Published online Aug 21, 2014. doi: 10.3748/wjg.v20.i31.10921
Revised: March 15, 2014
Accepted: April 28, 2014
Published online: August 21, 2014
Processing time: 206 Days and 9.2 Hours
AIM: To describe an optimal route to the Braun anastomosis including the use of retrieval-balloon-assisted enterography.
METHODS: Patients who received a Billroth II gastroenterostomy (n = 109) and a Billroth II gastroenterostomy with Braun anastomosis (n = 20) between January 2009 and May 2013 were analyzed in this study. Endoscopic retrograde cholangiopancreatography (ERCP) was performed under fluoroscopic control using a total length of 120 cm oblique-viewing duodenoscope with a 3.7-mm diameter working channel. For this procedure, we used a triple-lumen retrieval balloon catheter in which a 0.035-inch guidewire could be inserted into the “open-channel” guidewire lumen while the balloon could be simultaneously injected and inflated through the other 2 lumens.
RESULTS: For the patients with Billroth II gastroenterostomy and Braun anastomosis, successful access to the papilla was gained in 17 patients (85%) and there was therapeutic success in 16 patients (80%). One patient had afferent loop perforation, but postoperative bleeding did not occur. For Billroth II gastroenterostomy, there was failure in accessing the papilla in 15 patients (13.8%). ERCP was unsuccessful because of tumor infiltration (6 patients), a long afferent loop (9 patients), and cannulation failure (4 patients). The papilla was successfully accessed in 94 patients (86.2%), and there was therapeutic success in 90 patients (82.6%). Afferent loop perforation did not occur in any of these patients. One patient had hemorrhage 2 h after ERCP, which was successfully managed with conservative treatment.
CONCLUSION: Retrieval-balloon-assisted enterography along an optimal route may improve the ERCP success rate after Billroth II gastroenterostomy and Braun anastomosis.
Core tip: For patients with a Billroth II gastroenterostomy, endoscopic retrograde cholangiopancreatography (ERCP) is difficult because of altered anatomy, and the success rate decreases for those with Braun anastomosis. ERCP failure in such patients is caused by difficulties in entering the afferent loop and accessing the papilla. We reported the use of a wire-guided retrieval balloon to remove common bile duct stones and facilitate endoscope insertion for successful ERCP in post-gastrointestinal surgery patients. We termed the procedure “retrieval-balloon-assisted enterography”. We believe that retrieval-balloon-assisted enterography along the optimal route may improve the ERCP success rate after Billroth II gastroenterostomy and Braun anastomosis.
- Citation: Wu WG, Zhang WJ, Gu J, Zhao MN, Zhuang M, Tao YJ, Liu YB, Wang XF. Retrieval-balloon-assisted enterography for ERCP after Billroth II gastroenterostomy and Braun anastomosis. World J Gastroenterol 2014; 20(31): 10921-10926
- URL: https://www.wjgnet.com/1007-9327/full/v20/i31/10921.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i31.10921
Endoscopic retrograde cholangiopancreatography (ERCP) is very useful in pancreaticobiliary disease management in patients with a normal anatomy and surgically altered anatomy. For patients with Billroth II gastroenterostomy, ERCP is difficult because of the altered anatomy, and the success rate decreases for those with Braun anastomosis. The success rate was reported to be 83% for simple Billroth II gastroenterostomy but only 29% in patients with a Billroth II gastroenterostomy and an additional Braun anastomosis[1]. ERCP failure in such patients was caused by difficulties in entering the afferent loop and accessing the papilla[2-4]. Recently, we reported the use of a wire-guided retrieval balloon to remove common bile duct stones and facilitate endoscope insertion for successful ERCP in post-gastrointestinal surgery patients[5,6]. We termed the procedure “retrieval-balloon-assisted enterography”. In this retrospective study, we aimed to describe endoscope insertion technique for patients with a Billroth II gastroenterostomy and Braun anastomosis.
An institutional review board-approved retrospective analysis was performed at the Department of General Surgery, Xinhua Hospital, School of Medicine, Shanghai Jiao Tong University. In this study, we included patients who underwent Billroth II gastroenterostomy and Braun anastomosis for therapeutic biliary interventions between January 2009 and May 2013 in the ERCP unit in the Department of General Surgery. During this period, 2994 ERCP procedures were performed. Patients who had normal anatomy and other surgically altered anatomy were excluded from the study. The study included 109 patients who had a Billroth II gastroenterostomy and 20 patients who had a Billroth II gastroenterostomy with Braun anastomosis.
