Published online Jul 7, 2015. doi: 10.3748/wjg.v21.i25.7884
Peer-review started: December 9, 2014
First decision: January 22, 2015
Revised: February 2, 2015
Accepted: April 17, 2015
Article in press: April 17, 2015
Published online: July 7, 2015
Processing time: 211 Days and 19 Hours
AIM: To investigate the performance of magnifying endoscopy with narrow-band imaging (ME-NBI) in the diagnosis of early gastric cancer (EGC).
METHODS: Systematic literature searches were conducted until February 2014 in PubMed, EMBASE, Web of Science, Ovid, Scopus and the Cochrane Library databases by two independent reviewers. Meta-analysis was performed to calculate the pooled sensitivity, specificity and diagnostic odds ratio and to construct a summary receiver operating characteristic (ROC) curve. Subgroup analyses were performed based on the morphology type of lesions, diagnostic standard, the size of lesions, type of assessment, country and sample size to explore possible sources of heterogeneity. A Deeks’ asymmetry test was used to evaluate the publication bias.
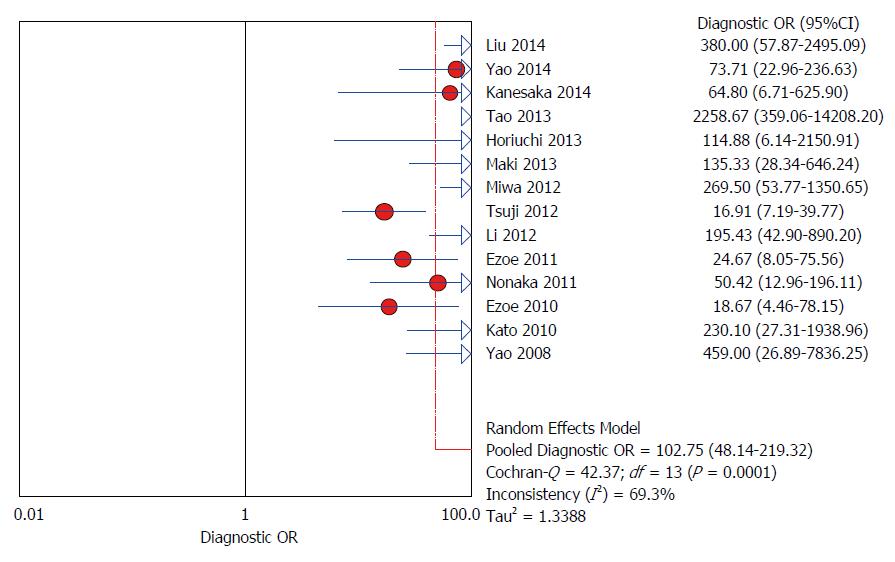
RESULTS: Fourteen studies enrolling 2171 patients were included. The pooled sensitivity, specificity and diagnostic odds ratio for ME-NBI diagnosis of EGC were 0.86 (95%CI: 0.83-0.89), 0.96 (95%CI: 0.95-0.97) and 102.75 (95%CI: 48.14-219.32), respectively, with the area under ROC curve being 0.9623. Among the 14 studies, six also evaluated the diagnostic value of conventional white-light imaging, with a sensitivity of 0.57 (95%CI: 0.50-0.64) and a specificity of 0.79 (95%CI: 0.76-0.81). When using “VS” (vessel plus surface) ME-NBI diagnostic systems in gastric lesions of depressed macroscopic type, the pooled sensitivity and specificity were 0.64 (95%CI: 0.52-0.75) and 0.96 (95%CI: 0.95-0.98). For the lesions with a diameter less than 10 mm, the sensitivity and specificity were 0.74 (95%CI: 0.65-0.82) and 0.98 (95%CI: 0.97-0.98).
CONCLUSION: ME-NBI is a promising endoscopic tool in the diagnosis of early gastric cancer and might be helpful in further target biopsy.
Core tip: This is the first meta-analysis to systematically evaluate the diagnostic performance of magnifying endoscopy with narrow-band imaging (ME-NBI) for early gastric cancer (EGC) and the pooled results showed that ME-NBI was an effective endoscopic tool in EGC diagnosis, which has a better performance than conventional white-light imaging. Moreover, the morphology type of lesions, diagnostic standard and the size of lesions might influence the diagnostic value of ME-NBI.
- Citation: Hu YY, Lian QW, Lin ZH, Zhong J, Xue M, Wang LJ. Diagnostic performance of magnifying narrow-band imaging for early gastric cancer: A meta-analysis. World J Gastroenterol 2015; 21(25): 7884-7894
- URL: https://www.wjgnet.com/1007-9327/full/v21/i25/7884.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i25.7884
Gastric cancer remains the second leading cause of cancer-associated death worldwide[1]. Early detection and therapy for gastric cancer can improve 5 year survival rates to 96%, compared to the high mortality of advanced gastric cancer[2]. Therefore, it is a top priority to make a diagnosis at an early stage in the management of gastric cancer.
Conventional white-light imaging (C-WLI) has been applied as the standard endoscopic examination for the identification of suspicious lesions but it is difficult to make an accurate diagnosis of early neoplastic lesions in most cases[3]. Several studies have indicated that the sensitivity of C-WLI for diagnosing early gastric cancer varied from 33% to 75% and specificity from 57.0% to 93.8%[3-8]. The ultimate goal of endoscopists is to make a reliable diagnosis under microscopic view, with a decreased number of biopsies[3]. To this end, C-WLI would not be entitled and it is urgent to find a novel endoscopic imaging technology with high diagnostic accuracy.
Magnifying endoscopy with narrow-band imaging (ME-NBI) is an advanced endoscopic imaging technology launched recently, in which spectral bandwidth filters in a red-green-blue (R/G/B) sequential illumination system are used to improve the accuracy of diagnosis[9]. It has been developed to enhance the visualization of the superficial mucosal structure and vascular architecture[10]. So far, ME-NBI has been applied in the diagnoses of various diseases, such as Barrett’s esophagus[11,12], esophageal carcinoma[13], Helicobacter pylori-associated chronic gastritis[14], intestinal metaplasia[15], colonic polyps[10] and so forth. Moreover, it has also been applied to evaluate the histological type of early gastric cancer (EGC)[16] and to measure the horizontal extent and invasion depth of the tumor before endoscopic submucosal dissection[17,18].
