Published online Sep 21, 2014. doi: 10.3748/wjg.v20.i35.12662
Revised: May 18, 2014
Accepted: June 14, 2014
Published online: September 21, 2014
Processing time: 184 Days and 21 Hours
Liver test abnormalities have been described in up to 60% of patients with systemic lupus erythematodes (SLE) at some point during the course of their disease. Prior treatment with potentially hepatotoxic drugs or viral hepatitis is commonly considered to be the main cause of liver disease in SLE patients. However, in rare cases elevated liver enzymes may be due to concurrent autoimmune hepatitis (AIH). To distinguish whether the patient has primary liver disease with associated autoimmune clinical and laboratory features resembling SLE - such as AIH - or the elevation of liver enzymes is a manifestation of SLE remains a difficult challenge for the treating physician. Here, we present six female patients with complex autoimmune disorders and hepatitis. Patient charts were reviewed in order to investigate the complex relationship between SLE and AIH. All patients had coexisting autoimmune disease in their medical history. At the time of diagnosis of AIH, patients presented with arthralgia, abdominal complaints, cutaneous involvement and fatigue as common symptoms. All patients fulfilled the current diagnostic criteria of both, AIH and SLE. Remission of acute hepatitis was achieved in all cases after the initiation of immunosuppressive therapy. In addition to this case study a literature review was conducted.
Core tip: Hepatic involvement in patients with systemic lupus erythematodes (SLE) is considered to be rare. The differences between hepatic involvement caused by hepatotoxic drugs, coincident viral hepatitis, non-alcoholic fatty liver disease or concurrent autoimmune hepatitis (AIH) as independent disease has not been defined clearly in patients with SLE. This case report describes six patients who fulfill the current diagnostic criteria for both SLE and AIH, and thus represents the largest case series in the literature.
- Citation: Beisel C, Weiler-Normann C, Teufel A, Lohse AW. Association of autoimmune hepatitis and systemic lupus erythematodes: A case series and review of the literature. World J Gastroenterol 2014; 20(35): 12662-12667
- URL: https://www.wjgnet.com/1007-9327/full/v20/i35/12662.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i35.12662
Systemic lupus erythematodes (SLE) is a multisystem autoimmune disorder involving various organs such as kidneys, skin and the central nervous system. Liver involvement is normally not part of the spectrum of SLE, but is seen in up to 60% of SLE patients[1]. Hepatotoxic drugs, coincident viral hepatitis and non-alcoholic fatty liver disease (often induced by steroids) are the most commonly described causes of elevated liver enzymes in SLE[2].
The co-occurrence of autoimmune hepatitis (AIH) and SLE is considered to be rare and only few case reports have been published so far (Table 1). Diagnostic criteria in accordance with the International Autoimmune Hepatitis Group and the “simplified criteria” are based on elevation of Immunglobulin G (IgG), demonstration of characteristic autoantibodies, histological features of hepatitis and the absence of viral disease[3,4]. The clinical presentation of AIH ranges from asymptomatic disease recognized only by incidentally ascertained biochemical abnormalities to an acute or even fulminant hepatitis. Female predominance and occurrence peaks in early adult life and in the 4th decade of life are characteristic[5]. In symptomatic cases patients are often affected by non-specific symptoms such as nausea, anorexia, abdominal discomfort and jaundice. A common extrahepatic manifestation of AIH may be arthralgias, which are also often seen in SLE.
