Published online Sep 21, 2014. doi: 10.3748/wjg.v20.i35.12602
Revised: April 30, 2014
Accepted: June 12, 2014
Published online: September 21, 2014
Processing time: 195 Days and 10.5 Hours
AIM: To evaluate the efficacy of botulinum toxin type A injection to the puborectalis and external sphincter muscle in the treatment of patients with anismus unresponsive to simple biofeedback training.
METHODS: This retrospective study included 31 patients suffering from anismus who were unresponsive to simple biofeedback training. Diagnosis was made by anorectal manometry, balloon expulsion test, surface electromyography of the pelvic floor muscle, and defecography. Patients were given botulinum toxin type A (BTX-A) injection and pelvic floor biofeedback training. Follow-up was conducted before the paper was written. Improvement was evaluated using the chronic constipation scoring system.
RESULTS: BTX-A injection combined with pelvic floor biofeedback training achieved success in 24 patients, with 23 maintaining persistent satisfaction during a mean period of 8.4 mo.
CONCLUSION: BTX-A injection combined with pelvic floor biofeedback training seems to be successful for intractable anismus.
Core tip: Pelvic floor biofeedback was accepted to be an effective therapy for anismus. However, unfortunately the treatment proved to be ineffective in some cases. In our study, we performed biofeedback training combined with botulinum toxin type A injection to the puborectalis and external sphincter. Diagnosis was made by anorectal manometry, balloon expulsion test, surface electromyography of the pelvic floor muscle, and defecography. Follow-up was conducted before the paper was written. Improvement was evaluated using the chronic constipation scoring system. Botulinum toxin type A injection combined with pelvic floor biofeedback training achieved success in 24 (24/31) patients, with 23 maintaining persistent satisfaction during a mean period of 8.4 mo.
- Citation: Zhang Y, Wang ZN, He L, Gao G, Zhai Q, Yin ZT, Zeng XD. Botulinum toxin type-A injection to treat patients with intractable anismus unresponsive to simple biofeedback training. World J Gastroenterol 2014; 20(35): 12602-12607
- URL: https://www.wjgnet.com/1007-9327/full/v20/i35/12602.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i35.12602
Chronic constipation is one of the most common gastrointestinal problems worldwide, with an incidence between 2% to 34%. Obstructed outlet constipation (OOC) is the predominant subtype occurring in about 7% of the adult population[1]. Patients with OOC always complain of extremely difficult defecation but still experience the need for at least daily defecation. Prolonged defecation, excessive straining, inability to achieve complete evacuation, and laxative and enema abuse occur commonly in OOC patients[2]. The paradoxical contraction and/or defective relaxation of the puborectal muscle and the external anal sphincter induces great resistance against the stool during defecation. This paradoxical contraction of the pelvic floor muscles during straining at defecation is generally defined as anismus, outlet dysfunction constipation, or more precisely, pelvic floor dyssynergia.
Diagnosis of anismus indispensably needs an overall evaluation of the function of evacuation based on anorectal manometry (ARM), balloon expulsion test, surface electromyography of the pelvic floor muscle, and defecography[3-6]. Unfortunately, there is no single test can conclusively determine the presence and extent of anismus[7]. Experiences of therapy with laxatives and surgical operation have had conflicting results[1,8]. Biofeedback training is a physiologic process to relax the pelvic floor muscles and ultimately improve their concordant constriction. Botulinum toxin type A can be used to relax the problematic anal sphincter in the initial stage, which leads to instant defecation improvement. This greatly strengthens the confidence of patients suffering from this long-term affliction as well as producing a strong motivation for the following biofeedback training.
Botulinum toxin type A inhibits neuromuscular transmission and has a powerful muscle relaxing effect[9]. Therefore, we applied botulinum toxin type A injection in combination with biofeedback training to treat patients with anismus who were inefficient when treated with simplex biofeedback training. The clinic’s experience with botulinum toxin type A (BTX-A) in anismus patients has been reported over the past few years. In this study, we perform BTX-A injection guided by three-dimensional endoluminal ultrasonography. The aim of this retrospective study was to evaluate the results of BTX-A injection combined with biofeedback training after inefficient simplex biofeedback training in patients with anismus.
