Published online Jun 28, 2014. doi: 10.3748/wjg.v20.i24.7752
Revised: November 28, 2013
Accepted: March 8, 2014
Published online: June 28, 2014
Processing time: 244 Days and 18 Hours
Capsule endoscopy (CE) has transformed investigation of the small bowel providing a non-invasive, well tolerated means of accurately visualising the distal duodenum, jejunum and ileum. Since the introduction of small bowel CE thirteen years ago a high volume of literature on indications, diagnostic yields and safety profile has been presented. Inclusion in national and international guidelines has placed small bowel capsule endoscopy at the forefront of investigation into suspected diseases of the small bowel. Most commonly, small bowel CE is used in patients with suspected bleeding or to identify evidence of active Crohn’s disease (CD) (in patients with or without a prior history of CD). Typically, CE is undertaken after upper and lower gastrointestinal flexible endoscopy has failed to identify a diagnosis. Small bowel radiology or a patency capsule test should be considered prior to CE in those at high risk of strictures (such as patients known to have CD or presenting with obstructive symptoms) to reduce the risk of capsule retention. CE also has a role in patients with coeliac disease, suspected small bowel tumours and other small bowel disorders. Since the advent of small bowel CE, dedicated oesophageal and colon capsule endoscopes have expanded the fields of application to include the investigation of upper and lower gastrointestinal disorders. Oesophageal CE may be used to diagnose oesophagitis, Barrett’s oesophagus and varices but reliability in identifying gastroduodenal pathology is unknown and it does not have biopsy capability. Colon CE provides an alternative to conventional colonoscopy for symptomatic patients, while a possible role in colorectal cancer screening is a fascinating prospect. Current research is already addressing the possibility of controlling capsule movement and developing capsules which allow tissue sampling and the administration of therapy.
Core tip: First introduced more than 10 years ago, capsule endoscopy has been a major technical innovation, directly influencing investigation and management of small bowel diseases. A vast quantity of research has been published during this time, firmly cementing capsule endoscopy as the investigation of choice for suspected diseases of the small bowel. Technology is swiftly progressing, supporting the broadening indications and clinical applications of capsule endoscopy. This review summarises the current position and main indications for small bowel, oesophageal and colon capsule endoscopy while providing detailed insights into the future of this exciting field of gastroenterology.
- Citation: Hale MF, Sidhu R, McAlindon ME. Capsule endoscopy: Current practice and future directions. World J Gastroenterol 2014; 20(24): 7752-7759
- URL: https://www.wjgnet.com/1007-9327/full/v20/i24/7752.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i24.7752
The introduction of capsule endoscopy (CE) in 2000 provided a new non-invasive means of imaging the, previously difficult to access, small bowel. A swallowable pill camera acquires images (subsequently converted to a video format on a computer) as peristalsis propagates it through the gastrointestinal (GI) tract. It is now established as the first-line investigation for diseases of the small bowel. Uptake has been swift in the United Kingdom with 91% of gastroenterologists using CE in a survey in 2010[1]. Promising data from newer capsules to image the oesophagus and colon suggest that the role and clinical application of CE will continue to expand, while interactive manoeuvrable capsules able to take biopsies or deliver targeted therapy are an exciting prospect on the horizon.
