Published online Jun 7, 2015. doi: 10.3748/wjg.v21.i21.6526
Peer-review started: October 15, 2014
First decision: January 8, 2015
Revised: February 7, 2015
Accepted: March 31, 2015
Article in press: March 31, 2015
Published online: June 7, 2015
Processing time: 239 Days and 14 Hours
AIM: To establish a cellular model correctly mimicking the gastric epithelium to overcome the limitation in the study of Helicobacter pylori (H. pylori) infection.
METHODS: Aiming to overcome this limitation, clones of the heterogenic cancer-derived NCI-N87 cell line were isolated, by stably-transducing it with the human telomerase reverse-transcriptase (hTERT) catalytic subunit gene. The clones were first characterized regarding their cell growth pattern and phenotype. For that we measured the clones’ adherence properties, expression of cell-cell junctions’ markers (ZO-1 and E-cadherin) and ability to generate a sustained transepithelial electrical resistance. The gastric properties of the clones, concerning expression of mucins, zymogens and glycan contents, were then evaluated by haematoxylin and eosin staining, Periodic acid Schiff (PAS) and PAS/Alcian Blue-staining, immunocytochemistry and Western blot. In addition, we assessed the usefulness of the hTERT-expressing gastric cell line for H. pylori research, by performing co-culture assays and measuring the IL-8 secretion, by ELISA, upon infection with two H. pylori strains differing in virulence.
RESULTS: Compared with the parental cell line, the most promising NCI-hTERT-derived clones (CL5 and CL6) were composed of cells with homogenous phenotype, presented higher relative telomerase activities, better adhesion properties, ability to be maintained in culture for longer periods after confluency, and were more efficient in PAS-reactive mucins secretion. Both clones were shown to produce high amounts of MUC1, MUC2 and MUC13. NCI-hTERT-CL5 mucins were shown to be decorated with blood group H type 2 (BG-H), Lewis-x (Lex), Ley and Lea and, in a less extent, with BG-A antigens, but the former two antigens were not detected in the NCI-hTERT-CL6. None of the clones exhibited detectable levels of MUC6 nor sialylated Lex and Lea glycans. Entailing good gastric properties, both NCI-hTERT-clones were found to produce pepsinogen-5 and human gastric lipase. The progenitor-like phenotype of NCI-hTERT-CL6 cells was highlighted by large nuclei and by the apical vesicular-like distribution of mucin 5AC and Pg5, supporting the accumulation of mucus-secreting and zymogens-chief mature cells functions.
CONCLUSION: These traits, in addition to resistance to microaerobic conditions and good responsiveness to H. pylori co-culture, in a strain virulence-dependent manner, make the NCI-hTERT-CL6 a promising model for future in vitro studies.
Core tip: In this study, we aimed to establish and characterize novel human gastric epithelial cell lines derived from NCI-N87 cells after over-expression of human telomerase catalytic activity. The two most promising NCI-N87-derived clones were shown to be composed of cells with homogenous phenotype, to produce gastric zymogens and to produce and secrete neutral mucins. In addition, these clones showed very good in vitro growth properties, resistance to microaerobic conditions and good responsiveness to Helicobacter pylori. Due to their improved properties, compared to the heterogeneous parental line, these NCI-N87-derived clones are promising models of the human gastric epithelium.
- Citation: Saraiva-Pava K, Navabi N, Skoog EC, Lindén SK, Oleastro M, Roxo-Rosa M. New NCI-N87-derived human gastric epithelial line after human telomerase catalytic subunit over-expression. World J Gastroenterol 2015; 21(21): 6526-6542
- URL: https://www.wjgnet.com/1007-9327/full/v21/i21/6526.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i21.6526
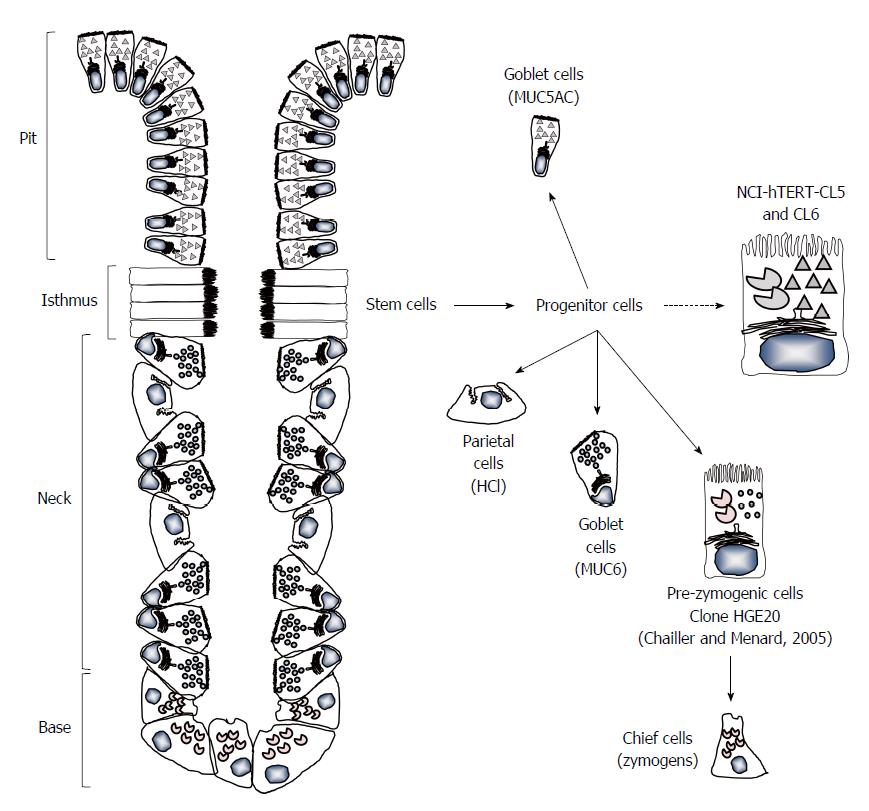
The normal physiological functions of the human stomach rely on the distinct populations of specialized epithelial cells present at the gastric mucosa. Early in foetal life, this simple columnar epithelium forms invaginations into the inner layers of the mucosa, which originate the gastric pit glands. In the continuous renewing of this tissue, its organization is maintained through a bidirectional migration of the gastric stem and progenitor cells, primarily located at the isthmus of the glands (reviewed in). In oxyntic glands (glands from fundus and corpus), the stem cells migrating upward into the pit and surface give rise to mucin (MUC) 5AC (MUC5AC)-secreting cells, while those that migrate down differentiate into MUC6-secreting and parietal (HCl-secreting) cells at the neck, and mature chief (zymogens-secreting) cells at the base of the gland. In pyloric glands (glands from the antrum), instead of parietal and chief cells, the downward migrating stem cells give rise to cells specialized in the production of gastrin (G cells) and of somatostatin (D cells). These hormones ensure the endocrine regulation of the acid production by oxyntic parietal cells[1-4].
Despite our knowledge on the importance of this organization, the research on the identification of specific regulators of the development and maintenance of human gastric functions, and their underlying mechanisms, requires the establishment of human gastric cell lines closely resembling the natural features of the gastric epithelium. Such in vitro model is also urgently needed for the study of the still poorly understood molecular mechanisms involved in the pathogenesis of severe gastric diseases associated with the Gram-negative bacterium Helicobacter pylori (H. pylori). Having the human gastric mucosa as ecological niche, this spiral-shaped, microaerophilic bacterium survives the extreme conditions of the human stomach and, constantly evading (or interacting with) the human immune system, persists throughout the patient life. Indeed, almost invariably, this pathogen/host interaction starts in patient’s childhood, always eliciting an acute host immune response, which is however inefficient for bacteria clearance[5,6]. Although often asymptomatic, most patients experience dyspeptic symptoms (non-ulcer dyspepsia) because of the resulting chronic gastritis[7] and, later in the adulthood, 15%-20% of them end up developing peptic ulcer disease and 2%-5% gastric cancer[8,9]. Despite all the spent efforts, there is still a lack of knowledge on the events that occur in the time lag that goes from the colonization in the childhood to peptic ulceration and/or gastric carcinogenesis, late in the patients’ adult life. We have shown that these events are dependent on the virulence of the strain itself[10-13], but also on its interaction with the human host, changing the expression pattern of mucins of the patient’s gastric mucosa[14-17]. Indeed, sustained infection is known to depend on the bacteria adhesion to host mucins of the epithelial cells’ surface and mucus layer lining the gastric epithelium[5,6]. Many experiments addressing these issues have been conducted on primary cultures of cells freshly isolated from human gastric biopsy samples[1,4,18]. Albeit being more representative of the human gastric epithelium, such primary cultures present important limitations regarding the availability of human donors, restricting the number of experiments that can be performed. Furthermore, primary cultures can only be cultured for a few days before they become apoptotic, limiting the type of experiments that can be performed. Similarly, for many studies gastric primary cultures of rodents are not a suitable option due to important distinctive features of their physiology compared to the human’s[19]. In fact, only human chief cells produce/secrete not only pepsinogen, but simultaneously an acid-tolerant gastric lipase, ensuring gastric digestion of triglycerides, a prerequisite for optimal intestinal lipolysis. Again, these are not a suitable option for long-term studies because, beyond the limitations of their availability, these cells also proliferate for only a small number of doublings before entering into senescence[1,4]. An extensively used alternative are cancer cell lines derived from poorly differentiated [e.g., KATO-III [American type culture collection (ATCC) HBT-103] and Hs746t (ATCC HBT-135) cells], or moderately [e.g., AGS (ATCC CRL-1739) cells] and well differentiated [e.g., NCI-N87 (ATCC CRL-5822) and MKN-7 (Riken Cell Bank, Japan) cells] human gastric carcinomas[1,20,21]. Lacking important epithelial and/or glandular properties, these in vitro cellular models are limited in resembling the native tissue. For instance, AGS cells harbour a mutated E-cadherin encoding gene that results in a non-functional truncated form of this protein, thus these cells form monolayers that do not polarize and eventually lose their integrity after reaching confluency[1,21-23]. Furthermore, despite reaching a good polarization status upon transfection with E-cadherin cDNA, they do not secrete mucus, acid or zymogens[22,24]. The MKN7 cell line, polarize and present the mucin MUC1 apically, however, again the problem is that it does not produce an adherent mucus layer[21,25]. As far as we can ascertain, the properties of this cell line regarding the acid/zymogens production/secretion have never been described.
