INTRODUCTION
Black hairy tongue (BHT) is an acquired, benign condition characterized by the appearance of abnormally hypertrophied and elongated filiform papillae on the dorsal surface of the tongue. The name is a misnomer and comes from its classical presentation as a superficial black and hairy carpet-like lingual growth (Figure 1). Hairy tongue may also appear brown, yellow, green, blue, or even unpigmented (Figure 2)[1-3]. BHT typically causes aesthetic concerns to the patient and leads to frequent physician visits. It may, however, be rarely associated with gagging, nausea, dysgeusia, xerostomia, burning mouth syndrome and halitosis in some patients[4-6] a constellation of symptoms that, in clinical practice, frequently leads to an evaluation by a gastroenterologist.
Figure 1 Classic black hairy tongue.
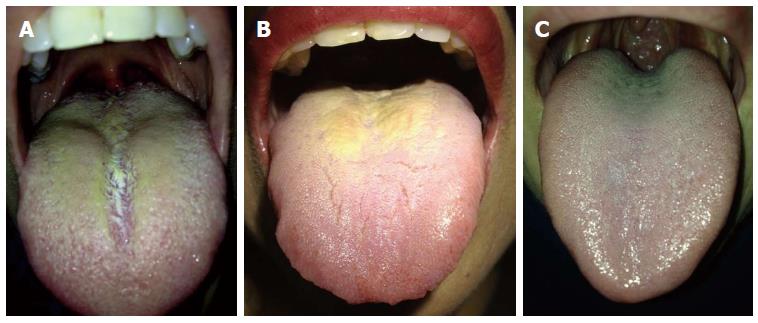
Figure 2 Palette variations of hairy tongue (A and B), Normal tongue (C).
Originally described by Amatus Lusitanus in 1557 as hairs on the tongue that would regrow upon being removed, BHT has also been referred to as hyperkeratosis of the tongue, lingua villosa nigra, nigrites linguae, keratomycosis linguae, and melanotrihia lingua[3,6,7]. Its etiology and pathophysiology have not been fully elucidated and are likely multifactorial. Male sex, older age, smoking, alcohol use, poor oral hygiene, and certain medications place patients at higher risk for developing BHT. Visual inspection is often sufficient for diagnosis. Overall prognosis is excellent as the disease is largely self-limiting and rarely requires procedural intervention.
In this latest review, we discuss the epidemiology, pathophysiology, etiology, clinical presentation, differential diagnoses, management, complications, and finally prognosis of BHT.
EPIDEMIOLOGY
Review of the medical literature shows that BHT is not uncommon. A large cross-sectional study of 5150 Turkish dental outpatients has reported an overall prevalence of 11.3% with increased rates in men (18%) compared to women (6%)[8]. However, a cross-sectional study of 1901 Iranian dental patients only reported a prevalence of 1.2%[9]. BHT occurred in 0.6% of Minnesota school-aged children in contrast to 8.4% patients in a young Finnish population[10-12]. Discordance of the observed rates may stem from difference patient’s demographics (age, sex, ethnicity, practices and habits) and interobserver variability in defining lesions in corresponding study populations.
Selected populations are at a higher risk of developing BHT. Patients with oncological disorders, smokers, black tea drinkers, and those with poor oral hygiene are more likely to develop BHT[8]. BHT also shows clear gender and age predilection. Men are about three times more commonly affected than women[8,9,13]. This can be attributed to greater prominence of smoking and higher rates of poor oral hygiene in males. This difference is offset in Finland, where smoking rates have been declining among men and young women are slightly more likely to be affected with BHT[10,14]. In addition, BHT is positively correlated with increasing age with some studies showing a prevalence of nearly 40% in patients over the age of 60[8], though cases have been reported in patients as young as 2-mo-old[2,15]. Although uncommon, in elderly patients, additional tongue conditions associated with BHT may include fissured tongue (12%) and macroglossia (4%)[8]. Advanced age, poor general condition as well as selected neurological disorders affecting tongue movement and mastication place a patient at a higher risk of developing BHT, largely due to the limited effective friction that results in desquamation of the keratinized layers of the filiform papillae. Finally, globally, there may also be geographic deviations in the prevalence of BHT due to differences in oral hygiene habits and dietary patterns, and variation in oral flora.
