0)] |
| 4. | Nagase H, Woessner JF. Matrix metalloproteinases. J Biol Chem. 1999;274:21491-21494. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3230] [Cited by in RCA: 3153] [Article Influence: 121.3] [Reference Citation Analysis (0)] |
| 5. | Farina AR, Mackay AR. Gelatinase B/MMP-9 in Tumour Pathogenesis and Progression. Cancers (Basel). 2014;6:240-296. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 148] [Cited by in RCA: 156] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
| 6. | Chu D, Zhao Z, Zhou Y, Li Y, Li J, Zheng J, Zhao Q, Wang W. Matrix metalloproteinase-9 is associated with relapse and prognosis of patients with colorectal cancer. Ann Surg Oncol. 2012;19:318-325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 46] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 7. | Tutton MG, George ML, Eccles SA, Burton S, Swift RI, Abulafi AM. Use of plasma MMP-2 and MMP-9 levels as a surrogate for tumour expression in colorectal cancer patients. Int J Cancer. 2003;107:541-550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 101] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 8. | Aaronson DS, Horvath CM. A road map for those who don’t know JAK-STAT. Science. 2002;296:1653-1655. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 967] [Cited by in RCA: 993] [Article Influence: 43.2] [Reference Citation Analysis (0)] |
| 9. | Spiekermann K, Biethahn S, Wilde S, Hiddemann W, Alves F. Constitutive activation of STAT transcription factors in acute myelogenous leukemia. Eur J Haematol. 2001;67:63-71. [PubMed] |
| 10. | Yu H, Pardoll D, Jove R. STATs in cancer inflammation and immunity: a leading role for STAT3. Nat Rev Cancer. 2009;9:798-809. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2935] [Cited by in RCA: 3397] [Article Influence: 212.3] [Reference Citation Analysis (0)] |
| 11. | Slattery ML, Lundgreen A, Kadlubar SA, Bondurant KL, Wolff RK. JAK/STAT/SOCS-signaling pathway and colon and rectal cancer. Mol Carcinog. 2013;52:155-166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 152] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 12. | Mora LB, Buettner R, Seigne J, Diaz J, Ahmad N, Garcia R, Bowman T, Falcone R, Fairclough R, Cantor A. Constitutive activation of Stat3 in human prostate tumors and cell lines: direct inhibition of Stat3 signaling induces apoptosis of prostate cancer cells. Cancer Res. 2002;62:6659-6666. [PubMed] |
| 13. | Yuhara H, Steinmaus C, Cohen SE, Corley DA, Tei Y, Buffler PA. Is diabetes mellitus an independent risk factor for colon cancer and rectal cancer? Am J Gastroenterol. 2011;106:1911-1921; quiz 1922. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 225] [Cited by in RCA: 275] [Article Influence: 19.6] [Reference Citation Analysis (0)] |
| 14. | Deng L, Gui Z, Zhao L, Wang J, Shen L. Diabetes mellitus and the incidence of colorectal cancer: an updated systematic review and meta-analysis. Dig Dis Sci. 2012;57:1576-1585. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 165] [Cited by in RCA: 157] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 15. | Huang YC, Lin JK, Chen WS, Lin TC, Yang SH, Jiang JK, Chang SC, Lan YT, Wang HS, Liu CY. Diabetes mellitus negatively impacts survival of patients with colon cancer, particularly in stage II disease. J Cancer Res Clin Oncol. 2011;137:211-220. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 51] [Cited by in RCA: 50] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 16. | Dehal AN, Newton CC, Jacobs EJ, Patel AV, Gapstur SM, Campbell PT. Impact of diabetes mellitus and insulin use on survival after colorectal cancer diagnosis: the Cancer Prevention Study-II Nutrition Cohort. J Clin Oncol. 2012;30:53-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 86] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 17. | Takatani-Nakase T, Matsui C, Maeda S, Kawahara S, Takahashi K. High glucose level promotes migration behavior of breast cancer cells through zinc and its transporters. PLoS One. 2014;9:e90136. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 57] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 18. | Liu Z, Jia X, Duan Y, Xiao H, Sundqvist KG, Permert J, Wang F. Excess glucose induces hypoxia-inducible factor-1α in pancreatic cancer cells and stimulates glucose metabolism and cell migration. Cancer Biol Ther. 2013;14:428-435. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 47] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 19. | Chen PN, Hsieh YS, Chiang CL, Chiou HL, Yang SF, Chu SC. Silibinin inhibits invasion of oral cancer cells by suppressing the MAPK pathway. J Dent Res. 2006;85:220-225. [PubMed] |
| 20. | Wu KJ, Zeng J, Zhu GD, Zhang LL, Zhang D, Li L, Fan JH, Wang XY, He DL. Silibinin inhibits prostate cancer invasion, motility and migration by suppressing vimentin and MMP-2 expression. Acta Pharmacol Sin. 2009;30:1162-1168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 83] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 21. | Hoang AM, Oates TW, Cochran DL. In vitro wound healing responses to enamel matrix derivative. J Periodontol. 2000;71:1270-1277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 116] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 22. | Lackler KP, Cochran DL, Hoang AM, Takacs V, Oates TW. Development of an in vitro wound healing model for periodontal cells. J Periodontol. 2000;71:226-237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 42] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 23. | Fang Y, Svoboda KK. Nicotine inhibits human gingival fibroblast migration via modulation of Rac signalling pathways. J Clin Periodontol. 2005;32:1200-1207. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 34] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 24. | JOSLIN EP, LOMBARD HL, BURROWS RE, MANNING MD. Diabetes and cancer. N Engl J Med. 1959;260:486-488. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 32] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 25. | Giovannucci E, Harlan DM, Archer MC, Bergenstal RM, Gapstur SM, Habel LA, Pollak M, Regensteiner JG, Yee D. Diabetes and cancer: a consensus report. Diabetes Care. 2010;33:1674-1685. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1291] [Cited by in RCA: 1466] [Article Influence: 97.7] [Reference Citation Analysis (1)] |