The NCI-N87 cell line is known by its distinctive features, including colony-forming growth pattern, maintenance at post-confluency, expression of increased levels of gastric zymogens [namely, human gastric lipase (HGL) and fundic-type pepsinogen-5 (Pg5)], as well as expression of MUC6, zonula adherens marker E-cadherin and zonula occludens marker ZO-1[1]. Compared to the widely use AGS cells (ATCC, CRL-1739), the NCI-N87 cell line responds to H. pylori infection in a closer manner to that of primary gastric epithelial cell preparations[26]. However, the expression of these epithelial/gastric markers are confined only to some cell sub-populations[23]. Indeed, this is a heterogenic cell line composed of several phenotypic variants, also including non-epithelial cells. Homotypic epithelial phenotype was, interestingly, achieved by isolating non-transfected clones (using the limit-dilution approach) of those cell sub-populations, allowing the establishment of two NCI-N87-derived clones: the HGE-17 (human gastric epithelial-17 cell line), exhibiting features reminiscent of the granule-free stem cell type found in the isthmus of the glands; and the HGE-20, possessing a more differentiated, pre-zymogenic-like status (simultaneous synthesis and efficient secretion of MUC6 and zymogens)[23].
The ectopic expression of human telomerase reverse-transcriptase catalytic subunit gene (hTERT) in differentiated normal human cells is sufficient to restore telomerase activity, thus preventing telomeres’ shortening and inducing continuous cell proliferation[27]. Indeed, telomerase activity is only dependent on the presence of its hTERT subunit, since its template RNA component, used for the addition of telomere repeats at the chromosome tips at each cell cycle, is constitutively synthesized in normal cells[28]. Based on these findings, the induction of hTERT has been intensively used in the last decade in the establishment of novel immortalized cell lines from primary cultures of a variety of human cells and tissues (e.g., skin fibroblasts[28], T lymphocytes[29], airway epithelial cells[30], proximal renal tubules epithelial cells[31], stromal and epithelial immortalized endometriotic cells[32], etc.). These hTERT-expressing cell lines grow out of a background of senescence, present fewer, if any, karyotypic modifications and maintain their normal features of differentiation, a major improvement over the use of viral oncogenes[30,31,32,33]. The effect of hTERT over-expressing in immortalized cell lines, characterized by unlimited life span, is still poorly known. However, hTERT over-expression was shown to improve the classical immortalized and continuously dividing CHO-K1 (Chinese hamster ovary) cell line, increasing its resistance to serum-deprivation induced apoptosis and allowing this serum-dependent cell line to survive, attach and divide in un-supplemented basal medium[34]. Thus, considering these approaches as valuable strategies for cell engineering, here we aimed to establish novel NCI-N87-derived epithelial cell lines by ectopic over-expression of the hTERT, characterize them and assess their usefulness in H. pylori-infection in vitro assays.
The pGRN145 (ATCC MBA-141, Geron Corporation, Menlo Park, CA, United States) is a mammalian expression vector containing the full coding region of the hTERT catalytic subunit gene, under the control of the myeloproliferative sarcoma virus promoter. The plasmid contains the resistance gene for hygromycine B (HygB) for selection in mammalian cells.
The NCI-N87 cell line (ATCC CRL-5822) was grown at 37 °C with 5% CO2 and 99% humidity in Dulbecco’s modified Eagle’s medium (DMEM/F12) (Invitrogen, Life Technologies, Carlsbad, CA, United States) supplemented with 10% (v/v) of heat inactivated (56 °C for 30 min) foetal bovine serum (FBS) (Invitrogen). Cells were sub-cultured using 0.05% trypsin/EDTA solution (Invitrogen) for 5 min.
Transfection of NCI-N87 cell line with 2 μg of pGRN145 was made using the FuGENE®-HD reagent (Roche Diagnostics, Mannheim, Germany). After two weeks in 250 μg/mL HygB (Invitrogen) selection medium, 8 isolated clones were scraped with a micropipette under the microscope and seeded in new plates. The remaining hTERT-expressing clones were pulled together for control. From here, the hTERT-expressing cell lines were maintained under the same conditions as the parental cell line, with the culture medium now further supplemented with 250 μg/mL of HygB (medium that was found to be toxic for the parental NCI-N87 cell line). Longer incubations (20 to 30 min) with trypsin/EDTA were however required for total detachment of the hTERT-expressing cells, in the sub-culturing procedure.
The relative telomerase activity was measured with the telomeric repeat amplification protocol (TRAP), using the photometric enzyme immunoassay Telo TAGGG Telomerase PCR ELISAPLUS (Roche Diagnostics), according to the manufacturer’s instructions. Briefly, protein extracts prepared from 2 × 105 cells/sample were incubated with a biotin-labeled synthetic primer, allowing telomerase present on the cell sample, if expressed, to add telomeric repeats (TTAGGG) to its 3’-end. These elongation products were then amplified by PCR in the presence of an additional primer (anchor-primer). An internal standard provided by the manufacturers was also added to the reaction vessel, in order to detect Taq DNA polymerase inhibitors during this elongation step. The resulting products were denatured and hybridized to digoxigenin-labeled detection probes (specific for the telomeric repeats). Such complexes were immobilized in a streptavidin-coated microplate, via their biotin label, and were then detected with a horseradish peroxidase (HRP)-conjugated antibody anti-digoxigenin. After incubation with 3, 3’, 5, 5’-tetramethylbenzidine, the peroxidase substrate, the generated product was quantified by measuring the absorbance (Abs) of each sample at 450 nm, against the blank value (reference wavelength 690 nm) using an ELISA reader (SynergyTM 2, BioTek Instruments, Inc., Vermont, E.U.A.) and the respective software GEN5TM (BioTek Instruments, Inc.). A template control provided by the manufacturers was run in parallel. The level of telomerase activity is expressed in percentage as relative telomerase activity of each sample, compared with that of control template.
In order to test for epithelial monolayer polarity and integrity, cells were seeded on porous membranes (0.4 μm) supported by a detachable ring and transepithelial electrical resistance (TEER) was measured with an epithelial voltohmmeter (EVOM; World Precision Instruments, Sarasota, FL, United States) in the following days post-confluence. All cultures were started by expanding the cells in flasks, then about 7.5 × 104 cells were harvested and 200 to 400 μL of cells suspended in fresh media were added to the apical side of each tested filters. Proper volume of media (determined according to the manufacturer’s instructions) was also added to the basolateral compartment. These were considered the standard culture conditions. Tested inserts: SnapwellTM 3407 (polycarbonate) with a 12 mm diameter, providing a growth area of 1.12 cm2 (Corning Costar Corp., Cambridge, MA, United States); collagen-coated Transwell®-COL 3491 (polytetrafluoroethylene) with a 24 mm diameter, providing a growth area of 4.67 cm2 (Corning Costar Corp.); Transwell-clear 3450 (polyester) with a 24 mm diameter, providing a growth area of 4.67 cm2 (Corning Costar Corp.); hydrophilic polytetrafluoroethylene Millicell CM standing filters with a 12 mm diameter, providing a growth area of 0.6 cm2 (Millipore, Bedford, MA, United States); and polyester Millicell inserts with a 30 mm diameter, providing a growth area of 4.2 cm2 (Millipore). The latter 3 were pre-coated with a 0.05% (w/v) collagen IV solution (Sigma-Aldrich, St Louis, MO, United States) before use. The following culture conditions were also tested: DMEM/F12 medium (Lonza, Switzerland) containing 10% (v/v) FBS (Lonza) and 1% (v/v) penicillin-streptomycin (Lonza); Glucose free RPMI medium (Lonza) supplemented with 1% (w/v) galactose (AppliChem, Germany), 10% (v/v) FBS or FBS replacement media (Ultra media, Lonza) with 1% (v/v) penicillin-streptomycin; DMEM/F12 followed by mechanical stimulation; and glucose free RPMI medium supplemented with 1% (w/v) galactose followed by mechanical stimulation. Semi-wet interface was produced by 2 mL media in the basolateral compartment and 50 μL media in the apical compartment after confluency. Mechanical stimulation and continuous wetting of the apical surface were achieved by placing the culture plates on a rocking board in the incubator. Basolateral media was refreshed every two to three days. Electrical resistances of the supporting filter and buffer medium were subtracted to calculate TEER of the monolayer with final results reported per unit surface ohms × cm2.
Cells were seeded onto 8-well chamber slides (Lab-Tek®, Nalge Nunc International, Roskilde, Denmark) and allowed to reach high density before processing. Cells were fixed in 10% (v/v) formaldehyde (Sigma-Aldrich) in 96% ethanol for 1 min and at the end of all staining procedures, slides were mounted with glycerol and sealed with nail polish. For eosin/haematoxylin staining cells were incubated with a Harris haematoxylin solution (Sigma-Aldrich) for 10 min, ammoniacal water 0.4% (v/v) for 3 s and with Eosin Y 2% (w/v) (Panreac Química SA, Barcelona, Spain) for 2 min, with extensive phosphate-buffered saline (PBS) (Invitrogen) washings between each step. For Periodic acid Schiff (PAS)-staining, cells were incubated for 5 min with Periodic acid solution (Sigma-Aldrich), then for 15 min with Schiff reagent (Sigma-Aldrich) and, in some case, an extra incubation period of 90 s with Harris haematoxylin solution was carried out, again with extensive PBS washings between each step. For PAS/Alcian Blue-staining cells were grown on SnapwellTM 3407 inserts (Corning Costar Corp.), in glucose free RPMI, supplemented with galactose followed by mechanical stimulation. Paraffin sections were cut and after a dewax step specimens were treated in 100% ethanol (10 min), rinsed in water (10 min) followed by a 3 min incubation with 3% acetic acid, 2.5 h in 1% Alcian Blue 8GX in 3% acetic acid, rinsed in water for 10 min, oxidized in 1% periodic acid for equal period of time, washed for 5 min, immersed in Schiff´s reagent for 15 min. A final washing with water (5 min) and 0.5% sodium meta-bisulphite (3 min) was followed by a de-hydration step before mounting.
