Published online Jul 21, 2015. doi: 10.3748/wjg.v21.i27.8462
Peer-review started: February 10, 2015
First decision: April 13, 2015
Revised: April 27, 2015
Accepted: May 21, 2015
Published online: July 21, 2015
Processing time: 163 Days and 7.1 Hours
Endoscopic mucosal resection (EMR) allows the removal of flat or sessile lesions, laterally spreading tumors, and carcinoma of the colon or the rectum limited to the mucosa or the superficial submucosa. Acute appendicitis is the most common abdominal emergency requiring emergency surgery, and it is also a rare complication of diagnostic colonoscopy and therapeutic endoscopy, including EMR. In the case presented here, a 53-year-old female underwent colonoscopy due to a positive fecal occult blood test and was diagnosed with cecal adenoma. She was referred to our hospital and admitted for treatment. The patient had no other symptoms. EMR was performed, and 7 h after the surgery, the patient experienced right -lower abdominal pain. Laboratory tests performed the following day revealed a WBC count of 16000/mm3, a neutrophil count of 14144/mm3, and a C-reactive protein level of 2.20 mg/dL, indicating an inflammatory response. Computed tomography also revealed appendiceal wall thickening and swelling, so acute appendicitis following EMR was diagnosed. Antibiotics were initiated leading to total resolution of the symptoms, and the patient was discharged on the sixth post-operative day. Pathological analysis revealed a high-grade cecal tubular adenoma. Such acute appendicitis following EMR is extremely rare, and EMR of the cecum may be a rare cause of acute appendicitis.
Core tip: We report a case of a 53-year-old female who underwent colonoscopy and was diagnosed with cecal adenoma. Endoscopic mucosal resection (EMR) was performed, and she experienced right-lower abdominal pain 7 h post surgery. The following day, laboratory tests revealed a neutrophil count of 14144/mm3, and a C-reactive protein level of 2.20 mg/dL. Computed tomography also revealed appendiceal wall thickening and swelling, so acute appendicitis following EMR was diagnosed. Antibiotics were initiated leading to total symptom resolution, and the patient was discharged on the sixth post-operative day. Acute appendicitis following EMR is rare, and cecal EMR may be a rare cause of acute appendicitis.
- Citation: Nemoto Y, Tokuhisa J, Shimada N, Gomi T, Maetani I. Acute appendicitis following endoscopic mucosal resection of cecal adenoma. World J Gastroenterol 2015; 21(27): 8462-8466
- URL: https://www.wjgnet.com/1007-9327/full/v21/i27/8462.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i27.8462
Endoscopic mucosal resection (EMR), which involves snare resection of dysplastic lesions, is an endoscopic alternative to surgical resection of mucosal and submucosal neoplastic lesions and intra-mucosal cancers. Complications of EMR, including bleeding and perforation, have been reported. Appendicitis is one of the most common causes of acute abdomen and one of the most frequent indications for emergency abdominal surgery worldwide[1,2]. Appendicitis is also a rare complication of diagnostic colonoscopy and therapeutic endoscopic procedures, including EMR[3-7]. Here, we report a case of acute appendicitis following EMR of a cecal adenoma.
A 53-year-old female underwent colonoscopy following a positive fecal occult blood test, and a 15-mm cecal laterally spreading tumor (LST) was detected. The patient was then referred to our hospital and admitted for treatment of the cecal adenoma. She had no previous abdominal surgery and no history of smoking or alcohol consumption. Laboratory analysis revealed 7100 leukocytes/mm3, and a C-reactive protein (CRP) level of 0.01 mg/dL. Other parameters were also within normal limits.
On examination, the patient had a heart rate of 77 beats/min, a blood pressure of 110/62 mmHg, a temperature of 36.6 °C, and a BMI of 18.0 kg/m2. There was no abdominal pain, and her bowel sounds were normal on abdominal examination. Additionally, plain abdominal radiology demonstrated normal gas.