| 26. | Poulson J. The management of diabetes in patients with advanced cancer. J Pain Symptom Manage. 1997;13:339-346. [PubMed] |
| 27. | Wulaningsih W, Holmberg L, Garmo H, Zethelius B, Wigertz A, Carroll P, Lambe M, Hammar N, Walldius G, Jungner I. Serum glucose and fructosamine in relation to risk of cancer. PLoS One. 2013;8:e54944. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 28. | Pais R, Silaghi H, Silaghi AC, Rusu ML, Dumitrascu DL. Metabolic syndrome and risk of subsequent colorectal cancer. World J Gastroenterol. 2009;15:5141-5148. [PubMed] |
| 29. | Ortiz AP, Thompson CL, Chak A, Berger NA, Li L. Insulin resistance, central obesity, and risk of colorectal adenomas. Cancer. 2012;118:1774-1781. [RCA] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 42] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 30. | Magnusson I, Rothman DL, Katz LD, Shulman RG, Shulman GI. Increased rate of gluconeogenesis in type II diabetes mellitus. A 13C nuclear magnetic resonance study. J Clin Invest. 1992;90:1323-1327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 533] [Cited by in RCA: 553] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 31. | Boden G, Chen X, Stein TP. Gluconeogenesis in moderately and severely hyperglycemic patients with type 2 diabetes mellitus. Am J Physiol Endocrinol Metab. 2001;280:E23-E30. [PubMed] |
| 32. | Ramadoss P, Unger-Smith NE, Lam FS, Hollenberg AN. STAT3 targets the regulatory regions of gluconeogenic genes in vivo. Mol Endocrinol. 2009;23:827-837. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 85] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 33. | Inoue H, Ogawa W, Ozaki M, Haga S, Matsumoto M, Furukawa K, Hashimoto N, Kido Y, Mori T, Sakaue H. Role of STAT-3 in regulation of hepatic gluconeogenic genes and carbohydrate metabolism in vivo. Nat Med. 2004;10:168-174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 275] [Cited by in RCA: 301] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 34. | Tang H, Xie MH, Lei Y, Zhou L, Xu YP, Cai JG. The roles of aerobic exercise training and suppression IL-6 gene expression by RNA interference in the development of insulin resistance. Cytokine. 2013;61:394-405. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 35. | Du J, Wang L, Liu X, Zhou H, Fan Q, Luo J, Yao L, Wang J, Feng J, Ma J. Janus kinase 2/signal transducers and activators of transcription signal inhibition regulates protective effects of probucol on mesangial cells treated with high glucose. Biol Pharm Bull. 2010;33:768-772. [PubMed] |
| 36. | Scheele C, Nielsen S, Kelly M, Broholm C, Nielsen AR, Taudorf S, Pedersen M, Fischer CP, Pedersen BK. Satellite cells derived from obese humans with type 2 diabetes and differentiated into myocytes in vitro exhibit abnormal response to IL-6. PLoS One. 2012;7:e39657. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 49] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 37. | Dechow TN, Pedranzini L, Leitch A, Leslie K, Gerald WL, Linkov I, Bromberg JF. Requirement of matrix metalloproteinase-9 for the transformation of human mammary epithelial cells by Stat3-C. Proc Natl Acad Sci USA. 2004;101:10602-10607. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 199] [Cited by in RCA: 209] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 38. | Kim JE, Kim HS, Shin YJ, Lee CS, Won C, Lee SA, Lee JW, Kim Y, Kang JS, Ye SK. LYR71, a derivative of trimeric resveratrol, inhibits tumorigenesis by blocking STAT3-mediated matrix metalloproteinase 9 expression. Exp Mol Med. 2008;40:514-522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 47] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 39. | Syed ZA, Yin W, Hughes K, Gill JN, Shi R, Clifford JL. HGF/c-met/Stat3 signaling during skin tumor cell invasion: indications for a positive feedback loop. BMC Cancer. 2011;11:180. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 51] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 40. | Wang L, Luo J, He S. Induction of MMP-9 release from human dermal fibroblasts by thrombin: involvement of JAK/STAT3 signaling pathway in MMP-9 release. BMC Cell Biol. 2007;8:14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 37] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 41. | Schröer N, Pahne J, Walch B, Wickenhauser C, Smola S. Molecular pathobiology of human cervical high-grade lesions: paracrine STAT3 activation in tumor-instructed myeloid cells drives local MMP-9 expression. Cancer Res. 2011;71:87-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 59] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 42. | Taguchi A, Kawana K, Tomio K, Yamashita A, Isobe Y, Nagasaka K, Koga K, Inoue T, Nishida H, Kojima S. Matrix metalloproteinase (MMP)-9 in cancer-associated fibroblasts (CAFs) is suppressed by omega-3 polyunsaturated fatty acids in vitro and in vivo. PLoS One. 2014;9:e89605. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 56] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 43. | Koskensalo S, Hagström J, Linder N, Lundin M, Sorsa T, Louhimo J, Haglund C. Lack of MMP-9 expression is a marker for poor prognosis in Dukes’ B colorectal cancer. BMC Clin Pathol. 2012;12:24. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 1.4] [Reference Citation Analysis (0)] |