Cells were grown to total confluence on 8-well chamber slides for immunofluorescent images and on Transwell filters 3450 for confocal images. Cells were then rinsed twice with cold PBS supplemented with 1 mM CaCl2 and 1 mM MgCl2 and fixed for 30 min at 4 °C in a 4% (v/v) formaldehyde and 3.7% (w/v) sucrose (Merck, Darmstadt, Germany) solution, in PBS. After two washes with PBS, cells were permeabilized for 30 min with 0.2% (v/v) Triton X-100 (Sigma-Aldrich) in PBS at room temperature (RT), washed three times more with PBS and blocked with 1% (w/v) bovine serum albumin (BSA) in PBS for 1 h at RT, prior to incubation for 1 h at RT with the respective primary antibody (Ab). These were: anti-E-cadherin monoclonal Ab (mAb) (courtesy of Professor Figueiredo’s lab) (diluted 1:1000 in 0.5% (w/v) BSA in PBS); anti-α-tubulin (clone DM1A) mAb (Sigma-Aldrich) (diluted 1:50 in 0.5% (w/v) BSA in PBS); anti-MUC5AC (clone 2H7) mAb (Sigma-Aldrich) (diluted 1:25 in 1% (w/v) BSA in PBS); anti-MUC6 (clone H5) mAb (courtesy of Reis CA[35]) (diluted 1:5 in 1% (w/v) BSA in PBS); anti-PGA5 (clone 4G9) mAb (Sigma-Aldrich) (diluted 1:25 in 1% (w/v) BSA in PBS); and anti-HGL (H-70) polyclonal Ab (pAb) (Santa Cruz Biotechnology, Inc., CA, EUA) (diluted 1:25 in 1% (w/v) BSA in PBS). Cells were then washed three times with PBS and incubated for 1 h at 37 °C with the fluorescein isothiocyanate (FITC)-conjugated anti-mouse IgG (Sigma-Aldrich) [diluted 1:100 in 1% (w/v) BSA in PBS] and the FITC-conjugated anti-rabbit IgG (Sigma-Aldrich) (diluted 1:100 in 1% (w/v) BSA in PBS) for primary mAb and pAb recognition, respectively. After three additional washing steps, cell slides were mounted in Vectashield (Vector Laboratories, Burlingame, CA, United States) (whenever necessary it was used Vactashield containing 4, 6-diamino-2-phenylindole (DAPI) (Sigma-Aldrich) for nucleic acid staining) and their immunofluorescence was observed and recorded on an Axiovert 40CFL fluorescence microscope (Carl Zeiss, Jena, Germany) equipped with an Axiocam MRc5 (Carl Zeiss) camera. Images were processed with the software AxioVision Rel. 4.6.3 (Carl Zeiss). Confocal images were recorded with the 405 nm, 488 nm, and 532 nm laser lines of a Leica TCS-SPE confocal microscope and processed with Leica and Adobe Photoshop software.
Cell lines cultured on Snapwell membranes (5 μm) were fixed in Methanolic Carnoy’s solution, paraffin-embedded, dewaxed and rehydrated. Antigen retrieval used was: 10 mM citric acid (Sigma-Aldrich), pH 6 at 99 °C for 30 min, then 40 min at RT, followed by washing with PBS for MUC1, MUC5AC and MUC13; or with an additional step for the MUC2 and MUC6 antibodies using 10 mM 1,4-dithiothreitol (Fisher Scientific) in 0.1 M Tris/HCl buffer (pH 8.0) (37 °C) for 30 min, followed by 25 mM iodoacetamide (Alfa Aesar, United States) at RT (in dark) for 30 min and washed with PBS. No antigen retrieval was used for carbohydrate antigens. Sections were then treated with 3% (v/v) hydrogen peroxide (Fisher Scientific) for 10 min RT, washed twice with water and once with PBS containing 0.05% Tween 20. Nonspecific binding was blocked using serum free protein block (DAKO, Denmark) for 30 min and incubated with primary antibody for 1 h. The primary antibodies were diluted in serum free antibody diluent (DAKO): anti-MUC5AC mAb (clone 45M1, Sigma-Aldrich, diluted 1:4000), anti-MUC2 pAb (LUM2-3[36], diluted 1:1000) and anti-MUC6 pAb (LUM6-3[36], diluted 1:1000). The anti-MUC13 (R20C1)[37], the anti-MUC1 (BC2)[38] and the anti-carbohydrate antibodies [anti-Lewis A (BG5, Seraclone, Biotest, Dreieich, Germany); anti-Lewis B (BG6, Seraclone); anti-Lewis x (BG7, Seraclone); anti-Lewis y (BG8, Seraclone); anti-blood group A (A0581, Dako); anti-blood group B (A0582, Dako); and anti-blood group H (A0583, Dako)] were used at 1 μg/ml. The specimens were incubated with Broad Spectrum Zymed Poly HRP-conjugated polymer (Invitrogen) for 10 min followed by DAB chromogen (DAKO) for 10 min and counterstained with haematoxylin for 1 min. The samples were washed 3 times with PBS containing 0.05% Tween-20 between each step and in distilled water after the final stain. A human sample from antrum was used as positive control for MUC1 and MUC5AC, duodenum for MUC6, small intestine for MUC2 and colon for MUC13. The percentage of cells expressing the mucin was estimated using blinded scoring of the whole membrane.
For total protein extracts preparation, cells (about 2 × 106) were lysed in 100 μL of Laemmli sample buffer [1.5% (w/v) SDS; 5% (v/v) glycerol; 0.001% (w/v) bromophenol blue; 0.5 mM dithiothreitol (DTT); 31.25 mM Tris, pH 6.8] supplemented with 5 U of Benzonase (Sigma-Aldrich) and 10 mM MgCl2 for nucleic acids degradation. Protein quantification was carried out with the RC DCTM Protein Assay (BioRad, Laboratories, Hercules, CA, United States) according with the manufacturer’s instructions. For mucin detection, 100 μg of total protein extract were vacuum-fixed onto nitrocellulose filters (Schleicher and Schuell, Dassel, Germany) using a Bio-DotTM apparatus (Bio-Rad). For zymogen detection, 100 μg of total protein extract were separated by SDS-PAGE on 12.5% (w/v) polyacrylamide mini-gels and transferred onto nitrocellulose filters. After 15 min wash with 0.1% (v/v) Tween-20 in PBS (PBS-T), membranes were blocked for 2 h in 5% (w/v) skim milk in PBS-T at RT and, then, probed over-night, at 4 °C, with mucin/zymogen specific Ab diluted in the same skim milk solution. Used antibodies: anti-MUC5AC (clone 2H7) mAb (1:1000 diluted); anti-MUC6 (clone H5) mAb (1:5 diluted); anti-PGA5 (clone 4G9) mAb (1:800 diluted); and anti-HGL (H-70) polyclonal Ab (pAb) (1:800 diluted). For immunodetection, blots were incubated for 2 h at RT with the respective secondary Ab (anti-mouse IgG conjugated with HRP (BioRad) with proper dilution for mAb recognition, or anti-rabbit IgG conjugated with HRP (BioRad), with proper dilution for pAb recognition). Finally, blots were developed using the SuperSignal® West Pico Chemiluminescent Substrate detection system (Pierce, Rockford, IL, United States) and exposed to X-ray films (Fuji Super RX 100NIF, Fujifilm, Tokyo, Japan). Four washing steps with PBS-T were always performed between consecutive incubations.
Bacteria were grown in H. pylori selective medium (Biogerm, Maia, Portugal) at 37 °C in a microaerobic environment (Anoxomat®, MART Microbiology BV, Drachten, The Netherlands) for 24 h.
The bacterial biomass recovered from a 24 h grown blood agar plate was resuspended in NCI-N87 cells growth medium, and diluted to a final concentration of 1 × 108 CFU/mL. NCI-hTERT-CL6 cells grown on 24 multi-well plates (Nalge Nunc International) for cellular viability determination or on snapwell inserts for cytokine secretion evaluation, until 80% to 90% confluence were rinsed twice with PBS and fresh growth medium was added. Bacterial pools were then added at a multiplicity of infection (MOI) of 5 and the plates were maintained under standard cell growth conditions for 24 h. Non-infected cells were used as a control.
Human gastric cells’ viability was assessed by a standard MTT assay (Vybrant® MTT Cell Proliferation Assay, Invitrogen) according with the manufacturer’s instructions. For normalization the value of 100 corresponds to the viability of the control cells (under standard atmosphere conditions).
Culture supernatants were diluted 1:10 and cytokine production was quantified using the CBA Human Inflammatory Cytokines Kit (BD Biosciences, Franklin Lakes, NJ, United States) according to the manufacturer’s instructions. The samples were analyzed on a FACSCalibur™ (BD Biosciences).
Statistical methods should be described when they are used to verify the results. Choose suitable techniques for the statistical treatments; for example, t test (group or paired comparisons), χ2 test, Ridit, probit, logit, regression (linear, curvilinear, or stepwise), correlation, analysis of variance (ANOVA), analysis of covariance, etc.
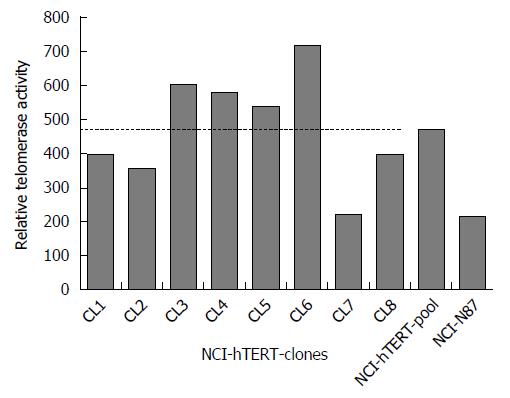
The NCI-N87 cell line was stably transfected with the pGRN145, a plasmid containing the hTERT cDNA. After HygB selection, surviving isolated clones were re-seeded resulting in establishment of eight new cell lines, hereafter named of NCI-hTERT-CL1 to NCI-hTERT-CL8. For control experiments, the remaining hTERT-transfected clones were pooled together, originating the NCI-hTERT-pool cell line. Relative telomerase activity analysis resulted in a clear evidence of the endogenous expression of telomerase in the parental NCI-N87cells (213 units) (Figure 1). This is easily justified by the origin of this cell line in a gastric carcinoma[27,39] and should allow the cells to proliferate beyond senescence. Even though, higher relative telomerase activity levels were observed for the majority of the isolated clones. In average, the clones exhibited a relative telomerase activity of 476 units (± 161), similar to that obtained for the NCI-hTERT-pool cell line (474 units), corresponding to 2.2 times the relative telomerase activity registered for the parental cell line. The highest relative telomerase activity level (717 units, i.e., 3.4 times the relative telomerase activity of the NCI-N87 cell line) was exhibited by the NCI-hTERT-CL6 clone. Therefore, by following our strategy, we were able to efficiently isolate clones of NCI-N87 cell sub-populations exhibiting higher relative telomerase activities, justified by the ectopic induction of the hTERT, which we went to further characterize in terms of growth pattern, phenotype and gastric properties.