| Author | Year of publication | Patients (n) | Sex | Age(in year) | Clinical presentation | Liver enzymes | Outcome |
| Chattopadhyay et al[15] | 2011 | 1 | Female | 20 | Fever, polyarthritis, jaundice | Elevated | Remission |
| Choi et al[16] | 2008 | 1 | Female | Unknown | Butterfly-type facial erythema | Elevated | Remission |
| Chowdhary et al[8] | 2008 | 6 | Unknown | Unknown | Unknown | Unknown | Unknown |
| Deen et al[17] | 2009 | 4 | 3 female 1 male | Median 11 Range 11-13 | Jaundice, splenomegaly, cutaneous involvement, articular involvement, proteinuria (> 0.5 g/d), cardiopulmonary involvement | Elevated | Remission in all cases |
| Efe et al[18] | 2011 | 4 | Female | Median 35 | Unknown | Elevated | Unknown |
| Range 27-40 | |||||||
| Iwai et al[19] | 2003 | 1 | Female | 60 | Elevated liver enzymes | Elevated | Remission |
| Kaw et al[20] | 2006 | 1 | Female | 34 | Arthralgia, myalgias, skin rash, nausea | Elevated | Remission |
| Kooy et al[21] | 1996 | 1 | Unknown | Unknown | Unknown | Elevated | Remission |
| Koshy et al[22] | 2012 | 1 | Female | 30 | Jaundice, abdominal distention | Elevated | Exitus letalis1 |
| Mackay et al[11] | 1999 | 1 | Female | 16 | Failure to thrive, jaundice, non-erosive arthritis, oral aftous lesions | Elevated | Progress |
| Moriwaki et al[23] | 1987 | 1 | Unknown | Unknown | Unknown | Unknown | Unknown |
| Satoh et al[24] | 1997 | 2 | Unknown | Unknown | Unknown | Unknown | Remission |
| Suzuki et al[25] | 1993 | 1 | Female | 33 | Intermittend fever, polyarthralgia, cutaneous involvement, pericardial effusion | Elevated | Remission |
| Takahashi et al[26] | 2007 | 1 | Female | 69 | Fever, cough, pleural and pericardial effusion | Elevated | Remission |
| Tojo et al[27] | 2004 | 5 | Female | Median 43 | Raynaud’s phenomenon, arthralgia, butterfly-type facial erythema, dry mouth, jaundice, edema, ascites, pleural effusion, struma, skin ulcer, fatigue, fever | Elevated in 4 of 5 cases | Remission in all cases |
| Range 21-56 | |||||||
| Usta et al[28] | 2007 | 1 | Female | 12 | Jaundice, hepatosplenomegaly, polyarthralgia, malaise, butterfly-type facial erythema, arthritis | Elevated | Stable |
| Yamasaki et al[29] | 2004 | 1 | Female | 48 | Ascites | Elevated | Remission |
| Yoon et al[30] | 2003 | 2 | Female | Unknown | Unknown | Elevated | Unknown |
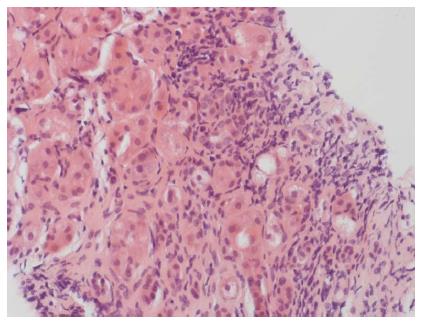
A patient with SLE and elevated liver enzymes presents a demanding differential diagnosis for the rheumatologist. While elevated IgG and anti-nuclear antibodies (ANAs) are characteristic for both AIH and SLE[5], there are few serological markers, which are highly specific for the two different diseases. Anti-double stranded DNA (anti-dsDNA) antibodies are associated with SLE but are also found in patients suffering from AIH[6]. Data on sensitivity for the diagnosis of SLE range from 25%-85%[7]. Czaja et al[6] tested sera from 53 patients with AIH by enzyme immunosorbent assay and indirect immunofluorescence using the Crithidia luciliae substrate and detected anti-dsDNA in 30 patients (57%). Also anti-Smith antibodies are frequently found in SLE patients and approximately 99% of individuals with positive anti-SM match the diagnostic criteria for SLE[7]. Specific markers for AIH, which usually do not occur in SLE, are soluble liver antigen (SLA), Liver-pancreas, smooth-muscle antibody (SMA) with specificity for F-actin and microsomal autoantigens, such as anti-liver kidney antibodies (anti-LKM antibody)[5]. While these markers may help to segregate AIH coincident with SLE serologically, liver histopathology represents the key feature that distinguishes AIH in SLE from nonspecific hepatic involvement in SLE. In patients with AIH liver histopathology shows characteristic lesions, such as interface hepatitis, rosetting of hepatocytes, emperipolesis and - consecutive to inflammation - fibrosis (Figure 1)[5]. In contrast, liver histology in SLE usually shows changes attributable either to drug toxicity or non-specific liver involvement as e.g., fatty degeneration or hydropic hepatocytes[2,8].