A randomized and controlled trial reported that ME-NBI was more accurate than C-WLI endoscopy in identifying small, depressed gastric mucosal cancers[3]. However, the accuracy of ME-NBI for the diagnosis of EGC was variable, with the sensitivity ranging from 60% to 100% and the specificity ranging from 84% to 100%[3-8,19-26]. The aim of this meta-analysis was to systematically assess the diagnostic performance of ME-NBI in EGC.
We systematically searched in PubMed, EMBASE, Web of Science, Ovid, Scopus and the Cochrane Library databases up to February 2014 to identify relevant articles. The search terms were as follows: (“narrow band” OR “narrow band imaging” OR “NBI” OR “electronic chromoendoscopy” OR “digital chromoendoscopy” OR “optical chromoendoscopy”) AND (“gastric cancer” OR “gastric carcinoma” OR “gastric neoplasm” OR “stomach cancer” OR “stomach carcinoma” OR “stomach neoplasm”). To avoid missing studies, we also read through the reference lists of relevant articles and reviews. The retrieved studies were carefully examined to exclude duplicate data. After scanning titles and abstracts of articles selected from the initial search, we reviewed the full text of potential eligible studies. This meta-analysis was designed, conducted and reported according to the PRISMA statement.
Articles were included if they met all the following inclusion criteria: (1) ME-NBI was used for the diagnosis of EGC; (2) numbers of true-positive (TP), false-positive (FP), true-negative (TN) and false-negative (FN) cases were reported or could be calculated; (3) histopathology was applied as a reference standard; and (4) published as full articles in English. Articles that met any of the following exclusion criteria were excluded: (1) combined examinations for EGC diagnosis, such as ME-NBI combined with trimodal imaging endoscopy or AFI; (2) previous known gastric cancer lesions; (3) only high-grade intraepithelial neoplasia; (4) hereditary diffuse gastric cancer or gastric remnant carcinoma; and (5) review articles, case reports, editorials, comments, letters to the editor, meeting abstracts.
Data were extracted independently by 2 reviewers and the following information was obtained from each study: the first author, year of publication, age and gender, morphology type of lesions, diagnostic standard, lesion size, type of assessment, endoscopic system and number of endoscopists. Numbers of TP, FP, TN and FN were also extracted. Discrepancies were resolved by a third investigator. The quality of the included studies was estimated using the Quality Assessment of Diagnostic Accuracy Studies (QUADAS). A total of 14 items were assessed, with each item assessed as “yes”, “no” or “unclear”.
Meta-analysis was carried out to evaluate the accuracy of ME-NBI in differentiating malignant from benign early gastric lesions. The pooled sensitivity, specificity, positive LR, negative LR and diagnostic OR (with corresponding 95%CI) were estimated by a fixed-effect model (Mantel-Haenszel method) when significant heterogeneity was absent or a random effect model (DerSimonian-Laird method) when there was significant heterogeneity. Heterogeneity among the included studies was tested by the Cochrane Q test. Inconsistency (I2) was used to express the percentage variability attributable to heterogeneity. I2 greater than 50% was considered significant for heterogeneity. A summary receiver operating characteristic (SROC) curve was constructed. The area under the curve (AUC) was an overall summary measure index of the diagnosis and a perfect test would have an AUC close to 1. To explore possible sources of heterogeneity among the studies, subgroup analyses were performed with the following covariates such as the morphology type of lesions (depressed vs not depressed), diagnostic standard (an irregular microvascular (MV) pattern or/and an irregular microsurface (MS) pattern with a demarcation line vs others), lesion size (the diameter more than 10 mm vs less than 10 mm), type of assessment (real-time vs post-procedure), country (China vs Japan) and sample size (< 100 patients vs≥ 100 patients). Spearman coefficient was assessed to assess threshold effect. A strongly positive correlation between the log of sensitivity and the log of 1-specificity indicates the presence of threshold effect.
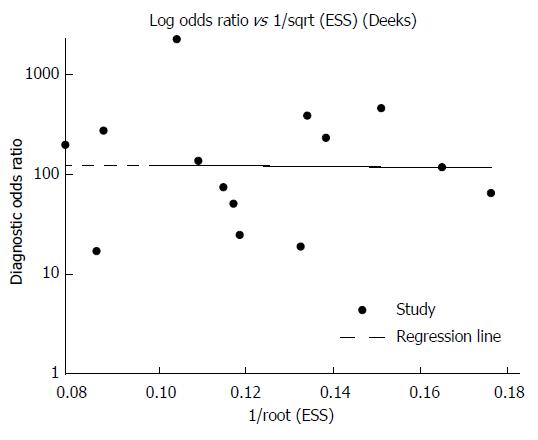
Deeks’ asymmetry was employed to evaluate the publication bias by constructing a funnel plot of diagnostic log odds ratio vs 1/sqrt (effective sample size). The pooled sensitivity, specificity, positive LR, negative LR, diagnostic OR, SROC curve, Spearman coefficient and subgroup analysis were performed using Meta-Disc version 1.4 (Ramony Cajal Hospital, Madrid, Spain). Meta-regression and publication bias were analyzed using STATA version 12.0 (Stata Corporation, College Station, Tex). P < 0.05 was considered statistically significant.
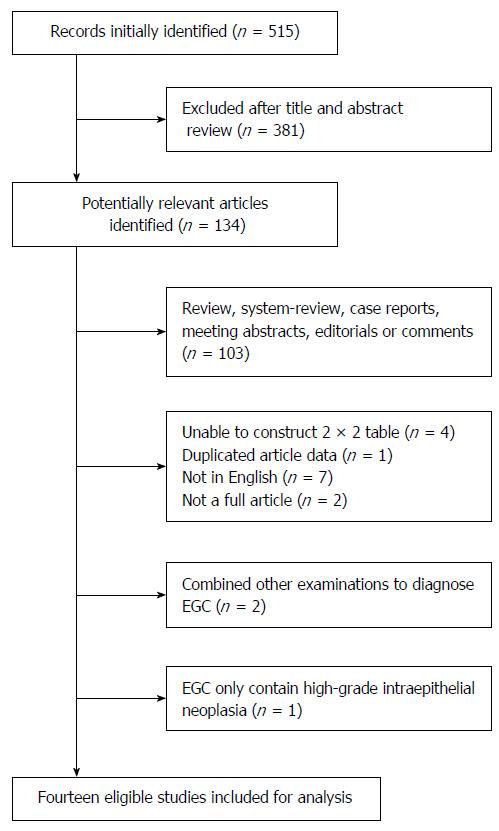
After searching PubMed, EMBASE, Web of Science, Ovid, Scopus and the Cochrane Library databases, 515 articles were identified. On the basis of titles and abstracts, 343 articles were excluded, leaving 172 studies for further selection. The selection process and reasons for exclusion are summarized in Figure 1. Fourteen studies comprising 2171 participants were eligible for final analysis.