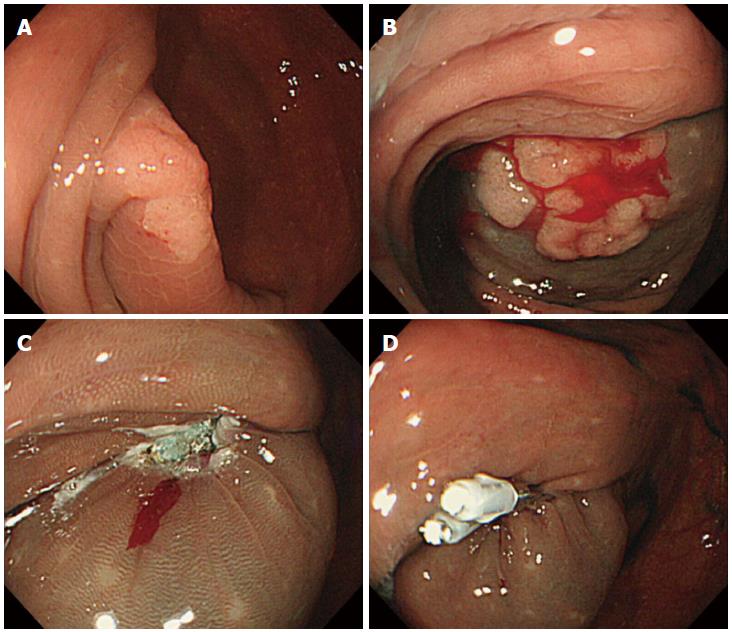
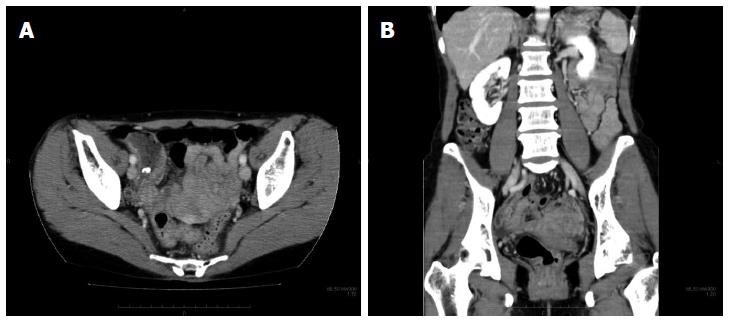
The patient underwent colonoscopy for EMR, and a large IIa LST (granular -type) was found adjacent to the orifice of appendix (Figure 1). The size of the lesion was 20 mm × 12 mm × 2 mm. There was no post-procedural bleeding. Pathological examination revealed a high-grade tubular adenoma. The patient was asymptomatic until developing mild right-lower abdominal pain 7 h after the EMR. At 20 h post-EMR, she had low-grade fever and localized rebound tenderness was present at McBurney’s point. Laboratory tests revealed a WBC count of 16000/mm3, a neutrophil count of 14144/mm3, and a CRP level of 2.20 mg/dL, indicating an inflammatory response. Intravenous antibiotics (fosfomycin sodium, 4 g/d) were initiated, and on the third postoperative day, the inflammation decreased, and the symptoms markedly improved. Abdominal and pelvic computed tomography (CT) revealed appendiceal wall thickening and swelling (Figures 2A and 2B), leading to a diagnosis of acute appendicitis following EMR.
Oral intake was resumed on the fifth postoperative day, and the patient was discharged the following day. She has remained well and symptom free since discharge.
Acute appendicitis is the most frequent cause of acute abdominal emergencies[1]. Although the precise pathogenic mechanism is unknown, potential causes include one or more of the following: bacterial infection, viral infection, a foreign body, an allergic reaction, and circulatory disease (ischemia). Blockage or stenosis of the appendiceal lumen is observed in most cases of acute appendicitis, which may be caused by foreign bodies, including food residue, fecal matter, mucous membrane epithelial hyperplasia, follicular hyperplasia, adenoma, and adenocarcinoma[2].
Acute appendicitis caused by neighboring inflammatory conditions, including enteritis, and diverticulitis, is known as non-obstructive appendicitis and is managed conservatively. Non-obstructive appendicitis may be diagnosed bases on the extent and degree of abnormal findings in the neighboring intestinal tract[8]. In particular, multi-detector CT has a sensitivity of 98.5% and a specificity of 98% for detecting acute appendicitis[9].
