Published online Jun 28, 2014. doi: 10.3748/wjg.v20.i24.7979
Revised: February 9, 2014
Accepted: March 19, 2014
Published online: June 28, 2014
Processing time: 191 Days and 9.4 Hours
We report the case of a 25-year-old male with Neurofibromatosis type I (NF-1), who presented at the time of admission with clinical findings of an acute abdomen caused by a mechanical obstruction. Computerized tomography showed a volvulus of the terminal ileum with mesenteric swirling as the cause of the patient’s symptoms. Consecutive exploratory laparotomy confirmed the diagnosis and 70 cm of the small intestine was resected due to an affection of the mesentery by multiple neurofibromas. The gastrointestinal tract is affected in approximately 10% of patients with NF-1, however the mesentery is almost always spared. Here we describe the unique case of a patient with a volvulus caused by mesenteric manifestation of von Recklinghausen’s disease, emphasizing the role of surgery in a team of multidisciplinary specialists to treat this multiorganic disease.
Core tip: Neurofibromatosis type I (NF-1) is one of the most common single gene disorders known for its phenotypical presentation with café au lait macules and neurofibromas. Although every organ system can be involved, the intra-abdominal manifestation is rare. To the best of our knowledge, this is the first reported case of a patient with mesenteric involvement of NF-1 manifesting as a volvulus, underscoring the role of surgery in this heterogeneous disease.
- Citation: Werner TA, Kröpil F, Schoppe MO, Kröpil P, Knoefel WT, Krieg A. Small bowel volvulus as a complication of von Recklinghausen’s disease: A case report. World J Gastroenterol 2014; 20(24): 7979-7983
- URL: https://www.wjgnet.com/1007-9327/full/v20/i24/7979.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i24.7979
Neurofibromatosis type I (NF-1), also named von Recklinghausen’s disease after its first describer German pathologist Friedrich Daniel von Recklinghausen, is a genetic disorder caused by a mutation of the NF1-gene. This genetic alteration can either be inherited through an autosomal dominant lineage, as observed in 50% of the cases, or it results through de novo spontaneous mutations of NF1. Approximately 1 in 3000 persons worldwide is affected[1]. The mutation results in an inactivation of the tumor suppressor neurofibromin, which normally functions as a negative regulator of Ras kinase, accelerating the conversion of activated Ras-GTP to inactivated Ras-GDP and thereby controlling cellular growth and differentiation[2].
The medical condition of NF-1 is diagnosed according to the National Institutes of Health Consensus Development Conference criteria (Table 1)[3]. The cardinal clinical features are café au lait spots and benign cutaneous neurofibromas, enabling a visual diagnosis in adulthood. These clinical findings and phenotypic traits can differ widely between individuals making it a heterogeneous disease. Other clinical symptoms include axillary or inguinal freckling, gliomas of the optic nerve, two or more Lisch nodules of the iris and specific lesions of the skeletal system, including sphenoid dysplasia and pseudarthrosis, preferentially affecting the tibia. A first-degree relative diagnosed with NF-1 is another sign pointing towards the diagnosis. If two or more of these findings are present the criteria are fulfilled and the diagnosis established.
| Diagnostic criteria of NF1 |
| ≥ 2 criteria are needed |
| Six or more café au lait macules |
| > 5 mm in prepubertal individuals |
| > 15 mm in postpubertal individuals |
| Two or more neurofibromas of any type or one plexiform neurofibroma |
| Freckling in the axillary or inguinal regions |
| Optic glioma |
| Two or more Lisch nodules |
| A distinctive osseous lesion |
| Sphenoid dysplasia |
| Thinning of long bone cortex with or without pseudoarthrosis |
| A first-degree relative with NF1 by the above criteria |
Besides the characteristics described above, NF-1 can affect nearly every organ system and is additionally associated with malignant and benign tumors such as pheochromocytoma and malignant peripheral nerve sheath tumor (MPNST). The frequency of an intra-abdominal manifestation of the disease varies greatly in the literature, ranging between 5%-20%. Most of the intra-abdominal findings are incidental, with only 5% of the affected patients reporting clinical symptoms. Although the vast majority of patients are asymptomatic, one quarter requires further surgical intervention in their lifetime, making the intra-abdominal manifestation of NF-1 a challenging disease for both patient and clinician[4].
A 25-year-old male presented to our department with worsening abdominal pain, nausea and vomiting for the past two days. He had a known history of von Recklinghausen’s disease with multiple café au lait spots and cutaneous neurofibromas as well as axillar and inguinal freckling. His abdominal condition thus far had been unremarkable with no prior surgery and no history of altered bowel habits or abdominal discomfort.