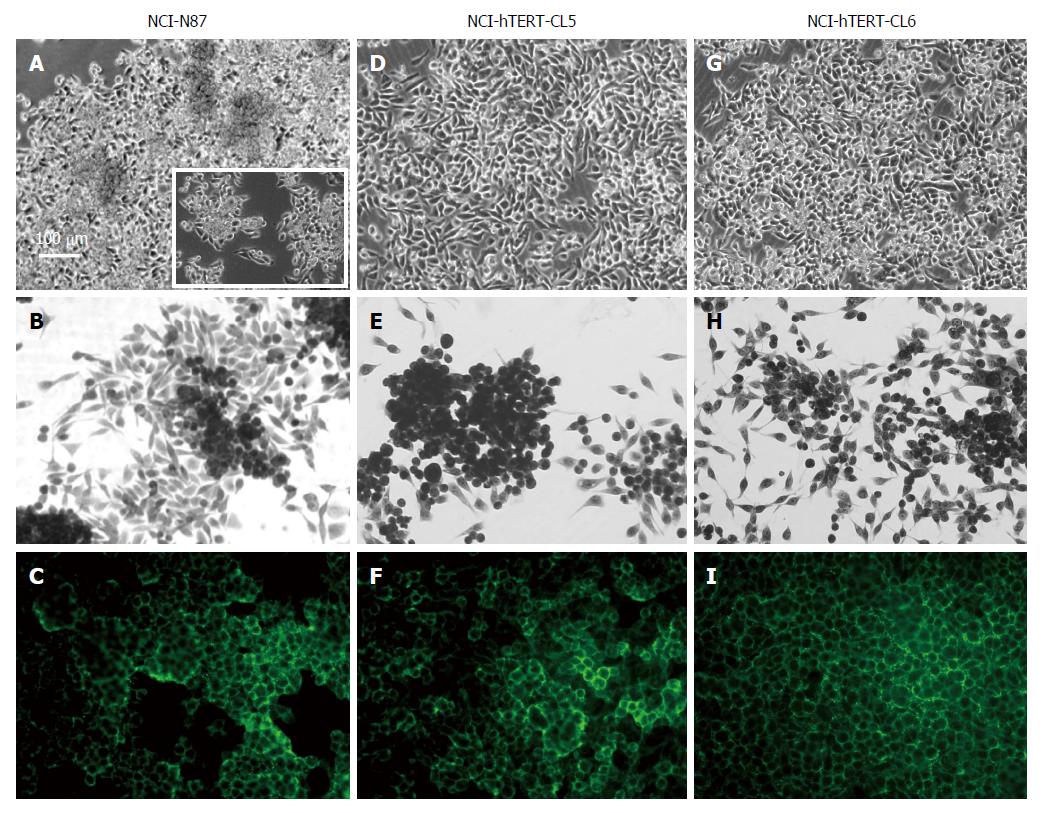
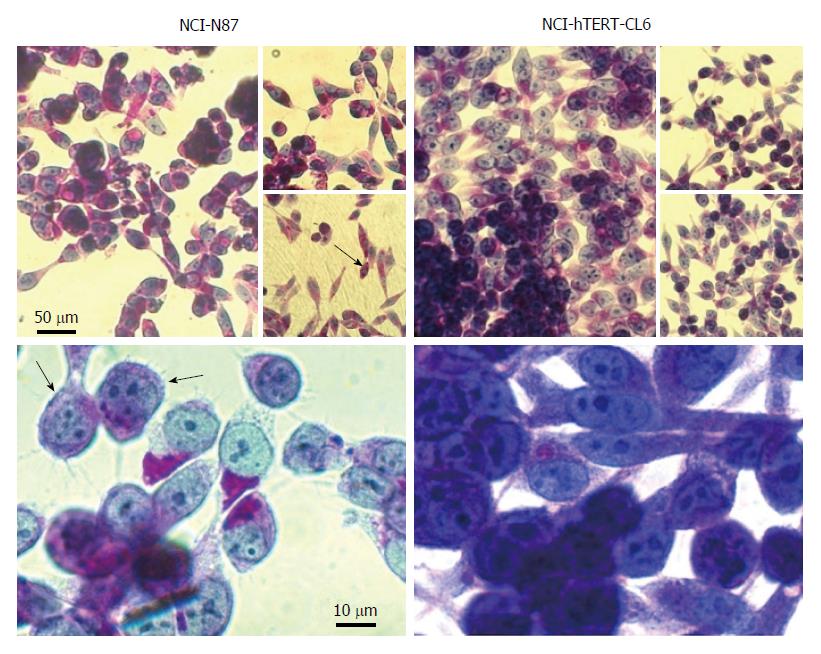
Corroborating its true epithelial nature, already described by Chailler and Ménard[23], the parental NCI-N87 cell line exhibited a colony growth pattern with regions of dense clusters (Figure 2A). Complete adherence was only achieved in hydrophilic plastic surfaces (proper for tissue culture assays) with culture medium supplemented with 10% (v/v) of heat-inactivated FBS. In such conditions, the population doubling time was about 48 h. When seeded at low density, some cells appeared elongated, extending fibres towards the neighbouring cells (Figure 2B) and, at confluency, cells expressed E-cadherin in their cell to cell contacts (Figure 2C).
In agreement with similar experiments with other cell lines[34], over-expression of hTERT resulted in sub-cloned cell lines with enhanced adherence properties. Indeed, those NCI-hTERT clones presenting higher levels of relative telomerase activity (Figure 1), namely CL3, CL5 and CL6, presented the ability to grow in conditions that did not favour the attachment of NCI-N87 cells, i.e., in hydrophobic plastic surfaces with the culture medium supplemented with non-heat-inactivated FBS. This was particularly evident in the NCI-hTERT-CL6, for which longer periods of incubation (30 min compared with the 5 min required for the parental cell line) with trypsin/EDTA were required for complete CL6 cells detachment in sub-culturing procedures. Moreover, those NCI-hTERT-clones exhibited higher mitotic rates compared with the parental cell line, with the CL6 presenting the highest rate, doubling the cell population in about 24 h. When seeded at low density, the NCI-hTERT-clones extended more pronounced elongations (lamellipodia-like protrusions) towards the neighbouring cells, a marked phenotype of CL6 (Figure 2E and 2H). Additionally, despite maintaining a colony growth pattern, the NCI-hTERT-clones 5 and 6 originated more organized post-confluent monolayers (Figure 2D and G, respectively) with all sub-confluent and post-confluent cells systematically expressing E-cadherin (Figure 2F and I, respectively). Again the CL6 presented a more uniform honeycomb-like pattern (Figure 2I).
In contrast with the observations of Fiorentino et al[40] and Lemieux et al[41], that have described the expression of ZO-1 in the all NCI-N87 cell contacts, and of Chailler and Ménard[23] that reported the expression of this protein in relative small cell sub-populations of the NCI-N87 cell line, we were not able to detect the expression of ZO-1 in our parental cell line, nor in the NCI-hTERT clones. This may explain the inability of any of these new cell lines to generate sustained TEER despites all the efforts spent in optimization of culture conditions. Indeed, after testing several proper filters and different culture conditions (see Material and Methods), only low values of TEER (about 70 ohms × cm2) were registered for prolonged cultures (21 d post-confluency) of NCI-hTERT-clones 5 and 6 in polycarbonate Snapwells (3407, Corning Costar Corp.), once grown in RPMI medium supplemented with galactose followed by mechanical stimulation. Notwithstanding, and contrasting with the parental NCI-N87 cells, these hTERT-expressing cell lines, particularly the CL6, could be maintained for long periods post-confluency (up to 4 wk).
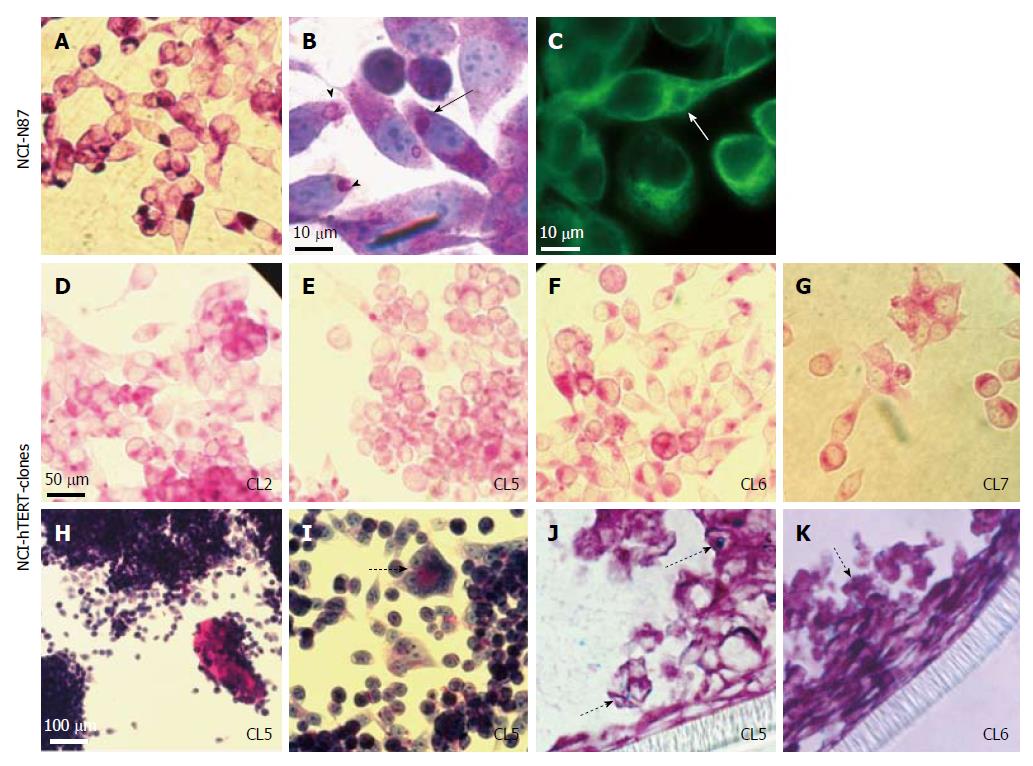
PAS-staining revealed the expression of neutral mucins by the parental NCI-N87 cell line and all the NCI-hTERT clones. The intense vesicular PAS-reactivity exhibited by some cells of the parental cell line (Figure 3A) is supportive of the presence of mucus secreting vesicles that are formed in the endoplasmic reticulum vicinity (arrow head at Figure 3B). Such vesicles, in a close interaction with the microtubule network (white arrow at Figure 3C), migrate towards the cytoplasmic membrane and are exocytosed (black arrows at Figure 3B), following a mucin secretion pathway described by others[42]. However, such phenotype was only acquired by the NCI-hTERT clones in a more differentiated state, upon full confluence. Indeed, sub-confluent cultures of NCI-hTERT cell lines, in particular the NCI-hTERT-CL2, CL5, CL6 and CL7, exhibited a less intense cytoplasmatic PAS reactivity (Figure 3D-G, respectively). A similar pattern was described by Chailler and Ménard[23], who have linked it with an enhanced ability for mucin-secretion exhibited by their non-transfected NCI-N87-derived cell lines. This hypothesis was further supported by the continuous observation of extracellular accumulation of PAS-reactive mucins in some NCI-hTERT clones, namely in CL5 and CL6 (Figure 3H). This event was sometimes accompanied by the appearance of more organized cellular structures, suggesting a more differentiated state for the cells (dashed arrow at Figure 3I). Additionally, traces of Alcian Blue-reactive mucins (acid mucins) were detected for both NCI-hTERT-CL5 and CL6 when grown in polarization favouring culture conditions (semi wet interphase culture for 28 d post confluency), indicated the presence of residual amounts of acidic mucins (dotted arrows at Figure 3J and K). Despite these important data, the tested clones were only able to generate a loose/partial mucus layer, as determined by observation of PAS/Alcian blue stained fixed slides (data not shown).
