Published online May 14, 2015. doi: 10.3748/wjg.v21.i18.5622
Peer-review started: November 29, 2014
First decision: December 26, 2014
Revised: January 15, 2015
Accepted: February 12, 2015
Article in press: February 13, 2015
Published online: May 14, 2015
Processing time: 170 Days and 3.2 Hours
AIM: To assess the safety and feasibility of peroral esophageal myotomy (POEM) in patients with achalasia.
METHODS: From January 2012 to March 2014, 50 patients (28 men, 22 women; mean age: 42.8 years, range: 14-70 years) underwent POEM. Pre- and postoperative symptoms were quantified using the Eckardt scoring system. Barium swallow and esophagogastroscopy were performed before and after POEM, respectively. Esophageal motility was evaluated in all patients, both preoperatively and one month after POEM treatment, using a high-resolution manometry system. Manometry data, Eckardt scores, lower esophageal sphincter pressure and barium swallow results were used to evaluate the effect of the procedure.
RESULTS: POEM was successfully completed for all patients. The mean procedure time was 55.4 ± 17.3 min and the mean total length of myotomy of the circular esophagus was 10.5 ± 2.6 cm. No specific complications occurred, with the exception of two patients that developed asymptomatic pneumomediastinum and subcutaneous emphysema. Clinical improvement in symptoms was achieved in all patients. Approximately 77.5% of patients experienced weight gain 6 mo after POEM, with an average of 4.78 kg (range: 2-15 kg). The lower esophageal sphincter resting pressure, four second integrated relaxation pressure and Eckardt scores were all significantly reduced after POEM (Ps < 0.05). A small segment of proximal esophageal peristalsis appeared postoperatively in two patients, but without normal esophageal peristalsis. The average diameter of the esophageal lumen decreased significantly from 4.39 to 3.09 cm (P < 0.01).
CONCLUSION: POEM can relieve achalasia symptoms, improve gastroesophageal junction relaxation and restore esophageal body motility function, but not normal esophageal peristalsis.
Core tip: This clinical study describes the successful use peroral esophageal myotomy to treat achalasia patients. The efficacy of this procedure was evaluated by changes in esophageal motility, esophageal morphology and symptoms. The results show that achalasia symptoms were relieved and gastroesophageal junction relaxation and esophageal body motility function were improved up to one year after the procedure.
- Citation: Lu B, Li M, Hu Y, Xu Y, Zhang S, Cai LJ. Effect of peroral esophageal myotomy for achalasia treatment: A Chinese study. World J Gastroenterol 2015; 21(18): 5622-5629
- URL: https://www.wjgnet.com/1007-9327/full/v21/i18/5622.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i18.5622
Achalasia is an esophageal motility disorder of unknown etiology, characterized by the aperistalsis of the distal esophagus and defective relaxation of the lower esophageal sphincter (LES)[1,2]. Although achalasia is rare, recent reports suggest an increasing incidence, with rates of up to 16 per 1000000 per year in some populations, mainly in South America and Europe[3,4]. Clinical symptoms of achalasia include dysphagia, retrosternal pain and the regurgitation of undigested food. The diagnosis of achalasia is made on the basis of symptoms, results of a barium esophagram and endoscopy, as well as esophageal manometry, which is the gold standard. This type of high-resolution manometry (HRM) has demonstrated an increased diagnostic accuracy and yield of achalasia patients compared to traditional methods of diagnosis[5,6].
Although the pathophysiology of achalasia remains largely unknown[5], it has a low mortality rate. However, achalasia is a chronic disorder that severely affects patient quality of life. Endoscopic and surgical therapies focus on relaxation or mechanical disruption of the LES. However, these methods are inefficient, with a high degree of temporary relapse and complications, such as bleeding and perforation[7,8]. Recently, a novel endoscopic technique called peroral endoscopic myotomy (POEM) was developed as a treatment for achalasia treatment[9]. This technique is based on natural orifice transluminal endoscopic surgery[10], in which surgical instruments, and often a camera, are passed through existing openings in the body to avoid scarring and potential complications of invasive surgery. However, the outcomes for POEM need to be critically assessed by clinical studies. Therefore, the aim of this paper was to describe the use of POEM for treating achalasia patients and to evaluate its efficacy via high-resolution manometry (HRM), validated Eckardt symptom scores, esophagogastroscopy and barium swallow.