The procedure was performed with the patient under pharyngeal anesthesia, and sedation with an intramuscular injection of 10 mg diazepam. All the patients received oxygen and were monitored by electrocardiography and pulse oximetry. The patient was placed in the prone position. ERCP was performed under fluoroscopic control using a total length of 120 cm oblique-viewing duodenoscope with a diameter of 3.7 mm working channel (Olympus V260, Olympus Medical Systems, Tokyo, Japan). For this procedure, we used a triple-lumen retrieval balloon catheter (Extractor Pro RX retrieval balloon catheter, Boston Scientific, Shanghai, China) in which a 0.035-inch (0.089 mm) guidewire could be inserted into the “open-channel” guidewire lumen while the balloon could be simultaneously injected and inflated through the other 2 lumens.
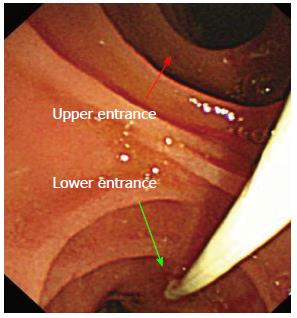
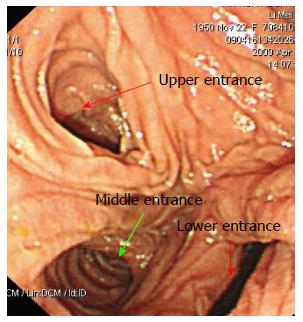
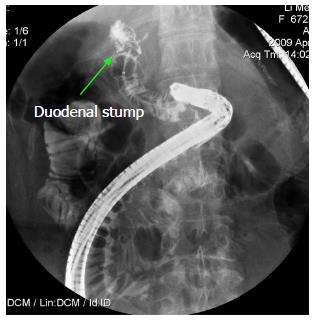
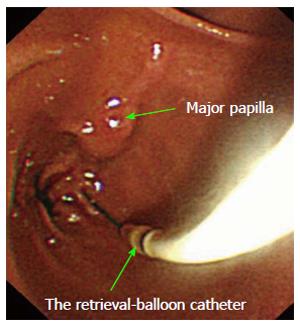
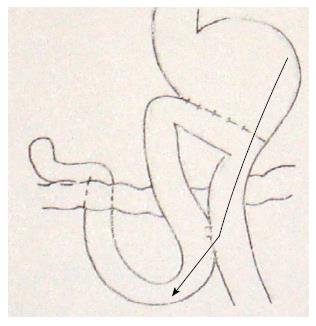
In our technique, we first review the patient’s previous surgical records, which most often indicate that the efferent loop is at the greater curvature of the stomach. The solution is to extend the duodenoscope along the greater stomach curvature until the gastrojejunal anastomosis becomes visible, from which perspective the “lower entrance” is the correct efferent loop (Figure 1). The efferent loop is a better entrance for the duodenoscope because it is less angulated than the afferent loop. In such cases, our solution is to extend the duodenoscope along the efferent loop until the Braun anastomosis becomes visible. Three stomal openings can be visualized endoscopically, but identifying the correct entrance is a major challenge (Figure 2). The “middle entrance” is the entrance to the loop that can be used to reach the papilla of Vater when the endoscope is advanced from the efferent loop and is unique irrespective of the endoscopic approach used. The endoscope tip appears to be located in the difficult-to-negotiate portion when all 3 stomal openings are visible at the Braun anastomosis site; thereafter, we insert the guidewire of the retrieval balloon catheter through the “middle entrance” and then insert the retrieval balloon catheter over the guidewire (Figure 3). The balloon is hooked to the duodenal limb which is inflated. The retrieval balloon catheter can be used to explore the limb tract by injecting a contrast medium through the catheter under radiography and then confirming whether the limb is a duodenal stump (Figure 4). By laying it on the duodenal stump as a guide, the retrieval-balloon catheter could also be used to prevent the duodenoscope from sliding out of the right limb into another limb upon forward motion. After successful access to the right limb is achieved, the retrieval balloon is visible within the tract ahead, instead of emerging from it. While the retrieval-balloon catheter is strongly retracted into the working channel to allow the scope to advance, the endoscope is then propelled slightly forward to the major papilla (Figure 5).