Physical examination is crucial in the diagnosis of acute appendicitis, and emergency surgery is considered as the standard treatment. However, the treatment of acute appendicitis has diversified due to advances in imaging and antibiotics and increasing use of laparoscopic surgery. As a result, non-operative therapy, delayed appendectomy, and interval appendectomy have all become widely accepted for patients with non-perforated appendicitis[1].
Colorectal adenomas represent the single most important premalignant lesion of the gastrointestinal tract worldwide, and large (> 20-mm) colorectal polyps have been found in 0.8%-5.2% of patients undergoing colonoscopy for different indications[10]. In general, when candidate polyps for colorectal EMR are smaller than 20-mm in size, EMR techniques achieve satisfactory rates of en bloc and complete resection. Currently, however, there are no uniformly accepted infection prevention techniques or electrocautery settings[11].
It is possible that more than one mechanism contributes to the inflammatory process, triggered by either the preparation and or the procedure itself[12]. In our case, colonoscopy was initially performed. Acute appendicitis following colonoscopy is thought to be caused by increased intra luminal pressure due to over-inflation with air and by secondary obstruction of the appendiceal orifice due to inflammation of intestinal contents, including fecaliths and fecal matter[6]. However, regardless of whether post-colonoscopy appendicitis represents an incidental finding or a true complication of colonoscopy, it is important to consider acute appendicitis as a differential diagnosis of the acute abdomen after colonoscopy[7].
Glycerol was then injected into the submucosal layer. Submucosal injection, which elevates the mucosa to be resected and protects the muscularis propria from injury, is believed to reduce thermal injury as well as the risk of perforation and hemorrhage[13]. Although glycerol is not thought to cause tissue damage[14], one study reported that submucosal injection may be due to a misdirected injection outside the bowel wall[15].
In the case described here, the LST was cut using a snare and coagulative diathermy. Post-polypectomy coagulation syndrome (PPCS), also known as post-polypectomy syndrome or transmural burn syndrome, refers to the development of abdominal pain, fever, leukocytosis, and peritoneal inflammation in the absence of frank perforation following colonoscopic polypectomy with electrocoagulation[16-25]. Recognition of PPCS is important to avoid unnecessary exploratory laparotomy because the syndrome has been shown to resolve with conservative treatment in most patients.
The EMR ulcer was sutured with two clips in the current case. Recently, it was reported that prophylactic clipping of the resection sites after EMR of an LST using low-power coagulation current reduced the risk of delayed postpolypectomy hemorrhage[26]. Trauma or physical irritation of the resection site during clipping is thought to be a causative factor.
In our patient, submucosal glycerol injection and electrocoagulation seemed to cause a greater degree of appendicitis than in previously reported cases. As the location of the LST was adjacent to the appendiceal orifice, it led to obstruction of the appendiceal lumen. Theoretically, submucosal injection may reduce the risk of PPCS[27], and we also made a deliberate attempt to approach the injection site in a tangential fashion to avoid administering the injection outside the bowel wall. PPCS develops when the electrical current applied during colonoscopic polypectomy extends past the mucosa into the muscularis propria and serosa, resulting in a transmural burn, without perforation[20-25]. In previous reports, the median durations of therapeutic fasting, hospitalization, and antibiotic use were 3, 5.5, and 7 days, respectively[27], whereas our patient had a shorter course.
Two cases of acute appendicitis after EMR have been reported[6]. Similar to the present case, these cases involved EMR of a cecal adenoma adjacent to the appendiceal orifice. One patient (without clipping) had a severe inflammatory reaction after EMR, and the other patient (with clipping) had a mild inflammatory reaction. Considering those cases along with ours, clipping does not appear to influence appendicitis. However, it might be useful to avoid clipping of the appendiceal orifice to prevent appendicitis when lesions scheduled for EMR are in close proximity to the appendix. Additionally, the clinical courses of the two previously reported cases of post-EMR appendicitis were similar to those observed in PPCS, so the adenoma location is a likely risk factor for appendicitis after EMR. Furthermore, submucosal injection may obstruct the appendiceal orifice and PPCS may lead to appendiceal edema. Prophylactic antibiotic administration prior to the treatment of an appendiceal LST may be effective in preventing appendicitis, and prompt diagnosis of appendicitis following EMR can facilitate medical treatment, without the need for surgical intervention.
