Published online Apr 14, 2015. doi: 10.3748/wjg.v21.i14.4419
Peer-review started: October 28, 2014
First decision: November 14, 2014
Revised: December 14, 2014
Accepted: January 30, 2015
Article in press: January 30, 2015
Published online: April 14, 2015
Processing time: 170 Days and 10.4 Hours
A 20-year-old female patient presented with two masses located in the left liver. In this patient, a computed tomography (CT) scan revealed a hypodense mass and a second well-defined mass with a calcified nodule in the left hepatic lobe. No enhancements were apparent in or around the masses. A laparotomy was performed due to the patient’s symptoms, namely, the atypical CT findings and a risk of rupture of the subcapsular lesion. The operation revealed two masses in the left hepatic lobe and a left liver resection was subsequently performed. One of the masses involved segment III and the other mass was located in segment IV. The histopathologic findings supported a diagnosis of collagenous nodule mixed simple cyst and hemangioma. A diagnosis of collagenous nodule mixed simple hepatic cyst is extremely rare and radiologically mimics a teratoma, hepatolithiasis, parasitic cyst, or hemangioma. Although hepatic hemangiomas are the most common benign tumors found in the liver, the present case showed atypical radiographic features.
Core tip: This case represents a rare presentation of a patient with multiple liver masses. A definitive diagnosis depends on the histopathologic findings. Collagenous nodules are a rare clinicopathologic finding in the liver. This paper discusses the pathogenesis of a collagenous nodule found in the liver. Although hepatic hemangiomas are the most common benign tumor in the liver, this case showed atypical radiographic features.
- Citation: Zheng ZJ, Zhang S, Cao Y, Pu GC, Liu H. Collagenous nodule mixed simple cyst and hemangioma coexistence in the liver. World J Gastroenterol 2015; 21(14): 4419-4422
- URL: https://www.wjgnet.com/1007-9327/full/v21/i14/4419.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i14.4419
Collagenous nodule mixed simple hepatic cyst is an extremely rare mass that has not been reported previously in the publically available literature. Hyaline degeneration of the connective tissue is the predominant pathologic feature of a collagenous nodule. This form of degenerative alteration has been found in atrophic breast tissue, scar tissue, atheromatous plaques, and organized tissue. In contrast, hepatic hemangiomas are the most common benign tumor in the liver[1]. Diagnosis of a hepatic hemangioma is generally straightforward and accurately diagnosed by the various imaging modalities. The case described here, however, presented with atypical radiographic features. The diagnosis of hepatic hemangioma was considered due to the pathologic findings. Here, we present a case of hepatic hemangioma in conjunction with a collagenous nodule mixed simple hepatic cyst in a 20-year-old female patient.
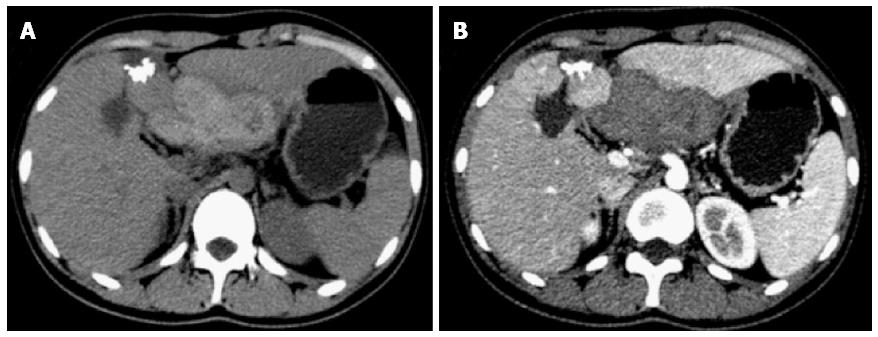
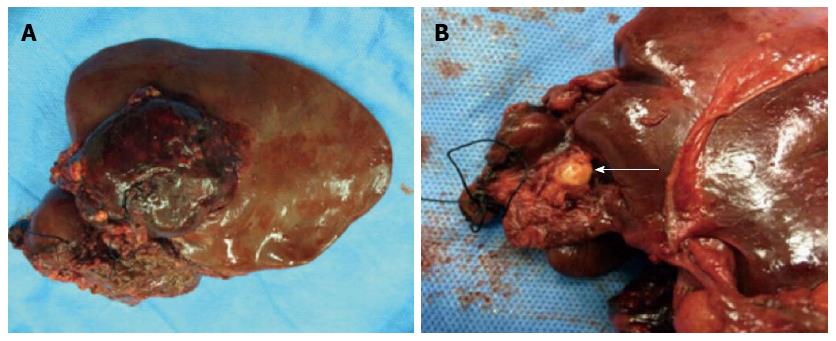
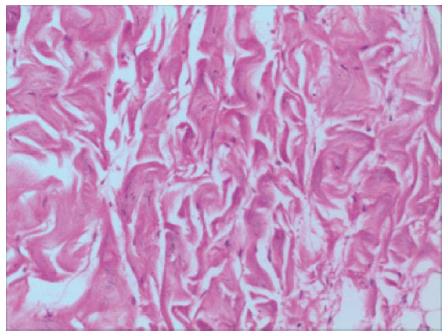
A 20-year-old female patient presented with a two-month history of recurrent right epigastric pain. She had no history of exposure to parasites. Serum alpha-fetoprotein and eosinophil levels were normal. Serological testing for hydatid antibody was negative. A computed tomography (CT) scan revealed a hypodense mass and a second well-defined mass with a calcified nodule in the left hepatic lobe. Enhancements were not apparent in or around the masses (Figure 1). The chief radiographic differential diagnosis included teratoma, hepatolithiasis, parasitic cyst, or hemangioma. Both the patient and her relatives consented to a laparotomy. The operation revealed two masses in the left hepatic lobe and a left liver resection was performed. One of the masses involved segment III and the other was localized to segment IV. The segment III mass was a tender, rufous and subcapsular mass (diameter: 9 cm), while the mass in segment IV was described as a cystic mass (diameter: 5 cm). A hard, gray-white, translucent, and inelastic nodule (diameter: 2 cm) was observed in the inner wall of the cystic mass (Figure 2, arrow). Histologically, the segment III mass had dilated vascular channels, fibrous stroma, and dark venous blood. The segment IV mass revealed thickened, banded and sheet-like collagenous fibers (Figure 3). No parasites were observed in the specimen obtained from the cystic mass. After a histopathologic analysis, the diagnosis of collagenous nodule mixed simple cyst and hemangioma was confirmed. The patient made an uneventful recovery.
