Published online Sep 28, 2014. doi: 10.3748/wjg.v20.i36.13200
Revised: May 9, 2014
Accepted: June 13, 2014
Published online: September 28, 2014
Processing time: 188 Days and 10.7 Hours
Surgery such as digestive tract reconstruction is usually required for pancreatic trauma and severe pancreatitis as well as malignant pancreatic lesions. The most common digestive tract reconstruction techniques (e.g., Child’s type reconstruction) for neoplastic diseases of the pancreatic head often encompass pancreaticojejunostomy, choledochojejunostomy and then gastrojejunostomy with pancreaticoduodenectomy, whereas these techniques may not be applicable in benign pancreatic diseases due to an integrated stomach and duodenum in these patients. In benign pancreatic diseases, the aforementioned reconstruction will not only increase the distance between the pancreaticojejunostomy and choledochojejunostomy, but also the risks of traction, twisting and angularity of the jejunal loop. In addition, postoperative complications such as mixed fistula are refractory and life-threatening after common reconstruction procedures. We here introduce a novel pancreaticojejunostomy, hepaticojejunostomy and double Roux-en-Y digestive tract reconstruction in two cases of benign pancreatic disease, thus decreasing not only the distance between the pancreaticojejunostomy and choledochojejunostomy, but also the possibility of postoperative complications compared to common reconstruction methods. Postoperatively, the recovery of these patients was uneventful and complications such as bile leakage, pancreatic leakage and digestive tract obstruction were not observed during the follow-up period.
Core tip: In most cases, digestive tract reconstruction is essential for pancreatic trauma and severe pancreatitis as well as malignant pancreatic lesions. Digestive tract reconstruction used for neoplastic diseases of the pancreas is not applicable in benign pancreatic diseases due to an integrated stomach and duodenum in these patients. In benign pancreatic diseases, the aforementioned reconstruction methods increase not only the distance between the pancreaticojejunostomy and choledochojejunostomy, but also the risks of traction, twisting and angularity of the jejunal loop. Furthermore, postoperative complications such as mixed fistula are refractory and life-threatening. Therefore, we introduced a novel pancreaticojejunostomy, hepaticojejunostomy and double Roux-en-Y digestive tract reconstruction in two cases of benign pancreatic diseases in order to reduce the risk of postoperative complications. This type of reconstruction may be an alternative treatment modality for benign pancreatic diseases.
- Citation: Jia CK, Lu XF, Yang QZ, Weng J, Chen YK, Fu Y. Pancreaticojejunostomy, hepaticojejunostomy and double Roux-en-Y digestive tract reconstruction for benign pancreatic diseases. World J Gastroenterol 2014; 20(36): 13200-13204
- URL: https://www.wjgnet.com/1007-9327/full/v20/i36/13200.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i36.13200
Pancreatic trauma and pancreatitis are common benign pancreatic diseases. Pancreatic trauma may result in pancreatic duct fracture or severe pancreatic head damage in combination with duodenal and biliary duct damage. Severe pancreatitis has long-term complications such as pancreatic leakage, pseudocyst, bile leakage, biliary obstruction and intestinal fistula. Therefore, surgery is usually needed for both pancreatic trauma and severe pancreatitis[1,2]. In most cases, digestive tract reconstruction is essential for pancreatic trauma and severe pancreatitis as well as malignant pancreatic lesions. Digestive tract reconstruction for neoplastic diseases of the pancreas often encompasses pancreaticojejunostomy, choledochojejunostomy and then gastrojejunostomy under the circumstance of pancreaticoduodenectomy[3], whereas these techniques may not be applicable in benign pancreatic diseases due to an integrated stomach and duodenum in these patients. In benign pancreatic diseases, the aforementioned reconstruction will not only increase the distance between the pancreaticojejunostomy and choledochojejunostomy, but also the risks of traction, twisting and angularity of the jejunal loop[4,5]. In addition, postoperative complications such as mixed fistula, which can be explained by the enzyme activation theory, are refractory and life-threatening. For instance, in Child’s type reconstruction, which is one of the most common reconstruction methods performed, the hepatojejunostomy site is several centimeters distal to the pancreaticojejunostomy site. Once leakage develops at the hepatojejunostomy site, the presence of pancreatic juice will exacerbate the leakage[3]. We herein introduce a novel pancreaticojejunostomy, hepaticojejunostomy and double Roux-en-Y digestive tract reconstruction based on a retrospective analysis of two patients with benign pancreatic disease.