The characteristics of the 14 studies are presented in Table 1. Among them, 6 studies[3-8] compared the diagnostic values between ME-NBI and C-WLI. Eleven studies were performed in Japan[3,5-8,20-22,24-26] and three in China[4,19,23]. Seven studies used “an irregular microvascular (MV) pattern and/or an irregular microsurface (MS) pattern with a demarcation line” as a diagnostic standard[3-7,20,24] and others used less defined criteria of fine mucosal structure, white opaque substance[26] or crypt openings[21]. Real-time assessment was conducted in eight studies[3,7,8,19,20,23,25,26] and post-procedure assessment in the remaining ones[4-6,21,22,24]. The macroscopic appearance of lesions was limited to depressed type in three studies[3,7,20], with “VS” (vessel plus surface) diagnostic systems applied, and the rest of the studies recruited non-depressed lesions[4-6,8,19,21-26]. The overall quality of the selected studies was excellent according to the QUADAS questionnaires and the details are listed in Table 2.
| Ref. | No. of patients | Sex,male/female | Age, mean | Country | Diagnostic standard | Morphology type of lesions (depressed/not depressed) | Lesion size (mm) | Type of assessment | Endoscopic system (Lucera/Exera) | Endoscopists number |
| Liu et al[19] | 90 | 49/41 | 57.5 | China | Type1 A-E | 47/160 | NA | Real-time | NA | 2 |
| Yao et al[20] | 310 | 183/127 | 66 | Japan | Irregular MV and/or irregular MS with a demarcation line | 231/134 | NA | Real-time | Lucera | 20 |
| Kanesaka et al[21] | 49 | 35/16 | NA | Japan | Presence of dense-type crypt openings | 0/51 | NA | Post-procedure | Lucera | 4 |
| Tao et al[4] | 508 | 316/192 | 63 | China | Irregular MV and/or irregular MS with a demarcation line | 192/451 | 7 | Post-procedure | NA | NA |
| Horiuchi et al[22] | 51 | 31/20 | 65 | Japan | Micrification of fine mucosal structure | 0/64 | NA | Post-procedure | Lucera | NA |
| Maki et al[5] | 93 | 73/20 | NA | Japan | Irregular MV and/or irregular MS with a demarcation line | 0/93 | NA | Post-procedure | Lucera | NA |
| Miwa et al[6] | 135 | 77/58 | 70.1 | Japan | Irregular MV and/or irregular MS with a demarcation line | 26/109 | NA | Post-procedure | Lucera | NA |
| Tsuji et al[24] | 137 | 101/36 | NA | Japan | Irregular MV and/or irregular MS with a demarcation line | 19/118 | NA | Post-procedure | Lucera | 4 |
| Li et al[23] | 146 | 88/58 | 59.3 | China | Type2 A-C | 52/112 | 21.9 | Real-time | Lucera | 2 |
| Ezoe et al[3] | 353 | 278/75 | 69 | Japan | Irregular MV with a demarcation line | 353/0 | 5.6 | Real-time | Lucera | 31 |
| Nonaka et al[25] | 93 | 71/22 | 70 | Japan | Type3 I-V | 0/93 | 15.1 | Real-time | NA | 4 |
| Ezoe et al[7] | 53 | NA | NA | Japan | Irregular MV with a demarcation line | 57/0 | ≤ 10 | Real-time | Lucera | 5 |