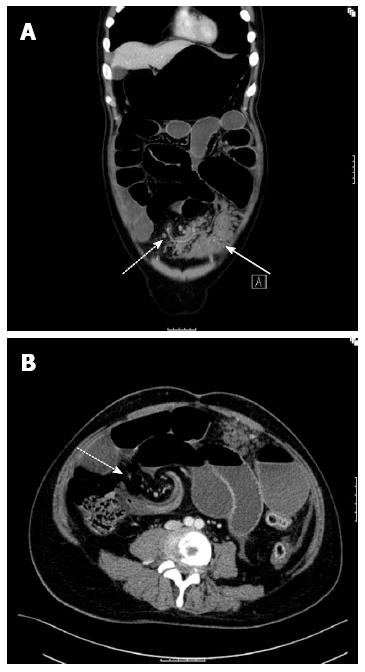
During clinical examination the abdomen appeared excessively distended with generalized tenderness, but no signs of muscular guarding or peritonitis. No bowel sounds were audible. In the ultrasound examination small collections of free intra-abdominal fluid were seen, together with grossly bloated bowel loops. With the clinical picture of a mechanical obstruction a computer tomography (CT) was preformed to identify the underlying pathology. The CT-scan revealed the typical findings of a mechanical obstruction caused by a volvulus located at the terminal ileum, showing the characteristic whirlpool-sign and prestenotic dilation of the small intestine (Figure 1). In addition, a tumorous mass directly adjacent to the mesenteric root could be identified as the cause of the volvulus (Figure 1B).
The patient was taken to the operating theatre and an exploratory laparotomy was performed. The intraoperative findings confirmed the initial diagnosis. In direct proximity to the volvulus we found a vast nodular tumorous infiltration within the mesenteric fat involving 60-70 cm of the ileum. The tumorous mass was reaching right up to the mesenteric root, rendering the affected bowel segment completely immobile. Inspection of the entire abdominal cavity revealed no other tumorous lesions.
After reposition of the volvulus no visual signs of ischemia were present. However, because of the fixed anchorage of the mesentery and consecutive inflexibility of the affected small bowel, a segmental resection including the infiltrated mesentery with end-to-end ileo-ileostomy was imperative. The postoperative period was uneventful and the patient was discharged within eight days.
Pathological examination revealed an area measuring 16 cm × 10 cm × 2.5 cm of affected mesenteric fat exhibiting nodular lesions respecting the organ margins and without any signs of infiltration of the adjacent serosa and free resection margins (Figure 2A). Histological findings were consistent with neurofibromatosis showing spindle cell-like growth patterns and a positive reaction for S100 but negative reaction for MIB-1 proliferation marker in the immunohistochemical investigations (Figure 2B). In addition, immunohistochemical staining of CD34, CD117 and synaptophysin were negative and thus excluded the differential diagnoses of gastrointestinal stromal tumor and ganglioneuroma (Figure 2B).
One year after surgery the patient is in a good healthy condition, showing no signs of post-operative complications. In an ultrasound examination no signs of an intra-abdominal recurrence were imminent. In the future further examinations will be conducted on a regular basis to ensure an early diagnosis of a relapse or secondary manifestations of his underlying disease.
The abdominal manifestation is present in approximately 10%-20% of the patients with NF-1-associated neoplasms[5]. They can be grouped into five different categories: neurogenic, neuroendocrine, non-neurogenic, embryonal and miscellaneous tumours[5]. Previously, for neurogenic tumors affecting the gastrointestinal tract a population-based prevalence of 2% has been reported[6]. Neurogenic tumors include localized and plexiform neurofibromas, as well as ganglioneuromas and malignant peripheral nerve sheath tumour (MPNST). The MPNST are the most common malignancies associated with NF-1 and arise in 10% from plexiform precursor lesions[2]. Ganglioneuromas on the other hand are benign tumors, which develop from sympathetic ganglia and are rarely associated with the intestine and generally found in the paraspinal region. The neurofibromas originate from peripheral nerves or the myenteric plexus, consisting of Schwann cells, fibroblasts and a myxoid matrix[1,7]. They are mostly found in the upper gastrointestinal tract, affecting the jejunum or the stomach. Their isolated localization at the ileal mesentery is extremely rare[8].
Most of these tumours are asymptomatic and are often found incidentally. However, when they increase in size, they can cause a myriad of non-specific signs and symptoms, with the most common being altered bowel habits, abdominal pain, chronic anemia due to occult bleeding or a palpable mass especially in younger patients[9]. Although complications caused by an obstructive tumor growth have been reported, particularly for intestinal wall associated neurofibromas, to our knowledge, this is the first report of mesenteric neurofibromatosis manifesting as a volvulus.
A preoperative CT-scan is a helpful diagnostic tool for an adequate assessment of the intra-abdominal pathology in patients with NF-1. Neurofibromas typically appear as smooth, nodular structures within the organ margins[5]. The imaging characteristics alone though are not specific enough to differentiate between a benign tumorous lesion and a malignant mass[10].
Surgery is a first line treatment in the management of complicated neurofibromatosis. Although surgery is not curative, it can reduce pain, enable normal bowel passage and prevent possible malignant transformation of plexiform neurofibromas to the MPNST, if the lesion is fully resected[5]. The plexiform neurofibromas are often demanding in their removal and a complete resection is sometimes not achievable, particularly if vital structures are involved and the growth is advanced[7].
