Published online Sep 14, 2015. doi: 10.3748/wjg.v21.i34.10018
Peer-review started: October 6, 2014
First decision: October 29, 2014
Revised: March 16, 2015
Accepted: April 9, 2015
Article in press: April 9, 2015
Published online: September 14, 2015
Processing time: 344 Days and 1.3 Hours
AIM: To investigate the accuracy and inter-observer variation of bowel sound assessment in patients with clinically suspected bowel obstruction.
METHODS: Bowel sounds were recorded in patients with suspected bowel obstruction using a Littmann® Electronic Stethoscope. The recordings were processed to yield 25-s sound sequences in random order on PCs. Observers, recruited from doctors within the department, classified the sound sequences as either normal or pathological. The reference tests for bowel obstruction were intraoperative and endoscopic findings and clinical follow up. Sensitivity and specificity were calculated for each observer and compared between junior and senior doctors. Interobserver variation was measured using the Kappa statistic.
RESULTS: Bowel sound sequences from 98 patients were assessed by 53 (33 junior and 20 senior) doctors. Laparotomy was performed in 47 patients, 35 of whom had bowel obstruction. Two patients underwent colorectal stenting due to large bowel obstruction. The median sensitivity and specificity was 0.42 (range: 0.19-0.64) and 0.78 (range: 0.35-0.98), respectively. There was no significant difference in accuracy between junior and senior doctors. The median frequency with which doctors classified bowel sounds as abnormal did not differ significantly between patients with and without bowel obstruction (26% vs 23%, P = 0.08). The 53 doctors made up 1378 unique pairs and the median Kappa value was 0.29 (range: -0.15-0.66).
CONCLUSION: Accuracy and inter-observer agreement was generally low. Clinical decisions in patients with possible bowel obstruction should not be based on auscultatory assessment of bowel sounds.
Core tip: Abdominal auscultation is often used in clinical practice when bowel obstruction is suspected; the usefulness is poorly documented. Early diagnosis and treatment of bowel obstruction is imperative to reduce the risk of intestinal strangulation, necrosis and perforation. Clinicians must know which components to focus on in the physical examination. The present study shows a generally low accuracy and inter-observer agreement when recorded bowel sounds from 98 patients were assessed by 53 doctors. No difference in accuracy was observed between junior and senior doctors. Clinical decisions in patients with possible bowel obstruction should not depend on auscultatory assessment of bowel sounds.
- Citation: Breum BM, Rud B, Kirkegaard T, Nordentoft T. Accuracy of abdominal auscultation for bowel obstruction. World J Gastroenterol 2015; 21(34): 10018-10024
- URL: https://www.wjgnet.com/1007-9327/full/v21/i34/10018.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i34.10018
Bowel obstruction is a common emergency condition in abdominal surgery[1]. The risk of complications of bowel obstruction such as intestinal strangulation, necrosis and perforation are reported to be as high as 5%-16%[2,3]. Early diagnosis and treatment of bowel obstruction are imperative in reducing these risks. Because of the need for prompt and reliable assessment of patients suspected of having bowel obstruction, clinicians must know which components to focus on in the history and the physical examination. Auscultation of bowel sounds is a quick and low-cost examination, and has been used for more than 150 years to assess various abdominal conditions[4]. Contemporary textbooks often state that hyperactive, tinkling, metallic or high-pitched bowel sounds are characteristic clinical findings in patients with bowel obstruction[5-8], but the evidence supporting the clinical utility of these findings is sparse. Two prospective studies in patients with acute abdominal pain found that increased[9] or abnormal[10] bowel sounds were independent markers of bowel obstruction. However, these studies did not assess the influence of observer variation in bowel sound assessments. In clinical practice, the description and assessment of bowel sounds is often vague and inconclusive[11]. Hence, previous studies have demonstrated low to moderate inter-observer agreement for bowel sound assessment[12-16].
Had abdominal auscultation not been such a cheap investigation, it would probably not have survived for more than 150 years[4]-given the very limited documentation of its clinical value.