As the diagnosis of AIH is relevant in SLE patients with regards to choices of immunosuppressants, long-term outcome and optimal surveillance of the patients, adequate attention should be taken to differentiate between “true additional” AIH or non-specific liver involvement.
In the following, we present six patients with SLE and the concomitant diagnosis of autoimmune hepatitis. All patients matched the current diagnostic criteria of both AIH as well as of SLE. A review of the literature was performed and published cases were summarized (Table 1).
Six female patients with arthralgias, elevated transaminases and additional symptoms were seen either at the I. Department of Medicine of the University-Medical Center Hamburg-Eppendorf or at the Johannes Gutenberg University Hospital Mainz, Germany, between 1991 and 2011. The median age at presentation was 44 years (range: 27-60 years). All patients presented with arthralgia (n = 6) as main complaint at time of diagnosis. Abdominal complaints (n = 4), cutaneous involvement (n = 4) and fatigue (n = 4) were the second most common symptoms. Jaundice (n = 1), fever (n = 1), photosensitivity (n = 1), sicca symptoms (n = 1) and myalgia (n = 1) were less often described. All patients presented with elevated liver enzymes (AST median: 238.5 U/L, range: 59-323 U/L; ALT median: 174.5 U/L, range: 53-413 U/L). Five of six showed increased levels of IgG (median 24.15 g/L; range 6.7-44 g/L) and ANA titers with a homogeneous pattern on immuno fluorescence diagnostics, (median 1:960, range 1:160-1:2560) (Table 2).
| Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 | |
| Demographic data | ||||||
| Age at time of diagnosis (yr) | 43 | 59 | 40 | 60 | 27 | 45 |
| Sex | Female | Female | Female | Female | Female | Female |
| Year of diagnosis | 2012 | 2003 | 2006 | 2001 | 1994 (SLE) | 1991 |
| 2005 (AIH) | ||||||
| Laboratory tests | ||||||
| Hemoglobin (g/dL) | 10.7 | NA | NA | 14.7 | 13 | 13.4 |
| Leukocytes (/μL) | 0.7 | NA | NA | 8.9 | 4.84 | 8.7 |
| Platelets (/μL) | 21 | NA | NA | 291 | 232 | 181 |
| AST (U/L) | 316 | 170 | 59 | 307 | 125 | 323 |
| ALT (U/L) | 99 | 164 | 53 | 298 | 185 | 413 |
| Total bilirubin (mg/dL) | 8.9 | 1 | 1.8 | 0.83 | 0.9 | 4.1 |
| IgG (g/L) | 44 | 19.3 | 6.77 | 10.13 | 29 | 29 |
| C3 (mg/dL) | 4.1 | Normal | Low | NA | 0.14 | NA |
| C4 (mg/dL) | 4.1 | Normal | Low | NA | 0.14 | NA |
| ANA, homogeneous pattern (titer) | 1:2560 | 1:320 | 1:640 | 1:1280 | 1:160 | 1:1280 |
| SMA (titer) | 1:2380 | 1:320 | Negative | 1:60 | 1:160 | Negative |
| Anti-dsDNA (units) | 39 | 941 | Negative | Negative | 37 | > 200 |
| RNP-Sm (immunoblot) | NA | Positive | NA | NA | Positive | NA |
| Liver biopsy (Grading/staging1) | Cirrhosis (G2/F4) | Cirrhosis (G1/F4) | Cirrhosis (G3/F4) | Fibrosis (G1/F3) | Fibrosis (G2/F1) | Fibrosis (G3/F3) |
| Chronic hepatitis | Chronic hepatitis | Chronic hepatitis | Chronic hepatitis | Chronic hepatitis | Chronic hepatitis | |
| NASH | PSC | |||||
| Clinical symptoms of SLE | Arthritis | Arthritis | Arthritis | Arthritis | Arthritis | Arthtitis |
| Photosensitivity | Malar rash | Malar rash | Malar rash | |||
| Oral ulcers | ||||||
| Serositis | ||||||
| Therapy regime | Prednisolone | Prednisolone | Prednisolone | Prednisolone | Prednisolone | Prednisolone |
| Azathioprine | MMF | Azathioprine | Azathioprine | Azathioprine | Azathioprine | |