Patients at the First Affiliated Hospital of Zhejiang Chinese Medical University in China diagnosed with achalasia based on clinical symptoms, barium swallow and HRM [4s integrated relaxation pressure (4sIRP) ≥ 15 mmHg] from January 2012 to March 2014 were eligible for enrollment in the study. Patient exclusion criteria included previous surgery of the stomach and/or esophagus, Barrett’s esophagus, esophageal malignancy, premalignant esophageal lesions, esophageal stricture, liver cirrhosis and/or esophageal varices, active esophagitis, pregnancy, hiatal hernia (> 2 cm) or other coagulopathy. Previous treatment failure, such as botulinum toxin injection or endoscopic balloon dilation, was not considered a criterion for exclusion.
Before POEM treatment, a comprehensive preoperative evaluation was completed for all patients, which included assessment by the Eckardt symptom scoring system[11] and routine biochemical examination, esophagogastroduodenoscopy and computed tomography (CT) scan. The esophageal motility of patients, including lower esophagus sphincter resting pressure (LESP), 4sIRP and lower esophageal sphincter relaxation rate (LESRR), was evaluated using an HRM system (Sierra Scientific Instruments Inc., Los Angeles, CA, United States). HRM was performed by the same evaluating physician each time to minimize variability. All patients were then categorized into three subgroups according to the Chicago classification criteria of esophageal motility disorders based on HRM results and various diagnostic criteria: subtype I, patients with a divided mean 4sIRP ≥ 15 mmHg and 100% failed peristalsis; subtype II, patients with the additional feature of pan-esophageal pressurization with ≥ 20% of swallows; and subtype III, patients with subtype I and II characteristics as well as preserved fragments of distal peristalsis or premature (spastic) contractions with ≥ 20% of swallows[12,13].
All patients provided written informed consent for enrollment in this study, which was reviewed and approved by the Medical Ethics Committee of the First Affiliated Hospital of Zhejiang Chinese Medical University (March 8, 2012; 2012X003).
The equipment for POEM included a single-channel high-definition gastroscope (GIF-H260, CLV-260), a triangle-tip knife (KD-640L), insulation-tipped electrosurgical (IT) knife (KD-611L) and a hook knife (KD-620LR) (Olympus Medical Systems Co., Tokyo, Japan). A transparent distal cap (D-206-02; Olympus) was attached to the tip of the gastroscope with an outer diameter of 9.8 mm. Other equipment included hemostatic clips (HX-610-090L), hot biopsy forceps (5XK), injection needles (NM-200U-0423) (Olympus) and an electrosurgical energy high-frequency generator (VIO 200D; ERBE, Tokyo, Japan).
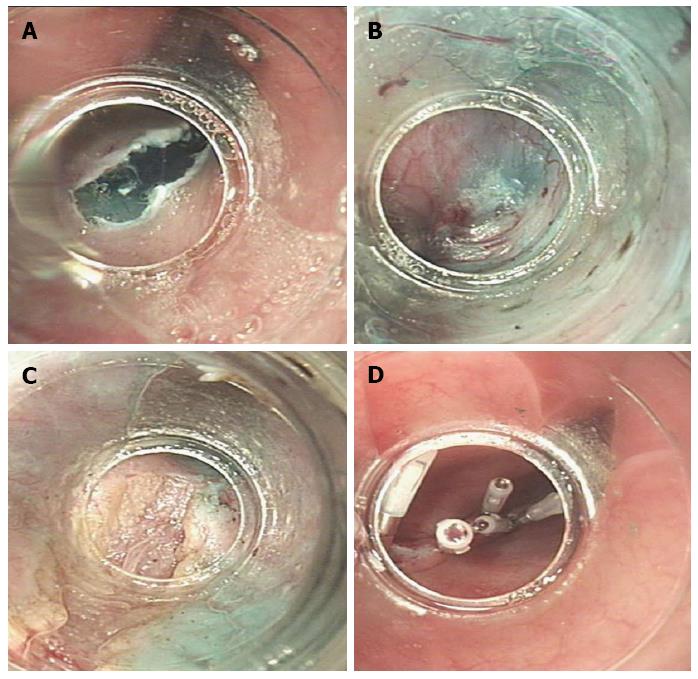
Patients were maintained on a clear liquid diet for three days preoperatively, followed by 24 h of fasting. Appropriate rehydration therapy, prophylactic antibiotics and double-dose proton pump inhibitors (PPI) were given. Before the POEM procedure, patients underwent esophagogastroduodenoscopy to observe the esophageal lumen and to clean out any food remnants from the esophagus. POEM was performed under general anesthesia, requiring endotracheal intubation with the patient in the left lateral decubitus position. The same gastroenterologist performed POEM on all patients. Carbon dioxide gas insufflation was performed using a CO2 insufflator (UCR; Olympus) to control endoscopic air pressure throughout the operation. The procedure is shown in Figure 1.