A 64-year-old male patient was admitted to a local hospital because of epigastric pain and fever on October 10, 2011. The diagnosis of acute pancreatitis was made. Epigastric pain was relieved after fasting, nasogastric decompression, and inhibition of pancreatic enzymes. However, repeated fever, with the highest body temperature of 39.6 °C, was not well controlled. The patient was then transferred to our department for further treatment on October 25, 2011. On the day of admission, computed tomography (CT) scan showed a swollen gallbladder, dilated common bile duct, and necrosis in the pancreatic head and uncinate process with a peripancreatic abscess. Ultrasound B-guided abscess paracentesis and drainage were immediately performed. Approximately 100 mL/d of brown liquid and necrotic tissues were drained. The amylase content in the drained liquid was 5938 U/L. Fever was relieved after drainage. On day 2 after admission, a nasojejunal tube was catheterized and enteral nutrition was administered. Both epigastric pain and fever were significantly improved. However, shaking chills and high fever (40 °C) reappeared on day 5 after admission. Laboratory examination showed WBC counts of 20.11 × 109/L [normal range (NR): 4 × 109/L-10 × 109/L] and PLT counts of 449 × 109/L (NR: 100 × 109/L-300 × 109/L). Serum total bilirubin increased progressively from 23.4 μmol/L (NR: 1.7-20 μmol/L) at admission to 169.59 μmol/L on day 5 after admission and direct bilirubin was 136.74 μmol/L (NR: 0-6 μmol/L). CT scan was performed again which showed that gallbladder swelling and common bile duct dilation were more obvious than observed previously. The abscess in the pancreatic head and uncinate process shrank after drainage. However, the abscess in the pancreatic body did not shrink and a gas bubble was seen in the pancreatic bed. Therefore, the diagnoses of severe pancreatitis and acute suppurative obstructive cholangitis were made. Endoscopic retrograde cholangiopancreatography was performed, but failed due to duodenum deformation and duodenal papilla dislocation. Therefore, laparotomy was performed on November 1, 2011. Cholecystectomy, debridement and necrosectomy, T-tube drainage of the common bile duct, lesser omental cavity and pancreatic bed drainage were carried out. Postoperatively, the patient recovered well and his parameters on routine blood analysis and liver function gradually returned to normal.
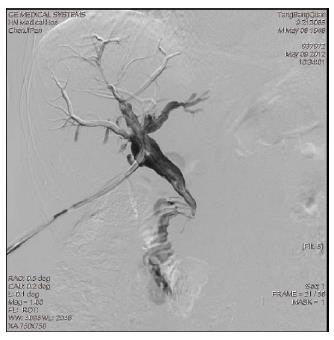
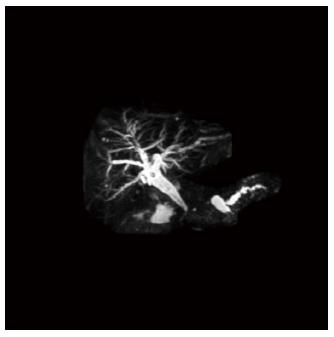
Lower segment stricture of the common bile duct and choledochoduodenal fistula were detected by T-tube cholangiography on day 50 and 6 mo after operation, respectively (Figure 1). Magnetic resonance cholangiopancreatography showed discontinuity of the pancreatic duct 6 mo after operation. The duct in the pancreatic head and neck was not detected and pancreatic leakage from the proximal duct of the pancreatic body and dilation of the distal duct of the pancreatic body and tail were not observed (Figures 2, 3). One hundred to three hundred milliliters of abdominal collection per day were drained after debridement and necrosectomy. Amylase content in the collection drained from the pancreatic bed was continuously higher than the NR.
To resolve the pancreatic leakage, lower segment stricture of the common bile duct and choledochoduodenal fistula, the patient underwent a second laparotomy on May 16, 2012. Intraoperative findings verified the preoperative diagnosis of upper segment dilation of the common bile duct, choledochoduodenal fistula, absence of normal pancreatic tissues in the pancreatic head and neck due to necrosis, and a pseudocyst communicating to the pancreatic bed drainage tube in the proximal duct of the pancreatic body. The common hepatic duct and common bile duct were isolated. The upper segment of the common bile duct was resected and its lower segment was closed superior to the first portion of the duodenum. The proximal pancreatic body and pseudocyst were isolated and resected. Fifteen centimeters of the jejunum to the Treitz ligament was transected with side closures. A retrocolic end-to-side pancreaticojejunostomy was then performed using a distal jejunal limb. A proximal jejunal limb was prepared for the Roux-en-Y side-to-side enteroenterostomy. Because this patient had an intact and integrated stomach and duodenum, common procedure of digestive tract reconstruction increased the distance between the pancreaticojejunostomy and hepaticojejunostomy and the risks of intestinal twisting or angulation. Therefore, at 20 cm distal to the pancreaticojejunostomy, the jejunum was interrupted with side closures. Then an antecolic end-to-side hepaticojejunostomy was performed using a distal jejunal limb. The first enteroenterostomy was then performed 20 cm from the hepaticojejunostomy using a distal jejunal limb to the pancreaticojejunostomy and the second enteroenterostomy was performed 20 cm from the first enteroenterostomy using a distal jejunal limb to the Treitz ligament. Thus, the pancreaticojejunostomy, hepaticojejunostomy and double Roux-en-Y digestive tract reconstruction was completed (Figure 4). Postoperatively, recovery of this patient was uneventful and complications such as bile leakage, pancreatic leakage and digestive tract obstruction were not observed during the follow-up period. Routine blood parameters and liver function were normal.