The aim of this study was to investigate the accuracy and inter-observer agreement for bowel sound assessment in patients suspected of intestinal obstruction.
Patients aged 16 years or older admitted with suspected intestinal obstruction or constipation to the Department of Surgery, Hvidovre University Hospital, Denmark were included. No exclusion criteria were considered relevant. Within 24 h of admission, bowel sounds were recorded by one of the authors using a 3M Littmann® Electronic Model 3000 Stethoscope. The stethoscope can record six sound sequences, each of eight seconds duration. The recording is continuous and the final eight seconds of each sequence are saved once the recording is stopped.
The protocol for recording bowel sounds was as follows: the abdomen was auscultated in quadrants until bowel sounds were heard in any quadrant. Six sound sequences of eight seconds were then recorded in this quadrant.
For each patient, three of the six sound sequences considered superior in respect of volume and noise were selected by one of the authors (BB), who was blinded to the patient data. These three sequences were then joined into a single sound sequence lasting 25 s, with half a second pause between the three sequences. The duration of the joined sequences was assessed as being representative of the time taken to perform auscultation in clinical practice. Because the native file format of the stethoscope is not directly playable on a regular PC, the files were converted into playable .wav files.
Hence, for each patient a 25 s sound sequence was created and used for assessment.
Following acquisition of this data, all doctors working in the department from November 2007 to November 2008 were invited to evaluate the bowel sounds as described below. In order to evaluate the impact of experience, doctors were divided into junior and senior groups. Consultants and senior registrars were considered seniors. A website was designed (English version available at http://www.bowel-sounds.com) where the participating doctors accessed and evaluated the bowel sounds. Each participating doctor received a personal log-on to the website and the sound files were arranged in a randomized order unique to the log-on.
In order to achieve uniformity in respect of the listening environment, doctors were instructed to use headphones (supplied) during their evaluation.
After each bowel sound sequence, doctors were asked to evaluate whether the sound sequence was either pathological or normal. The sequence was repeated until it was evaluated. It was possible to listen to all the sound sequences in a row or to log in at a later date and listen to the remaining sequences. Evaluations could not be revised once complete.
Doctors were considered to be included in the study when they logged-in to the study website for the first time. Doctors were considered excluded if they did not evaluate all sounds.
The final diagnosis for each patient was extracted from medical records six months after recording of the bowel sounds. Bowel obstruction was defined in three ways: (1) based on laparotomy findings; (2) endoscopic therapy with attempted or successful colorectal stenting; and (3) bowel obstruction found at autopsy. The discharge diagnoses were extracted for patients who recovered without laparotomy or stenting, and in patients who died from causes other than bowel obstruction.
To determine accuracy, sensitivity, specificity, positive predictive value and negative predictive value were calculated for each doctor’s bowel sound assessments (pathological or normal sounds vs bowel obstruction or no bowel obstruction).
Median, quartiles and range were used to describe the distribution of accuracy estimates across doctors. Cochran’s test for equality of proportions in matched samples was used to assess homogeneity between doctor’s frequencies of finding pathological bowel sounds assessments[17].
Accuracy between junior and senior doctors was compared in order to determine the influence of experience. For this analysis the diagnostic odds ratio (DOR) was used as a single measure of accuracy[18]. The DOR is calculated as (tp × tn)/(fn × fp), where tp, tn, fn, fp is the number of patients with true-positive, true-negative, false-negative and false-positive bowel sound assessments, respectively.
A paired t-test was used to compare mean values of DOR between junior and senior doctors, and the Mann-Whitney U-test was used to compare across doctors the median proportion with pathological bowel sounds between patients with and without bowel obstruction.