Mucosal incision: A distal transparent oblique dissecting cap was attached to the endoscope tip to separate tissues inside the submucosal space. The gastroesophageal junction (EGJ) was located and the distance to the incision was measured. A submucosal injection was performed and an initial mucosal incision was made at the level of the mid-esophagus, approximately 10-15 cm proximal to the EGJ on the anterior/posterior esophagus. Approximately 5-10 mL of a 0.9% saline solution containing methylene blue (0.2 mg/mL) and epinephrine (5 μg/mL) was injected to lift the mucosa. After adequate lifting, a 2 cm oblique incision was made on the mucosal surface using a hook knife to allow the endoscope to enter the submucosal space.
Submucosal tunnel: The submucosa and muscular layer were progressively dissected distally using an endoscopic technique, creating a long submucosal tunnel that extended to the EGJ and ended 2-3 cm into the proximal stomach. Hot biopsy forceps were used to cauterize any large blood vessels that were hemorrhaging.
Circular myotomy: The myotomy of the esophageal circular muscle bundle began 2-3 cm distal to the mucosal entry, approximately 7-8 cm above the EGJ, under endoscopic control. The edge of the triangle-tip knife was used to capture and lift the inner circular muscle bundles toward the esophageal lumen. The exposed circular muscle bundle was then cut using the same knife and forceps were used for cauterization. The muscle layer myotomy was performed gradually, cutting distally until reaching the gastric submucosa extending 2-3 cm from the EGJ. Caution was taken to leave the outer longitudinal muscle intact and avoid disruption of extraneous tissues. The esophageal lumen was then left completely unobstructed.
Closure of the mucosal entry: After myotomy, the fluids within the submucosal tunnel and esophageal lumen were absorbed as needed. Small bleeding vessels or hemorrhaging spots were cauterized using hot biopsy forceps. The 2-3 cm long incision site was closed from the distal to the proximal end of the mucosal fenestration with standard hemostatic clips and was confirmed by endoscopic analysis. The endoscope was reintroduced into the esophageal lumen down to the stomach to ensure smooth passage through the EGJ and the gastrointestinal decompression tube was placed under the endoscope to relieve pressure.
After POEM, all patients were kept nil per OS for 24 h, followed by rehydration, antiemetics (i.v.), PPIs and hemostatic treatment as needed. On postoperative day 1, a chest X-ray/fluoroscopy examination was used to rule out procedure-related adverse events, such as opening of mucosal incisions and leaking at the esophageal closure site. Pneumothorax, subcutaneous emphysema and pleural effusion were detected by chest CT on postoperative day 3. If there was no evidence of leaking or incision dysraphism, patients were placed on a clear liquid diet and the gastrointestinal decompression tube was removed. Once patients demonstrated no difficulties with ingesting a full liquid diet, they were gradually adjusted to a semi-liquid diet, followed by a soft diet. Patients were typically discharged from the hospital with a double-dose of PPI for two weeks, pending anticipated results.
One month post-procedure, all patients were scheduled for barium swallow and HRM to re-examine LES pressure, esophageal motility and patency of the EGJ. Follow-up upper endoscopy was performed two months postoperatively to examine esophageal relaxation and healing of the wound. Six months after POEM, the barium swallow was repeated.
The GerdQ questionnaire[14] was used to assess gastroesophageal reflux-related symptoms postoperatively. Postoperative symptoms at 1, 2, 6 and 12 mo were assessed using follow-up patient questionnaires to assess the current Eckardt score. Therapeutic success was defined as amelioration of symptoms, which was based on a drop ≤ 3 points on the Eckardt score after POEM[13].
SPSS version 17.0 (SPSS Inc., Chicago, IL, United States) was used to analyze the data. Measurements were compared using Student’s t-tests for independent or paired samples and are expressed as mean ± SD or mean (range). Linear regression analysis was used to assess the association between manometric parameters and Eckardt score. A two-tailed correlation analysis adopted a Pearson product-moment correlation. Two-sided P < 0.05 was considered as statistically significant. The statistical methods of this study were reviewed by Ji Chonghua from the First Affiliated Hospital of Zhejiang Chinese Medical University.