Although CE is generally considered a safe and straightforward procedure, there are a few limitations. CE is contraindicated in patients with swallowing disorders and known gastro-intestinal obstruction due to the risks of aspiration and retention of the capsule. Capsule retention is reported in up to 2% of procedures and risk factors include prolonged use of non-steroidal anti-inflammatory drugs, previous abdomino-pelvic irradiation and Crohn’s disease (CD)[2,3]. Occasionally the capsule may be retained in the stomach as a consequence of gastroparesis; specifically designed “capsule delivery systems” are available to deliver the capsule directly into the small bowel in such circumstances[4]. The concern with capsule retention is that it may lead to intestinal obstruction or perforation. In fact, it seems capsule retention is mostly asymptomatic and rarely causes obstruction[5,6]. In some cases one can follow an expectant approach, although future magnetic resonance imaging (MRI) examinations are contraindicated[7]. In most cases retrieval is eventually required and this can be done with medical, endoscopic or surgical methods[8,9]. There is a theoretical risk of interference with permanent pacemakers, and implantable cardiac defibrillators by the radiofrequency of the capsule and data recorder, however several studies have failed to demonstrate interference with a wide range of cardiac devices[10-12]. Finally, CE reporting can be a time consuming exercise for gastroenterologists and despite its worthy diagnostic potential, CE currently has no biopsy or therapeutic capability.
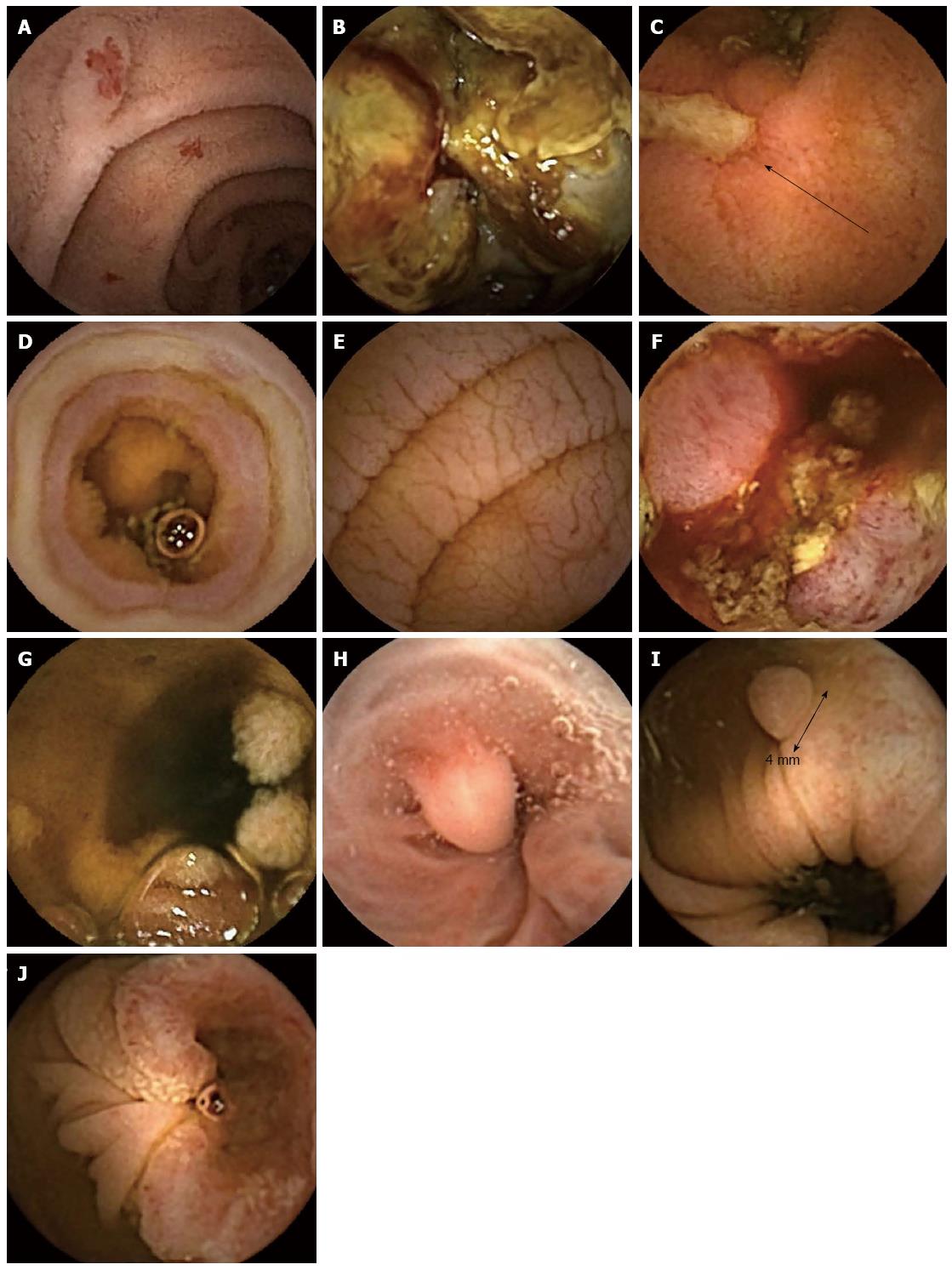
The commonest indication for small bowel CE is GI bleeding (obscure or overt), conventionally after non-diagnostic upper and lower GI endoscopic investigation. CE identifies pathology in 46%-60%[13] of such patients and is more sensitive than small bowel barium contrast radiology, small bowel computed tomography (CT), MRI, push enteroscopy and angiography[14]. Double balloon enteroscopy (DBE) has similar diagnostic yields to CE in this context[15] but is considerably more invasive, procedure times can be lengthy (1-2 h), sedation or general anaesthesia is often required and completion rates are less compared to CE (62.5% compared to 90.6% respectively; P < 0.05)[16]. As such DBE remains the interventional counterpart to CE, allowing direct visualisation, biopsy or therapy to abnormal areas already identified and located by CE. A recent meta-analysis demonstrated that the yield at DBE is significantly higher (75%) after a positive CE compared to after a