The study group included 109 patients who had a simple Billroth II gastroenterostomy (102 male, 21 female; mean age, 69.4 years; age range, 47-90 years) and 20 patients who underwent Billroth II gastroenterostomy and Braun anastomosis (16 male, 4 female; mean age, 72.4 years; age range, 55-86 years). Table 1 summarizes the demographic and clinical characteristics of the patients and the interventions they received. ERCP was unsuccessful in 3 patients because of failure to access the papilla due to the presence of a long afferent loop, and the procedure was unsuccessful in 1 patient because of cannulation failure as the papilla of Vater could not be located in the duodenal stump. The papilla was successfully reached in 17 patients (85%), and there was therapeutic success in 16 patients (80%). One patient had afferent loop perforation, underwent laparotomy, and was discharged 2 wk later. Postoperative bleeding did not occur.
| Cases | Sex | Age (yr) | Previous surgery | Indication | Enterography success | Cannulation success | Intervention |
| 1 | M | 61 | Gastric cancer | Cholangitis, CBD stone | Yes | Yes | Stone extraction |
| 2 | M | 83 | Peptic ulcer | Cholangitis, CBD stone | Yes | No | / |
| 3 | M | 77 | Gastric cancer | Jaundice, cholestasis | Yes | Yes | Stone extraction |
| 4 | M | 86 | Peptic ulcer | Cholangitis, CBD stone | Yes | Yes | Drainage (stent) |
| 5 | M | 72 | Gastric cancer | Cholangitis, CBD stone | Yes | Yes | Stone extraction |
| 6 | M | 63 | Gastric cancer + CBD exploration | Cholangitis, CBD stone | No | / | / |
| 7 | F | 59 | Gastric cancer | Cholangitis, CBD stone | Yes | Yes | Drainage (stent) |
| 8 | M | 77 | Gastric cancer | Jaundice, cholestasis | No | / | / |
| 9 | M | 85 | Gastric cancer | Jaundice, cholestasis | Yes | Yes | Drainage (stent) |
| 10 | F | 58 | Gastric cancer | Cholangitis, CBD stone | Yes | Yes | Drainage (NBD) |
| 11 | F | 66 | Gastric cancer | Jaundice, cholestasis | No | / | / |
| 12 | M | 84 | Gastric cancer | Jaundice, cholestasis | Yes | Yes | Drainage (stent) |
| 13 | M | 84 | Gastric cancer | Jaundice, cholestasis | Yes | Yes | Drainage (NBD) |
| 14 | M | 55 | Gastric cancer | Cholangitis, CBD stone | Yes | Yes | Stone extraction |
| 15 | F | 69 | Gastric cancer | Cholangitis, CBD stone | Yes | Yes | Stone extraction |
| 16 | M | 72 | Gastric cancer | Cholangitis, CBD stone | Yes | Yes | Drainage (stent) |
| 17 | M | 80 | Peptic ulcer | Cholangitis, CBD stone | Yes | Yes | Stone extraction |
| 18 | M | 58 | Gastric cancer | Jaundice, cholestasis | Yes | Yes | Drainage (stent) |
| 19 | M | 83 | Gastric cancer | Jaundice, cholestasis | Yes | Yes | Drainage (stent) |
| 20 | M | 76 | Gastric cancer | Jaundice, cholestasis | Yes | Yes | Drainage (stent) |
For Billroth II gastroenterostomy, there was failure in accessing the papilla in 15 patients (13.8%). ERCP was unsuccessful because of tumor infiltration (6 patients), a long afferent loop (9 patients), and cannulation failure (4 patients). The papilla was successfully accessed in 94 patients (86.2%), and there was therapeutic success in 90 patients (82.6%). Afferent loop perforation did not occur in any of these patients. One patient had hemorrhage 2 h after ERCP, which was successfully managed with conservative treatment.