From January 2012 to March 2014, POEM was successfully performed in 50 patients with achalasia. The demographic information and clinical characteristics of all enrolled patients are presented in Table 1. None of the patients showed signs of other unrelated diseases.
| Characteristic | Value |
| Male:female | 28:22 |
| Age (yr) | 42.5 (14-70) |
| Duration of symptoms (yr) | 6.6 (0.17-40) |
| Eckardt score | 7.5 (3-11) |
| Previous treatments, n (%) | |
| Pneumatic dilation | 8 (16) |
| Nifedipine | 2 (4) |
| Achalasia subtype, n (%) | 35 (70) |
| I | 3 |
| II | 28 |
| III | 4 |
The duration of the POEM procedures ranged from 30 to 120 min, with an average time of 55.4 ± 17.3 min. The dentate line was a mean of 43.4 (36.0-55.0) cm from the incision, the submucosal tunnel was a mean length of 13.5 (8.0-23.0) cm and circular myotomy was 10.5 (3.0-19.0) cm. During the procedure, the entry site within the submucosal tunnel was closed with 2-15 hemostatic clips. No instances of major bleeding occurred intra- or postoperatively. Furthermore, there were no serious complications related to POEM. Mild chest pain appeared in most patients after 7-14 d, which ultimately subsided without additional treatment. A small amount of postoperative asymptomatic pneumomediastinum and subcutaneous emphysema occurred in 2/50 (4%) patients, which resolved after one week.
Patients were followed-up for a mean of 7.25 mo. Thirty-six patients completed 6 mo of postoperative treatment and 12 cases were followed up for > 1 year (Figure 2). POEM was successful in almost all (49/50; 98%) cases, as determined by patient assessment at a 1 mo follow-up exam; one patient had an Eckardt score of 5 (preoperative Eckardt: 11) and unimproved LESP (13.2 mmHg vs 26.0 mmHg, pre- and postoperative, respectively) by HRM, indicating relapse. This patient was then treated with endoscopic balloon dilation (EBD), which reduced the Eckardt score to 2, a score that was maintained for the remainder of the study. Another patient relapsed 2 mo after POEM, presenting with a solid swallowing obstruction for which EBD was requested, which restored the Eckardt score to 1. An additional five cases that did not meet the score of recurrence required supplementary treatment with EBD after POEM for slight discomfort.
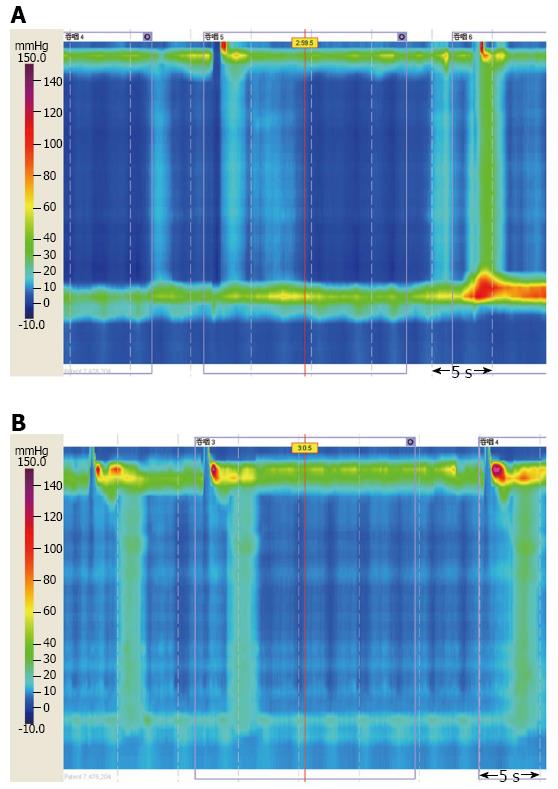
Pre- and postoperative results were available for 35/50 patients, with three patients failing to undergo HRM due to the high pressure within the LES. One month after POEM, LESP and 4sIRP were significantly decreased and LESRR was significantly increased in liquid swallows compared to baseline values (all Ps < 0.01) (Table 2). Representative HRM results are shown in Figure 3. The change in Eckardt score was correlated with the decrease in LESP and 4sIRP (Ps < 0.05), but not with LESP. Interestingly, two patients exhibited a small segment of proximal esophageal peristalsis at postoperative examinations, but normal esophageal peristaltic function was not completely restored.