ANATOMY AND PATHOPHYSIOLOGY
The tongue is a highly muscular organ located in the oropharynx. It consists of a root, an apex, a curved dorsum, and an inferior surface. The muscles of the tongue are mainly innervated by the hypoglossal nerve, with a small contribution from the pharyngeal plexus[16]. Somatosensory innervation of the tongue is also divided between two nerves. The lingual branch of mandibular division of the trigeminal nerve innervates the anterior two-thirds of the tongue while the glossopharyngeal nerve innervates the posterior third of the tongue. Finally, the lingual artery and its branches supply blood to most of the tongue[16].
BHT typically affects the dorsum of the tongue, which is divided into the oral (presulcal) part and the pharyngeal (postsulcal part) by the V-shaped sulcus terminalis. The dorsal epithelium is lined by non-keratinized stratified squamous epithelium posteriorly and fully keratinized epithelium anteriorly. The dorsal mucosa is directly attached to the underlying muscle with no interposed submucosa. The underlying lamina propria is composed of dense fibrous connective tissue with numerous vessels and nerves supplying papillae. Lingual papillae are protrusions of dorsal mucosa on the presulcal part of the tongue[16].
The four main types of lingual papillae are filiform, fungiform, foliate, and circumvallate papillae. Filiform papillae densely cover most of the presulcal dorsal tongue and are predominately affected in BHT. They are small conical or cylindrical protrusions consisting of a central body surrounded by numerous threadlike cornified projections termed secondary papillae. They function to increase friction between the tongue and food and move particles within oral cavity[16,17].
The pathophysiology of BHT has not been fully elucidated. It is thought to arise from defective desquamation of the dorsal surface of the tongue. This then prevents normal debridement, leading to accumulation of keratinized layers[17]. The resulting hypertrophy and elongation of the filiform papillae appear hairlike superficially. Normally less than 1 mm in length, the elongated papillae can reach a length of 12-18 mm and width of 2 mm[3,4,8,18]. These then secondarily collect fungi, bacteria, and debris[19]. This collection can include residue from tobacco, coffee, tea, and other foods as well as porphyrin-producing chromogenic organisms in the oral flora, which lend the lesion a characteristic hue[7,19]. Using antikeratin probes on BHT epithelium, Manabe et al[17] found that the “hairs” are highly elongated cornified spines that result from delayed desquamation of the cells in the central column of filiform papillae and marked retention of secondary papillary cells that expressed hair-type keratins.
ETIOLOGY
The etiology of BHT remains unclear and is likely multifactorial, resulting from combination of local and systemic insults. Various palette appearance of the hairy tongue likely originates in differences in potentially contributing extrinsic (environmental) and intrinsic (chromogenic oral microflora) factors[2]. Although casual smoking poses a slightly increased risk of having BHT compared to non-smokers (15% to 10% in men, 5.5% to 5.2% in women), heavy use of tobacco leads to estimated prevalence of 58% in men and 33% in women[8]. Similar to smoking, heavy black tea consumption lead to increased prevalence of BHT in both male and female patients[8]. Alcohol and intravenous drug use, excessive coffee consumption, poor oral hygiene, general debilitation, and recent radiation therapy to the head and neck region are important risk factors that predispose some patients to develop BHT[6,8,12,20]. Prolonged use of oxidizing mouthwashes containing sodium perborate, sodium peroxide, and hydrogen peroxide has also been associated with the development of BHT[18]. Dietary consumption of herbal tea and sugars may lead to lowering pH on the dorsum of the tongue promoting chromogenic bacterial overgrowth[2]. Most recently, a number of cases of BHT have been reported after allogenic stem-cell transplantation as a cutaneous presentation of graft-versus-host-disease[21]. Finally, prevalence of BHT is increased in malignancies, with one study showing rates as high as 30% in men and 18% in women[22]. Debates on causative relationship between microbial infection and development of BHT date back to 1869 paper by Dr. Raynau, and although previously linked to the presence of various microbial agents, including Candida and Aspergillus species in the oral cavity, microflora found in BHT may be largely coincidental rather than causative[18,23,24].
