Published online Jan 28, 2015. doi: 10.3748/wjg.v21.i4.1324
Peer-review started: May 6, 2014
First decision: June 10, 2014
Revised: June 26, 2014
Accepted: August 13, 2014
Article in press: August 28, 2014
Published online: January 28, 2015
Processing time: 266 Days and 7.1 Hours
Localized amyloidosis is characterized by amyloid protein deposition restricted to one organ or tissue without systemic involvement. Gastrointestinal manifestations of localized amyloidoma are unusual, which makes amyloidoma restricted to the rectum a very rare diagnosis requiring a high index of suspicion. We present a rare account for rectal amyloidoma with an unusual presentation of obstructive symptoms and its treatment using a sophisticated surgical modality, transanal endoscopic microsurgery (TEM), which resulted in complete excision of the lesion without hospitalization and complications. The successful treatment for this rectal amyloidoma using TEM emphasizes the need to broaden its application in the treatment of various rectal lesions while preserving organ function and decreasing recurrence.
Core tip: This case represents the first transanal endoscopic microsurgery (TEM) approach for full-thickness excision to treat organ restricted amyloidosis of the rectum, a very rare entity requiring high suspicion for diagnosis and treatment. Although TEM is the preferred modality to treat early rectal cancers and rectal adenomas, it should also be considered for other benign and non-advanced rectal lesions, such as localized amyloidoma. TEM is a less invasive procedure that provides lower morbidity and mortality by decreasing incidence of local recurrence and complications while preserving rectal continence and function.
- Citation: Sharma R, George VV. Transanal endoscopic microsurgery: The first attempt in treatment of rectal amyloidoma. World J Gastroenterol 2015; 21(4): 1324-1328
- URL: https://www.wjgnet.com/1007-9327/full/v21/i4/1324.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i4.1324
Amyloidosis is a rare group of disorders with an annual incidence of eight patients per million and is characterized by pathological deposition of fibrillar protein named amyloid, which disrupts organ structure and function[1]. The diagnosis of amyloidosis requires a high index of suspicion since the symptoms are nonspecific and may involve a single or multiple organ systems. Additionally, slow progression of the disease often delays diagnosis causing limited or palliative treatments. The manifestation of amyloidosis can be classified as primary, secondary, localized, or familial with prognosis varying in regards to the specific type of disease process[2,3].
Localized amyloidosis, an extremely rare condition, is limited to a single organ. Furthermore, systemic features such as urinary and serum monoclonal proteins and/or clonal plasma cells in the bone marrow are absent making diagnosis difficult. Common sites of organ-restricted deposition include respiratory[4,5], genitourinary tract[6,7], in addition to, skin and soft tissue[8,9]. The mechanism underlying the formation of a localized amyloidoma remains poorly understood. De novo amyloid production[10], in addition to, local plasmacytosis in chronic inflammatory diseases[6,11] have been proposed for tissue restricted amyloidoma. Additionally, localized amyloid has been found to arise from certain fibrillary proteins produced by neoplasms such as calcitonin in medullary thyroid carcinoma[12,13], amylin in insulinoma[14] or prolactin in prolactinoma[15,16].
Localized amyloidoma of the gastrointestinal tract is extremely unusual. All reported cases affecting the large bowel presented clinically with lower gastrointestinal bleeding[17-20]. Rarely amyloid of the colon produces a mass lesion causing obstructive symptoms[21]. Only two cases have been described in literature for rectal amyloidoma[22,23]. This case study is a rare account of the presentation of rectal amyloidoma and its surgical resection using an older but sophisticated surgical device, transanal endoscopic microsurgery (TEM).
A 66-year-old Caucasian male with past medical history of diabetes mellitus type II, hypertension, hyperlipidemia, and obstructive sleep apnea presented with unusual lower abdominal pain in September 2013. On digital rectal examination, the lesion was easily graspable and characterized as a hard, lobulated mass at the dentate line. Computed tomography scan was obtained, which showed a thickening of the left lower rectal wall with adjacent free gas due to the local perforation of the amyloidoma (Figure 1). A follow up colonoscopy found an irregular, poor defined, semi circumferential rectal mass occupying about 50% of the rectal lumen located 2 cm from the dentate line and biopsy of the mass was taken. Pathology evaluation demonstrated abnormal deposit, which was found to be positive for congo red stain and was confirmed to be a rectal amyloidoma. No personal or family history of amyloid diseases or chronic inflammatory diseases was reported.