| Variable | Before | After (1 mo) | P value |
| Lower esophagus sphincter resting pressure, mmHg | 28.94 ± 18.70 | 16.02 ± 5.46 | 0.000 |
| 4s integrated relaxation pressure, mmHg | 27.18 ± 14.63 | 12.22 ± 6.75 | 0.000 |
| Lower esophageal sphincter relaxation rate | 23.00% ± 18.55% | 35.59% ± 21.78% | 0.005 |
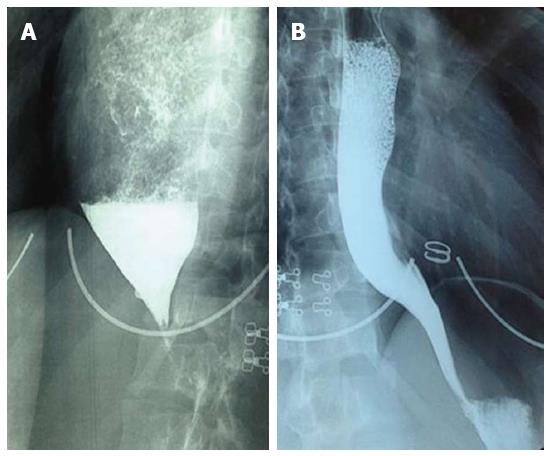
One month after POEM, substantially improved emptying from the esophagus to the EGJ could be observed by a barium swallow (Figure 4). The average esophageal diameter at its widest changed from 4.4 (2.5-8.5) to 3.1 (2.0-7.0) cm. After 6 mo of follow-up, the mean diameter was 3.0 (1.7-7.0) cm, with no retention of barium in the esophagus. The 2 mo postoperative assessment using upper gastrointestinal endoscopy showed that the esophageal mucosal incisions healed well and the endoscopes could pass through the cardiae smoothly, without any signs of esophagitis. Six months after POEM treatment, approximately 77.5% of patients had gained an average of 4.8 (2.0-15.0) kg. There were no reports of reflux symptoms or specific complications during any of the postoperative follow-up assessments (Table 3).
| Complications | Value |
| Pneumomediastinum | 2 (4) |
| Cervical emphysema | 0 |
| Junctional flap perforation | 0 |
| Major bleeding | 0 |
| Acute bleeding or intraoperative bleeding | 0 |
| Delayed bleeding | 0 |
| GER | 0 |
As there is no cure for achalasia, most therapeutic strategies aim to alleviate symptoms by reducing LESP and relieving esophageal obstruction. Traditional treatments for achalasia include medications, EBD, endoscopic botulinum toxin injection and surgical myotomy, all of which have various advantages and drawbacks[5,15-18]. Natural orifice transluminal endoscopic surgery is gaining attention because it is minimally invasive and results in little to no visible scarring. POEM is a related technique that was first described by Pasricha et al[19] in 2007, who performed a myotomy via the esophageal lumen in a porcine model of achalasia. Three years later, Inoue et al[9] demonstrated its effectiveness in relieving achalasia symptoms in human patients, generating fewer traumas and less complications and allowing for rapid recovery.
A number of recent Chinese studies on POEM have been reported, which have focused on the evaluation of its effectiveness[20], patient criteria for treatment[21], management of complications[22], length and location of entry incision[23] and the comparison with other types of surgery, including Heller myotomy[24]. In this study, all patients successfully underwent POEM without reflux symptoms or serious complications and with significantly improved Eckardt scores. There was a 100% (50/50) instant remission rate after surgery and a 96% (48/50) symptom remission rate after six months. This rate of symptomatic relief with POEM is considered high and is in line with previous reports[25,26]. The observed symptom recurrence may have been due to insufficient incision length of the esophageal circular muscle. Supplementary treatment with EBD in seven cases demonstrates the feasibility and safety of POEM. Moreover, 20% of our patients had received prior treatment, demonstrating that POEM can be performed efficiently and safely in recurrent cases. Although some studies have shown that prior therapies (such as EBD or endoscopic botulinum toxin injection) can make the operation more difficult and diminish the outcome[27,28], we found no influence of prior treatment regimens on the ultimate success rate of POEM in treating achalasia, in agreement with other reports[29,30]. Taken together, these results demonstrate that POEM is a suitable treatment option for achalasia patients with various disease stages.
The manometry results show a clear improvement on EGJ relaxation, as evidenced by the significant decrease in LESP and 4sIRP after POEM treatment. Furthermore, the 4sIRP reduction correlates with the decrease in Eckardt score, which is consistent with previous reports[31]. As such, these assessments could be used as a positive predictor before treatment. Furthermore, 4sIRP is a quantifiable method of distinguishing impaired LES relaxation in achalasia from that of a healthy individual[32]. In addition, while the decrease in LESRR is thought to result from the failure of LES relaxation, this measure rises after intervention and has been a continuing issue of debate in achalasia studies[33].