Inter-observer agreement was assessed using the Kappa statistic (κ), which is calculated as observed agreement (po) beyond chance agreement (pc) divided by perfect agreement beyond chance agreement: Κ = (po-pc)/(1-pc). In the common interpretation, Kappa is a measure of inter-observer agreement adjusted for chance agreement. Landis and Koch have proposed the following classification of κ values[19]: less than zero signifies poor agreement, 0-0.20 slight agreement, 0.21-0.40 fair agreement, 0.41-0.60 moderate agreement, 0.61-0.80 substantial agreement and 0.81-1 excellent agreement. κ was calculated for all possible pairs of doctors, and for pairs of junior as well as senior doctors. The resulting distributions of Kappa values were described by median, quartiles and range. Due to the influence of prevalence on the Kappa estimate, no tests of statistical significance were performed as part of the sensitivity analyses for inter-observer agreement. All analyses were performed using STATA 9 software.
The study design was presented to the local research ethics committee before study start. The committee did not consider a formal assessment procedure necessary. Verbal informed consent was obtained from patients prior to inclusion.
Bowel sounds from 102 patients were recorded between October 2005 and September 2006. Four patients were excluded: The final diagnoses were missing in three patients because insufficient data was registered to identify the patients’ files, and in one case bowel sounds were recorded after surgery. Therefore, the analyses are limited to 98 patients. Of these patients, the median age was 66 years (range: 19-96 years) and 53 were women. Between November 2007 and October 2008 fifty-four doctors were included in the study, of these 34 were junior and 20 were senior doctors. One junior doctor was subsequently excluded due to incomplete assessment of all the bowel sound sequences.
Forty-seven patients underwent laparotomy and 35 had intraoperative findings consistent with bowel obstruction. 20 patients had small bowel obstruction and 15 large bowel obstruction. In addition, two patients underwent colorectal stenting due to large bowel obstruction. No findings of bowel obstruction were revealed on autopsy. Laparotomies and endoscopies were performed within two days of the bowel sound recordings in 46 patients (94%) and within five days in the remaining three patients. Discharge diagnoses in patients without bowel obstruction are summarized in Table 1.
| Diagnosis | Number of patients |
| Constipation | 34 |
| Appendicitis | 5 |
| Gastroenteritis | 3 |
| Perforated viscous organ | 3 |
| Cholecystitis | 3 |
| Intestinal ischemia | 2 |
| Other | 11 |
| Total | 61 |
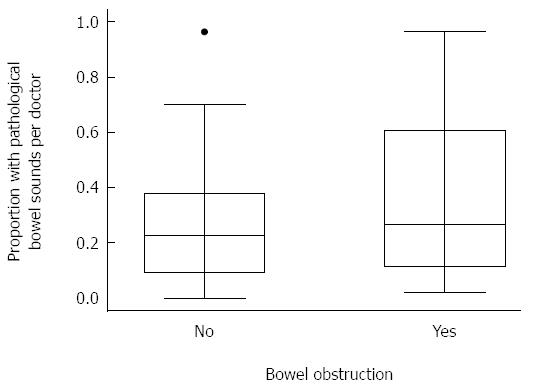
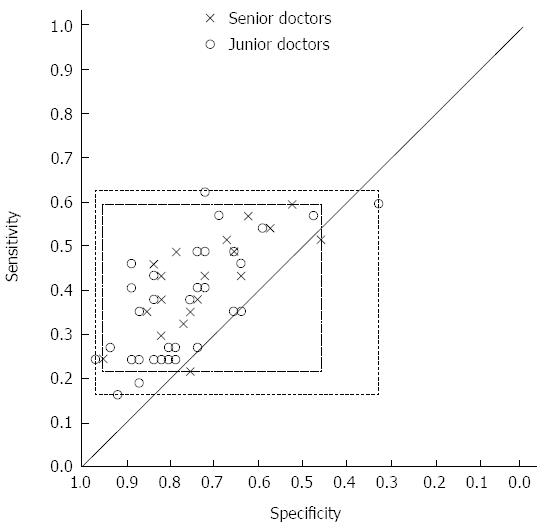
The proportion of patients in which doctors evaluated the bowel sounds as pathological varied widely between doctors (median 0.28, range: 0.11-0.64) and statistically significantly (P < 0.001, Cochran’s test, 52 degrees of freedom). Across doctors, the median of the proportion of patients with pathological bowel sounds was slightly higher in patients with bowel obstruction than in patients without (Figure 1), but the difference was not statistically significant (26% vs 23%, P = 0.08, Mann Whitney U-test). For all 53 doctors the median sensitivity and specificity of pathological bowel sounds with respect to bowel obstruction was 0.42 (range: 0.19-0.64) and 0.78 (range: 0.35-0.98), respectively. Figure 2 shows the distribution of estimates of sensitivity and specificity. The median positive and negative predictive value was 0.48 (range: 0.35-0.82) and 0.67 (range: 0.57-0.76), respectively. There was no difference in accuracy between the 33 junior and the 20 senior doctors (geometric means of DOR: 2.138 vs 2.132, respectively, P = 0.99, paired t-test).