Proper workup was performed to assess for systemic amyloidosis. Serum blood count, comprehensive metabolic panel, coagulation studies, and liver and kidney function tests were all within standard limits. Serum total protein, albumin, alpha-1 globulin, alpha-2 globulin, beta globulin, and gamma globulin were normal. Urine analysis revealed a low level of monoclonal peak is present on electrophoretogram but was too small to quantitate and immunofixation yielded no abnormal bands. Furthermore, serum free kappa and free lambda protein levels were within regular limits resulting in a normal free kappa:lambda ratio of 1.02 (0.26-1.65). Chest X-ray, electrocardiogram, and echocardiogram showed no findings. Conclusively, work up was negative for systemic amyloidosis.
Amyloidoma of the rectum is an extremely rare rectal tumor. Lesions this low and of this size are more commonly treated by radical surgical intervention (low anterior resection or abdominal perineal resection) to achieve negative margins and evaluate the lymphovascular system for invasion. Due to the benign behavior of localized amyloid tumors, we offered the patient a local excision with a TEM.
TEM includes an adjustable, multi-port proctoscope combined with CO2 mediated insufflation for optimal exposure of the rectum. This closed in-vivo system is then connected to a stereoscopic angulated optical system, which allows visualization and projection on a screen with higher resolution capabilities.
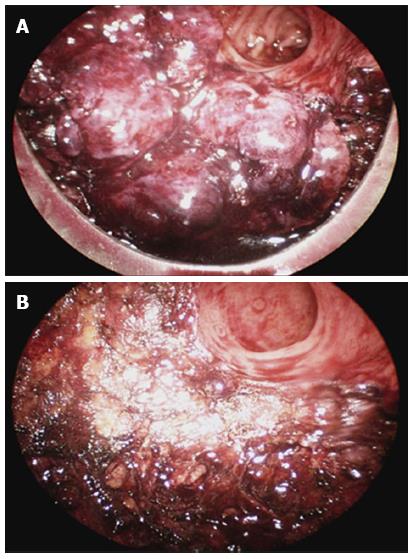
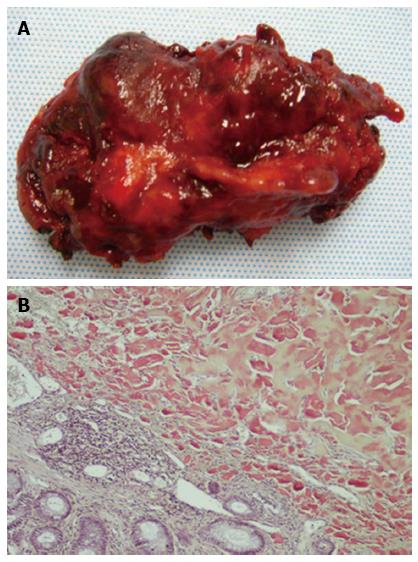
Briefly, for this case, the patient was placed in a lithotomy position. After examination of the rectum with a rigid, beveled, proctoscope, patient was positioned appropriately to localize the lesion inferiorly. The TEM device was connected to the anesthesia table. The TEM proctoscope was advanced to visualize the lesion in the left posterior aspect of the rectum at the inferior part of the TEM proctoscope (Figure 2A). Insufflation of CO2 was started. The diameter of the patient’s rectum was too large to keep the lesion in the center, which led to mobilization of the lesion 1 cm distally and using this edge as a handle in order to allow optimal exposure for full thickness excision of the rectal wall using the monopolar cautery. After establishing the posterior dissection, we advanced in the mesorectal fat where the mass was divided full-thickness circumferentially from left and right and lastly, proximal aspect (Figure 2B). Small bleeding was controlled with the cautery device. The mass was completely excised, margins were obtained, and specimen was sent for pathology (Figure 3A). The defect was left open due to the large size and the lack of bleeding after cautery, in addition to, decreasing the likelihood of complications such as abscess formation and increased pain that have occurred in previous TEM cases when closing the defect.
Post-operatively, the patient did not have any bleeding from the surgical site and was able to go home the same day of surgery after recovering from anesthesia. Patient was gas incontinent for 2 wk post-operatively but resumed normal bowel habits afterwards without any local recurrence thus far. Findings of the histopathological report revealed acellular, homogenous, eosinophilic material underlying benign colonic mucosa positive for congo red stain and identified as local rectal amyloidoma (Figure 3B). Small fibers of the internal sphincter were also noted within the specimen (Figure not shown).