To the best of our knowledge, normal driving esophageal peristalsis cannot be restored by POEM in achalasia patients[34]. Nevertheless, there are several studies showing that some patients can recover a certain level of peristalsis after intervention[35]. A small segment of proximal esophageal peristalsis was recovered in two patients in our study. These peristaltic changes may be explained by a higher accuracy of measurement achieved using the manometry catheter, the narrowing of the dilated esophagus after POEM, or the varying levels in impairment of esophageal inhibitory neurons. If these neurons are damaged beyond repair, it is unlikely that POEM is sufficient to completely restore normal peristaltic function. Thus, POEM cannot completely restore normal esophageal peristalsis, but can improve esophageal body motility and EGJ relaxation.
Our study has several limitations. First, the follow-up assessment period was only one year post-procedure and some patients may show symptom relapse or develop long-term complications. Therefore, a longer-term follow-up study is required to assess the efficacy and safety of this novel treatment method for achalasia. Furthermore, this study is based on a small sample size and the number of each subtype of cases is limited. As POEM is still a relatively new technique, large-scale and/or multicenter studies are needed to fully demonstrate its benefits. Lastly, this was a retrospective study, which has a larger bias than a prospective study. The reliability of its outcomes is directly affected by the integrity and authenticity of collected data. Therefore, there is a need for a randomized controlled trial with long-term follow-up.
In conclusion, POEM is a promising, feasible and safe treatment option for patients with achalasia. This technique demonstrates substantial short-term therapeutic effectiveness, with relief of achalasia symptoms, improved EGJ relaxation and restoration of a certain degree of esophageal body motility function, although normal esophageal peristalsis was not obtained. Importantly, POEM is still in its initial stages of development and further modifications will likely improve the overall benefits. Long-term follow-ups are still needed to thoroughly assess its effectiveness compared with other therapies for the management of achalasia.
Many studies suggest that peroral esophageal myotomy (POEM) is a new therapeutic method for achalasia. However, the short- and long-term outcomes should be assessed by clinical studies, particularly among various populations.
This study reports the initial experience of POEM performed on achalasia patients in the Zhejiang province. The efficacy of POEM was measured with high-resolution manometry, Eckardt symptom scores and barium swallow.
The majority of previous studies assessing POEM in achalasia patients were single- or double-dimension evaluations with short follow-up periods. In the present study, we utilized a multi-dimensional evaluation, which encompasses esophageal motility, esophageal morphology and symptoms. Postoperative assessments at 1, 2, 6 and 12 mo show that POEM can relieve achalasia symptoms, improve gastroesophageal junction relaxation and restore a certain degree of esophageal body motility function. More importantly, this study was performed successfully for the first time in humans in Zhejiang province, China.
While long-term observation of the efficacy of POEM is still required, our data indicate that POEM is a safe and effective therapy for achalasia. Thus, the use of POEM may promote clinical treatment and management and contribute towards progression in achalasia treatments.
Achalasia is an esophageal motility disorder characterized by aperistalsis of the distal esophagus and defective relaxation of the lower esophageal sphincter.
This is a retrospective study of 50 patients with achalasia in Zhejiang province, China, which demonstrates the safety and feasibility of POEM. This study provides strong evidence that POEM is a potential therapeutic treatment that should be considered in clinical application.