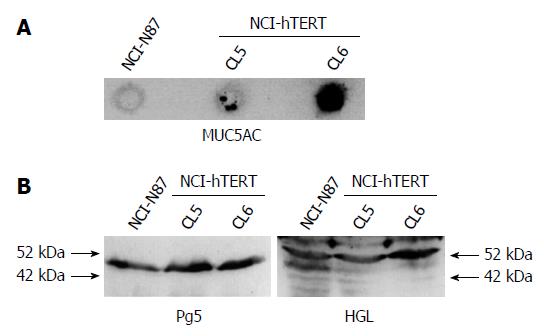
By immunodetection (Figure 4), we were able to confirm the presence of MUC5AC among the secreted and intracellular PAS-reactive mucins. Indeed, our immunocytochemistry data on paraffin-embedded cell lines cultured on Snapwell membranes pointed to an equivalent number of MUC5AC-positive cells in both NCI-hTERT-CL5 and -CL6 (about 25% and about 20%, respectively) (Table 1). Slot-blot analysis proved the expression of MUC5AC by NCI-hTERT-CL6 (Figure 4A), but showed a much lower abundance of this mucin in protein extracts of both NCI-hTERT-CL5 and the parental cell lines. These discrepancies in the abundance of MUC5AC may be explained by the use of different anti-MUC5AC antibodies in each of these two approaches, the 45M1 mAb (Sigma-Aldrich) more suitable for immunocytochemistry and the 2H7 mAb (Sigma-Aldrich) more suitable for western-blot analysis, both recognizing different epitopes. Despite the traces of Alcian-blue-reactive mucins, we were not able to immunodetect MUC6 with none of the used anti-MUC6 antibodies (H5 mAb[35] for western-blot and LUM6-3 pAb[36] for immunocytochemistry), in any of the tested cell lines, i.e., NCI-hTERT-CL5, CL6 and parental cell line (Table 1). Nevertheless, MUC2 is counting for those traces of Alcian-Blue-reactive mucins, since it was detected in about 2% of the cells of both clones 5 and 6. Regarding the membrane-bound mucins, we observed by immunocytochemistry analysis that about 2% of the cells of both clones were positive for MUC13 expression and that about 90% and about 60% of the cells of NCI-hTERT-clones 5 and 6, respectively, were positive for MUC1 (an acidic mucin counting for the membrane/intracellular PAS-reactive mucins) (Table 1). This is a quite interesting result because of the importance of MUC1 for the interaction with H. pylori[43]. These two cell lines differ in their glycan content (Table 2); the NCI-hTERT-CL5 cells were all positive for blood group H type 2 (BG-H) and Lewis x (Lex) antigens that were not detected in CL6 cells. Moreover, Lewis a (Lea) and Lewis y (Ley) antigens were found in a smaller percentage of NCI-hTERT-CL6 (21 to 70%) than CL5 (100%) cells. Both cell lines exhibited BG-A (blood group A) antigens. Further analysis on the glycan status of these mucins led us to conclude that, if present at all, both cell lines display undetectable levels of BG-B (blood group B), Leb, Sialyl-Lea and Sialyl-Lex (Table 2).
| Percent of positive cells | |||||
| Cell line | MUC1 | MUC2 | MUC5AC | MUC6 | MUC13 |
| NCI-hTERT-CL5 | +++ | (+) | ++ | - | (+) |
| NCI-hTERT-CL6 | ++ | (+) | + | - | (+) |
| Glycan structures | |||||||||
| Cell line | BG-A | BG-B | BG-H | Sialyl-Lea | Sialyl-Lex | Lex | Ley | Lea | Leb |
| NCI-hTERT-CL5 | ++ | - | +++ | - | - | +++ | +++ | +++ | - |
| NCI-hTERT-CL6 | ++ | - | - | - | - | - | ++ | ++ | - |
Chailler and Ménard[23] described the less intense cytoplasmatic PAS-reactivity, similar to that observed in the NCI-hTERT clones (Figure 3), as being typical of the cells with mixed phenotype, i.e., able of simultaneous production of mucins and zymogens. Further corroborating this assumption, the majority of the NCI-hTERT clones exhibited a homogenous positive PAS/haematoxylin staining (in Figure 5 it is exemplified with NCI-hTERT-CL6), suggesting the presence of basic molecules, such as zymogens, in the cell cytoplasm, in addition to neutral mucins (PAS-reactive mucins). Such PAS/haematoxylin positive pattern was observed in all subconfluent and postconfluent NCI-hTERT transfected cells, in contrast to the parental cell line in which this phenotype was observed only in some cell subpopulations (black arrows in Figure 5). Such observation led us to conclude that the NCI-hTERT-CL5 and CL6 derive from these NCI-N87 cell subpopulations. With this staining procedure, it has also become evident (Figure 5) that the cells of both clones exhibit relative large nuclei, feature shared by progenitor-like gastric cells (reviewed in[3]). In contrast, no reactivity to eosin was observed either in the parental cell line or in its hTERT-expressing-derived clones (data not shown), clearly demonstrating the absence of parietal-related cells in these cell lines.
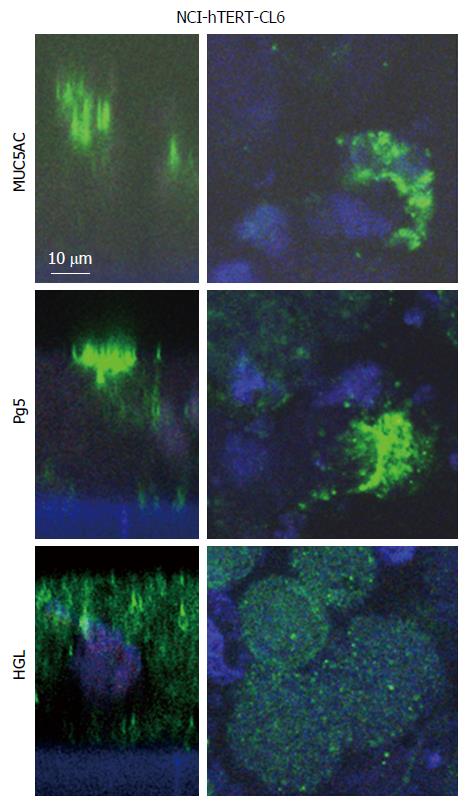
By Western blot analysis, we were able to confirm the expression of both HGL and Pg5 zymogens in the parental cell line and NCI-hTERT-clones 5 and 6 (Figure 4B). Immunocytochemistry analyses (Figure 6) have further confirmed the progenitor-like phenotype, i.e., simultaneous expression of mucins (MUC5AC) and zymogens (Pg5 and HGL), of NCI-hTERT-CL6. Confocal images showed ubiquitous apical vesicular-like distribution of both MUC5AC and Pg5 and cytoplasmic granular-like (dotted signal) distribution for HGL.
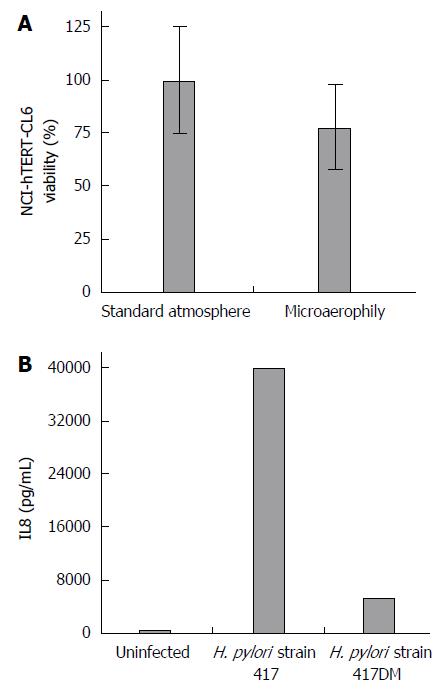
To better recreate the natural niche of H. pylori infection it would be important to carry out the co-culture assays under microaerobic conditions to avoid bacterial death[1,21]. After 48 h of incubation in this conditions, confluent NCI-hTERT-CL6 monolayers showed only a slight decrease (with no statistical significance) in cell viability (Figure 7A) and maintained their integrity (data not shown), favouring its use for in vitro H. pylori infection assays. The measurement of IL-8 and other secreted cytokines has been important in assessing the cellular response of in vitro models to H. pylori virulence factors[40]. Therefore, to further assess the usefulness of this hTERT-expressing gastric cell line for H. pylori research, co-culture assays were performed using two H. pylori strains differing in virulence, i.e., the clinical strain 417, positive for homB, which is a paediatric-ulcer associated biomarker, with proinflammatory characteristics, and its homB double mutant (strain 417DM), with both homB copies inactivated[10]. By measuring the IL-8 secretion by NCI-hTERT-CL6 cells upon infection (Figure 7B), it was possible to verify that these cells are quite sensitive to H. pylori, presenting a response dependent on the virulence of the strain. Indeed, 24 h of co-culture with the strain 417 caused a about 66 fold increase in IL-8 secretion by NCI-hTERT-CL6 cells, which was dramatically higher than with the homB double-mutant strain (417DM), in accordance to the pro-inflammatory characteristics of this virulence factor.