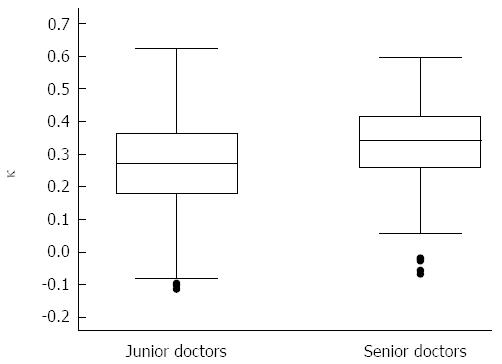
The 53 doctors were paired with each other in 1378 unique pairs. For these pairs, the median observed agreement was 0.70 (range: 0.38-0.91) and the median value of Kappa was 0.29 (range: -0.15-0.66). The interquartile range of Kappa values was 0.20-0.38; hence, Kappa estimates were fair or worse in 75% of the pairs. The median Kappa value was marginally higher in 190 pairs of senior doctors compared to 528 pairs of junior doctors (0.34 vs 0.27) (Figure 3). The median proportion of patients with pathological bowel sounds was also slightly higher among senior than among junior doctors (0.30 vs 0.24).
In this prospective multi-observer study we found low accuracy of bowel sound assessment for bowel obstruction, with estimates of sensitivity and specificity varying considerably between observers. Inter-observer agreement was also low. The variability in estimates of sensitivity and specificity is not surprising, since there is no validated classification of bowel sounds. The variation in the proportion of patients with pathological sounds across doctors indicates that the threshold of abnormality varied between observers. Some of this variation could be due to observers focusing on different qualitative aspects of the sounds (high pitched, metallic tinkling, roaring, loud etc.). A liberal threshold (i.e., a higher proportion with pathological sounds) will lead to higher sensitivity and lower specificity, whereas a more stringent threshold will lead to lower sensitivity and higher specificity.
Variation in threshold for abnormality is probably also an important factor in explaining the poor inter-observer agreement. Observer agreement was slightly higher between senior than between junior doctors (Kappa: 0.34 vs 0.27). However, comparison of Kappa values is challenging, because Kappa varies with the prevalence of abnormality[20]. Hence, a part of the difference is accounted for by the higher median frequency of pathological assessments among senior doctors. Previous studies of inter-observer variation in bowel sound assessment have reported moderate or low Kappa values[12,14,15], but none of these values are directly comparable to ours. For comparison, studies on inter-observer agreement for heart and lung auscultation have found mean Kappa values of
-0.02-0.55 for findings such as systolic murmurs, bronchial breath sounds and prolonged expiration[21,22].