| Kato et al[8] | 111 | 98/13 | 66.3 | Japan | Disappearance of fine mucosal structure, microvascular dilation, heterogeneity | NA | 7.0 | Real-time | Lucera | NA |
| Yao et al[26] | 42 | NA | NA | Japan | Either WOS with a regular distribution or a regular MV | 0/46 | NA | Real-time | Lucera | 1 |
| Ref. | Item 1 | Item 2 | Item 3 | Item 4 | Item 5 | Item 6 | Item 7 | Item 8 | Item 9 | Item 10 | Item 11 | Item 12 | Item 13 | Item 14 | Scores |
| Liu et al[19] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 14 |
| Yao et al[20] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 14 |
| Kanesaka et al[21] | N | Y | Y | Y | Y | Y | Y | Y | Y | U | Y | Y | Y | Y | 12 |
| Tao et al[4] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | U | Y | Y | Y | 13 |
| Horiuchi et al[22] | Y | Y | Y | Y | Y | Y | Y | Y | Y | U | U | Y | Y | Y | 12 |
| Maki et al[5] | Y | Y | Y | Y | Y | Y | Y | Y | Y | U | U | Y | Y | Y | 12 |
| Miwa et al[6] | Y | Y | Y | Y | Y | Y | Y | Y | Y | U | U | Y | Y | Y | 12 |
| Tsuji et al[24] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 14 |
| Li et al[23] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 14 |
| Ezoe et al[3] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | U | Y | Y | N | 12 |
| Nonaka et al[25] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 14 |
| Ezoe et al[7] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | U | Y | Y | Y | 13 |
| Kato et al[8] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | Y | Y | Y | 13 |
| Yao et al[26] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | U | Y | Y | 13 |
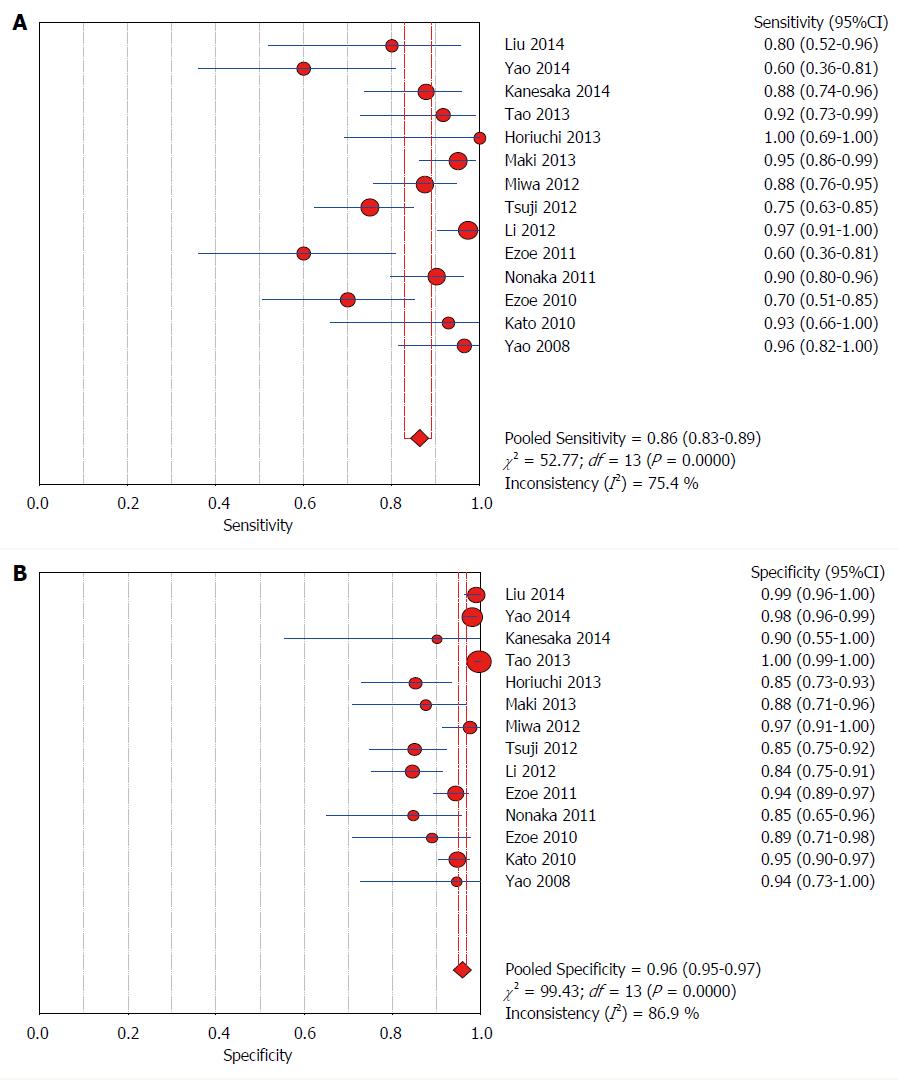
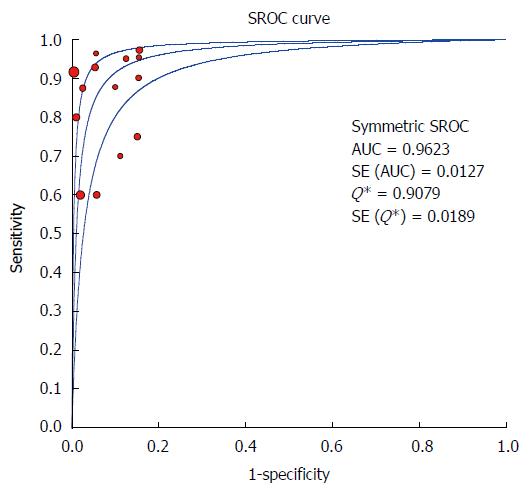
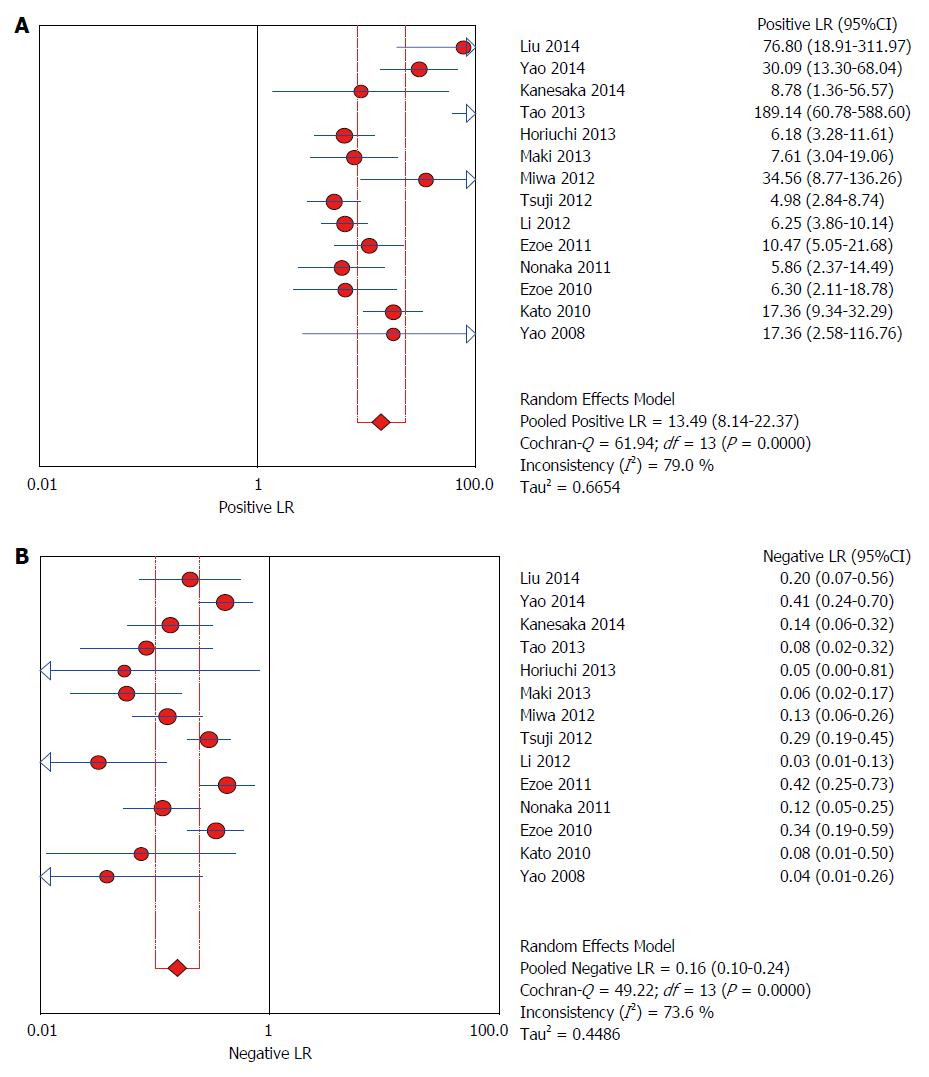
Calculated by a random effect model, the pooled sensitivity and specificity of ME-NBI for diagnosing early gastric cancer were 0.86 (95%CI: 0.83-0.89) and 0.96 (95%CI: 0.95-0.97), respectively (Figure 2). Significant heterogeneities were found in sensitivity (I2 = 75.4%) and specificity (I2 = 86.9%). The AUC was 0.9623 (E = 0.0127) (Figure 3), indicating an excellent performance of ME-NBI in the diagnosis of EGC. For C-WLI, the sensitivity, specificity and AUC for diagnosing EGC were 0.57 (95%CI: 0.50-0.64), 0.79 (95%CI: 0.76-0.81) and 0.6634, respectively, indicating a limited diagnostic performance of C-WLI compared with ME-NBI. Moreover, for the depressed-type lesions, C-WLI has a low sensitivity of 0.30 (95%CI: 0.18-0.45) and specificity of 0.68 (95%CI: 0.10-0.24). The overall positive LR, negative LR and diagnostic OR for diagnosing EGC by ME-NBI were 13.49 (95%CI: 8.14-22.37), 0.16 (95%CI: 0.10-0.24) and 102.75 (95%CI: 48.14-219.32), respectively (Figures 4 and 5). Significant heterogeneities were found in positive LR (I2 =79.0%), negative LR (I2 = 73.6%) and diagnostic OR (I2 =69.3%).