Prior to surgery, high-density nodules were classified as hepatic calcifications. Bezerra et al[2] retrospectively analyzed 1362 consecutive CT scans of the abdomen and identified intrahepatic calcifications in 3.6% (49/1362) of the patients. Calcifications that develop within a hepatic mass are either produced by the tumor itself or, more commonly, represent dystrophic calcification secondary to necrosis and/or hemorrhage within the mass[3]. Calcifications may be found in inflammatory hepatic lesions and in benign and malignant liver masses[4]. The clinical appearance of a cystic mass with a high-density nodule is nonspecific and can mimic a teratoma, hepatolithiasis, parasitic cyst, or hemangioma. Although supporting evidence was lacking, a diagnosis of hepatic hydatidosis was primarily considered, as it is endemic in the Sichuan Province. The patient presented with no personal history of potential exposure to parasites, a normal level of eosinophils, and a negative hydatid antibody test. Thus, the patient underwent a left liver resection to avoid a misdiagnosis that may have potential deleterious consequences. A pathologic examination subsequently confirmed that the mass was a collagenous nodule mixed simple hepatic cyst, which has not been reported previously.
The predominant pathologic feature of a collagenous nodule is hyaline degeneration of connective tissue. This kind of degenerative alteration can be found in atrophic breast tissue, scar tissue, atheromatous plaques, and organized tissue. The cause of a collagenous nodule in a liver simple cyst is unclear. It is possible that the cyst was infected or bleeding, after which the pus or blood clot was replaced by granulation tissue, which is known as organization. This granulation tissue may then have been replaced by fibrous connective tissue. The process is analogous to wound healing and scar tissue formation. In this case, the collagenous nodule appeared as a high-density shadow on a CT scan. There are no specific radiologic features that differentiate a collagenous nodule from calcification. A definitive diagnosis is dependent on histopathologic findings. Had the diagnosis of a collagenous nodule mixed simple hepatic cyst been considered preoperatively, conservative observation may have been an option.
Cavernous hemangiomas are the most common benign tumor in the liver, with a reported incidence ranging from 1% to 20%[1]. This lesion occurs more frequently in women than in men. A hepatic hemangioma originates from the proliferation of vascular endothelial cells and enlarges by ectasia rather than hyperplasia[5]. Hemangiomas are usually detected incidentally while imaging for other purposes. The classic enhanced CT scan shows early peripheral enhancement of the mass, followed by centripetal fill-in of the contrast medium with persistent enhancement on delayed phase images[6]. In this case, the radiographic finding was atypical, with a lesion that showed a hypodense mass without enhancement. Slow flow in the central sinusoids, central fibrosis, central thrombosis, and hemorrhage may have contributed to the nonenhancement of the hemangioma[7]. Knowledge of the broad spectrum of atypical hepatic hemangiomas is critical and can help avoid most diagnostic errors[8]. Atypical hemangioma findings include a non-enhancing central core and septa (usually seen in large hemangiomas), calcification, fluid-fluid level, and multicystic hemangiomas[9]. Hepatic hemangiomas that are larger than 4 cm in diameter are classified as giant hemangiomas[10]. The surgical indications for liver hemangiomas are Kasabach-Merritt syndrome, symptoms of organ compression that have been well established (excluding other diseases), and traumatic or spontaneous rupture[11]. Asymptomatic or minimally symptomatic patients can be safely observed[12]. Previous studies have demonstrated that nonoperative management of a giant liver hemangioma is safe in most patients, indicating that the size of the lesion is not a criterion for surgery[13].