Three previous studies have reported accuracy estimates for the clinical assessment of bowel sounds in patients with possible bowel obstruction. In a study similar to the present study, Gu et al[14] presented 20 physicians with 60-s sequences of digitally recorded bowel sounds from 20 healthy volunteers, nine patients with ileus and seven patients with bowel obstruction. The average proportion of correctly identified sound sequences from patients with bowel obstruction was 0.42, which is similar to the median sensitivity (0.42) in our study. No estimate of average specificity was reported by Gu et al[14]. In another study, 100 physicians were presented with 60-s sequences of bowel sounds from four healthy volunteers and eight emergency patients from the surgical ward[13]. Digitally recorded bowel sounds were played on a hearing aid loudspeaker in a wooden dummy with a linoleum covering. Physicians auscultated the covering and evaluated bowel sounds as either normal or pathological. In six patients with bowel obstruction and the four volunteers, average sensitivity and specificity were 64% and 72%, respectively. Compared with our results, sensitivity was substantially higher and specificity slightly lower. However, accuracy is generally higher in studies with separate sampling of cases and healthy controls than in cohort studies, such as ours, that include grey-zone patients with clinical findings that mimic the condition of interest[23]. In the third study, information from history and clinical examination was recorded prospectively in 1254 patients presenting with acute abdominal pain[9]. The prevalence of bowel obstruction was 4%, and sensitivity and specificity of increased bowel sounds were 40% and 89%, respectively. Again, sensitivity is close to the median sensitivity in the present study, whereas specificity is higher than our median specificity (0.78). However, improved performance is unsurprising since the observers were aware of other markers of bowel obstruction such as distended abdomen, history of vomiting, and previous surgery. This knowledge is likely to be incorporated in the assessment of the bowel sounds and improve accuracy[24].
A recent study into evaluation of bowel sounds found inter-observer agreement among physicians which was slight to fair; however, this study involved only four healthy volunteers and eight emergency patients from a surgical gastroenterological ward[16].
The main strengths of the present study lie in the high number of both patients and observers, the prospective cohort design and the use of digital bowel sound recorded from a relevant study population in a typical clinical setting. These recordings ensured that all observers assessed exactly the same bowel sounds and eliminated assessment bias from other clinical findings. It could be argued that our model is poorly representative of the clinical situation because the length of the sound sequences was too short, because auscultation was limited to a single abdominal quadrant and because the bowel sounds were selected and processed to reduce noise artefacts before presentation to the observers. Pathological bowel sounds could be missed during the relatively short sound sequences, particularly in patients with bowel obstruction of longer duration, where bowel sounds may occur less frequently[8]. Hence, the short duration of the sound sequences may explain the generally low sensitivity. On the other hand, in the study by Gu et al[14] referred to above, average sensitivity was comparable to ours, although the length of the sound sequences was more than twice as long (25 s vs 60 s). Thus, the low sensitivity in our study is not necessarily attributable to the length of the sound sequences. Auscultation was limited to a single quadrant, which appears to be equivalent to auscultating all four abdominal quadrants[25]. Lastly, by selecting and processing the bowel sound recordings to improve the signal to noise ratio we may have introduced a bias that exaggerates accuracy and observer agreement. However, processing was minimal, so the potential overestimation, if such exists, is small.
The results of the present study question the usefulness of abdominal auscultation in patients with suspected bowel obstruction. Likewise, a recent study of spectral analysis of bowel sounds recorded with an electronic stethoscope in patients with possible bowel obstruction concluded that auscultation of bowel sounds is non-specific and of limited significance in diagnosing bowel obstruction[26]. We are aware of no systematic account of surgeons use of bowel sound assessment in patients with suspected bowel obstruction. In our experience, some surgeons incorporate bowel sound assessment in their clinical evaluation of such patients, others do not. Furthermore, textbooks state that abnormal bowel sounds are characteristic findings in patients with bowel obstruction and medical students are trained in abdominal auscultation. Our results indicate that assessment of bowel sounds is subjective and inaccurate. Thus, the tradition for bowel sound assessment in patients with suspected bowel obstruction is not supported by our results.
Only obstructive bowel disease was assessed and not, e.g., paralytic ileus or other conditions. No repeated assessments on the same patients were performed, to reveal pathology if there was a change in bowel sounds over time.
The present study does not examine the possibility of improvements by training. There is a possibility that the diagnostic value increases with the addition of patient history and other findings.