Use of systemic and local medications has been commonly implicated in the development of BHT. Antibiotics, including penicillin, aureomycin, erythromycin, doxycycline, and neomycin are most often associated with this disorder[3,4,6,25,26]. However, it should be noted that the cause and effect factor between antibiotics and development of black hairy tongue needs to be further elucidated. Specifically, local or systemic antibiotic use may significantly alter oral flora, thus potentially predisposing the patient to develop BHT. On the other hand, pronounced anatomical alteration in the filiform papillae may predispose the patient to trap foreign material and stimulate local microbial overgrowth that leads to typical color changes seen in patients with this condition. Importantly, earlier studies linking BHT to the use of antibiotics reported local (aerosol or lozenges) oral penicillin use, a type of medication not used in today’s medical practice[6]. Additionally, xerostomie agents, including antipsychotics (olanzapine and chlorpromazine) may predispose patients to develop BHT[27,28]. Particular care should be delegated in identifying local inciting factors in the development of BHT, including recent use of new toothpaste or mouthwash[6]. Interestingly, a case of BHT was also reported after four days of erlotinib treatment in a patient with advanced lung cancer, possibly due to an unclear interruption of epidermal grown factor and its receptor in the lingual epithelium[29].
Other diseases and medical conditions associated with BHT include HIV, advanced cancer, and general body illness[6,22]. In addition, BHT has been reported in patients with trigeminal neuralgia. This painful condition, associated with poor oral intake and decreased mastication, is thought to limit tongue movement, resulting in decreased tongue friction with food, palate, and teeth and ultimately hindering normal desquamation of the keratinized filiform papillae, thus leading to the development of BHT[30].
CLINICAL PRESENTATION
A typical patient with BHT is an elderly male smoker on antibiotics or antipsychotics with poor oral hygiene, who presents with painless black hair-like lesion on the dorsum of the tongue anterior to the circumvallate papillae. It generally does not occur on the tip or sides of the tongue. Although recognized for its distinctive black color, its hue can range from blackish-brown to yellow-green to unpigmented[7,12]. BHT is generally asymptomatic, though metallic taste, dysgeusia, burning mouth, halitosis, and even gagging have been reported in some patients[31]. Submandibular or cervical lymphadenopathy may occasionally be present in selected cases[2]. Review of systems may be significant for chronic pain, major physical disabilities, psychiatric illnesses, or other debilitating symptoms that preclude the maintenance of proper oral hygiene and normal tongue movement. Other associated clinical conditions include smoking, advanced malignancy, psychiatric conditions, and trigeminal neuralgia. Physical exam is unremarkable aside from the hairy appearing tongue lesion itself. Associated laboratory findings may include positive fungal cultures, HIV test, and blood and urine toxicology studies.
DIFFERENTIAL DIAGNOSIS
Classic BHT presents as a black, hairy-appearing lesion on the dorsum of the tongue (Figure 1). Differential diagnosis includes “pseudo-hairy tongue”, oral hairy leukoplakia, pigmented fungiform papillae of the tongue and acanthosis nigricans[31]. “Pseudo-black hairy tongue” (Figure 3) appears as a darkly stained tongue in absence of elongated filiform papillae seen in BHT. Foods, tobacco, and drugs, including antibiotics, antidepressants, and bismuth salicylate, can cause this condition[6,26,32-34]. Oral hairy leukoplakia can be seen in the immunocompromised patients and has a white plaque appearance on the dorsal and ventral surfaces of the tongue, as well as buccal mucosa, and gingiva. Pigmented (due to melanin laden macrophages) fungiform papillae are rare, characterized by isolated hypertrophied lesions primarily on the lateral aspect and apex of the tongue that has a predilection to dark skinned patients. Acanthosis nigricans in the oral cavity manifests as multiple dark and demarcated papillary lesions on the dorsum and lateral region of the tongue with frequent labial involvement and may be associated with underlying malignancy[31]. Detailed history and physical exam is essential to arriving at the correct diagnosis, with particular emphasis on identifying known etiologic factors. If dubious, biopsy specimens may be required to exclude “mimicking” conditions and confirm the diagnosis. In infants, congenital lingual melanotic macules and congenital melanocytic nevi should be sought for and diligently excluded[2].
Figure 3 Pseudo black hairy tongue with bismuth salicylate use.
CLINICAL DIAGNOSIS
The diagnosis of BHT primarily relies on a visual intraoral examination. BHT shows a predilection for the dorsal tongue, anterior to the circumvallate papillae and sulcus terminalis. Microscopic examination may be used as an adjunct to diagnosis; demonstrating elongated filiform papillae on the dorsal tongue more than 3 mm in length. Cultures may be considered to rule out superimposed bacterial or fungal infections associated with BHT[35]. Tongue biopsy is supportive but not usually required if the lesion appears characteristic for BHT and responds to mechanical debridement. Careful review of known precipitating factors and recent medication changes is also fundamental in the diagnosis of BHT.