Here, we reported a case of acute appendicitis following EMR of a cecal LST, which was successfully treated with antibiotics. Cecal EMR may thus be a rare cause of acute appendicitis.
A 53-year-old female presented with right-lower abdominal pain 7 h after endoscopic mucosal resection of a cecal adenoma.
Acute appendicitis.
Post-polypectomy coagulation syndrome, thermal injury, bleeding, perforation, peritonitis.
The patient had elevated hematological values, including a neutrophil count of 14144/mm3 and a C-reactive protein level of 2.20 mg/dL.
Competed tomography showed appendiceal wall thickening and swelling.
Pathological analysis showed a high-grade cecal tubular adenoma.
Antibiotics were initiated leading to total resolution of the symptoms.
Two cases of acute appendicitis following endoscopic mucosal resection (EMR) have been reported.
Acute appendicitis is the most common abdominal emergency and is also a rare complication of diagnostic colonoscopy and therapeutic endoscopy.
This case report presents the clinical characteristics of acute appendicitis following EMR. Prompt diagnosis of appendicitis following EMR can facilitate medical treatment, without the need for surgical intervention.
The authors have described acute appendicitis following EMR. The article highlights the clinical characteristics of acute appendicitis following EMR and suggests that EMR of the cecum may be a rare cause of acute appendicitis.
P- Reviewer: Leung FW S- Editor: Ma YJ L- Editor: A E- Editor: Liu XM
| 1. | Shogilev DJ, Duus N, Odom SR, Shapiro NI. Diagnosing appendicitis: evidence-based review of the diagnostic approach in 2014. West J Emerg Med. 2014;15:859-871. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 117] [Cited by in RCA: 139] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 2. | Humes DJ, Simpson J. Acute appendicitis. BMJ. 2006;333:530-534. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 290] [Cited by in RCA: 286] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 3. | Houghton A, Aston N. Appendicitis complicating colonoscopy. Gastrointest Endosc. 1988;34:489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Izzedine H, Thauvin H, Maisel A, Bourry E, Deschamps A. Post-colonoscopy appendicitis: case report and review of the literature. Am J Gastroenterol. 2005;100:2815-2817. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Shaw D, Gallardo G, Basson MD. Post-colonoscopy appendicitis: A case report and systematic review. World J Gastrointest Surg. 2013;5:259-263. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 21] [Cited by in RCA: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 6. | Horimatsu T, Fu KI, Sano Y, Yano T, Saito Y, Matsuda T, Fujimori T, Yoshida S. Acute appendicitis as a rare complication after endoscopic mucosal resection. Dig Dis Sci. 2007;52:1741-1744. [PubMed] |
| 7. | Wong GYM, Stranz CV. Acute Appendicitis Following Colonoscopy. CRSLS. 2014;121. [DOI] [Full Text] |
| 8. | Roberts KE, Starker LF, Duffy AJ, Bell RL, Bokhari J. Stump appendicitis: a surgeon’s dilemma. JSLS. 2011;15:373-378. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 49] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 9. | Pickhardt PJ, Lawrence EM, Pooler BD, Bruce RJ. Diagnostic performance of multidetector computed tomography for suspected acute appendicitis. Ann Intern Med. 2011;154:789-796, W-291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 126] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 10. | Puli SR, Kakugawa Y, Gotoda T, Antillon D, Saito Y, Antillon MR. Meta-analysis and systematic review of colorectal endoscopic mucosal resection. World J Gastroenterol. 2009;15:4273-4277. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 71] [Cited by in RCA: 70] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 11. | Edmundowicz SA. To clip or not to clip: is that the question? Gastrointest Endosc. 2013;77:408-409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Saito Y, Uraoka T, Yamaguchi Y, Hotta K, Sakamoto N, Ikematsu H, Fukuzawa M, Kobayashi N, Nasu J, Michida T. A prospective, multicenter study of 1111 colorectal endoscopic submucosal dissections (with video). Gastrointest Endosc. 2010;72:1217-1225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 591] [Cited by in RCA: 591] [Article Influence: 39.4] [Reference Citation Analysis (0)] |