This study comprised a study of 31 patients with OOC due to anismus. They were recruited for the study from September 2010 to September 2011. Prior to the study, all included patients had finished a course of biofeedback training and received an unsatisfied result. Additionally, there was no significant difference in functional assessment before and after the biofeedback training.
18 males and 13 females with a mean age of 50.1 ± 18.9 years (range: 23-86 years old) and a mean duration of constipation of 5.6 ± 5.4 years (range: 1-20 years) were included in the study.
The inclusion criteria were: fulfilled the Rome III constipation criteria; the diagnosis of anismus was made by clinical examination, including anorectal manometry, balloon expulsion test, and defecography; evidence of inappropriate contraction or failure to relax the pelvic floor muscles during attempts to defecate in at least two of the aforementioned tests; evidence of adequate propulsive forces during attempts to defecate (rectal pressure during straining > 45 mmHg); and roughly normal rectal sensation.
The patients suffered from incomplete, prolonged, and difficult evacuation, with constant use of enema, laxatives, and digital evacuation, but having a daily and sometimes more frequent urge to defecate even without enema and laxatives. Colon transportation test showed normal motivation in those cases.
The exclusion criteria were: anismus patients with a simultaneous secondary cause of constipation; patients who underwent pelvic floor and anorectal surgery, colonic inertia, or were suffering the lingering effects of a cerebrovascular accident; and patients with a cognitive handicap or any other condition making biofeedback training impossible. Patients with constipation-related primary disease (e.g., hypothyroidism) were also excluded.
After careful explanation of the clinical condition and the options of treatment, all included patients have written informed consent. Patients were then given the BTX-A injection before biofeedback training.
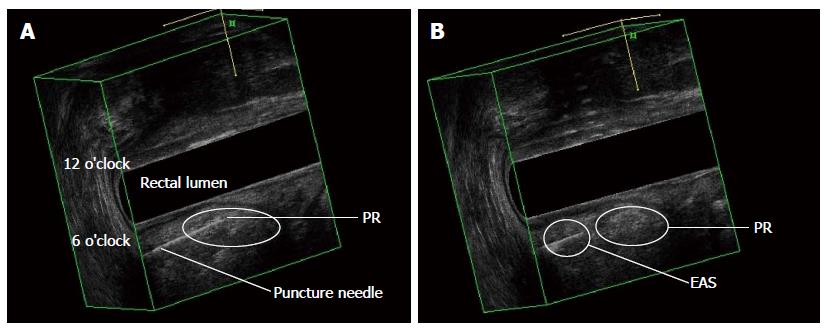
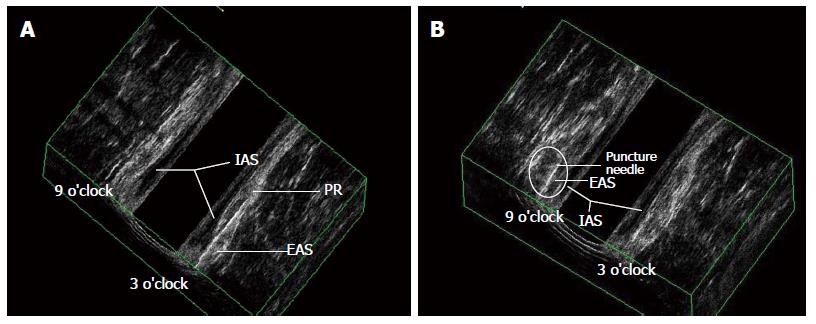
All 31 patients were injected with botulinum toxin type A before undergoing biofeedback training. The toxin was injected with a caudal anesthesia while the patients were in the lithotomy position. A vial of BTX-A, 100 μ (BTX-A, China), was dissolved in 3 mL 0.9% sodium chloride solution 30 min before use. The injection was given with an insulin syringe fitted to a needle size of 21 gauze and 6 cm in length. The needle tip was guided by the contralateral index finger into the puborectalis through the external sphincter. The position of the needle tip was confirmed by three-dimensional endoluminal ultrasonography. The BTX-A was injected into the puborectalis and the external anal sphincter consecutively during the needle withdrawal at 3, 6, and 9 o’clock in the lithotomy position (Figures 1 and 2). The dosages for the two muscles were assigned according to the results of anorectal manometry and defecography. Generally, the volume dose was 100u divided equally for the puborectalis and the external anal sphincter. The doses for the three positions were assigned to 30u, 40u, and 30u (Table 1). This procedure was done as a hospitalization procedure. The patients started biofeedback training 2 wk after the injection.