P- Reviewer: Attam R, Xu MD, Zhong YS S- Editor: Qi Y L- Editor: Roemmele A E- Editor: Zhang DN
| 1. | Moonen AJ, Boeckxstaens GE. Management of achalasia. Gastroenterol Clin North Am. 2013;42:45-55. [PubMed] [DOI] [Full Text] |
| 2. | Boeckxstaens GE, Zaninotto G, Richter JE. Achalasia. Lancet. 2014;383:83-93. [PubMed] [DOI] [Full Text] |
| 3. | O’Neill OM, Johnston BT, Coleman HG. Achalasia: a review of clinical diagnosis, epidemiology, treatment and outcomes. World J Gastroenterol. 2013;19:5806-5812. [PubMed] [DOI] [Full Text] |
| 4. | Sadowski DC, Ackah F, Jiang B, Svenson LW. Achalasia: incidence, prevalence and survival. A population-based study. Neurogastroenterol Motil. 2010;22:e256-e261. [PubMed] [DOI] [Full Text] |
| 5. | Francis DL, Katzka DA. Achalasia: update on the disease and its treatment. Gastroenterology. 2010;139:369-374. [PubMed] [DOI] [Full Text] |
| 6. | Pandolfino JE, Ghosh SK, Rice J, Clarke JO, Kwiatek MA, Kahrilas PJ. Classifying esophageal motility by pressure topography characteristics: a study of 400 patients and 75 controls. Am J Gastroenterol. 2008;103:27-37. [PubMed] |
| 7. | Muehldorfer SM, Schneider TH, Hochberger J, Martus P, Hahn EG, Ell C. Esophageal achalasia: intrasphincteric injection of botulinum toxin A versus balloon dilation. Endoscopy. 1999;31:517-521. [PubMed] |
| 8. | Karamanolis G, Sgouros S, Karatzias G, Papadopoulou E, Vasiliadis K, Stefanidis G, Mantides A. Long-term outcome of pneumatic dilation in the treatment of achalasia. Am J Gastroenterol. 2005;100:270-274. [PubMed] |
| 9. | Inoue H, Minami H, Kobayashi Y, Sato Y, Kaga M, Suzuki M, Satodate H, Odaka N, Itoh H, Kudo S. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy. 2010;42:265-271. [PubMed] [DOI] [Full Text] |
| 10. | Kim CG. Natural orifice transluminal endoscopic surgery and upper gastrointestinal tract. J Gastric Cancer. 2013;13:199-206. [PubMed] [DOI] [Full Text] |
| 11. | Eckardt VF, Aignherr C, Bernhard G. Predictors of outcome in patients with achalasia treated by pneumatic dilation. Gastroenterology. 1992;103:1732-1738. [PubMed] |
| 12. | Bredenoord AJ, Fox M, Kahrilas PJ, Pandolfino JE, Schwizer W, Smout AJ. Chicago classification criteria of esophageal motility disorders defined in high resolution esophageal pressure topography. Neurogastroenterol Motil. 2012;24 Suppl 1:57-65. [PubMed] [DOI] [Full Text] |
| 13. | Fox MR, Bredenoord AJ. Oesophageal high-resolution manometry: moving from research into clinical practice. Gut. 2008;57:405-423. [PubMed] |
| 14. | Irvine EJ, Whitehead WE, Chey WD, Matsueda K, Shaw M, Talley NJ, Veldhuyzen van Zanten SJ. Design of treatment trials for functional gastrointestinal disorders. Gastroenterology. 2006;130:1538-1551. [PubMed] |
| 15. | Boeckxstaens GE, Annese V, des Varannes SB, Chaussade S, Costantini M, Cuttitta A, Elizalde JI, Fumagalli U, Gaudric M, Rohof WO. Pneumatic dilation versus laparoscopic Heller’s myotomy for idiopathic achalasia. N Engl J Med. 2011;364:1807-1816. [PubMed] [DOI] [Full Text] |
| 16. | Cheatham JG, Wong RK. Current approach to the treatment of achalasia. Curr Gastroenterol Rep. 2011;13:219-225. [PubMed] [DOI] [Full Text] |
| 17. | Pasricha PJ, Ravich WJ, Hendrix TR, Sostre S, Jones B, Kalloo AN. Intrasphincteric botulinum toxin for the treatment of achalasia. N Engl J Med. 1995;332:774-778. [PubMed] |
| 18. | Annese V, Bassotti G, Coccia G, Dinelli M, D’Onofrio V, Gatto G, Leandro G, Repici A, Testoni PA, Andriulli A. A multicentre randomised study of intrasphincteric botulinum toxin in patients with oesophageal achalasia. GISMAD Achalasia Study Group. Gut. 2000;46:597-600. [PubMed] |
| 19. | Pasricha PJ, Hawari R, Ahmed I, Chen J, Cotton PB, Hawes RH, Kalloo AN, Kantsevoy SV, Gostout CJ. Submucosal endoscopic esophageal myotomy: a novel experimental approach for the treatment of achalasia. Endoscopy. 2007;39:761-764. [PubMed] |