negative CE (28%)[17]. Flat vascular lesions, angioectasia (Figure 1A) and inflammatory lesions are the most common findings while small bowel tumours (Figure 1B) account for 5%-9.6% of patients presenting with obscure gastrointestinal bleeding[18]. Factors associated with a higher diagnostic yield with CE include low haemoglobin measurements/transfusion dependence, older age and closer proximity of CE to the bleeding episode[19-22].
CE can be used to assist with diagnosis of CD or assessment of disease activity and extent in patients with known CD. CE has superior diagnostic yields to small bowel barium studies, ileo-colonoscopy, push enteroscopy and CT enterography in both suspected and established small bowel CD[23-25]. CE appears to be better than magnetic resonance enterography (MRE) at identifying small bowel mucosal lesions, while MRE is more accurate at diagnosing mural, peri-mural and extra-enteric manifestations[26,27]. With capsule retention occurring in 5%-13% of those with CD[3], small bowel MR is seen as the mainstay of investigation for those with established penetrating or stenosing disease as transmural involvement can be defined in cross section, but CE remains useful to assess mucosal activity. Radiology may not exclude short strictures in all cases[28] and therefore to confirm functional patency of the GI tract, a dissolving capsule (the same size and shape as the capsule endoscope) containing a radiofrequency tag has been developed (PillCam Patency capsule, Given Imaging, Yoqneam, Israel). Absence of the radio frequency signal 30 h post ingestion predicts safe GI transit of the capsule endoscope[29].
CE findings suggestive of CD can be rather non-specific and include ulceration, erythema, mucosal oedema and strictures (Figure 1C). This presents a significant challenge to the interpreting physician since minor mucosal breaks may occur in 10%-15% of normal individuals while mucosal erosions are present in two thirds of patients taking non-steroidal anti-inflammatory drugs[30]. Characteristics of small bowel injury due to nonsteroidal anti-inflammatory drugs (NSAIDs) include multiple petechiae, loss of villi, erosions, and ulcers with round, irregular, and punched-out shapes, and thus can be difficult to distinguish from CD endoscopically (Figure 1D)[31]. However, concentric diaphragmatic strictures are considered pathognomonic of NSAID mucosal injury and can present with obstructive symptoms. Endoscopic balloon dilatation is an effective strategy for such strictures since the muscularis propria remains intact leading to a low perforation rate[32,33].