In conclusion, this case represents a rare presentation of a patient with multiple liver masses. Surgical resection was performed due to the symptoms, uncertain diagnosis as a result of atypical CT findings, and a risk of rupture of the subcapsular lesion. Liver resection is a safe procedure. In our case, the preoperative diagnosis remained uncertain, and the surgical resection was justified. The management of liver masses should be based on a balance between the risks that might be prevented by surgical resection and the estimated risks of surgery.
A 20-year-old female patient presented with a two-month history of recurrent right epigastric pain.
Tenderness in the upper abdomen.
Teratoma, hepatolithiasis, parasitic cyst, or hemangioma.
Serum alpha-fetoprotein and eosinophil levels were normal and serologic testing for hydatid antibody was negative.
A computed tomography scan revealed a hypodense mass and a second well-defined mass with a calcified nodule in the left hepatic lobe, without enhancements in or around either mass.
Histological examination revealed a collagenous nodule mixed simple cyst and a hepatic hemangioma.
A left liver resection was performed.
A collagenous nodule is a rare clinicopathologic characteristic of the liver. This paper discusses the pathogenesis of a collagenous nodule occurring in the liver. Although a hepatic hemangioma is the most common benign tumor of the liver, our case presented with atypical radiographic features.
The primary pathologic feature of a collagenous nodule is hyaline degeneration of connective tissue. This form of degenerative alteration can be found in atrophic breast tissue, scar tissue, atheromatous plaques, and organized tissue. The cause of a collagenous nodule in a liver simple cyst is unclear. It is possible that the cyst was infected or bleeding after which the pus or blood clot was replaced by granulation tissue, which is known as organization. This granulation tissue may then be replaced by fibrous connective tissue.
The diagnosis and treatment of atypical masses in the liver should depend on a histologic examination during surgery.
The article can be published due to the rarity of the three diseases at the same time. The surgical procedure has been performed well due to the difficulties of the diagnosis.
P- Reviewer: Di Carlo I S- Editor: Ma YJ L- Editor: Wang TQ E- Editor: Liu XM
| 1. | Gore RM, Newmark GM, Thakrar KH, Mehta UK, Berlin JW. Hepatic incidentalomas. Radiol Clin North Am. 2011;49:291-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 2. | Bezerra ASA, D’Ippolito G, Martelli P, Pinto GADH, Filho MMG, Szejnfeld J. Calcificações hepáticas: freqüência e significado. Radiol Bras. 2003;36:199-205. [RCA] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Scatarige JC, Fishman EK, Saksouk FA, Siegelman SS. Computed tomography of calcified liver masses. J Comput Assist Tomogr. 1983;7:83-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 45] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 4. | Stoupis C, Taylor HM, Paley MR, Buetow PC, Marre S, Baer HU, Vock P, Ros PR. The Rocky liver: radiologic-pathologic correlation of calcified hepatic masses. Radiographics. 1998;18:675-685; quiz 726. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 50] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 5. | Trastek VF, van Heerden JA, Sheedy PF, Adson MA. Cavernous hemangiomas of the liver: resect or observe? Am J Surg. 1983;145:49-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 108] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 6. | Moon HK, Kim HS, Heo GM, Shin WG, Kim KH, Jang MK, Lee JH, Kim HY, Kim DJ, Cho SJ. A case of pedunculated hepatic hemangioma mimicking submucosal tumor of the stomach. Korean J Hepatol. 2011;17:66-70. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 7. | Johnson CM, Sheedy PF, Stanson AW, Stephens DH, Hattery RR, Adson MA. Computed tomography and angiography of cavernous hemangiomas of the liver. Radiology. 1981;138:115-121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 63] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 8. | Vilgrain V, Boulos L, Vullierme MP, Denys A, Terris B, Menu Y. Imaging of atypical hemangiomas of the liver with pathologic correlation. Radiographics. 2000;20:379-397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 319] [Cited by in RCA: 257] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 9. | Cha EY, Kim KW, Choi YJ, Song JS, Cho KJ, Lee MG. Multicystic cavernous haemangioma of the liver: ultrasonography, CT, MR appearances and pathological correlation. Br J Radiol. 2008;81:e37-e39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 10. | Adam YG, Huvos AG, Fortner JG. Giant hemangiomas of the liver. Ann Surg. 1970;172:239-245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 161] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 11. | Toro A, Mahfouz AE, Ardiri A, Malaguarnera M, Malaguarnera G, Loria F, Bertino G, Di Carlo I. What is changing in indications and treatment of hepatic hemangiomas. A review. Ann Hepatol. 2014;13:327-339. [PubMed] |
| 12. | Yoon SS, Charny CK, Fong Y, Jarnagin WR, Schwartz LH, Blumgart LH, DeMatteo RP. Diagnosis, management, and outcomes of 115 patients with hepatic hemangioma. J Am Coll Surg. 2003;197:392-402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 133] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 13. | Schnelldorfer T, Ware AL, Smoot R, Schleck CD, Harmsen WS, Nagorney DM. Management of giant hemangioma of the liver: resection versus observation. J Am Coll Surg. 2010;211:724-730. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 104] [Article Influence: 6.9] [Reference Citation Analysis (0)] |