Retrieval-balloon-assisted enterography improves the overall success rate in reaching the papilla in ERCP after Billroth II gastroenterostomy and Braun anastomosis. The previously reported success rate was approximately 30% in patients who had a Billroth II gastroenterostomy with Braun anastomosis[1,7]. ERCP failure in these patients was due to failure in entering the afferent loop and the increased number of anastomoses. Thus far, no reports have indicated the optimal enterography route in which cannulation can be performed. For patients with Billroth II gastroenterostomy and Braun anastomosis, we describe our experience in establishing an ERCP enterography route. We first review the patient’s previous surgical records, which most often indicate that the efferent loop is at the greater curvature of the stomach. One major challenge is distinguishing between the afferent and efferent loops. The solution is to extend the duodenoscope along the greater curvature of the stomach until the gastrojejunal anastomosis becomes visible, from which perspective the “lower entrance” in endoscopic image is the correct efferent loop. Occasionally, we are able to draw back the duodenoscope along the greater curvature of the stomach to “relax” the gastrojejunal anastomosis and thus differentiate the “upper entrance” from the “lower entrance.” The efferent loop makes a better entrance for the duodenoscope because it is less angulated than the afferent loop. Thus, this route is useful for increasing the success rate of the enterography procedure. Many endoscopists attempt to enter the afferent loop via the site of the gastrojejunal anastomosis, but the sharp angulation caused by adhesions may make it impossible to advance the endoscope to the afferent loop. Premature entry into the afferent loop at the gastrojejunal anastomosis is the main cause of failure to access the papilla. Three stomal openings can be visualized endoscopically at the site of the Braun anastomosis, but identifying the correct entrance is a major challenge. The “middle entrance” is the entrance to the loop that can be used to reach the papilla of Vater when the endoscope is advanced from the efferent loop and is invariable irrespective of the endoscopic approach used. We recommend extending the duodenoscope along the greater curvature of the stomach until the gastrojejunal anastomosis, then advancing the endoscope through the “lower entrance”, along this efferent loop to the Braun anastomosis, and the “middle entrance” is the correct entrance to reach the papilla of Vater. For patients with Billroth II gastroenterostomy and Braun anastomosis, We believe that this is the optimal ERCP enterography route (Figure 6)[8].
As in patients with normal anatomy[9,10], anterior oblique-viewing endoscopes[11,12], side-viewing endoscopes[3,13-16], forward-viewing gastroscopes[17], and multibending endoscopes[18] have been reported in previous studies on ERCP for those patients with prior Billroth II gastrectomy. It was reported that the success rate of reaching the papilla of Vater ranges from 63% to 92%[1,2,4,15,19]. In our study, the overall success rate in reaching the papilla was 86.2%, and 82.6% patients had therapeutic success using a conventional duodenoscope for ERCP, which is a little better than and quite comparable with the success rates in previous reports. In patients who have had a Braun anastomosis, the ERCP failure rate is reported to be 70%[1]. A long afferent loop and the Braun anastomosis are the main reasons of failure in accessing the papilla. To solve these altered anatomy challenges, a stiffer endoscope along with manual compression has been used to access the papilla. It has been suggested to increase the success rate in accessing the papilla and avoiding loop formation at the ligament of Treitz[1]. Insufficient stiffness of the endoscope may be an important cause of failure in accessing the papilla. Instruments such as a polypectomy snare can be placed into the endoscope to increase the overall stiffness during intubation. Alternative methods such as cap-assisted or double-balloon endoscopy can also improve the ERCP success rate in those patients with Billroth II gastrectomy and Braun anastomosis[20,21]. In our technique, the guidewire of the retrieval balloon is advanced to the right limb. Subsequently, a retrieval balloon is inserted over the guidewire. We use this retrieval balloon to explore the right limb by using contrast enhancement to observe the tract of the limb on the radiographic images. The balloon is hooked to the duodenal limb which is inflated, and not only indicates the direction of the tract to guide the endoscope forward but also facilitates the forward movement of the endoscope with fewer injuries to the intestinal wall. While the balloon catheter is strongly retracted into the working channel to allow the scope to advance, the endoscope is then propelled slightly forward. By laying it on the right limb, the retrieval balloon catheter could also be used as a guide to prevent the duodenoscope from sliding out of the right limb into another limb upon forward motion. After successful access of the right limb is achieved, the retrieval balloon becomes visible within the tract ahead, instead of emerging from it. This is particularly important at the Braun anastomosis site, where 3 stomal openings can be endoscopically identified; thus, retrieval-balloon-assisted enterography could ensure the success of ERCP. For patients with a Billroth II gastroenterostomy and Braun anastomosis, the overall success rate in reaching the papilla was 85%, and the therapeutic success rate was 80%in this study.