MANAGEMENT
BHT is generally a self-limiting disease and carries a good prognosis. General preventative strategies should be employed and the patient should be educated of this condition as a potential side effect of antibiotic and antipsychotic medications. Care should be taken to promote comprehensive daily oral hygiene. After the diagnosis, a thorough medical history and physical examination are essential in establishing causative relationship to potential environmental triggers and excluding other mimickers of the disease. Proper patient reassurance to the benign nature of BHT is important, both to decrease the level of aesthetic anxiety and to promote appropriate treatment. The goal of therapy is the discontinuation of potential offending agents (including dietary or medicinal causes) and modifying predisposing factors (smoking, black tea consumption, neurological conditions, general debilitation), followed by maintaining good oral hygiene and gentle debridement with a soft toothbrush or tongue scraper to promote desquamation of the hyperkeratotic papillae. Topical application of baking soda or rinsing with diluted hydrogen peroxide solution may help improve desquamation of the keratinized filiform papillae and bleach the color. Lifestyle modifications, including aggressive oral hydration are important and increased dietary consumption of raw fruits and vegetables may help improve this condition by facilitating the roughage on the tongue[27]. Anecdotal use of antimicrobial therapies, topical triamcinolone acetonide, gentian violet, salicylic acid, vitamin B complex, thymol, and topical or oral retinoids (e.g., isotretinoin), as well as keratin olytics (podophyllin), topical 30% urea solution, and trichloroacetic acid have been reported in the literature, although potential side effects from local irritation and possible systemic absorption are important factors to consider[1,2,18,24,36-38]. Yogurt and probiotic supplementation may be employed with various degree of success. Candida associated glossopyrosis should be treated with antifungal medications. Routine use of proton pump inhibitors is not indicated, although may be of benefit in cases with concomitant severe gastroesophageal reflux disease. Dental evaluation may be indicated in challenging cases, although this is rare. Resistant BHT may require clipping or removal of the papillae by electrodessication or carbon dioxide laser[31].
COMPLICATIONS
Typically, BHT is a self limiting disorder and the development of this condition commonly precipitates only aesthetic concern in affected people. Patients should be reassured about the benign nature of the condition to address anxiety and promote recognition and treatment. In rare instances, patients may report irritation, nausea, and gagging sensation mainly due to the size of unusually elongated papillae. Others may experience a disabling metallic taste, general dysgeusia, and perceived halitosis[18]. Microbial or fungal superinfection is an important consideration in management patients with BHT and proper recognition and treatment may preclude progression to glossopyrosis or burning mouth syndrome.
PROGNOSIS
The long-term outcomes for BHT are excellent as the disease is benign and may even improve spontaneously. Review of the literature shows prompt resolution of this condition within days to few weeks after mechanical debridement and removal of a suspected precipitating agent. Patient education on proper oral hygiene and lifestyle modifications including smoking cessation and alcohol abstinence are vital to preventing reoccurrence. The development of BHT does not typically cause any sequelae. Other co-existing clinical conditions associated with BHT (xerostomia, HIV, cancer, and trigeminal neuralgia) should be sought for and managed appropriately as well to reduce the risk of BHT reappearance.
CONCLUSION
BHT is a relatively common disease that classically manifests as a black and hairy appearing lesion on the dorsum of the tongue arising from abnormally hypertrophied and elongated filiform papillae. Striking as it may appear, this benign condition is usually asymptomatic and its apparent presentation typically triggers only local aesthetic concerns. Rarely, BHT can be accompanied by metallic taste, halitosis, burning mouth, and gagging. Its etiology and pathophysiology continue to be evolving and are undoubtedly multifactorial. Male gender, advanced age, smoking, alcohol abuse, excessive black tea or coffee consumption, HIV, debilitated general condition, and malignancy places patients at a higher risk for developing BHT. Visual inspection and thorough medical history establishes correct diagnosis, although microscopic examination, cultures of tongue swabs, and tongue biopsies may be of additional value in challenging cases. Patients with BHT typically present with indolent self-limited course that responds well to local treatment. Management is primarily focused on mechanical debridement, maintenance of proper oral hygiene, and removal of potential causative agents. Overall clinical prognosis of BHT is excellent.
P- Reviewer: Leonard NJ, Liu ZW S- Editor: Qi Y L- Editor: A E- Editor: Ma S