The Spearman correlation coefficient was 0.367 (P = 0.196), suggesting no evidence of significant threshold effect. Meta-regression and subgroup analyses were performed in order to explore the potential sources of heterogeneity. The results indicated that the morphology type of lesions, diagnostic standard, lesion size and sample size might be the possible sources of heterogeneity (Table 3). Studies in which “VS classification system” was regarded as diagnostic standard revealed reduced benefits over those using other diagnostic standards in terms of sensitivity (81% vs 93%, P = 0.01) but not in the specificity (97% vs 93%, P = 0.36). When the “VS” was applied in the depressed lesions, the sensitivity and specificity were 0.64 (95%CI: 0.52-0.75) and 0.96 (95%CI: 0.95-0.98), while in the non-depressed lesions, the sensitivity and specificity were as high as 0.86 (95%CI: 0.81-0.91) and 0.98 (95%CI: 0.96-0.98). The diagnostic sensitivity of ME-NBI was strikingly lower in depressed lesions than that in non-depressed ones (64% vs 90%, P < 0.001). Nevertheless, the difference of the specificity between them was not significant (96% vs 96%, P = 0.75). ME-NBI had a significantly higher sensitivity when assessing lesions with a diameter more than 10 mm than those less than 10 mm (90% vs 74%, P = 0.04), while there was an opposite result in terms of specificity (88% vs 98%, P = 0.02). For the studies with a sample size less than 100 patients, the specificity of ME-NBI for EGC was higher than that of other studies (97% vs 87%, P = 0.04), while no marked difference of sensitivity between them was observed (84% vs 90%, P = 0.22). Meta-regression and subgroup analysis based on type of assessment and country did not show remarkable significance considering the values of sensitivity and specificity (Table 3).
| Number of studies (lesions examined) | Sensitivity (95%CI) | Specificity (95%CI) | AUC | I2 | ||
| Sensitivity | Specificity | |||||
| Overall | 14 (2433) | 0.86 (0.83-0.89) | 0.96 (0.95-0.97) | 0.9623 | 75.4% | 86.9% |
| Type of lesion | ||||||
| Depressed | 3 (605) | 0.64 (0.52-0.75) | 0.96 (0.95-0.98) | 0.7877 | 0.0% | 74.1% |
| Not depressed | 10 (1828) | 0.90 (0.86-0.92) | 0.96 (0.95-0.97) | 0.9694 | 64.9% | 90.1% |
| Diagnosis standard | ||||||
| Diagnosis (IMVP/IMSP + DL) | 7 (1613) | 0.81 (0.76-0.85) | 0.97 (0.96-0.98) | 0.9407 | 78.0% | 88.8% |
| Diagnosis (others) | 7 (820) | 0.93 (0.89-0.96) | 0.93 (0.91-0.95) | 0.9719 | 36.6% | 80.5% |
| Lesion size | ||||||
| Diameter (> 10 mm) | 8 (777) | 0.90 (0.86-0.93) | 0.88 (0.85-0.91) | 0.9585 | 71.2% | 44.7% |
| Diameter ( ≤ 10 mm) | 5 (1449) | 0.74 (0.65-0.82) | 0.98 (0.97-0.98) | 0.9458 | 67.1% | 86.6% |
| Sample size | ||||||
| ≥ 100 patients | 8 (2035) | 0.84 (0.79-0.88) | 0.97 (0.96-0.97) | 0.9663 | 79.1% | 90.7% |
| < 100 patients | 6 (398) | 0.90 (0.85-0.93) | 0.87 (0.81-0.92) | 0.9422 | 67.3% | 0.0% |
| Type of assessment | ||||||
| Real-time | 8 (1310) | 0.85 (0.81-0.90) | 0.95 (0.94-0.96) | 0.9617 | 81.6% | 81.2% |
| Post-procedure | 6 (1123) | 0.87 (0.82-0.91) | 0.97 (0.95-0.98) | 0.9608 | 65.5% | 91.6% |
| Country | ||||||
| China | 3 (1014) | 0.94 (0.88-0.97) | 0.98 (0.97-0.99) | 0.9864 | 62.5% | 95.7% |
| Japan | 11 (1419) | 0.84 (0.80-0.88) | 0.94 (0.92-0.95) | 0.9526 | 74.6% | 71.2% |
Deeks’ funnel plot did not display significant asymmetry (P = 0.967), indicating that no striking publication bias was present in this study (Figure 6).
Nowadays, ME-NBI has been applied in the diagnostic workup of gastrointestinal tumors, especially in the differentiation of colonic lesions[10], while its diagnostic accuracy for EGC is unclear. In this meta-analysis, we demonstrated that ME-NBI is a highly specific diagnostic tool for EGC, with a high sensitivity (86%), specificity (96%) and diagnostic odds ratio (102.75), which were higher than those of C-WLI (57%, 79% and 3.46), indicating that ME-NBI had a better diagnostic performance for EGC.