In conclusion, NF-1 is a disease with many presentations, ranging widely in severity and location of manifestation. Since no definitive therapy exists, the prevention and treatment of its complications is the primary task for both patient and the clinical team. Here we report the first case of a patient with mesenteric involvement of NF-1 manifesting as a volvulus. Although surgery cannot cure NF-1, it most commonly remains the sole option in acute complications of this multiorganic disease.
A 25-years-old male with known von Recklinghausen’s disease presented with worsening abdominal pain, nausea and vomiting for the past two days.
Excessively distended abdomen with generalized tenderness in the absence of bowel sounds.
Constipation, intraabdominal adhesions, tumorous mass e.g., gastrointestinal stromal tumor, malignant peripheral nerve sheath tumor, appendicitis, inflammatory bowel disease.
WBC 13.50 × 109/L; HGB 10.20 gm/dL; CRP 15.6 mg/dL, metabolic panel and liver function test were within normal limits.
CT-scan showed a mechanical obstruction caused by a volvulus located at the terminal ileum, displaying the characteristic whirlpool-sign and prestenotic dilation of the small intestine as well as a tumorous mass directly adjacent to the mesenteric root.
Histological investigations of the tumor were consistent with neurofibromatosis showing spindle cell-like growth patterns and a positive reaction for S100 but negative reaction for MIB-1 proliferation marker in the immunohistochemical analysis as well as negative staining-results for CD34, CD117 and synaptophysin.
After exploratory laparotomy a segmental resection including the infiltrated mesentery with end-to-end ileo-ileostomy was performed.
The intra-abdominal manifestation of Neurofibromatosis type I (NF-1) is rare and normally presents itself with non-specific signs and symptoms like altered bowel habits, abdominal pain, chronic anemia due to occult bleeding or a palpable mass.
Immunohistochemistry is a laboratory method to detect proteins in tissue specimens using antigen-specific antibodies.
Mesenteric involvement in Neurofibromatosis type I is extremely rare but can lead to life threatening complications that demand urgent and decisive treatment.
This case report presents a rare abdominal complication of NF-1 (small bowel volvulus because of mesenteric neurofibromatosis) and reviews the manifestations, diagnosis and treatment of the disease. It is a good review of a rare complication.
P- Reviewers: Gaertner W, Tang HH S- Editor: Zhai HH L- Editor: A E- Editor: Zhang DN
| 1. | Williams VC, Lucas J, Babcock MA, Gutmann DH, Korf B, Maria BL. Neurofibromatosis type 1 revisited. Pediatrics. 2009;123:124-133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 456] [Cited by in RCA: 419] [Article Influence: 26.2] [Reference Citation Analysis (0)] |
| 2. | Jouhilahti EM, Peltonen S, Heape AM, Peltonen J. The pathoetiology of neurofibromatosis 1. Am J Pathol. 2011;178:1932-1939. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 113] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 3. | Tabarsi P, Merza MA, Marjani M. National Institutes of Health Consensus Development Conference Statement: neurofibromatosis. Bethesda, Md., USA, July 13-15, 1987. Neurofibromatosis. 1988;1:172-178. [PubMed] |
| 4. | Pinsk I, Dukhno O, Ovnat A, Levy I. Gastrointestinal complications of von Recklinghausen’s disease: two case reports and a review of the literature. Scand J Gastroenterol. 2003;38:1275-1278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 32] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 5. | Basile U, Cavallaro G, Polistena A, Giustini S, Orlando G, Cotesta D, Petramala L, Letizia C, Calvieri S, De Toma G. Gastrointestinal and retroperitoneal manifestations of type 1 neurofibromatosis. J Gastrointest Surg. 2010;14:186-194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 53] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 6. | Magro G, Piana M, Venti C, Lacagnina A, Ruggieri M. Solitary neurofibroma of the mesentery: report of a case and review of the literature. Pathol Res Pract. 2000;196:713-718. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Cavallaro G, Crocetti D, Pedullà G, Giustini S, Letizia C, De Toma G. Retrocaval mass in patient with von Recklinghausen disease: case report. G Chir. 2012;33:26-30. [PubMed] |
| 8. | Yano K, Okamura T, Yoshida Y, Osaki T, Ichiyoshi Y, Yasumoto K. Mesenteric neurofibroma with von Recklinghausen’s disease: a case report. Hepatogastroenterology. 1998;45:456-458. [PubMed] |
| 9. | Carter JE, Laurini JA. Isolated intestinal neurofibromatous proliferations in the absence of associated systemic syndromes. World J Gastroenterol. 2008;14:6569-6571. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 25] [Cited by in RCA: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 10. | Tonsgard JH, Kwak SM, Short MP, Dachman AH. CT imaging in adults with neurofibromatosis-1: frequent asymptomatic plexiform lesions. Neurology. 1998;50:1755-1760. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 102] [Article Influence: 3.8] [Reference Citation Analysis (0)] |