| 20. | Ling TS, Guo HM, Yang T, Peng CY, Zou XP, Shi RH. Effectiveness of peroral endoscopic myotomy in the treatment of achalasia: a pilot trial in Chinese Han population with a minimum of one-year follow-up. J Dig Dis. 2014;15:352-358. [PubMed] [DOI] [Full Text] |
| 21. | Li HK, Linghu EQ. New endoscopic classification of achalasia for selection of candidates for peroral endoscopic myotomy. World J Gastroenterol. 2013;19:556-560. [PubMed] [DOI] [Full Text] |
| 22. | Ren Z, Zhong Y, Zhou P, Xu M, Cai M, Li L, Shi Q, Yao L. Perioperative management and treatment for complications during and after peroral endoscopic myotomy (POEM) for esophageal achalasia (EA) (data from 119 cases). Surg Endosc. 2012;26:3267-3272. [PubMed] [DOI] [Full Text] |
| 23. | Zhai Y, Linghu E, Li H, Qin Z, Wang X, Du H, Meng J. [Comparison of peroral endoscopic myotomy with transverse entry incision versus longitudinal entry incision for achalasia]. Nan Fang Yi Ke Da Xue Xue Bao. 2013;33:1399-1402. [PubMed] |
| 24. | Zhou PH, Li QL, Yao LQ, Xu MD, Chen WF, Cai MY, Hu JW, Li L, Zhang YQ, Zhong YS. Peroral endoscopic remyotomy for failed Heller myotomy: a prospective single-center study. Endoscopy. 2013;45:161-166. [PubMed] [DOI] [Full Text] |
| 25. | Sharata A, Kurian AA, Dunst CM, Bhayani NH, Reavis KM, Swanström LL. Peroral endoscopic myotomy (POEM) is safe and effective in the setting of prior endoscopic intervention. J Gastrointest Surg. 2013;17:1188-1192. [PubMed] [DOI] [Full Text] |
| 26. | Von Renteln D, Fuchs KH, Fockens P, Bauerfeind P, Vassiliou MC, Werner YB, Fried G, Breithaupt W, Heinrich H, Bredenoord AJ. Peroral endoscopic myotomy for the treatment of achalasia: an international prospective multicenter study. Gastroenterology. 2013;145:309-11.e1-3. [PubMed] [DOI] [Full Text] |
| 27. | Smith CD, Stival A, Howell DL, Swafford V. Endoscopic therapy for achalasia before Heller myotomy results in worse outcomes than heller myotomy alone. Ann Surg. 2006;243:579-84; discussion 584-6. [PubMed] |
| 28. | Snyder CW, Burton RC, Brown LE, Kakade MS, Finan KR, Hawn MT. Multiple preoperative endoscopic interventions are associated with worse outcomes after laparoscopic Heller myotomy for achalasia. J Gastrointest Surg. 2009;13:2095-2103. [PubMed] [DOI] [Full Text] |
| 29. | Ling T, Guo H, Zou X. Effect of peroral endoscopic myotomy in achalasia patients with failure of prior pneumatic dilation: a prospective case-control study. J Gastroenterol Hepatol. 2014;29:1609-1613. [PubMed] [DOI] [Full Text] |
| 30. | Vigneswaran Y, Yetasook AK, Zhao JC, Denham W, Linn JG, Ujiki MB. Peroral endoscopic myotomy (POEM): feasible as reoperation following Heller myotomy. J Gastrointest Surg. 2014;18:1071-1076. [PubMed] |
| 31. | Yaghoobi M, Mikaeli J, Montazeri G, Nouri N, Sohrabi MR, Malekzadeh R. Correlation between clinical severity score and the lower esophageal sphincter relaxation pressure in idiopathic achalasia. Am J Gastroenterol. 2003;98:278-283. [PubMed] |
| 32. | Pandolfino JE, Fox MR, Bredenoord AJ, Kahrilas PJ. High-resolution manometry in clinical practice: utilizing pressure topography to classify oesophageal motility abnormalities. Neurogastroenterol Motil. 2009;21:796-806. [PubMed] [DOI] [Full Text] |
| 33. | Swanstrom LL, Kurian A, Dunst CM, Sharata A, Bhayani N, Rieder E. Long-term outcomes of an endoscopic myotomy for achalasia: the POEM procedure. Ann Surg. 2012;256:659-667. [PubMed] [DOI] [Full Text] |
| 34. | Verlaan T, Rohof WO, Bredenoord AJ, Eberl S, Rösch T, Fockens P. Effect of peroral endoscopic myotomy on esophagogastric junction physiology in patients with achalasia. Gastrointest Endosc. 2013;78:39-44. [PubMed] [DOI] [Full Text] |
| 35. | Logan MS, Vossoughi F, Watson CM, Amarnath R, Camps JI. A novel technique for the surgical treatment of achalasia in children: evaluated with postoperative esophageal manometry. J Laparoendosc Adv Surg Tech A. 2009;19:589-593. [PubMed] [DOI] [Full Text] |