| 13. | Yeh RW, Triadafilopoulos G. Submucosal injection: safety cushion at what cost? Gastrointest Endosc. 2005;62:943-945. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 14. | Fujishiro M, Yahagi N, Kashimura K, Matsuura T, Nakamura M, Kakushima N, Kodashima S, Ono S, Kobayashi K, Hashimoto T. Tissue damage of different submucosal injection solutions for EMR. Gastrointest Endosc. 2005;62:933-942. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 131] [Article Influence: 6.6] [Reference Citation Analysis (1)] |
| 15. | Binmoeller KF. Underwater endoscopic mucosal resection. J Interv Gastroenterol. 2014;4:113-116. [RCA] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 16. | Heldwein W, Dollhopf M, Rösch T, Meining A, Schmidtsdorff G, Hasford J, Hermanek P, Burlefinger R, Birkner B, Schmitt W. The Munich Polypectomy Study (MUPS): prospective analysis of complications and risk factors in 4000 colonic snare polypectomies. Endoscopy. 2005;37:1116-1122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 213] [Cited by in RCA: 213] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 17. | Arora G, Mannalithara A, Singh G, Gerson LB, Triadafilopoulos G. Risk of perforation from a colonoscopy in adults: a large population-based study. Gastrointest Endosc. 2009;69:654-664. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 173] [Cited by in RCA: 189] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 18. | Watabe H, Yamaji Y, Okamoto M, Kondo S, Ohta M, Ikenoue T, Kato J, Togo G, Matsumura M, Yoshida H. Risk assessment for delayed hemorrhagic complication of colonic polypectomy: polyp-related factors and patient-related factors. Gastrointest Endosc. 2006;64:73-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 179] [Cited by in RCA: 187] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 19. | Tolliver KA, Rex DK. Colonoscopic polypectomy. Gastroenterol Clin North Am. 2008;37:229-251, ix. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 54] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 20. | Waye JD. Management of complications of colonoscopic polypectomy. Gastroenterologist. 1993;1:158-164. [PubMed] |
| 21. | Waye JD, Lewis BS, Yessayan S. Colonoscopy: a prospective report of complications. J Clin Gastroenterol. 1992;15:347-351. [PubMed] |
| 22. | Waye JD, Kahn O, Auerbach ME. Complications of colonoscopy and flexible sigmoidoscopy. Gastrointest Endosc Clin N Am. 1996;6:343-377. [PubMed] |
| 23. | Christie JP, Marrazzo J. “Mini-perforation” of the colon--not all postpolypectomy perforations require laparotomy. Dis Colon Rectum. 1991;34:132-135. [PubMed] |
| 24. | Nivatvongs S. Complications in colonoscopic polypectomy: lessons to learn from an experience with 1576 polyps. Am Surg. 1988;54:61-63. [PubMed] |
| 25. | Nelson DB, McQuaid KR, Bond JH, Lieberman DA, Weiss DG, Johnston TK. Procedural success and complications of large-scale screening colonoscopy. Gastrointest Endosc. 2002;55:307-314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 284] [Cited by in RCA: 279] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 26. | Liaquat H, Rohn E, Rex DK. Prophylactic clip closure reduced the risk of delayed postpolypectomy hemorrhage: experience in 277 clipped large sessile or flat colorectal lesions and 247 control lesions. Gastrointest Endosc. 2013;77:401-407. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 194] [Cited by in RCA: 205] [Article Influence: 17.1] [Reference Citation Analysis (0)] |
| 27. | Cha JM, Lim KS, Lee SH, Joo YE, Hong SP, Kim TI, Kim HG, Park DI, Kim SE, Yang DH. Clinical outcomes and risk factors of post-polypectomy coagulation syndrome: a multicenter, retrospective, case-control study. Endoscopy. 2013;45:202-207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 98] [Article Influence: 8.2] [Reference Citation Analysis (0)] |