Corroborating the findings of others, here we have demonstrated that the NCI-N87 cell line exhibits some of the features of a true gastric epithelium[1,44]. Deriving from a well differentiated human gastric carcinoma, we observed that these cells preserve the colony-forming growth pattern, the expression of E-cadherin in cell to cell contact and, only in some cell sub-populations, the expression of PAS-reactive mucins and haematoxylin-reactive zymogens. Although advantageous in closer-resembling the heterogeneity of the native tissue, the presence of several types of cells with marked phenotypic differences among them, may hamper the reproducibility of in vitro studies using this cellular model. Indeed, lab maintenance of heterogenic cell lines may lead to accidental loss of some cell sub-populations, always favouring the presence of those with better adhesion and/or mitotic rates properties, which may not necessarily be the ones that better represent the functions of that native tissue. This may explain differences between our NCI-N87 cell line and the equivalent cell line used by others[23,41], despite their common origin (ATCC CRL-5822). Indeed, in contrast to the previously described intense immunodetection of MUC6 in some cell sub-populations of the NCI-N87 cell line[1,23], we were not able to immunodetect this particular mucin, either in protein extracts or in cell slides. In addition, no ZO-1-expressing cells were detected in the NCI-N87 cell line used in the present study, opposing to the observations of Fiorentino et al[40] and Lemieux et al[41] that described the expression of ZO-1 in the all NCI-N87 cell contacts and of Chailler and Ménard[23] that reported the expression of this protein in few NCI-N87 cell sub-populations.
As Chailler and Ménard[23], we were thus prompted to generate new NCI-N87-derived cell lines exhibiting more homogenous phenotype and, simultaneously, the functional properties of the gastric glandular epithelial cells. Using a completely different approach, we succeed in isolating eight NCI-N87-derived clones of cells by transduction of the hTERT cDNA, which in average showed a 2.2 times increase in the relative telomerase activity over the endogenous level registered for the parental cell line. In normal circumstances, telomerase is active in embryonic cells, germ cells, and some cell sub-populations in tissues with regenerative capacity, but repressed (partially or fully) in somatic cells. Such somatic cells once in culture, by loosing telomeric DNA at each cell division, eventually enter in senescence, a non-replicative state that can be avoided by transfection with some viral oncogenes[45]. Nevertheless, when telomeres become critically short, these transformed cells with extended replicative life span eventually cease dividing, a second proliferative blockade named crisis. Therefore, telomeric shortening represents the molecular device that tallies replicative doublings and induces senescence and then crisis[27]. Accordingly, spontaneous telomerase activation warrants the ability of cancer cells to divide beyond the replicative capacity of normal somatic cells, exhibiting unlimited growth in culture. This is fairly known to be a frequent, although not essential, late event in gastric cancer progression[39]. Naturally, its origin in a human gastric carcinoma justifies the endogenous relative telomerase activity registered in our parental NCI-N87 cell line. In 1998, the ectopic over-expression of hTERT was shown to be sufficient to induce cellular immortalization by allowing cells to proliferate beyond crisis[27]. This strategy has been ever since extensively used in the establishment of novel immortalized cell lines without inducing malignant phenotypic effect, but instead preserving their native features[28-33]. hTERT over-expression was also shown to bring better features to the CHO-K1 cell line. Indeed, by presenting higher amounts of hTERT than those endogenously observed for the CHO-K1 cell line, the hTERT-transfected CHO-K1 cells presented an increase in the maximum cell number in batch culture, reduced apoptosis, prolonged culture duration and reduced serum dependency[34]. Corroborating these findings, we have shown here that the NCI-hTERT-clones presenting higher levels of relative telomerase activity (CL3, 5 and 6) exhibited better adhesion properties, much higher mitotic rates and much prolonged culture maintenance compared to the parental NCI-N87 cell line. These properties were much more pronounced in the NCI-hTERT-CL6, the one with the highest rate of relative telomerase activity, which we were able to maintain in culture for up to 4 wk post-confluency. Additionally, this clone exhibited more pronounced lamellipodia-like structures at low cell density, protrusions observed by Chailler and Ménard[23] in their NCI-N87-derived clone HGE-17 (human gastric epithelial-17 cell line), but only under the exogenous growth factors treatment. The NCI-hTERT-CL6 cell line also exhibited a more uniform honeycomb-like pattern of expression for E-cadherin. Probably due to the lack of ZO-1 expression, also registered for the other tested clones and for the parental cell line, only low levels of TEER were achieved even for prolonged cultures (21 d post-confluency), never exceeding 70 ohms × cm2. Better values were obtained by Chailler and Ménard[23] for their NCI-N87-derived clones, reaching similar TEER values for the clone HGE-17 and higher values (about 300 ohms × cm2) for the clone HGE-20, at 14 days post-confluency, both cell lines exhibiting ZO-1 expression at all cells’ periphery. Contrasting with us, but also with these authors, Fiorentino et al[40] and Lemieux et al[41] presented independently the NCI-N87 cell line itself, as a gastric epithelial barrier model, able to generate per si much higher TEER values (> 1000 and of about 500 ohms × cm2, respectively)[40,41]. As mentioned above, in this case, and probably justifying these data discrepancy, the used NCI-N87 cell line exhibited generalized expression of ZO-1 at cell contact surfaces. Future experiments will dictate whether higher TEER values can be generated after ectopic induction of ZO-1 in our NCI-hTERT-CL6 cell line.
PAS-staining revealed huge differences between the parental cell line and its hTERT-expressing derived clones, suggestive of a more differentiated secretory phenotype for the latter. Indeed, for NCI-hTERT-CL5 and -CL6, although presenting slightly distinctive features between them, abundant expression of MUC1 and MUC5AC, and traces of MUC2 and MUC13 were detected by immunohistochemistry, corroborating previous results[46]. In this way, we demonstrated the ability of both NCI-hTERT-CL5 and -CL6 to produce and secrete the gel-forming glycoprotein MUC5AC (supported by the PAS-positive secreted glycoconjugates and the apical accumulation of fluorescent signal specific for MUC5AC in confocal images), a major component of the mucus layer covering the healthy gastric superficial epithelium. It is an important finding, even considering that these cells are able to generate only a loose mucus layer (data not shown). In addition to close resemblance of the healthy epithelial native tissue, these cells expressed high amounts of MUC1, the most common membrane-tethered mucin of the healthy gastric mucosa. In contrast, these cell lines did not show reactivity with the used anti-MUC6 antibodies, indicating that MUC6, the second most abundant mucin of the mucus layer, mainly found in the deep glands of the healthy gastric mucosa, if present at all, occurs in very low amounts. It is known that the normal pattern of mucins expression changes during gastric neoplasic transformation, resulting in a decrease of MUC5AC in the late stages of disease and of MUC6 in intestinal metaplasia and/or intestinal-type gastric carcinomas. Moreover, such disease process is also accompanied by an increase in the gastric expression of MUC2 (secreted mucin) and MUC13 (transmembrane mucin), two human intestinal mucins usually absent in the normal gastric mucosa[47]. Thus, the residual expression of these two mucins by the NCI-hTERT-clones 5 and 6 corroborates the origin of the parental cell line in a well differentiated-type human gastric carcinoma. Mucins are naturally decorated with a vast number of glycans which differ between individuals and change during disease[36,48]. Indicating the isolation of different cell sub-types, the clones NCI-hTERT-CL5 and CL6 differ in their glycan content. Indeed, the BG-H and Lex antigens were only detected in NCI-hTERT-CL5 cell line (in about 100% of the cells), which also presented higher amounts of Ley and Lea compared with the NCI-hTERT-CL6. Notwithstanding, both cell lines exhibited equivalent amounts of BG-A and undetectable levels of BG-B and Leb. Moreover, in agreement with the residual expression of cancer-associated mucins (MUC2 and MUC13), we were not able to detect the presence of sialyl-Lex nor sialyl-Lea, glycans commonly found in tumour samples[36,48].
Entailing good gastric functions to these new cell lines, both NCI-hTERT-clones 5 and 6 were shown to express HGL and Pg5. Confocal microscopy showed the accumulation of Pg5 in vesicle-like structures in the apical region of the CL6 cells grown in polarization-favouring conditions, suggesting the efficient secretion of this zymogen, as described by Chailler and Ménard[23] for their HGE-20 clone. Furthermore, a dotted fluorescence spread through the cell cytoplasm for HGL, similar to that observed for the HGE cell lines[23], proved the production and suggests a not so efficient secretion of this zymogen. Although future experiments are needed to measure the enzymatic activity of both Pg5 and HGL (by specific enzymatic assays) on our new cell lines, based on the literature we may speculate good lipase and pepsin activities[1,4,23,44]. It is well known that gastric epithelial cells and their organization into pit-glands (Figure 8) play a major role in the normal physiology of the human stomach. These include the foveolar cells of the surface (MUC5AC-secreting cells) and neck (MUC6-secreting cells), the acid-secreting parietal cells of the neck, and the zymogens (HGL and Pg5)-secreting chief cells (oxyntic glands) or the endocrine cells (pyloric glands) of the base of those tubular structures. Leblond et al, in the late 1940s, have shown that the cellular renewal of the gastric glands upon tissue injury is dependent on a group of undifferentiated cells of the isthmus (reviewed in[2,3]). These cells migrate bidirectionally up to the mucosal surface and down to the gland base, as they differentiate into mature cells of the gastric unit. Nowadays, it is well established that the perpetual renewal of healthy mucosa is dependent on the presence of isthmal stem (with high nucleus/cytoplasm ratios, open chromatin, small and scant organelles, many ribosomes and mini-granules) and progenitor cells (still presenting relative large nuclei). The latter include those exhibiting dual lineage features (i.e., uncommitted progenitor cells) and those already presenting features of only one lineage of mature cells (i.e., committed progenitor cells) (reviewed in[2,3]). One of the cell subpopulations isolated by Chailler and Ménard[23] from the parental NCI-N87 cell line, the HGE20 clone, presented a pre-zymogenic-like phenotype, being able of packaging zymogens (simultaneously HGL and Pg5) into granule-like structures, just as normal gastric chief cells, and co-synthesized MUC6 (Figure 8). Such type of immature cells correspond to mucous cells of the neck that further differentiate into zymogenic cells, giving rise to mature chief cells during their down-migration into the base of the gland. Interestingly, cells from both NCI-hTERT-clones 5 and 6 accumulate the functions of mature surface foveolar cells and chief cells and present large nuclei, representing a different type of uncommitted progenitor-like cells (Figure 8).
The glandular organization of this tissue, also critical to its role as a barrier to a range of environmental noxious and immunogenic molecules[1,4,44], is jeopardized by H. pylori[5]. During an established infection, the vast majority of H. pylori cells (about 70%) are found in the mucus layer of the superficial gastric mucosa, either motile or adhered to the heavily glycosylated secreted mucins. This location favours the gain of nutrients released from the damaged host cells. In a mucin-type dependent manner, this location is also favourable for the bacteria replication. Indeed, as we have recently shown, higher H. pylori proliferation rates were observed with tumour-derived mucins and mucins from the surface mucosa (MUC5AC) compared with gland-derived mucins (MUC6), with the latter having an antimicrobial activity[48,49]. Therefore, the lack of MUC6 expression by NCI-hTERT-clones 5 and 6 may somehow be advantageous for in vitro infection studies, facilitating the proliferation of H. pylori in co-cultures. Only a smaller fraction of bacteria (about 30%) is found adhered to the epithelial cells’ surface[50], a step that is essential for the ability of H. pylori to cause disease. This intimate attachment prevents bacteria from being eliminated from the stomach by mucus turnover and gastric peristalsis, facilitates evasion from the human immune system and ensures the efficient delivery of the bacterial toxic proteins. This interaction is highly affected by the presence of MUC1 in the apical surface of the epithelium[43], highlighting once again the usefulness of the NCI-hTERT-clones 5 and 6.