We recommend extending the duodenoscope along the greater curvature of the stomach to the gastrojejunal anastomosis, then advancing the endoscope through the “lower entrance”, along this efferent loop to the Braun anastomosis, and the “middle entrance” is the correct entrance to reach the papilla of Vater. For patients with Billroth II gastroenterostomy and Braun anastomosis, we believe that this is the optimal ERCP enterography route. Retrieval-balloon-assisted enterography along the optimal route may improve the ERCP success rate in these patients. This study was retrospective, reflecting the experience of a single center and suggesting that the reproducibility of this technique should be assessed in prospective studies in the future.
Endoscopic retrograde cholangiopancreatography (ERCP) is very practical in pancreaticobiliary disease management in patients with normal anatomy and surgically altered anatomy. The success rate was reported to be 83% in patients with a Billroth II gastroenterostomy but only 29% with a Billroth II gastroenterostomy and an additional Braun anastomosis. ERCP failure in such patients was caused by difficulties in entering the afferent loop and accessing the papilla. In this retrospective study, we described the use of retrieval-balloon-assisted enterography along an optimal route in challenging patients with a Billroth II gastroenterostomy and Braun anastomosis.
Anterior oblique-viewing endoscopes, side-viewing endoscopes, forward-viewing gastroscopes, and multibinding endoscopes have been used in most studies on ERCP for patients with prior Billroth II gastrectomy. The success rate of reaching the papilla is 63%-92%. In patients who have had a Braun anastomosis, ERCP failure rate is reported to be 70%.
The authors reported the use of a wire-guided retrieval balloon to remove common bile duct stones and facilitate endoscope insertion for successful ERCP in post-gastrointestinal surgery patients. They termed the procedure retrieval-balloon-assisted enterography. They believe that retrieval-balloon-assisted enterography along an optimal route may improve the ERCP success rate in patients with a Billroth II gastroenterostomy and Braun anastomosis.
Retrieval-balloon-assisted enterography along the optimal route may improve the ERCP success rate in patients with a Billroth II gastroenterostomy and Braun anastomosis.
Braun anastomosis is an anastomosis between the afferent and efferent loops of the jejunum after a loop gastroenterostomy.
This manuscript is a retrospective study and the sequel of a prior publication. The technique is very interesting and the results are very encouraging but it reflects only a single center experience. For this reason the results are not valid but it would be interesting to start a prospective study on this topic to valid the procedure. However, the study suggests a new therapeutic possibility to perform ERCP in patients with Billroth II that can be reproduced in other Centers and for this reason it could be published.
P- Reviewer: Bove A, Camellini L, Fabozzi M, Lorenzo-Zuniga V, Perazzo H S- Editor: Qi Y L- Editor: Cant MR E- Editor: Ma S
| 1. | Ciçek B, Parlak E, Dişibeyaz S, Koksal AS, Sahin B. Endoscopic retrograde cholangiopancreatography in patients with Billroth II gastroenterostomy. J Gastroenterol Hepatol. 2007;22:1210-1213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 48] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 2. | Hintze RE, Veltzke W, Adler A, Abou-Rebyeh H. Endoscopic sphincterotomy using an S-shaped sphincterotome in patients with a Billroth II or Roux-en-Y gastrojejunostomy. Endoscopy. 1997;29:74-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 48] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 3. | Kim MH, Lee SK, Lee MH, Myung SJ, Yoo BM, Seo DW, Min YI. Endoscopic retrograde cholangiopancreatography and needle-knife sphincterotomy in patients with Billroth II gastrectomy: a comparative study of the forward-viewing endoscope and the side-viewing duodenoscope. Endoscopy. 1997;29:82-85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 82] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 4. | Faylona JM, Qadir A, Chan AC, Lau JY, Chung SC. Small-bowel perforations related to endoscopic retrograde cholangiopancreatography (ERCP) in patients with Billroth II gastrectomy. Endoscopy. 1999;31:546-549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 94] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 5. | Zhuang M, Zhang W, Gu J, Gong W, Wang X. ERCP with retrieval balloon-assisted enterography using traditional duodenoscope in post-GI surgery patients. Gastrointest Endosc. 