Many classifications have emanated for Amyloidosis over the years due to the advancement in knowledge for the disease process. Amyloidosis can be classified into four major categories. Primary amyloidosis, also known as immunoglobulin light chain amyloidosis, is diagnosed in individuals without previous diseases or coexisting conditions except multiple myeloma. Secondary or reactive amyloidosis is associated with chronic inflammatory conditions resulting in accumulation of hazardous byproducts. Familial amyloidosis includes variety of heritable mutations of proteins, such as transthyretin (TTR - most common form), apolipoprotein A-I, fibrinogen, cystatin and gelsolin[2,3]. Furthermore, the central nervous system and its’ exclusive environment is susceptible to amyloid deposition, which manifests as various forms of familial dementias[24]. The gastrointestinal system is a common site of amyloid deposition in patients with primary amyloidosis (70%) and secondary amyloidosis (50%) and the colon is frequently involved within the multi-systemic disease process[25]. However, single organ or localized form of amyloidosis, without systemic involvement, is rarely found in the colon[26-28].
Localized amyloidomas of the gastrointestinal track are extremely rare, usually affecting the colon with bleeding as a chief complaint due to the lesion outgrowing the blood supply causing necrosis. In this case review, a low rectal amyloidoma, measuring 5 cm and occupying 50% circumference, presented with unusual obstructive symptoms and surgery was performed with the first TEM approach for full-thickness excision to treat this organ restricted amyloidosis. TEM is discovered in Germany, gained much popularity in Europe for resection of large rectal tumors since 1983. However, the US, housing merely 9% of TEM systems worldwide, has considered the technique appropriate only for the treatment of early rectal cancers and rectal adenomas[29,30]. Due to the characteristics of localized amyloidomas such as absence of systemic disease, slow growth of the lesion with clearly defined margins, and no malignant transformation, resection is the best treatment. TEM is proposed as the most optimal technique for resection of a low rectal lesion due to its allowance for superior visualization with adequate insufflation, so that the lesion can be clearly seen and removed with adequate margins while preserving all functionality of the gastrointestinal tract instead of a radical surgery that requires a colostomy. Furthermore, several studies have compared the use of TEM versus the conventional transanal resection for removal of localized rectal lesions[29,31-35]. These studies demonstrate TEM to have a markedly higher rate of negative margins and a significantly lower incidence rate of local recurrence. In addition, TEM allows for accurate pathological evaluation for staging of rectal lesions. Furthermore, TEM offers a less invasive option for full-thickness excision, which is much preferred over a partial wall, piecemeal endoscopic resection[29].
Diagnosis of localized amyloidosis is challenging owing to the non-specific clinical presentation, normal serum and urine protein screen, frequent lack of family history, and the rarity of organ-restricted amyloidosis. It is imperative to establish the correct diagnosis so that unnecessary procedures, incorrect therapy, and delay of diagnosis can be avoided to afford the patient the best chance for a cure, often by a surgical intervention. TEM is a safe, minimally invasive procedure that provides significantly lower morbidity and mortality as compared to traditional treatments for rectal lesions. Functional outcomes are better since sphincter complex is preserved while having minimal to no damage to the pelvic region/structures. This technique provides superior visibility due to the stereoscopic capability in combination with revolutionary instrumentation that allows manipulation of larger and difficult to reach lesions. Also, use of both hands of the surgeon gives better exposure and precise excision of the lesion. More importantly, TEM has minor complications and the patient in this case was able to receive the procedure on an outpatient basis with restoration of normal bowel function within 2 wk. The patient will have close follow up of every 6 mo for surveillance of local recurrence, an extremely rare and almost negligible occurrence. Conclusively, TEM could prove to be an excellent, non-invasive, and effective technique for removal of large rectal lesions such as an amyloidoma.
Patient presented with lower abdominal pain.
Digital rectal examination revealed a hard, lobulated, and easily graspable lesion at the dentate line.
Due to the symptoms and physical exam findings, computed tomography (CT) was the appropriate next step which revealed thickening of left lower rectal wall with adjacent free air. Follow up colonoscopy visualized an irregular and large mass with biopsies, which revealed positive congo red stain leading to the diagnosis of rectal amyloidoma.
CBC, CMP, and UA within normal limits with a normal free serum kappa:lambda ratio of 1.02 (0.26-1.65) leading to exclusion of systemic amyloidosis.