| Muscle | Position | Total | ||
| 3 o’clock | 6 o’clock | 9 o’clock | ||
| Puborectalis | 15u | 20u | 15u | 50u |
| EAS | 15u | 20u | 15u | 50u |
| Total | 30u | 40u | 30u | 100u |
Patients received rehabilitation treatment including a section of in-anal electro-stimulation and biofeedback training after a successful explanation of the aim and rationale of this physical treatment. The biofeedback training system was mediated by surface EMG signal. Anorectal electromyogram sensors and surface electrodes were placed to collect electrical signals and give electro-stimulation. Patients were subjected to the treatment once or twice a day for 30 min for each treatment, including 15 min of electro-stimulation and 15 min of biofeedback training. The intensity of electro-stimulation was adjusted in such a way that the patient felt a considerable sensation without experiencing pain. Stimulation was done with a frequency of 10 MHz and the impulse duration was 10 s with a pause of 10 s thereafter. The Kegel exercise was applied in this biofeedback training session. Patients were allowed to see the trace of pelvic floor muscle activity at rest and during voluntary contraction. Patients were then taught to make the trace of pelvic floor muscle activity coincide with the Kegel diagram by relaxing the anus and doing voluntary constriction. All patients finished a period of therapy of at least one month and suggested to do Kegel training at home after the out-patient training program.
Follow-up was conducted twice; after pelvic floor biofeedback following the PTX-A injection a month after the injection) and before this paper with the range 6 to 12 mo (8.4 ± 3.44 mo) after treatment by telephone. The patient then completed a CSS (constipation scoring system) symptom questionnaire[10].
Frequency of bowel movements, difficulty, completeness, abdominal pain, time in lavatory per attempt, type of assistance, unsuccessful evacuation attempts per 24 h, and duration of constipation were recorded.
For each patient, anorectal manometry with a balloon expulsion test was performed after the complete treatment (including PTX-A injection and consecutive biofeedback training). The clinical follow-up was always conducted by the same author, with the same applying to the manometry. This study was approved by the hospital ethics committee. Each patient gave written informed consent before entering this study.
Data were expressed as mean ± SD. Student’s t-test was used to compare the treatment results and the Chi-square test was used for comparison of proportions. P < 0.05 was considered statistically significant.
From October 2010 to July 2011, 31 patients with a final diagnosis of anismus and who were unresponsive to a period of pelvic biofeedback training received PTX-A injection. The study group included 18 males and 13 females, with a mean age of 50.1 ± 18.9 years and mean disease duration of 5.61 ± 5.4 years. The CSS score and ARM parameters showed no significant difference between before and after the pelvic floor biofeedback training, or in patients who were unsatisfied with the final biofeedback training effect. The 31 patients then underwent the PTX-A injection and consecutive pelvic floor biofeedback training. This article summarizes our clinical observations for an 8.4-mo follow-up period.
The ARM parameters and balloon expulsion test were performed before BTX-A injection and after the pelvic rehabilitation following the PTX-A injection. After treatment, the pressure of the anal canal during rest and defecation was significantly reduced from (93 ± 16.5) mmHg and (105 ± 28.3) mmHg to (63 ± 8.6.3) mmHg and (42 ± 8.9) mmHg, respectively. However, the pressure of the rectum when defecation occurred was unchanged. The functional length of the anal sphincter decreased from (4.5 ± 0.84) cm to (3.2 ± 0.54) cm with statistical significance. The success rate of the balloon expulsion test increased from 0% to 74.2% (23/31). Furthermore, the CSS result was improved accordingly, with the score decreasing from (14.3 ± 2.49) to (6.4 ± 3.20) (Tables 2 and 3).