In conclusion, the accuracy and inter-observer agreement of bowel sound assessment in patients with possible bowel obstruction was low in both senior and junior doctors in a surgical department. Clinical decisions in patients with possible bowel obstruction should not be based on auscultatory assessment of bowel sounds.
Abdominal auscultation is regularly used when bowel obstruction is suspected, but its usefulness is poorly documented.
Correlation between abdominal auscultation and bowel obstruction has been reported, but the extent of the clinical value has not.
Imaging technologies are continuously improved. Since abdominal auscultaton is useless it should be abandoned in countries with access to imaging technologies.
Since abdominal auscultation is useless, it should be abandoned in order to avoid delayed diagnosis or even misjudgement of patients with suspected bowel obstruction.
Abdominal auscultation has no validated terminology. The authors chose to use broad terms “pathological” and “normal” and let each observer decide what constitutes pathological.
Only obstructive bowel disease was assessed and not e.g., paralytic ileus or other conditions. No repeated assessments on the same patients were performed, to reveal pathology if there is a change in bowel sounds over time. The present study does not examine the possibility of improvements by training. There is a possibility that the diagnostic value increases with the addition of patient history and other findings.
P- Reviewer: Decorti G, Grundmann O, Sadik R S- Editor: Ma YJ L- Editor: Logan S E- Editor: Liu XM
| 1. | Irvin TT. Abdominal pain: a surgical audit of 1190 emergency admissions. Br J Surg. 1989;76:1121-1125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 171] [Cited by in RCA: 147] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 2. | Fevang BT, Fevang J, Stangeland L, Soreide O, Svanes K, Viste A. Complications and death after surgical treatment of small bowel obstruction: A 35-year institutional experience. Ann Surg. 2000;231:529-537. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 145] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 3. | Markogiannakis H, Messaris E, Dardamanis D, Pararas N, Tzertzemelis D, Giannopoulos P, Larentzakis A, Lagoudianakis E, Manouras A, Bramis I. Acute mechanical bowel obstruction: clinical presentation, etiology, management and outcome. World J Gastroenterol. 2007;13:432-437. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 158] [Cited by in RCA: 152] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 4. | Hooker C. An Essay on Intestinal Auscultation. Boston Med Surg J. 1849;1439-1440. |
| 5. | Chang GJ, Shelton AA, Welton ML. Current Diagnosis & Treatment Surgery. 13th ed. 2009;647-697 Available from: http://books.google.com/books?id=a14yDQKv4vMC&pgis=1. |
| 6. | Houghton SG, De la Medina AR, Sarr MG. Maingot’s Abdominal Operations. 11th ed. In: Zinner M, Ashley SW, editors. 2007;479-507 Available from: http://books.google.com/books?id=EanJv7mvip0C&pgis=1. |
| 7. | Tavakkolizadeh A, Whang EE, Ashley SW, Zinner MJ. Schwartz’s Principles of Surgery. 9th ed. In: Brunicardi F, Andersen D, Billiar T, Dunn D, Hunter J, Matthews J, editors. McGraw Hill Professional; 2009: 979-1012. Available from: http://books.google.com/books?id=zGVIyHiqL5wC&pgis=1. |
| 8. | Welch JP. General considerations and mortality. Available from: http: //books.google.com/books?id=YBxsAAAAMAAJ&pgis=1. |
| 9. | Böhner H, Yang Q, Franke C, Verreet PR, Ohmann C. Simple data from history and physical examination help to exclude bowel obstruction and to avoid radiographic studies in patients with acute abdominal pain. Eur J Surg. 1998;164:777-784. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 10. | Eskelinen M, Ikonen J, Lipponen P. Contributions of history-taking, physical examination, and computer assistance to diagnosis of acute small-bowel obstruction. A prospective study of 1333 patients with acute abdominal pain. Scand J Gastroenterol. 1994;29:715-721. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 30] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Dombal FT De. The physical examination revisited. Diagnosis of acute abdominal pain. 2nd ed. Churchill Livingstone;. Bowel obstruction: differential diagnosis and clinical management. 1th ed. W.B. Saunders Company; 1991; 47-62 Available from: http://books.google.com/books?id=IXhsAAAAMAAJ&pgis=1. |