This meta-analysis also demonstrated that the diagnostic performance of ME-NBI was influenced by the type and size of gastric lesions, especially the depressed type and in lesions less than 10 mm. Since the depressed mucosa type is the predominant morphology among gastric cancers, early detection and diagnosis of depressed type cancer are an effective way to decrease the mortality of gastric cancer[27-29]. However, we observed that ME-NBI had a relatively lower sensitivity of 64% for lesions of a depressed type than those of a non-depressed type (90%), while the specificity was similar as 96% for both of them. These results indicated that ME-NBI was more reliable in identifying non-depressed EGC lesions. Interestingly, the size of most depressed lesions was less than 10 mm in enrolled studies and thus the diagnostic performance for depressed type lesions is representative of lesions with a diameter less than 10 mm. As for the depressed type lesions with a diameter over 10 mm, we failed to find relevant studies and further research might be required in the future. In addition, our results showed that the diagnostic sensitivity was as low as 74% in gastric lesions with a diameter less than 10 mm, but the sensitivity for lesions with a diameter over 10 mm was 90%. Although the sensitivity was low in the lesions with a diameter less than 10 mm, the specificity for these lesions was as high as 98%, while for the lesions with a diameter over 10 mm, the specificity was only 88%. Accordingly, depressed lesions and lesions with a diameter less than 10 mm might limit the application of ME-NBI in the diagnosis of EGC. When identifying depressed gastric lesions with a diameter less than 10 mm, it would be better to combine ME-NBI with other examinations to improve the diagnosis of EGC.
Although ME-NBI was far from enough to identify depressed type lesions, it was a better option than C-WLI. Ezoe et al[7] reported that ME-NBI was more accurate than C-WLI in identifying small, depressed gastric mucosal cancers, with a higher sensitivity (70% vs 33%) and specificity (89% vs 67%). Kaise et al[30] discovered that in the differential diagnosis of superficial depressed gastric lesions, ME-NBI showed a superior specificity (85%) than C-WLI (65%), but the sensitivities for both of them were comparably moderate. In our meta-analysis, two studies[3,7] reported the role of C-WLI in the diagnosis of depressed type EGC, with a sensitivity of 30% and a specificity of 68%, both of which were lower than those of ME-NBI (sensitivity: 64%; specificity: 96%). Our study also demonstrated a higher diagnostic performance of ME-NBI than C-WLI in depressed EGC diagnosis.
Several diagnostic criteria have been developed to guide endoscopists in optical diagnosis EGC by ME-NBI. Yao et al[9] firstly proposed a simple classification system called the “VS (vessel plus surface) classification system”, in which an irregular microsurface pattern and/or an irregular microvascular pattern with a demarcation line are significant markers of EGC. This diagnostic reference has been used in several studies with variable diagnostic performance. This author also demonstrated that in cases of gastric neoplasia of 0-IIa type, a white opaque substance (WOS) obscured the subepithelial capillaries of the lesion and 83% of EGC showed an irregular distribution[26]. In another study, Kato et al[8] used a triad-based diagnosis of disappearance of fine mucosal structure, microvascular dilation and heterogeneity to identify superficial gastric lesions. In our study, when the “VS (vessel plus surface) classification system” was applied as the diagnostic criteria, the sensitivity was 81%, which was lower than that using other diagnostic criteria. For the lesions of depressed type, the sensitivity and specificity were 64% and 96% with the “VS classification system” diagnostic criteria and there were no other diagnostic criteria applied in these lesions in our enrolled studies. In contrast, when the diagnostic criteria of “VS” was used in non-depressed lesions, it had a higher sensitivity of 86% and the specificity was 98%. This indicates that the “VS classification system” was limited in depressed EGC. However, it has been reported that when only microvascular irregularity was used as the diagnostic standard for depressed gastric cancers, the mean sensitivity was as high as 86.7%[31]. These variable results suggest that further research is still required to evaluate the “VS classification system” in the differential diagnosis of depressed gastric lesions. There were other diagnostic standards in depressed gastric cancer but the results were not entirely optimistic. It was reported that when the triad of FMS disappearance, microvascular dilation and heterogeneity was used as the diagnostic standard for superficial depressed gastric cancer, the sensitivity was only 69.1%[30]. Thus, it is urgent to improve the sensitivity of ME-NBI, especially for depressed gastric lesions.
The variability of observers in the diagnostic performance of ME-NBI has increasingly caught our attention. Mochizuki et al[32] reported that among the experts, the interobserver κ value was 0.85, with 88.0% consensus of diagnoses in the differential diagnosis of gastric adenoma and carcinoma, while with the two inexperienced endoscopists, the interobserver κ value was 0.44, with 68.0% consensus of diagnoses, implying that the diagnostic performance of ME-NBI might be improved through specific training. Kaise et al[30] evaluated the interobserver concordance among 11 endoscopists, concerning the triad of FMS disappearance, microvascular dilation and heterogeneity, and the κ values from 0.34 to 0.54 showed low-to-modest reliability. Yoo et al[33] discovered that the κ value for interobserver agreement of experts and trainees were similar as 0.49 and 0.40 when using the “VS classification system” for the gastric mucosal surface. In view of these inconsistent results, further studies are still required to find how to improve diagnostic performance of ME-NBI in a multiple-observer setting.
This meta-analysis has several limitations. First, we could not make a clear distinction between expert and non-expert. In some studies, an endoscopist was regarded as an expert after a specific training but in others, only those who have done a specific number of ME-NBI had this honor. Second, the cost-effectiveness of ME-NBI was not reported as well as the comparison with that of histopathology. Recently, Takeuchi et al[34] proposed that “a new resect and discard strategy” with ME-NBI in colorectal cancer screening might reduce the costs of histopathology. Third, the heterogeneity of this study was relatively high. We showed that the morphology type of lesions, diagnostic standard, lesion size and sample size were the possible sources. In addition, the inequality of expertise, the absence of a validated training, different disease spectrum and pathological type might reduce the generalizability of the overall performance and increase the heterogeneity of this study. Fourth, all the selected articles were conducted in China and Japan so the overall performance of ME-NBI for early gastric cancer may not represent other populations. Finally, only articles written in English were selected.
In conclusion, ME-NBI is a reliable technique for EGC diagnosis and has a better diagnostic performance than C-WLI. Further research should be focused on establishing a standard classification system and specific training of ME-NBI to reduce various biases and improve its diagnostic accuracy.
We thank our colleagues in the School of Medicine, Zhejiang University for their assistance in writing this paper.