| Pre-BTX-A injection | Post-BTX-A injection and consecutive biofeedback training | t | P | |
| Pressure of rectum during defecation (mmHg) | 64 ± 27 | 67 ± 28 | 1.335 | 0.192 |
| Rest pressure of anal canal (mmHg) | 93 ± 16.5 | 63 ± 8.6.3 | 11.726 | 0.000 |
| Pressure of anal canal during defecation (mmHg) | 105 ± 28.3 | 42 ± 8.9 | 12.328 | 0.000 |
| Functional length of anal sphincter (cm) | 4.5 ± 0.84 | 3.2 ± 0.54 | 8.9 | 0.000 |
| Balloon expulsion test success rate | 0% | 74.2% (23/31) | 9.185 | 0.002 |
| Chronic constipation score | 14.3 ± 2.49 | 6.4 ± 3.20 | 14.108 | 0.000 |
| Pre-BTX-A injection | Post-BTX-A injection and consecutive biofeedback training | t | P | |
| Frequency of bowel movements | 0.39 ± 0.62 | 0.10 ± 0.30 | 3.057 | 0.005 |
| Difficulty: painful evacuation | 3.29 ± 0.53 | 1.45 ± 0.72 | 13.146 | 0.000 |
| Completeness: feeling incomplete | 3.45 ± 0.57 | 1.52 ± 0.72 | 14.816 | 0.000 |
| abdominal pain | 0.77 ± 1.1 | 0.54 ± 0.85 | 2.040 | 0.050 |
| Time: minutes in lavatory per attempt | 2.38 ± 0.88 | 0.97 ± 0.66 | 10.330 | 0.000 |
| Assistance: type of assistance | 1.81 ± 1.73 | 0.39 ± 0.77 | 4.295 | 0.000 |
| Failure: unsuccessful attempts for evacuation per 24 h | 1.00 ± 0.37 | 0.29 ± 0.46 | 7.473 | 0.000 |
The follow-up was conducted after the complete treatment (PTX-A injection and consecutive biofeedback training) and before the paper by telephone. The patient completed a CSS symptom questionnaire and the incidence of fecal incontinence was inquired. We found that there was no difference between the CSS evaluation of post-treatment and before the paper. The incidence of fecal incontinence was significantly reduced over time. However, there were no significant changes in the CSS and satisfaction rate right after the whole treatment course and before the paper (Table 4).
| Follow-up | CSS | Fecal incontinence occurred | Satisfaction rate |
| After BTX-A injection and consecutive biofeedback training | 6.4 ± 3.20 | 22.6% (7/31) | 77.4% (24/31) |
| Before the paper | 6.5 ± 3.20 | 3.2% (1/31) | 74.2% (23/31) |
| T or χ2 | -0.902 | 5.167 | 0.088 |
| P | 0.374 | 0.023 | 0.767 |
For the majority of patients suffering from constipation that were referred to our center, their cases were related to an outlet obstruction problem. Although there is no etiological data on the frequency of anismus, according the observations in our center it is probably the commonest etiology of outlet obstruction constipation. Generally, more patients with anismus were satisfied with biofeedback treatment[11]. However, there are still a few anismus patients who are not so responsive to a routine course of biofeedback training because of a failure to relax the pelvic floor muscles first, which is a key premise for the muscles in order to do functional practice. A wide variety of surgical and pharmacologic approaches have been proposed to reduce the pressure provided by the spastic puborectalis and anal sphincter[12-14]. Unfortunately, doctors have not yet found a dependable therapeutic approach to solving anismus. Surgical treatments aimed at weakening or dilating the puborectalis muscle are often unsuccessful[8], whereas injections of botulinum toxin directly into the puborectalis muscle have provided promising results[15].
A number of papers have reported that biofeedback training is an effective treatment for anismus patients, albeit with conflicting efficacy rates that range from 9% to 100%[16].