CT scan showed thickening of the left lower rectal wall with adjacent free gas due to the local perforation of the amyloidoma.
Acellular, homogenous, eosinophilic deposit underlying benign colonic mucosa positive for congo red stain and identified as local rectal amyloidoma.
Full-thickness excision of the rectal amyloidoma using transanal endoscopic microsurgery (TEM) without hospitalization and complications.
Rectal amyloidosis is a very rare entity that presents with non-specific symptoms requiring a high index of suspicion to establish the correct diagnosis so that the patient can receive timely surgical intervention, which often leads to cure.
Localized amyloidoma is a benign, pathological deposition of fibrillar protein named amyloid, which can disrupt organ structure and function.
The successful treatment for this rectal amyloidoma using TEM emphasizes the need to broaden its application worldwide.
The case report is an intresting case presentation of a rare rectal disorder. Gastrointestinal manifestations of localized amyloidoma are unusual, which makes amyloidoma restricted to the rectum a very rare diagnosis requiring a high index of suspicion. Using TEM as a surgical treatment for it is worth to try.
P- Reviewer: Heise, CP, Mayol J, Sipos F, Tong WD S- Editor: Ma YJ L- Editor: A E- Editor: Zhang DN
| 1. | Gertz MA, Lacy MQ, Dispenzieri A, Hayman SR. Amyloidosis. Best Pract Res Clin Haematol. 2005;18:709-727. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 53] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 2. | Falk RH, Comenzo RL, Skinner M. The systemic amyloidoses. N Engl J Med. 1997;337:898-909. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 900] [Cited by in RCA: 794] [Article Influence: 28.4] [Reference Citation Analysis (0)] |
| 3. | Hazenberg BP. Amyloidosis: a clinical overview. Rheum Dis Clin North Am. 2013;39:323-345. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 112] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 5. | Rubinow A, Celli BR, Cohen AS, Rigden BG, Brody JS. Localized amyloidosis of the lower respiratory tract. Am Rev Respir Dis. 1978;118:603-611. [PubMed] |
| 6. | Fujihara S, Glenner GG. Primary localized amyloidosis of the genitourinary tract: immunohistochemical study on eleven cases. Lab Invest. 1981;44:55-60. [PubMed] |
| 7. | Lim JH, Kim H. Localized amyloidosis presenting with a penile mass: a case report. Cases J. 2009;2:160. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Pasternak S, Wright BA, Walsh N. Soft tissue amyloidoma of the extremities: report of a case and review of the literature. Am J Dermatopathol. 2007;29:152-155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 29] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 9. | Habermann MC, Montenegro MR. Primary cutaneous amyloidosis: clinical, laboratorial and histopathological study of 25 cases. Identification of gammaglobulins and C3 in the lesions by immunofluorescence. Dermatologica. 1980;160:240-248. [PubMed] |
| 10. | Hamidi Asl K, Liepnieks JJ, Nakamura M, Benson MD. Organ-specific (localized) synthesis of Ig light chain amyloid. J Immunol. 1999;162:5556-5560. [PubMed] |
| 11. | Bhagwandeen BS, Taylor S. Primary localized amyloidosis of the bladder with a monoclonal plasma cell infiltrate. Pathology. 1988;20:67-69. [PubMed] |
| 12. | Sletten K, Westermark P, Natvig JB. Characterization of amyloid fibril proteins from medullary carcinoma of the thyroid. J Exp Med. 1976;143:993-998. [PubMed] |
| 13. | Schimke RN, Hartmann WH. Familial amyloid-producing medullary thyroid carcinoma and pheochromocytoma. A distinct genetic entity. Ann Intern Med. 1965;63:1027-1039. [PubMed] |
| 14. | Westermark P, Wernstedt C, Wilander E, Hayden DW, O’Brien TD, Johnson KH. Amyloid fibrils in human insulinoma and islets of Langerhans of the diabetic cat are derived from a neuropeptide-like protein also present in normal islet cells. Proc Natl Acad Sci USA. 1987;84:3881-3885. [PubMed] |
| 15. | Kubota T, Kuroda E, Yamashima T, Tachibana O, Kabuto M, Yamamoto S. Amyloid formation in prolactinoma. Arch Pathol Lab Med. 1986;110:72-75. [PubMed] |