Early detection and therapy of gastric cancer can improve 5 year survival rates of gastric cancer and therefore the diagnosis of early gastric cancer is significant in clinical work. Magnifying endoscopy with narrow-band imaging (ME-NBI) is a recently advanced endoscopic imaging technology which can enhance visualization of the superficial mucosal structure and vascular architecture. However, the diagnostic performance of ME-NBI in early gastric cancer (EGC) remains unclear.
Although ME-NBI has been applied in EGC diagnosis, the accuracy of ME-NBI for the diagnosis of EGC was variable. Therefore, the authors performed a meta-analysis to analyze the diagnostic performance of ME-NBI in EGC.
In this study, the authors found that ME-NBI was a promising technique for EGC diagnosis, with a better diagnostic performance than conventional white-light imaging (C-WLI). To the best of our knowledge, this is the first meta-analysis to systematically calculate the diagnostic performance of ME-NBI in EGC diagnosis, which will provide valuable information for clinical work.
ME-NBI may be a clinically useful tool to diagnose EGC and it can improve the diagnostic performance of EGC, compared with C-WLI.
Generally speaking, EGC is defined as gastric cancer which invades, limited to the mucosa or submucosa layer, regardless of lymphatic metastasis.
The article is a complete, systematic literature review investigating the utility of ME-NBI in the diagnosis of EGC. The results indicate that ME-NBI is a reliable technique for EGC diagnosis and has a better diagnostic performance than C-WLI in EGC diagnosis, which could be used for effective clinical work.
P- Reviewer: Imaeda H, Testini M, Wang YH, Zhang JZ S- Editor: Ma YJ L- Editor: Roemmele A E- Editor: Ma S
| 1. | Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127:2893-2917. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11128] [Cited by in RCA: 11837] [Article Influence: 845.5] [Reference Citation Analysis (4)] |
| 2. | Soetikno R, Kaltenbach T, Yeh R, Gotoda T. Endoscopic mucosal resection for early cancers of the upper gastrointestinal tract. J Clin Oncol. 2005;23:4490-4498. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 408] [Cited by in RCA: 395] [Article Influence: 19.8] [Reference Citation Analysis (0)] |
| 3. | Ezoe Y, Muto M, Uedo N, Doyama H, Yao K, Oda I, Kaneko K, Kawahara Y, Yokoi C, Sugiura Y. Magnifying narrowband imaging is more accurate than conventional white-light imaging in diagnosis of gastric mucosal cancer. Gastroenterology. 2011;141:2017-2025.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 254] [Cited by in RCA: 283] [Article Influence: 20.2] [Reference Citation Analysis (0)] |
| 4. | Tao G, Xing-Hua L, Ai-Ming Y, Wei-Xun Z, Fang Y, Xi W, Li-Yin W, Chong-Mei L, Gui-Jun F, Hui-Jun S. Enhanced magnifying endoscopy for differential diagnosis of superficial gastric lesions identified with white-light endoscopy. Gastric Cancer. 2014;17:122-129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 36] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 5. | Maki S, Yao K, Nagahama T, Beppu T, Hisabe T, Takaki Y, Hirai F, Matsui T, Tanabe H, Iwashita A. Magnifying endoscopy with narrow-band imaging is useful in the differential diagnosis between low-grade adenoma and early cancer of superficial elevated gastric lesions. Gastric Cancer. 2013;16:140-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 60] [Article Influence: 5.0] [Reference Citation Analysis (1)] |
| 6. | Miwa K, Doyama H, Ito R, Nakanishi H, Hirano K, Inagaki S, Tominaga K, Yoshida N, Takemura K, Yamada S. Can magnifying endoscopy with narrow band imaging be useful for low grade adenomas in preoperative biopsy specimens? Gastric Cancer. 2012;15:170-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 40] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 7. | Ezoe Y, Muto M, Horimatsu T, Minashi K, Yano T, Sano Y, Chiba T, Ohtsu A. Magnifying narrow-band imaging versus magnifying white-light imaging for the differential diagnosis of gastric small depressive lesions: a prospective study. Gastrointest Endosc. 2010;71:477-484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 81] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 8. | Kato M, Kaise M, Yonezawa J, Toyoizumi H, Yoshimura N, Yoshida Y, Kawamura M, Tajiri H. Magnifying endoscopy with narrow-band imaging achieves superior accuracy in the differential diagnosis of superficial gastric lesions identified with white-light endoscopy: a prospective study. Gastrointest Endosc. 2010;72:523-529. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 125] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 9. | Yao K, Anagnostopoulos GK, Ragunath K. Magnifying endoscopy for diagnosing and delineating early gastric cancer. Endoscopy. 2009;41:462-467. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 348] [Cited by in RCA: 337] [Article Influence: 21.1] [Reference Citation Analysis (0)] |
| 10. | Wanders LK, East JE, Uitentuis SE, Leeflang MM, Dekker E. Diagnostic performance of narrowed spectrum endoscopy, autofluorescence imaging, and confocal laser endomicroscopy for optical diagnosis of colonic polyps: a meta-analysis. Lancet Oncol. 2013;14:1337-1347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 85] [Reference Citation Analysis (0)] |
| 11. | Hamamoto Y, Endo T, Nosho K, Arimura Y, Sato M, Imai K. Usefulness of narrow-band imaging endoscopy for diagnosis of Barrett’s esophagus. J Gastroenterol. 2004;39:14-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 130] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 12. | Anagnostopoulos GK, Yao K, Kaye P, Hawkey CJ, Ragunath K. Novel endoscopic observation in Barrett’s oesophagus using high resolution magnification endoscopy and narrow band imaging. Aliment Pharmacol Ther. 2007;26:501-507. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 85] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 13. | Muto M, Horimatsu T, Ezoe Y, Morita S, Miyamoto S. Improving visualization techniques by narrow band imaging and magnification endoscopy. J Gastroenterol Hepatol. 2009;24:1333-1346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 46] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 14. | Tahara T, Shibata T, Nakamura M, Yoshioka D, Okubo M, Arisawa T, Hirata I. Gastric mucosal pattern by using magnifying narrow-band imaging endoscopy clearly distinguishes histological and serological severity of chronic gastritis. Gastrointest Endosc. 