A 54-year-old male patient was hospitalized due to acute upper abdominal pain and vomiting for 4 h following an attack with a piece of steel tube on May 23, 2011. Physical examination showed board-like rigidity of the abdomen accompanied by whole abdominal tenderness and rebound tenderness, especially at the upper abdomen. Extracted blood failed to coagulate after abdominal paracentesis. A CT examination indicated pancreatic trauma, pancreatic head and neck bleeding and possible duodenal injury. Emergent laparotomy was performed and intra-abdominal hemorrhage and retroperitoneal hematoma were found. Extensive hematoma was found within the pancreatic neck capsule and the right lateral duodenum. Furthermore, contusion and laceration of the pancreas neck accompanied by pancreatic duct damage and leakage of pancreatic juice were observed. A 1.8 cm long longitudinal laceration in front of the descending part of the duodenum with slight active bleeding at the edge and intestinal juice leakage were found. The pancreas neck was resected and the end of the pancreatic head was closed. The laceration at the descending part of the duodenum was double-stitched. To decrease the liquid flow and pressure in the duodenal lumen, the common bile duct was transected and closed at its distal end. Then pancreaticojejunostomy, hepaticojejunostomy and double Roux-en-Y digestive tract reconstruction was performed as outlined in Case 1. A piece of gastric tube was then placed in the descending part of the duodenum for decompression and another two pieces of abdominal drainage tube were applied. The patient recovered well after the operation without bile leakage, pancreatic leakage and digestive tract obstruction during the follow-up period.
Surgery is usually required for both pancreatic trauma and severe pancreatitis[1,2]. It is difficult to select the optimal treatment for the bile duct or duodenum involved in benign pancreatic diseases, in which digestive tract reconstruction is required[6,7]. A common digestive tract reconstruction technique such as Child’s type reconstruction may not be applicable in benign pancreatic diseases due to an integrated stomach and duodenum in these patients. The two benign cases of pancreatic disease reported here were complicated with biliary tract stricture, choledochoduodenal fistula or duodenal injury, respectively. To resolve these aforementioned complications, we performed pancreaticojejunostomy, hepaticojejunostomy and double Roux-en-Y digestive tract reconstruction to decrease the liquid flow and pressure in the duodenal lumen and reduce not only the distance between the pancreaticojejunostomy and choledochojejunostomy, but also the risks of traction, twisting and angularity of the jejunal loop associated with common reconstruction methods. A retrocolic end-to-side pancreaticojejunostomy and antecolic end-to-side hepaticojejunostomy were performed followed by two Y-type reconstructions of the jejunum (enteroenterostomies). The distance between the pancreaticojejunostomy and second enteroenterostomy (15 cm distal to the Treitz ligament) and the distance between the hepaticojejunostomy and second enteroenterostomy were at least 40 cm. Surgical planning and anastomosis were in accordance with the principle of Roux-en-Y digestive tract reconstruction.
Postoperative complications such as mixed digestive juice leakage, which can be explained by the enzyme activation theory, are refractory and life-threatening. Pancreatic anastomotic leaks are a major cause of morbidity and mortality following pancreaticoduodenectomy, and no single reconstruction technique has been shown to be superior[3,8]. In Child’s type reconstruction, which is one of the most common reconstruction methods performed, the hepatojejunostomy site is several centimeters distal to the pancreaticojejunostomy site. Once leakage develops at the pancreaticoduodenectomy site, the presence of bile will exacerbate the pancreatic leakage. In addition, when leakage develops at the hepatojejunostomy site, the presence of pancreatic juice will exacerbate the bile leakage[3]. Therefore, the safest type of anastomosis is the one in which the mixture of pancreatic and biliary enzymes is contained, such as in a jejunojejunostomy[9,10].
The separated loop method for pancreaticojejunostomy and hepatojejunostomy introduced in this study prevented critical complications such as mixed digestive juice leakage. The results demonstrated that complex digestive tract reconstruction did not increase the occurrence of complications when the anastomosis was in accordance with the principle of Roux-en-Y digestive tract reconstruction. Postoperatively, both patients had an uneventful recovery, and complications such as bile leakage, pancreatic leakage and digestive tract obstruction were not observed during the follow-up period. There are very few detailed reports on double Roux-en-Y digestive tract reconstruction and this technique may be an alternative treatment modality for benign pancreatic diseases.