2013;77:315-316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Zhuang M, Zhang WJ, Gu J, Liu YB, Wang XF. Retrieval-balloon-assisted enterography in post-pancreaticoduodenectomy endoscopic retrograde cholangiopancreatography. World J Gastroenterol. 2012;18:7109-7112. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Lin LF, Siauw CP, Ho KS, Tung JC. ERCP in post-Billroth II gastrectomy patients: emphasis on technique. Am J Gastroenterol. 1999;94:144-148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 57] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 8. | Wu WG, Gu J, Zhang WJ, Zhao MN, Zhuang M, Tao YJ, Liu YB, Wang XF. ERCP for patients who have undergone Billroth II gastroenterostomy and Braun anastomosis. World J Gastroenterol. 2014;20:607-610. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 11] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 9. | Eckardt AJ, Veltzke-Schlieker W, Hintze RE, Wiedenmann B, Adler A. ERCP in the sitting position--an alternative technique with potential benefits (with video). Surg Laparosc Endosc Percutan Tech. 2010;20:247-249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 10. | Ricci E, Bertoni G, Conigliaro R, Contini S, Mortilla MG, Bedogni G. Endoscopic sphincterotomy in Billroth II patients: an improved method using a diathermic needle as sphincterotome and a nasobiliary drain as guide. Gastrointest Endosc. 1989;35:47-50. [PubMed] |
| 11. | Sen-Yo M, Kaino S, Suenaga S, Uekitani T, Yoshida K, Harano M, Sakaida I. Utility of the Anterior Oblique-Viewing Endoscope and the Double-Balloon Enteroscope for Endoscopic Retrograde Cholangiopancreatography in Patients with Billroth II Gastrectomy. Gastroenterol Res Pract. 2012;2012:389269. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Nakahara K, Horaguchi J, Fujita N, Noda Y, Kobayashi G, Ito K, Obana T, Takasawa O. Therapeutic endoscopic retrograde cholangiopancreatography using an anterior oblique-viewing endoscope for bile duct stones in patients with prior Billroth II gastrectomy. J Gastroenterol. 2009;44:212-217. [PubMed] |
| 13. | Forbes A, Cotton PB. ERCP and sphincterotomy after Billroth II gastrectomy. Gut. 1984;25:971-974. [PubMed] |
| 14. | Osnes M, Rosseland AR, Aabakken L. Endoscopic retrograde cholangiography and endoscopic papillotomy in patients with a previous Billroth-II resection. Gut. 1986;27:1193-1198. [PubMed] |
| 15. | Hintze RE, Adler A, Veltzke W, Abou-Rebyeh H. Endoscopic access to the papilla of Vater for endoscopic retrograde cholangiopancreatography in patients with billroth II or Roux-en-Y gastrojejunostomy. Endoscopy. 1997;29:69-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 146] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 16. | Bergman JJ, van Berkel AM, Bruno MJ, Fockens P, Rauws EA, Tijssen JG, Tytgat GN, Huibregtse K. A randomized trial of endoscopic balloon dilation and endoscopic sphincterotomy for removal of bile duct stones in patients with a prior Billroth II gastrectomy. Gastrointest Endosc. 2001;53:19-26. [PubMed] |
| 17. | Anastassiades CP, Salah W, Pauli EM, Marks JM, Chak A. Cap-assisted ERCP with a forward-viewing gastroscope as a rescue endoscopic intervention in patients with Billroth II anatomy. Surg Endosc. 2013;27:2237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Koo HC, Moon JH, Choi HJ, Ko BM, Hong SJ, Cheon YK, Cho YD, Lee JS, Lee MS, Shim CS. The utility of a multibending endoscope for selective cannulation during ERCP in patients with a Billroth II gastrectomy (with video). Gastrointest Endosc. 2009;69:931-934. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 19. | Yao W, Huang Y, Chang H, Li K, Huang X. Endoscopic Retrograde Cholangiopancreatography Using a Dual-Lumen Endogastroscope for Patients with Billroth II Gastrectomy. Gastroenterol Res Pract. 2013;2013:146867. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 20. | Koshitani T, Matsuda S, Takai K, Motoyoshi T, Nishikata M, Yamashita Y, Kirishima T, Yoshinami N, Shintani H, Yoshikawa T. Direct cholangioscopy combined with double-balloon enteroscope-assisted endoscopic retrograde cholangiopancreatography. World J Gastroenterol. 2012;18:3765-3769. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 17] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 21. | Park CH, Lee WS, Joo YE, Kim HS, Choi SK, Rew JS. Cap-assisted ERCP in patients with a Billroth II gastrectomy. Gastrointest Endosc. 2007;66:612-615. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 48] [Article Influence: 2.7] [Reference Citation Analysis (0)] |