BTX-A has been used as a potent neurotoxin since the 1970s. Its mechanism of action is inhibition of acetylcholine release in the presynaptic region. It has been used in the treatment of neurologic disorders characterized by excessive muscle contraction such as facial dystonias, vocal spasms, torticollis, and limb dystonias. In the past decade BTX-A has been used to treat anismus. We performed a BTX-A injection to the puborectalis and external sphincter for the 31 anismus patients selected from the cases unresponsive to biofeedback training. Referring to the description of BTX-A injection in the anismus treatment, we used the Chinese form of BTX-A with a dosage of 100 units for each patient. In our study, we performed the injection with the guidance of three-dimensional endoluminal ultrasonography. Maria et al[17] used an EMG-guided technique for the exact location of the puborectalis muscle. We found that guidance by ultrasonography during the injection simplified the localization of the injection site as well as dosage distribution to the right muscle. BTX-A instantly caused the paralysis of muscles by presynaptic inhibition of acetylcholine release, which consequently reduced resistance during evacuation. However, anismus patients have a problem other than spasm of the puborectalis and external sphincter; lack of concordance during defecation. The goal of following biofeedback training is to improve the motor coordination of the puborectalis and external sphincter, which produces a persistent effect several authors have reported that botulinum toxin seemed to be a promising treatment for patients with anismus[18,19]. However, it has also been reported that repeated injections might be necessary to maintain clinical improvement. In our study, ARM and balloon expulsion test also showed a significant improvement post-treatment. As expected, CSS also decreased from a mean of 14.3 to 6.4. 23 out of 24 cases maintained satisfactory defecation after the treatment and before the paper, respectively. The results of our study differ from those reported by Farid and Ron.
In our study, we used the Chinese form of BTX-A. Complications of the injection such as post-injection pain, local infection, or bleeding were not observed. Hallan et al[20] reported that incontinence after injection of the British form of BTX-A had occurred in two cases in their series. We observed eight cases in which temple fecal incontinence occurred, of which seven were in the first month after the injection. The extent of fecal incontinence was slight.
The patients’ satisfaction is the key standard in deciding the success of the treatment procedure. BTX-A was considered to be a temporary treatment for anismus due to its temporal medical effective time. In our study, BTX-A injection combined with pelvic floor biofeedback training has proved to be a more valid way to treat anismus for its persisted effect. It is a safer and more effective treatment method for intractable anismus than simple treatment using BTX-A or biofeedback training alone.
The paradoxical contraction and/or defective relaxation of the puborectal muscle and the external anal sphincter induces great resistance against the stool during defecation. This paradoxical contraction of the pelvic floor muscles during straining at defecation is generally defined as anismus, outlet dysfunction constipation, or more precisely, pelvic floor dyssynergia. Biofeedback training is a physiologic process to relax the pelvic floor muscles and ultimately improve their concordant constriction. Unfortunately, doctors have not yet found a dependable therapeutic approach to solve anismus. Botulinum toxin type A (BTX-A) has been used as a potent neurotoxin since the 1970s. Since the past decade, BTX-A has been used to treat anismus. The authors performed BTX-A injection to the puborectalis and external sphincter for the 31 anismus patients selected from cases unresponsive to biofeedback training.
Obstructed outlet constipation is the predominant subtype, occurring in about 7% of the adult population. Diagnosis of anismus indispensably needs an overall evaluation of the function of evacuation based on anorectal manometry, balloon expulsion test, surface electromyography of the pelvic floor muscle, and defecography. A wide variety of surgical and pharmacologic approaches have been proposed to reduce the pressure provided by the spastic puborectalis and anal sphincter. However, pelvic floor biofeedback has been proven to be an ideal treatment method. Botulin toxin injection is a simple, easy, and safe method for the treatment of intractable anismus. It should thus be considered after biofeedback has failed.
In this study, we used the Chinese form of BTX-A. The authors found that guidance by ultrasonography during injection simplified the localization of the injection site and dosage distribution to the right muscle. They performed a longer period of follow-up than the former report.
In this study, BTX-A injection combined with pelvic floor biofeedback training has proved to be a more valid way to treat anismus due to its persisted effect. It is a safe and more effective treatment method for intractable anismus than the simple treatment using BTX-A or biofeedback training alone.
This is a very interesting manuscript about intractable anismus. In this manuscript, the authors evaluated the efficacy of botulinum toxin type A injection to the puborectalis and external sphincter muscle to treat patients with anismus unresponsive to simple biofeedback training.