| Hydroxychloroquine | Hydroxychloroquine | Hydroxychloroquine | Cyclophosphamide | |||
| Cyclophosphamide | ||||||
| Course of disease | Remission | Remission | Remission | Remission | Remission | Remission |
| Diagnosis of HCC in 2012 |
While all patients tested negative for anti-LKM-1 as well as SLA/LP antibody, three patients tested positive for SMA. Four patients showed positive anti-dsDNA titers, only one patient tested positive for anti-Sm antibody (case 4).
Five of six patients had a history of Hashimoto’s thyroiditis as coexisting autoimmune disease. Other concomitant autoimmune disorders like primary sclerosing cholangitis, psoriasis and Raynaud’s phenomenon occurred in one patient respectively.
The diagnosis of SLE was established based on the American College of Rheumatology (ACR) classification criteria[3,9]. All patients fulfilled the simplified diagnostic criteria of AIH with a median score of 8 points (range 6-8 points)[4].
Liver biopsy was performed due to elevated transaminases in all cases and showed typical signs of AIH (Figure 1). Advanced fibrosis/cirrhosis was found in three patients.
Treatment was initiated in all cases with prednisolone pulse-therapy[10] and extended to a combination of azathioprine and hydroxychloroquine in four cases. A monotherapy with azathioprine or mycophenolate mofetil after prednisolone pulse-therapy was started in one patient, respectively. Two patients required a change of treatment due to azathioprine intolerance and switched to treatment with cyclophosphamide. Remission of acute hepatitis was achieved in all cases. Complete biochemical remission including normalization of transaminases as well as IgG levels was achieved in all patients after six months of treatment.
One patient (case 3) developed hepatocellular carcinoma (HCC) in 2012, six years after diagnosis of AIH. In her first liver biopsy in 2006, the patient showed liver cirrhosis. The patient was regularly seen at the outpatient clinic for follow-up visits and ultrasound screening for HCC was performed every six month. Multifocal HCC (barcelona clinic liver cancer-stadium C) was diagnosed six years after diagnosis of AIH. Surgical resection or liver transplantation as curative treatment option was not feasible due to advanced tumor stage. The patient underwent transcatheter arterial chemoembolization every three month. Since July 2013, the patient receives additionally systemic therapy with sorafenib due to tumor progression. Information of patient characteristics is given in Table 2.
Hepatic involvement in patients with SLE is well documented, but considered to be rare[11]. The differences between hepatic involvement caused by hepatotoxic drugs, coincident viral hepatitis, non-alcoholic fatty liver disease or concurrent AIH as independent disease has not been defined clearly in patients with SLE.
In this case series, we present six patients who fulfill the current diagnostic criteria for both SLE and AIH[3,9]. Interestingly, these patients presented with clinical and serological symptoms suggestive for AIH and liver disease was the leading disease in five of our patients. In addition to symptoms suggestive for AIH, the patients had distinctive features of SLE, supporting the interpretation of coexistence of the two conditions.