| 16. | Jiménez L, Rivera ML, Ferrá S, Colón LE, Carro E. Prolactinoma with extensive amyloid deposits: a case report. P R Health Sci J. 2008;27:343-345. [PubMed] |
| 17. | Threlkeld C, Nguyen TH. Isolated amyloidosis of the colon. J Am Osteopath Assoc. 1996;96:188-190. [PubMed] |
| 18. | Bergman F. Amyloid “tumour” in sigmoid colon. Acta Pathol Microbiol Scand. 1962;55:395-400. [PubMed] |
| 19. | Watanabe T, Kato K, Sugitani M, Kaneda N, Hoshino N, Imatake K, Matsui T, Kawamura F, Iwasaki A, Arakawa Y. A case of solitary amyloidosis localized within the transverse colon presenting as a submucosal tumor. Gastrointest Endosc. 1999;49:644-647. [PubMed] |
| 20. | Hirata K, Sasaguri T, Kunoh M, Shibao K, Nagata N, Itoh H. Solitary “amyloid ulcer” localized in the sigmoid colon without evidence of systemic amyloidosis. Am J Gastroenterol. 1997;92:356-357. [PubMed] |
| 21. | Deans GT, Hale RJ, McMahon RF, Brough WA. Amyloid tumour of the colon. J Clin Pathol. 1995;48:592-593. [PubMed] |
| 22. | Zaky ZS, Liepnieks JJ, Rex DK, Cummings OW, Benson MD. Lambda II immunoglobulin light chain protein in primary localized rectal amyloidosis. Amyloid. 2007;14:299-304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 23. | Senapati A, Fletcher C, Bultitude MI, Jackson BT. Amyloid tumour of the rectum. J R Soc Med. 1995;88:48P-49P. [PubMed] |
| 24. | Glenner GG, Wong CW. Alzheimer’s disease: initial report of the purification and characterization of a novel cerebrovascular amyloid protein. Biochem Biophys Res Commun. 1984;120:885-890. [PubMed] |
| 25. | Sattianayagam PT, Hawkins PN, Gillmore JD. Systemic amyloidosis and the gastrointestinal tract. Nat Rev Gastroenterol Hepatol. 2009;6:608-617. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 83] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 26. | Jensen K, Raynor S, Rose SG, Bailey ST, Schenken JR. Amyloid tumors of the gastrointestinal tract: a report of two cases and review of the literature. Am J Gastroenterol. 1985;80:784-786. [PubMed] |
| 27. | John A, Dickey K, Fenwick J, Sussman B, Beeken W. Pneumatosis intestinalis in patients with Crohn’s disease. Dig Dis Sci. 1992;37:813-817. [PubMed] |
| 28. | Johnson DH, Guthrie TH, Tedesco FJ, Griffin JW, Anthony HF. Amyloidosis masquerading as inflammatory bowel disease with a mass lesion simulating a malignancy. Am J Gastroenterol. 1982;77:141-145. [PubMed] |
| 29. | Morino M, Arezzo A, Allaix ME. Transanal endoscopic microsurgery. Tech Coloproctol. 2013;17 Suppl 1:S55-S61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 20] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 30. | Saclarides TJ. Transanal endoscopic microsurgery. Semin Laparosc Surg. 2004;11:45-51. [PubMed] |
| 31. | Casadesus D. Surgical resection of rectal adenoma: a rapid review. World J Gastroenterol. 2009;15:3851-3854. [PubMed] |
| 32. | de Graaf EJ, Burger JW, van Ijsseldijk AL, Tetteroo GW, Dawson I, Hop WC. Transanal endoscopic microsurgery is superior to transanal excision of rectal adenomas. Colorectal Dis. 2011;13:762-767. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 98] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 33. | Langer C, Liersch T, Süss M, Siemer A, Markus P, Ghadimi BM, Füzesi L, Becker H. Surgical cure for early rectal carcinoma and large adenoma: transanal endoscopic microsurgery (using ultrasound or electrosurgery) compared to conventional local and radical resection. Int J Colorectal Dis. 2003;18:222-229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 109] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 34. | Moore JS, Cataldo PA, Osler T, Hyman NH. Transanal endoscopic microsurgery is more effective than traditional transanal excision for resection of rectal masses. Dis Colon Rectum. 2008;51:1026-1030; discussion 1026-1030. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 272] [Cited by in RCA: 253] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 35. | Wu Y, Wu YY, Li S, Zhu BS, Zhao K, Yang XD, Xing CG. TEM and conventional rectal surgery for T1 rectal cancer: a meta-analysis. Hepatogastroenterology. 2011;58:364-368. [PubMed] |