H. pylori expresses a multitude of different outer membrane proteins that are used for bacterial adhesion to the highly diverse glyco-epitopes on the secreted and superficial mucins. To date, the best characterized are the blood group antigen-binding adhesin (BabA), a ligand of the host Leb and H type-1 antigens[51], and the sialic acid binding adhesin (SabA) which mediates attachment to the inflammation-associated sialylated (sialyl-Lex and -Lea) antigens[52]. According to our recently presented data, the binding to Leb may lead to an increase in H. pylori proliferation[48]. Although we were not able to detect this type of H. pylori-binding antigens in non-infected NCI-hTERT-clones 5 and 6, our results point to an efficient adherence of different H. pylori strains (data not shown). Predictably there are other equally important ligands mediating this bacteria-host interaction.
Conlin et al[26] demonstrated that compared with the AGS cell line, NCI-N87 cells respond to H. pylori infection in a much closer manner to that of primary cultures of gastric epithelial cells. However, as mentioned by them and other authors[26,40], by making a literature review we may easily reach to the puzzling conclusion that the former is still the most commonly used cellular model for in vitro studies of the molecular events involved in this host-bacterium interaction, resulting many times in ambiguous and controversial data. The reliability of this cellular model is, indeed, questionable if we consider that, lacking E-cadherin expression, AGS monolayers may eventually lose their integrity after reaching confluency[1,4,22,44]. This is a significant bias since H. pylori is known to disrupt the cell-cell adhesion of the gastric epithelium, namely interfering with the E-cadherin distribution[26]. Moreover, the synthesis of zymogens in AGS cell line is confined to cell sub-populations always presenting a diffused cytoplasmic distribution, an obvious disadvantage when compared with their granular-like distribution observed in the NCI-N87 cell line or its clones[1,4,23,44]. Despite all these, it is only recently that the potential of the parental NCI-N87 cell line began to be explored[22,40,53]. Moreover, although quite promising, the NCI-N87-derived cellular models HGE-17 and HGE-20 have been scarcely used in the study of the H. pylori infection. We found only one reference to the use of the latter, demonstrating the ability of H. pylori to disrupt human gastric tight junctional claudin-4[54].
Hopefully, the NCI-hTERT-clones, namely CL5 and CL6, with all the improvements here described, may bring important input for future studies within H. pylori field. Here, we demonstrated the usefulness of NCI-hTERT-CL6 cell line for such studies, showing its resistance to microaerobic conditions. Indeed, in conditions that favour bacterial survival and growth[1,21], thus, resembling more closely the natural process of infection, confluent monolayers of NCI-hTERT-CL6 maintained their integrity and cells’ viability for at least 48 h. Moreover, here we have also shown the strong response of this hTERT-expressing NCI-derived clone to H. pylori, by measuring the IL-8 secretion upon infection with two strains varying in their virulence. As in the parental cell line NCI-N87[40,55], or perhaps in a more efficient manner, H. pylori elicits a huge IL-8 secretion in the NCI-hTERT-CL6 cells, which we show to be dependent on the virulence of the infecting strain.
In summary, NCI-hTERT-CL5 and -CL6 represent new hTERT over-expressing human gastric cell lines with very good in vitro growth properties, expression and secretion of gastric-type zymogens (Pg5 and HGL) and MUC5AC, as well as expression of normal membrane-bound mucins (namely MUC1), resistance to microaerobic conditions and good responsiveness to H. pylori. As the parental cell line has been established from a tumor, these subclones should also maintain the same malignant phenotype. This is an obvious limitation in their use for cancer related studies.
We thank Profeseor C. Figueiredo and Professor C. Dias for kindly providing us with the anti-E-cadherin and the anti-MUC6 (clone H5) antibodies.
Helicobacter pylori (H. pylori) is one of the most successful human pathogens, which colonizes the mucus layer of the gastric epithelium of more than 50% of the world’s population. This curved, microaerophilic, Gram-negative bacterium is implicated in gastric severe diseases such as peptic ulcer disease, gastric adenocarcinoma, and gastric mucosa-associated lymphoid tissue lymphoma. Studies on host-pathogen interactions rely on in vitro studies, using human cell lines. Presently, the lack of a cellular model which correctly mimics the natural niche of H. pylori, i.e., the human stomach, is still limitative for the study of this infection.
Further progress on the research on the normal functions of the epithelial barrier of the human stomach and on their disruption upon infection by requires a new in vitro cellular model that truly mimics the natural properties of this tissue. The present study aimed to establish a new in vitro cellular model of the human gastric epithelium, which is an important contribution in the field of gastroenterology.
The available gastric epithelial cell lines are composed of several types of cells with marked phenotypic differences among them, which may hamper the reproducibility of in vitro studies using this cellular model. In order to overcome this problem, in this study we have used an innovative approach to generate new NCI-N87-derived cell lines exhibiting more homogenous phenotype and, simultaneously, the functional properties of the gastric glandular epithelial cells.
This new cellular model will allow more accurate studies on the host-pathogen interaction in H. pylori infection, since it will be a better model to perform functional in vitro studies in order to evaluate how the bacterium damages the human gastric epithelium.
Cell lines are permanently established cell cultures that proliferate in laboratory conditions given appropriate fresh medium and space. All cell lines are developed from primary cultures
The paper by Saraiva-Pava1 et al is based on a clear-cut concept and presents excellent biochemical and cell-biological work. The established cell clones are shown to be useful for in vitro studies with Helicobacter. The paper is well written and is focusing on essential aspects. It will be of direct value for the specialist in the field, but also give the nonspecialist an excellent introduction into complicated and relevant biological problems of gastroenterology. New cell-lines on this manuscript are hopefully to use in gastric physiological studies. It is striking.
P- Reviewer: Bauer G, Matsui H S- Editor: Yu J L- Editor: A E- Editor: Wang CH
| 1. | Basque JR, Chénard M, Chailler P, Ménard D. Gastric cancer cell lines as models to study human digestive functions. J Cell Biochem. 2001;81:241-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 2. | Mills JC, Shivdasani RA. Gastric epithelial stem cells. Gastroenterology. 2011;140:412-424. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 166] [Cited by in RCA: 152] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 3. | Karam SM. A focus on parietal cells as a renewing cell population. World J Gastroenterol. 2010;16:538-546. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 35] [Cited by in RCA: 30] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 4. | Chailler P, Beaulieu JF, Ménard D. Isolation and functional studies of human fetal gastric epithelium in primary culture. Methods Mol Biol. 2012;806:137-155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 5. | Basso D, Plebani M, Kusters JG. Pathogenesis of Helicobacter pylori infection. Helicobacter. 2010;15 Suppl 1:14-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 67] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 6. | de Reuse H, Bereswill S. Ten years after the first Helicobacter pylori genome: comparative and functional genomics provide new insights in the variability and adaptability of a persistent pathogen. FEMS Immunol Med Microbiol. 2007;50:165-176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 23] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Lai LH, Sung JJ. Helicobacter pylori and benign upper digestive disease. Best Pract Res Clin Gastroenterol. 2007;21:261-279. [PubMed] |
| 8. | Atherton JC. The pathogenesis of Helicobacter pylori-induced gastro-duodenal diseases. Annu Rev Pathol. 2006;1:63-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 394] [Cited by in RCA: 410] [Article Influence: 22.8] [Reference Citation Analysis (0)] |
| 9. | Konturek PC, Konturek SJ, Brzozowski T. Helicobacter pylori infection in gastric cancerogenesis. J Physiol Pharmacol. 2009;60:3-21. [PubMed] |
| 10. | Oleastro M, Cordeiro R, Ferrand J, Nunes B, Lehours P, Carvalho-Oliveira I, Mendes AI, Penque D, Monteiro L, Mégraud F. Evaluation of the clinical significance of homB, a novel candidate marker of Helicobacter pylori strains associated with peptic ulcer disease. J Infect Dis. 2008;198:1379-1387. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 58] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 11. | Oleastro M, Cordeiro R, Yamaoka Y, Queiroz D, Mégraud F, Monteiro L, Ménard A. Disease association with two Helicobacter pylori duplicate outer membrane protein genes, homB and homA. Gut Pathog. 2009;1:12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 37] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 12. | Oleastro M, Santos A, Cordeiro R, Nunes B, Mégraud F, Ménard A. Clinical relevance and diversity of two homologous genes encoding glycosyltransferases in Helicobacter pylori. J Clin Microbiol. 2010;48:2885-2891. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 30] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 13. | Vitoriano I, Saraiva-Pava KD, Rocha-Gonçalves A, Santos A, Lopes AI, Oleastro M, Roxo-Rosa M. Ulcerogenic Helicobacter pylori strains isolated from children: a contribution to get insight into the virulence of the bacteria. PLoS One. 2011;6:e26265. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 14. | Lopes AI, Palha A, Lopes T, Monteiro L, Oleastro M, Fernandes A. Relationship among serum pepsinogens, serum gastrin, gastric mucosal histology and H. pylori virulence factors in a paediatric population. Scand J Gastroenterol. 2006;41:524-531. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 15. | McGuckin MA, Lindén SK, Sutton P, Florin TH. Mucin dynamics and enteric pathogens. Nat Rev Microbiol. 2011;9:265-278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 907] [Cited by in RCA: 1038] [Article Influence: 74.1] [Reference Citation Analysis (0)] |
| 16. | Linden SK, Sutton P, Karlsson NG, Korolik V, McGuckin MA. Mucins in the mucosal barrier to infection. Mucosal Immunol. 2008;1:183-197. [PubMed] |
| 17. | Lindén S, Semino-Mora C, Liu H, Rick J, Dubois A. Role of mucin Lewis status in resistance to Helicobacter pylori infection in pediatric patients. Helicobacter. 2010;15:251-258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 38] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 18. | Krueger S, Hundertmark T, Kuester D, Kalinski T, Peitz U, Roessner A. Helicobacter pylori alters the distribution of ZO-1 and p120ctn in primary human gastric epithelial cells. Pathol Res Pract. 2007;203:433-444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 46] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 19. | Kusters JG, van Vliet AH, Kuipers EJ. Pathogenesis of Helicobacter pylori infection. Clin Microbiol Rev. 2006;19:449-490. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1446] [Cited by in RCA: 1529] [Article Influence: 80.5] [Reference Citation Analysis (1)] |