P- Reviewer: Treepongkaruna S S- Editor: Qi Y L- Editor: Rutherford A E- Editor: Zhang DN
| 1. | D’Hoore A, Penninckx F. Obstructed defecation. Colorectal Dis. 2003;5:280-287. [PubMed] |
| 2. | Kuijpers HC, Bleijenberg G. The spastic pelvic floor syndrome. A cause of constipation. Dis Colon Rectum. 1985;28:669-672. [PubMed] |
| 3. | Weber J, Ducrotte P, Touchais JY, Roussignol C, Denis P. Biofeedback training for constipation in adults and children. Dis Colon Rectum. 1987;30:844-846. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 70] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 4. | Preston DM, Lennard-Jones JE. Anismus in chronic constipation. Dig Dis Sci. 1985;30:413-418. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 335] [Cited by in RCA: 278] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 5. | Johansson C, Nilsson BY, Mellgren A, Dolk A, Holmström B. Paradoxical sphincter reaction and associated colorectal disorders. Int J Colorectal Dis. 1992;7:89-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 28] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Kuijpers HC, Bleijenberg G, de Morree H. The spastic pelvic floor syndrome. Large bowel outlet obstruction caused by pelvic floor dysfunction: a radiological study. Int J Colorectal Dis. 1986;1:44-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 51] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Schouten WR, Briel JW, Auwerda JJ, van Dam JH, Gosselink MJ, Ginai AZ, Hop WC. Anismus: fact or fiction? Dis Colon Rectum. 1997;40:1033-1041. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 42] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 8. | Maria G, Anastasio G, Brisinda G, Civello IM. Treatment of puborectalis syndrome with progressive anal dilation. Dis Colon Rectum. 1997;40:89-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Dolly JO, Black J, Williams RS, Melling J. Acceptors for botulinum neurotoxin reside on motor nerve terminals and mediate its internalization. Nature. 1984;307:457-460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 251] [Cited by in RCA: 214] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 10. | Agachan F, Chen T, Pfeifer J, Reissman P, Wexner SD. A constipation scoring system to simplify evaluation and management of constipated patients. Dis Colon Rectum. 1996;39:681-685. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 818] [Cited by in RCA: 851] [Article Influence: 29.3] [Reference Citation Analysis (0)] |
| 11. | Gadel Hak N, El-Hemaly M, Hamdy E, El-Raouf AA, Atef E, Salah T, El-Hanafy E, Sultan A, Haleem M, Hamed H. Pelvic floor dyssynergia: efficacy of biofeedback training. Arab J Gastroenterol. 2011;12:15-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Andromanakos N, Skandalakis P, Troupis T, Filippou D. Constipation of anorectal outlet obstruction: pathophysiology, evaluation and management. J Gastroenterol Hepatol. 2006;21:638-646. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 94] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 13. | Faried M, El Nakeeb A, Youssef M, Omar W, El Monem HA. Comparative study between surgical and non-surgical treatment of anismus in patients with symptoms of obstructed defecation: a prospective randomized study. J Gastrointest Surg. 2010;14:1235-1243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 31] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 14. | Farid M, Youssef T, Mahdy T, Omar W, Moneim HA, El Nakeeb A, Youssef M. Comparative study between botulinum toxin injection and partial division of puborectalis for treating anismus. Int J Colorectal Dis. 2009;24:327-334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 30] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 15. | Albanese A, Maria G, Bentivoglio AR, Brisinda G, Cassetta E, Tonali P. Severe constipation in Parkinson’s disease relieved by botulinum toxin. Mov Disord. 1997;12:764-766. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 52] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 16. | Heymen S, Jones KR, Scarlett Y, Whitehead WE. Biofeedback treatment of constipation: a critical review. Dis Colon Rectum. 2003;46:1208-1217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 88] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 17. | Maria G, Brisinda G, Bentivoglio AR, Cassetta E, Albanese A. Botulinum toxin in the treatment of outlet obstruction constipation caused by puborectalis syndrome. Dis Colon Rectum. 2000;43:376-380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 45] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 18. | Shafik A, El-Sibai O. Botulin toxin in the treatment of nonrelaxing puborectalis syndrome. Dig Surg. 1998;15:347-351. [PubMed] |
| 19. | Ron Y, Avni Y, Lukovetski A, Wardi J, Geva D, Birkenfeld S, Halpern Z. Botulinum toxin type-A in therapy of patients with anismus. Dis Colon Rectum. 2001;44:1821-1826. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 64] [Article Influence: 2.7] [Reference Citation Analysis (0)] |