To our knowledge, only 35 cases of patients with the concurrent diagnosis of SLE and AIH have been published altogether (Table 1).
AIH and SLE are considered distinct diseases, which can be associated like other autoimmune diseases. This is supported by the fact, that five of our six patients had coexisting autoimmune disorders, as e.g., Hashimoto’s thyroiditis.
Differential diagnosis of elevated liver enzymes in patients with SLE as non-specific hepatic involvement or as AIH is demanding. While serological markers, such as ANA, anti-dsDNA or raised IgG can be strongly overlapping in SLE and AIH, histology is all the more essential to distinguish AIH in SLE from non-specific hepatic involvement in SLE. In accordance with the revised simplified criteria of AIH, histological demonstration of hepatitis compatible with AIH[12] is the essential diagnostic criterion of AIH[3,5]. We suggest that AIH needs to be considered in the differential diagnosis of any SLE patient with elevated liver enzymes. Liver biopsy is therefore crucial in these patients.
Treatment strategies are determined by the predominant disease, which in our case series was AIH. The recommended treatment for both, AIH and SLE, are immunosuppressive strategies with therapeutic success. Except one, all published cases responded well to immunosuppressive treatment (Table 1). It has been shown for AIH, that complete biochemical remission is crucial for long-term prognosis of these patients[13]. There is no data available for the prognosis of AIH with concomitant SLE but publications suggest, that achievement of complete remission is crucial not only for long-term survival in these patients but also regarding quality of life. However, AIH has a more aggressive histology pattern and prognosis of untreated symptomatic autoimmune hepatitis is poor with a five-year survival rate below 25% in untreated patients versus 80% in those treated with corticosteroids[14].
To summarize, AIH and SLE are distinct diseases, whose combination of clinical symptoms and diagnostic markers overlap. While SLE and AIH are rarely diagnosed as concomitant diseases in one patient, hepatic involvement in patients with SLE is sometimes observed during the course of disease. In our view, AIH needs to be considered in the differential diagnosis of any SLE patient with elevated liver enzymes, and liver biopsy should become mandatory in such patients.
We would like to thank Till Krech and Alexander Quaas from the Department of Pathology for the outstanding cooperation.
Authors report six female patients with systemic lupus erythematodes (SLE) and autoimmune hepatitis (AIH).
Current diagnostic criteria for both SLE and AIH were fulfilled.
Hepatic involvement caused by hepatotoxic drugs, coincident viral hepatitis or non-alcoholic fatty liver disease.
All patients presented with elevated liver enzymes. Five of six showed increased levels of IgG. While all patients tested negative for anti liver kidney-1 as well as soluble liver antigen/LP antibody, three patients tested positive for smooth muscle. Four patients showed positive anti-double stranded DNA titers, only one patient tested positive for anti-Sm antibody.
Liver biopsy was performed due to elevated transaminases in all cases and showed typical signs of AIH. Advanced fibrosis/cirrhosis was found in three patients.
Treatment was initiated in all cases with prednisolone pulse-therapy and extended to a combination of azathioprine and hydroxychloroquine in four cases. A monotherapy with azathioprine or mycophenolate mofetil after prednisolone pulse-therapy was started in one patient, respectively. Two patients required a change of treatment due to azathioprine intolerance and switched to treatment with cyclophosphamide.
Autoimmune hepatitis needs to be considered in the differential diagnosis of any SLE patient with elevated liver enzymes, and liver biopsy should become mandatory in such patients.
This is a case series and literature review paper of patients with AIH-SLE overlap. It is very important to clarify the characteristics of these patients.