| 20. | Yokozaki H. Molecular characteristics of eight gastric cancer cell lines established in Japan. Pathol Int. 2000;50:767-777. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 157] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 21. | Lindén SK, Driessen KM, McGuckin MA. Improved in vitro model systems for gastrointestinal infection by choice of cell line, pH, microaerobic conditions, and optimization of culture conditions. Helicobacter. 2007;12:341-353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 36] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 22. | Oliveira MJ, Costa AM, Costa AC, Ferreira RM, Sampaio P, Machado JC, Seruca R, Mareel M, Figueiredo C. CagA associates with c-Met, E-cadherin, and p120-catenin in a multiproteic complex that suppresses Helicobacter pylori-induced cell-invasive phenotype. J Infect Dis. 2009;200:745-755. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 85] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 23. | Chailler P, Ménard D. Establishment of human gastric epithelial (HGE) cell lines exhibiting barrier function, progenitor, and prezymogenic characteristics. J Cell Physiol. 2005;202:263-274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 24] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 24. | Costa AC, Pinto ML, Costa AM, Leite M, Ferreira RM, Oliveira MJ, Atherton JC, Mareel M, Figueiredo C. AGS cells expressing E-cadherin establish tight junctions and constitute a useful model for studying Helicobacter pylori infection (W8.6). Helicobacter. 2009;14:336. |
| 25. | Lindén S, Mahdavi J, Semino-Mora C, Olsen C, Carlstedt I, Borén T, Dubois A. Role of ABO secretor status in mucosal innate immunity and H. pylori infection. PLoS Pathog. 2008;4:e2. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 130] [Cited by in RCA: 129] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 26. | Conlin VS, Curtis SB, Zhao Y, Moore ED, Smith VC, Meloche RM, Finlay BB, Buchan AM. Helicobacter pylori infection targets adherens junction regulatory proteins and results in increased rates of migration in human gastric epithelial cells. Infect Immun. 2004;72:5181-5192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 48] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 27. | Counter CM, Hahn WC, Wei W, Caddle SD, Beijersbergen RL, Lansdorp PM, Sedivy JM, Weinberg RA. Dissociation among in vitro telomerase activity, telomere maintenance, and cellular immortalization. Proc Natl Acad Sci USA. 1998;95:14723-14728. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 468] [Cited by in RCA: 481] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 28. | Ouellette MM, McDaniel LD, Wright WE, Shay JW, Schultz RA. The establishment of telomerase-immortalized cell lines representing human chromosome instability syndromes. Hum Mol Genet. 2000;9:403-411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 157] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 29. | Rufer N, Migliaccio M, Antonchuk J, Humphries RK, Roosnek E, Lansdorp PM. Transfer of the human telomerase reverse transcriptase (TERT) gene into T lymphocytes results in extension of replicative potential. Blood. 2001;98:597-603. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 128] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 30. | Piao CQ, Liu L, Zhao YL, Balajee AS, Suzuki M, Hei TK. Immortalization of human small airway epithelial cells by ectopic expression of telomerase. Carcinogenesis. 2005;26:725-731. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 66] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 31. | Wieser M, Stadler G, Jennings P, Streubel B, Pfaller W, Ambros P, Riedl C, Katinger H, Grillari J, Grillari-Voglauer R. hTERT alone immortalizes epithelial cells of renal proximal tubules without changing their functional characteristics. Am J Physiol Renal Physiol. 2008;295:F1365-F1375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 201] [Cited by in RCA: 231] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 32. | Boccellino M, Quagliuolo L, Verde A, La Porta R, Crispi S, Piccolo MT, Vitiello A, Baldi A, Signorile PG. In vitro model of stromal and epithelial immortalized endometriotic cells. J Cell Biochem. 2012;113:1292-1301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 33. | Toouli CD, Huschtscha LI, Neumann AA, Noble JR, Colgin LM, Hukku B, Reddel RR. Comparison of human mammary epithelial cells immortalized by simian virus 40 T-Antigen or by the telomerase catalytic subunit. Oncogene. 2002;21:128-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 100] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 34. | Crea F, Sarti D, Falciani F, Al-Rubeai M. Over-expression of hTERT in CHO K1 results in decreased apoptosis and reduced serum dependency. J Biotechnol. 2006;121:109-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 26] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 35. | Reis CA, David L, Carvalho F, Mandel U, de Bolós C, Mirgorodskaya E, Clausen H, Sobrinho-Simões M. Immunohistochemical study of the expression of MUC6 mucin and co-expression of other secreted mucins (MUC5AC and MUC2) in human gastric carcinomas. J Histochem Cytochem. 2000;48:377-388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 113] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 36. | Lindén SK, Wickström C, Lindell G, Gilshenan K, Carlstedt I. Four modes of adhesion are used during Helicobacter pylori binding to human mucins in the oral and gastric niches. Helicobacter. 2008;13:81-93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 80] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 37. | Williams SJ, Wreschner DH, Tran M, Eyre HJ, Sutherland GR, McGuckin MA. Muc13, a novel human cell surface mucin expressed by epithelial and hemopoietic cells. J Biol Chem. 2001;276:18327-18336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 216] [Cited by in RCA: 236] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 38. | Price MR, Rye PD, Petrakou E, Murray A, Brady K, Imai S, Haga S, Kiyozuka Y, Schol D, Meulenbroek MF. Summary report on the ISOBM TD-4 Workshop: analysis of 56 monoclonal antibodies against the MUC1 mucin. San Diego, Calif., November 17-23, 1996. Tumour Biol. 1998;19 Suppl 1:1-20. [PubMed] |
| 39. | Hiyama E, Yokoyama T, Tatsumoto N, Hiyama K, Imamura Y, Murakami Y, Kodama T, Piatyszek MA, Shay JW, Matsuura Y. Telomerase activity in gastric cancer. Cancer Res. 1995;55:3258-3262. [PubMed] |
| 40. | Fiorentino M, Ding H, Blanchard TG, Czinn SJ, Sztein MB, Fasano A. Helicobacter pylori-induced disruption of monolayer permeability and proinflammatory cytokine secretion in polarized human gastric epithelial cells. Infect Immun. 2013;81:876-883. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 46] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 41. | Lemieux M, Bouchard F, Gosselin P, Paquin J, Mateescu MA. The NCI-N87 cell line as a gastric epithelial barrier model for drug permeability assay. Biochem Biophys Res Commun. 2011;412:429-434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 42. | Perez-Vilar J, Ribeiro CM, Salmon WC, Mabolo R, Boucher RC. Mucin granules are in close contact with tubular elements of the endoplasmic reticulum. J Histochem Cytochem. 2005;53:1305-1309. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 43. | Lindén SK, Sheng YH, Every AL, Miles KM, Skoog EC, Florin TH, Sutton P, McGuckin MA. MUC1 limits Helicobacter pylori infection both by steric hindrance and by acting as a releasable decoy. PLoS Pathog. 2009;5:e1000617. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 184] [Cited by in RCA: 207] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 44. | Basque JR, Ménard D. Establishment of culture systems of human gastric epithelium for the study of pepsinogen and gastric lipase synthesis and secretion. Microsc Res Tech. 2000;48:293-302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 45. | Shay JW, Wright WE, Werbin H. Defining the molecular mechanisms of human cell immortalization. Biochim Biophys Acta. 1991;1072:1-7. [PubMed] |
| 46. | Navabi N, McGuckin MA, Lindén SK. Gastrointestinal cell lines form polarized epithelia with an adherent mucus layer when cultured in semi-wet interfaces with mechanical stimulation. PLoS One. 2013;8:e68761. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 87] [Cited by in RCA: 101] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 47. | Sheng YH, Lourie R, Lindén SK, Jeffery PL, Roche D, Tran TV, Png CW, Waterhouse N, Sutton P, Florin TH. The MUC13 cell-surface mucin protects against intestinal inflammation by inhibiting epithelial cell apoptosis. Gut. 2011;60:1661-1670. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 106] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 48. | Skoog EC, Sjöling Å, Navabi N, Holgersson J, Lundin SB, Lindén SK. Human gastric mucins differently regulate Helicobacter pylori proliferation, gene expression and interactions with host cells. PLoS One. 2012;7:e36378. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 69] [Cited by in RCA: 72] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 49. | Kawakubo M, Ito Y, Okimura Y, Kobayashi M, Sakura K, Kasama S, Fukuda MN, Fukuda M, Katsuyama T, Nakayama J. Natural antibiotic function of a human gastric mucin against Helicobacter pylori infection. Science. 2004;305:1003-1006. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 253] [Cited by in RCA: 253] [Article Influence: 12.0] [Reference Citation Analysis (1)] |
| 50. | Schreiber S, Konradt M, Groll C, Scheid P, Hanauer G, Werling HO, Josenhans C, Suerbaum S. The spatial orientation of Helicobacter pylori in the gastric mucus. Proc Natl Acad Sci USA. 2004;101:5024-5029. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 215] [Cited by in RCA: 242] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 51. | Ilver D, Arnqvist A, Ogren J, Frick IM, Kersulyte D, Incecik ET, Berg DE, Covacci A, Engstrand L, Borén T. Helicobacter pylori adhesin binding fucosylated histo-blood group antigens revealed by retagging. Science. 1998;279:373-377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 872] [Cited by in RCA: 842] [Article Influence: 31.2] [Reference Citation Analysis (1)] |
| 52. | Mahdavi J, Sondén B, Hurtig M, Olfat FO, Forsberg L, Roche N, Angstrom J, Larsson T, Teneberg S, Karlsson KA. Helicobacter pylori SabA adhesin in persistent infection and chronic inflammation. Science. 2002;297:573-578. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 639] [Cited by in RCA: 665] [Article Influence: 28.9] [Reference Citation Analysis (0)] |
| 53. | Kawai S, Kato S, Imai H, Okada Y, Ishioka C. Suppression of FUT1 attenuates cell proliferation in the HER2-overexpressing cancer cell line NCI-N87. Oncol Rep. 2013;29:13-20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 27] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 54. | Lapointe TK, O’Connor PM, Jones NL, Menard D, Buret AG. Interleukin-1 receptor phosphorylation activates Rho kinase to disrupt human gastric tight junctional claudin-4 during Helicobacter pylori infection. Cell Microbiol. 2010;12:692-703. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 39] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 55. | Jung YJ, Lee KL, Kim BK, Kim JW, Jeong JB, Kim SG, Kim JS, Jung HC, Song IS. [Usefulness of NCI-N87 cell lines in Helicobacter pylori infected gastric mucosa model]. Korean J Gastroenterol. 2006;47:357-362. [PubMed] |