| 12. | Bjerregaard B, Brynitz S, Holst-Christensen J, Jess P, Kalaja E, Lund-Kristensen J, Thomsen C. The reliability of medical history and physical examination in patients with acute abdominal pain. Methods Inf Med. 1983;22:15-18. [PubMed] |
| 13. | Gade J, Kruse P, Andersen OT, Pedersen SB, Boesby S. Physicians’ abdominal auscultation. A multi-rater agreement study. Scand J Gastroenterol. 1998;33:773-777. [PubMed] |
| 14. | Gu Y, Lim HJ, Moser MA. How useful are bowel sounds in assessing the abdomen? Dig Surg. 2010;27:422-426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 23] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 15. | Yen K, Karpas A, Pinkerton HJ, Gorelick MH. Interexaminer reliability in physical examination of pediatric patients with abdominal pain. Arch Pediatr Adolesc Med. 2005;159:373-376. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 37] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 16. | Durup-Dickenson M, Christensen MK, Gade J. Abdominal auscultation does not provide clear clinical diagnoses. Dan Med J. 2013;60:A4620. [PubMed] |
| 17. | Fleiss JL, Levin B, Myunghee CP. The Analysis of Data from Matched Samples. Statistical Methods for Rates and Proportions. 3th ed. New York: Wiley 2003; 373-406 Available from: http://books.google.com/books?id=a5LwdxF2d10C&pgis=1. [DOI] [Full Text] |
| 18. | Glas AS, Lijmer JG, Prins MH, Bonsel GJ, Bossuyt PM. The diagnostic odds ratio: a single indicator of test performance. J Clin Epidemiol. 2003;56:1129-1135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1459] [Cited by in RCA: 1681] [Article Influence: 80.0] [Reference Citation Analysis (0)] |
| 19. | Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159-174. [PubMed] |
| 20. | Gjørup T. The kappa coefficient and the prevalence of a diagnosis. Methods Inf Med. 1988;27:184-186. [PubMed] |
| 21. | Iversen K, Greibe R, Timm HB, Skovgaard LT, Dalsgaard M, Hendriksen KV, Hrobjartsson A. A randomized trial comparing electronic and conventional stethoscopes. Am J Med. 2005;118:1289. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 22. | Iversen K, Søgaard Teisner A, Dalsgaard M, Greibe R, Timm HB, Skovgaard LT, Hróbjartsson A, Copenhagen O, Copenhagen S, Copenhagen K. Effect of teaching and type of stethoscope on cardiac auscultatory performance. Am Heart J. 2006;152:85.e1-85.e7. [PubMed] |
| 23. | Lijmer JG, Mol BW, Heisterkamp S, Bonsel GJ, Prins MH, van der Meulen JH, Bossuyt PM. Empirical evidence of design-related bias in studies of diagnostic tests. JAMA. 1999;282:1061-1066. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1223] [Cited by in RCA: 1287] [Article Influence: 49.5] [Reference Citation Analysis (0)] |
| 24. | Loy CT, Irwig L. Accuracy of diagnostic tests read with and without clinical information: a systematic review. JAMA. 2004;292:1602-1609. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 166] [Cited by in RCA: 160] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 25. | Hepburn MJ, Dooley DP, Fraser SL, Purcell BK, Ferguson TM, Horvath LL. An examination of the transmissibility and clinical utility of auscultation of bowel sounds in all four abdominal quadrants. J Clin Gastroenterol. 2004;38:298-299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 26. | Ching SS, Tan YK. Spectral analysis of bowel sounds in intestinal obstruction using an electronic stethoscope. World J Gastroenterol. 2012;18:4585-4592. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 32] [Cited by in RCA: 32] [Article Influence: 2.5] [Reference Citation Analysis (1)] |