2009;70:246-253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 103] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 15. | Uedo N, Ishihara R, Iishi H, Yamamoto S, Yamamoto S, Yamada T, Imanaka K, Takeuchi Y, Higashino K, Ishiguro S. A new method of diagnosing gastric intestinal metaplasia: narrow-band imaging with magnifying endoscopy. Endoscopy. 2006;38:819-824. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 240] [Cited by in RCA: 267] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 16. | Nakayoshi T, Tajiri H, Matsuda K, Kaise M, Ikegami M, Sasaki H. Magnifying endoscopy combined with narrow band imaging system for early gastric cancer: correlation of vascular pattern with histopathology (including video). Endoscopy. 2004;36:1080-1084. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 328] [Cited by in RCA: 335] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 17. | Yao K, Nagahama T, Matsui T, Iwashita A. Detection and characterization of early gastric cancer for curative endoscopic submucosal dissection. Dig Endosc. 2013;25 Suppl 1:44-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 49] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 18. | Jang JY. The Usefulness of Magnifying Endoscopy and Narrow-Band Imaging in Measuring the Depth of Invasion before Endoscopic Submucosal Dissection. Clin Endosc. 2012;45:379-385. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 19. | Liu H, Wu J, Lin XC, Wei N, Lin W, Chang H, Du XM. Evaluating the diagnoses of gastric antral lesions using magnifying endoscopy with narrow-band imaging in a Chinese population. Dig Dis Sci. 2014;59:1513-1519. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 20. | Yao K, Doyama H, Gotoda T, Ishikawa H, Nagahama T, Yokoi C, Oda I, Machida H, Uchita K, Tabuchi M. Diagnostic performance and limitations of magnifying narrow-band imaging in screening endoscopy of early gastric cancer: a prospective multicenter feasibility study. Gastric Cancer. 2014;17:669-679. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 108] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 21. | Kanesaka T, Sekikawa A, Tsumura T, Maruo T, Osaki Y, Wakasa T, Shintaku M, Yao K. Dense-type crypt opening seen on magnifying endoscopy with narrow-band imaging is a feature of gastric adenoma. Dig Endosc. 2014;26:57-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 22. | Horiuchi H, Kaise M, Inomata H, Yoshida Y, Kato M, Toyoizumi H, Goda K, Arakawa H, Ikegami M, Kushima R. Magnifying endoscopy combined with narrow band imaging may help to predict neoplasia coexisting with gastric hyperplastic polyps. Scand J Gastroenterol. 2013;48:626-632. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 11] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 23. | Li HY, Dai J, Xue HB, Zhao YJ, Chen XY, Gao YJ, Song Y, Ge ZZ, Li XB. Application of magnifying endoscopy with narrow-band imaging in diagnosing gastric lesions: a prospective study. Gastrointest Endosc. 2012;76:1124-1132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 52] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 24. | Tsuji Y, Ohata K, Sekiguchi M, Ohno A, Ito T, Chiba H, Gunji T, Fukushima J, Yamamichi N, Fujishiro M. Magnifying endoscopy with narrow-band imaging helps determine the management of gastric adenomas. Gastric Cancer. 2012;15:414-418. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 33] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 25. | Nonaka K, Arai S, Ban S, Kitada H, Namoto M, Nagata K, Ochiai Y, Togawa O, Nakao M, Nishimura M. Prospective study of the evaluation of the usefulness of tumor typing by narrow band imaging for the differential diagnosis of gastric adenoma and well-differentiated adenocarcinoma. Dig Endosc. 2011;23:146-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 25] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 26. | Yao K, Iwashita A, Tanabe H, Nishimata N, Nagahama T, Maki S, Takaki Y, Hirai F, Hisabe T, Nishimura T. White opaque substance within superficial elevated gastric neoplasia as visualized by magnification endoscopy with narrow-band imaging: a new optical sign for differentiating between adenoma and carcinoma. Gastrointest Endosc. 2008;68:574-580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 126] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 27. | Gotoda T, Yanagisawa A, Sasako M, Ono H, Nakanishi Y, Shimoda T, Kato Y. Incidence of lymph node metastasis from early gastric cancer: estimation with a large number of cases at two large centers. Gastric Cancer. 2000;3:219-225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1308] [Cited by in RCA: 1328] [Article Influence: 53.1] [Reference Citation Analysis (0)] |
| 28. | Everett SM, Axon AT. Early gastric cancer in Europe. Gut. 1997;41:142-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 215] [Cited by in RCA: 200] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 29. | Hirasawa T, Gotoda T, Miyata S, Kato Y, Shimoda T, Taniguchi H, Fujisaki J, Sano T, Yamaguchi T. Incidence of lymph node metastasis and the feasibility of endoscopic resection for undifferentiated-type early gastric cancer. Gastric Cancer. 2009;12:148-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 344] [Cited by in RCA: 368] [Article Influence: 24.5] [Reference Citation Analysis (0)] |
| 30. | Kaise M, Kato M, Urashima M, Arai Y, Kaneyama H, Kanzazawa Y, Yonezawa J, Yoshida Y, Yoshimura N, Yamasaki T. Magnifying endoscopy combined with narrow-band imaging for differential diagnosis of superficial depressed gastric lesions. Endoscopy. 2009;41:310-315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 111] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 31. | Sumie H, Sumie S, Nakahara K, Watanabe Y, Matsuo K, Mukasa M, Sakai T, Yoshida H, Tsuruta O, Sata M. Usefulness of magnifying endoscopy with narrow-band imaging for diagnosis of depressed gastric lesions. Mol Clin Oncol. 2014;2:129-133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 32. | Mochizuki Y, Saito Y, Kobori A, Ban H, Ishida M, Fujiyama Y, Andoh A. Magnifying endoscopy with narrow-band imaging in the differential diagnosis of gastric adenoma and carcinoma and identification of a simple indicator. J Gastrointestin Liver Dis. 2012;21:383-390. [PubMed] |
| 33. | Yoo CH, Park MI, Park SJ, Moon W, Kim HH, Song JY, Kim do H. Observer variability in gastric neoplasm assessment using the vessel plus surface classification for magnifying endoscopy with narrow band imaging. Clin Endosc. 2014;47:74-78. [PubMed] |
| 34. | Takeuchi Y, Hanafusa M, Kanzaki H, Ohta T, Hanaoka N. Proposal of a new ‘resect and discard’ strategy using magnifying narrow band imaging: pilot study of diagnostic accuracy. Dig Endosc. 2014;26 Suppl 2:90-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 1.5] [Reference Citation Analysis (0)] |