P- Reviewer: Yoshizawa K S- Editor: Gou SX L- Editor: A E- Editor: Liu XM
| 1. | Runyon BA, LaBrecque DR, Anuras S. The spectrum of liver disease in systemic lupus erythematosus. Report of 33 histologically-proved cases and review of the literature. Am J Med. 1980;69:187-194. [PubMed] |
| 2. | Matsumoto T, Yoshimine T, Shimouchi K, Shiotu H, Kuwabara N, Fukuda Y, Hoshi T. The liver in systemic lupus erythematosus: pathologic analysis of 52 cases and review of Japanese Autopsy Registry Data. Hum Pathol. 1992;23:1151-1158. [PubMed] |
| 3. | Alvarez F, Berg PA, Bianchi FB, Bianchi L, Burroughs AK, Cancado EL, Chapman RW, Cooksley WG, Czaja AJ, Desmet VJ. International Autoimmune Hepatitis Group Report: review of criteria for diagnosis of autoimmune hepatitis. J Hepatol. 1999;31:929-938. [PubMed] |
| 4. | Hennes EM, Zeniya M, Czaja AJ, Parés A, Dalekos GN, Krawitt EL, Bittencourt PL, Porta G, Boberg KM, Hofer H. Simplified criteria for the diagnosis of autoimmune hepatitis. Hepatology. 2008;48:169-176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1205] [Cited by in RCA: 1252] [Article Influence: 73.6] [Reference Citation Analysis (0)] |
| 5. | Lohse AW, Mieli-Vergani G. Autoimmune hepatitis. J Hepatol. 2011;55:171-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 143] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 6. | Czaja AJ, Morshed SA, Parveen S, Nishioka M. Antibodies to single-stranded and double-stranded DNA in antinuclear antibody-positive type 1-autoimmune hepatitis. Hepatology. 1997;26:567-572. [PubMed] |
| 7. | Rahman A, Isenberg DA. Systemic lupus erythematosus. N Engl J Med. 2008;358:929-939. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1314] [Cited by in RCA: 1326] [Article Influence: 78.0] [Reference Citation Analysis (0)] |
| 8. | Chowdhary VR, Crowson CS, Poterucha JJ, Moder KG. Liver involvement in systemic lupus erythematosus: case review of 40 patients. J Rheumatol. 2008;35:2159-2164. [PubMed] |
| 9. | Hochberg MC. Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. 1997;40:1725. [PubMed] |
| 10. | Lüth S, Weiler-Normann C, Schramm C, Lohse AW. [Autoimmune liver diseases]. Internist (Berl). 2009;50:310-317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Mackay IR. “Hepatic diseases and systemic lupus erythematosus,” in Systemic Lupus Erythematosus. 3rd edition. Lahita RG, editor. San Diego, Calif: Academic Press 1999; 747-763. |
| 12. | Lohse AW. Rolls Royce for everybody? Diagnosing liver disease by mini-laparoscopy. J Hepatol. 2011;54:584-585. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Hoeroldt B, McFarlane E, Dube A, Basumani P, Karajeh M, Campbell MJ, Gleeson D. Long-term outcomes of patients with autoimmune hepatitis managed at a nontransplant center. Gastroenterology. 2011;140:1980-1989. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 159] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 14. | Kirk AP, Jain S, Pocock S, Thomas HC, Sherlock S. Late results of the Royal Free Hospital prospective controlled trial of prednisolone therapy in hepatitis B surface antigen negative chronic active hepatitis. Gut. 1980;21:78-83. [PubMed] |
| 15. | Chattopadhyay P, Dhua D, Philips CA, Ghosh J. A patient of lupus presenting with myocarditis and overlapping autoimmune hepatitis. Case Rep Rheumatol. 2011;2011:402483. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 16. | Choi DH, Kim HK, Park TI, John BM, Kang SH, Lee YS, Kim TH, Lee UJ, Lee TS, Yoon GO. [A case of anti-LKM 1 positive autoimmune hepatitis accompanied by systemic lupus erythematosus]. Korean J Gastroenterol. 2008;51:190-193. [PubMed] |