Two male patients aged 64 years and 54 years were hospitalized due to acute pancreatitis and pancreatic trauma, respectively.
Clinical symptoms and auxiliary examinations were comprehensively used for clinical diagnosis; severe pancreatitis and acute suppurative obstructive cholangitis in case 1, and pancreatic trauma, pancreatic head and neck bleeding and possible duodenal injury in case 2.
Acute cholecystitis, perforation of the upper digestive tract, acute ileus, pancreatic trauma and spleen trauma.
The amylase content in drained liquid was 5938 U/L in case 1. WBC 20.11 × 109/L; serum total bilirubin increased progressively from 23.4 μmol/L at admission to 169.59 μmol/L on day 5 after admission. Extracted blood failed to coagulate after abdominal paracentesis in case 2.
On the day of admission, computed tomography (CT) scans showed a swollen gallbladder, dilated common bile duct, and necrosis in the pancreatic head and uncinate process with a peripancreatic abscess in case 1. The CT examination indicated pancreatic trauma, pancreatic head and neck bleeding and possible duodenal injury in case 2.
Both patients underwent a novel pancreaticojejunostomy, hepaticojejunostomy and double Roux-en-Y digestive tract reconstruction.
Pancreaticojejunostomy, hepaticojejunostomy and double Roux-en-Y digestive tract reconstruction may be an alternative treatment modality for benign pancreatic diseases in order to reduce the risk of postoperative complications.
Authors performed a novel pancreaticojejunostomy, hepaticojejunostomy and double Roux-en-Y digestive tract reconstruction in two patients with benign pancreatic disease, which decreased not only the distance between the pancreaticojejunostomy and choledochojejunostomy, but also the possibility of postoperative complications compared with the common reconstruction methods.
The authors present two cases treated with a modified surgical technique for non-malignant pancreatic diseases.
P- Reviewer: Camara-Lemarroy CR S- Editor: Ma YJ L- Editor: A E- Editor: Du P
| 1. | Hamidian Jahromi A, D’Agostino HR, Zibari GB, Chu QD, Clark C, Shokouh-Amiri H. Surgical versus nonsurgical management of traumatic major pancreatic duct transection: institutional experience and review of the literature. Pancreas. 2013;42:76-87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 26] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 2. | Behrns KE, Ben-David K. Surgical therapy of pancreatic pseudocysts. J Gastrointest Surg. 2008;12:2231-2239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 35] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 3. | Osada S, Imai H, Sasaki Y, Tanaka Y, Nonaka K, Yoshida K. Reconstruction method after pancreaticoduodenectomy. Idea to prevent serious complications. JOP. 2012;13:1-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 4. | Fragulidis GP, Arkadopoulos N, Vassiliou I, Marinis A, Theodosopoulos T, Stafyla V, Kyriazi M, Karapanos K, Dafnios N, Polydorou A. Pancreatic leakage after pancreaticoduodenectomy: the impact of the isolated jejunal loop length and anastomotic technique of the pancreatic stump. Pancreas. 2009;38:e177-e182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Doi R, Fujimoto K, Kobayashi H, Imamura M. Impact of reconstruction methods on outcome of pancreatoduodenectomy in pancreatic cancer patients. World J Surg. 2005;29:500-504. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Feng XF, Fan W, Shi CX, Li JH, Liu J, Liu ZH. Simplified pancreatoduodenectomy for complex blunt pancreaticoduodenal injury. Chin J Traumatol. 2013;16:311-313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 7. | Isaji S, Kawarada Y. Pancreatic head resection with second-portion duodenectomy for benign lesions, low-grade malignancies, and early stage carcinomas involving the pancreatic head region. Am J Surg. 2001;181:172-176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 25] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Kaman L, Sanyal S, Behera A, Singh R, Katariya RN. Isolated roux loop pancreaticojejunostomy vs single loop pancreaticojejunostomy after pancreaticoduodenectomy. Int J Surg. 2008;6:306-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 41] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 9. | Osada S, Imai H, Okumura N, Tokuyama Y, Hosono Y, Sakashita F, Sugiyama Y. A modified reconstruction method to prevent critical complications after pancreatoduodenectomy. Hepatogastroenterology. 2006;53:296-300. [PubMed] |
| 10. | Osada S, Sanada Y, Tanaka Y, Ikawa A, Tokuyama Y, Okumura N, Hosono Y, Nonaka K, Takahashi T, Yamaguchi K. Clinical evaluation of modified reconstruction method after pancreatoduodenectomy. Hepatogastroenterology. 2009;56:619-623. [PubMed] |