| 17. | Deen ME, Porta G, Fiorot FJ, Campos LM, Sallum AM, Silva CA. Autoimmune hepatitis and juvenile systemic lupus erythematosus. Lupus. 2009;18:747-751. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 18. | Efe C, Purnak T, Ozaslan E, Ozbalkan Z, Karaaslan Y, Altiparmak E, Muratori P, Wahlin S. Autoimmune liver disease in patients with systemic lupus erythematosus: a retrospective analysis of 147 cases. Scand J Gastroenterol. 2011;46:732-737. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 37] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 19. | Iwai M, Harada Y, Ishii M, Tanaka S, Muramatsu A, Mori T, Nakashima T, Okanoue T, Hirohata S. Autoimmune hepatitis in a patient with systemic lupus erythematosus. Clin Rheumatol. 2003;22:234-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 19] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 20. | Kaw R, Gota C, Bennett A, Barnes D, Calabrese L. Lupus-related hepatitis: complication of lupus or autoimmune association? Case report and review of the literature. Dig Dis Sci. 2006;51:813-818. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 22] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 21. | Kooy A, de Heide LJ, Engelkens HJ, Mulder AH, van Hagen M, Schalm SW. Hepatitis in a patient with SLE: is it autoimmune hepatitis? Neth J Med. 1996;48:128-132. [PubMed] |
| 22. | Koshy JM, John M. Autoimmune Hepatitis - SLE Overlap Syndrome. J Assoc Phys India. 2012;60:59-60. |
| 23. | Moriwaki Y, Maebo A, Yamade W, Yamamoto T, Amuro Y, Hada T, Higashino K. Autoimmune hepatitis or hepatic involvement in SLE?--A case report. Gastroenterol Jpn. 1987;22:222-227. [PubMed] |
| 24. | Satoh T, Hirakata M, Yoshida T, Matsumura M, Miyachi K, Mimori T, Akizuki M. Systemic lupus erythmatosus associated with autoimmune hepatitis two cases with novel autoantibodies to transfer RNA-related antigens. Clin Rheumatol. 1997;16:305-309. [PubMed] |
| 25. | Suzuki K, Matsuki Y, Hidaka T, Kawaguchi Y, Kawakami M, Hino K, Nakamura H. Double filtration plasmapheresis in a patient with autoimmune hepatitis-systemic lupus erythematosus overlap. Intern Med. 1993;32:725-729. [PubMed] |
| 26. | Takahashi A, Rai T, Onizawa M, Monoe K, Kanno Y, Saito H, Abe K, Yokokawa J, Irisawa A, Ohira H. Autoimmune hepatitis complicated by late-onset systemic lupus erythematosus. Hepatol Res. 2007;37:771-774. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 27. | Tojo J, Ohira H, Abe K, Yokokawa J, Takiguchi J, Rai T, Shishido S, Sato Y, Kasukawa R. Autoimmune hepatitis accompanied by systemic lupus erythematosus. Intern Med. 2004;43:258-262. [PubMed] |
| 28. | Usta Y, Gurakan F, Akcoren Z, Ozen S. An overlap syndrome involving autoimmune hepatitis and systemic lupus erythematosus in childhood. World J Gastroenterol. 2007;13:2764-2767. [PubMed] |
| 29. | Yamasaki S, Origuchi T, Nakata K, Toriyama K, Taguchi T, Ida H, Kawakami A, Eguchi K. Autoimmune hepatitis in a patient with systemic lupus erythematosus: a case report. Mod Rheumatol. 2004;14:169-173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 30. | Yoon JU, Park SH, Kim EJ, Hong JH, Lee HS, Oh KC, Park CH, Hahn TH, Lee DK, Kim JH. [Two cases of autoimmnune hepatitis associated with systemic lupus erythematosus]. Taehan Kan Hakhoe Chi. 2003;9:231-235. [PubMed] |