Typical mucosal changes of coeliac disease such as scalloping, nodularity, loss of mucosal folds and mosaicism can be seen at CE (Figure 1E) with a sensitivity of 89% and specificity of 95% as reported in a recent meta-analysis[34]. Although CE may be considered in coeliac antibody positive patients unwilling to undergo endoscopy, duodenal biopsy remains the gold-standard for the diagnosis of coeliac disease. However, a recent study found CE useful in equivocal cases of coeliac disease, particularly in patients with antibody negative villous atrophy in whom findings either confirmed the suspected diagnosis or provided evidence of an alternative diagnosis such as CD[35]. CE may also be of benefit in those with known coeliac disease on a gluten free diet with on-going symptoms or alarm symptoms to exclude complications such as ulcerative jejunitis and small bowel lymphoma (Figure 1F)[36,37].
Most small bowel tumours present with anaemia or obscure GI bleeding, but may present late with abdominal pain or weight loss[38,39]. They include malignant or potentially malignant (gastrointestinal stromal tumours, adenocarcinoma, carcinoid, lymphoma), benign (haemangioma, hamartoma, adenoma, lipoma) and metastatic lesions (particularly from melanoma, lung, renal or breast primaries) (Figure 1F and G). CE is more accurate than small bowel barium radiology at detecting small bowel tumours and can also detect smaller lesions in comparison to MRI[3]. CE can miss some lesions which are largely submucosal and thus if there is a high index of suspicion, cross-sectional imaging such as a contrast enhanced CT scan is recommended[40,41]. CE and DBE are comparable for detecting small bowel tumours, while DBE has the advantage of biopsy plus therapeutic potential, such as stenting, balloon dilatation and localization prior to surgery[34].
Now in its second generation, PillCam Eso 2 (Given Imaging, Yoqneam, Israel) was introduced in 2008. Unlike the small bowel capsule it has a camera at both ends, acquiring simultaneous bidirectional images at a higher rate (14 compared to 2/s) to overcome rapid transit through the oesophagus. PillCam Eso has a reported sensitivity of up to 80% for diagnosing reflux oesophagitis and up to 100% for Barrett’s oesophagus compared to conventional endoscopy[42]. Although well tolerated the procedure is limited by poor gastric visualisation and the inability to take biopsies.
Varices screening appears a more viable indication with a reported sensitivity of 83% in a recent meta-analysis compared to conventional endoscopy[43]. (Figure 1H) Detection of varices by CE allows informed decisions regarding surveillance and primary bleeding prophylaxis to be made and since oesophageal CE has a favourable patient tolerability profile[44], it may also improve compliance with screening and surveillance.
Colon capsule endoscopy utilises the concept of a double headed capsule and a wider angle of view (172°) to enable visualisation behind haustral folds. The problem of variable, and sometimes rapid transit noted with the first version of the colon capsule has been addressed in an updated model, PillCam Colon 2 (PCC2, Given Imaging Ltd) which adjusts the frame acquisition rate according to the speed of transit (to between 4 and 35 frames per second). Bowel preparation is critical and currently most regimens include an oral pro-kinetic agent and two additional “booster” doses of phosphosoda on top of a conventional polyethylene glycol-electrolyte solution regimen. Compared to the first colon capsule model, recent multicentre trials suggest a much improved sensitivity of PPC2 in detecting polyps of over 6mm of between 84%-89%[45]. (Figure 1I and J) Bowel cleanliness scores were “good” or “excellent” in 78%-81% of cases. The position of PPC2 compared to other colonic imaging modalities remains to be established, but these early data compare favourably to those for virtual colonoscopy and even to conventional colonoscopy when performed in “tandem” or “back to back” colonoscopy trials[46]. Colon capsule may present a feasible alternative to colonoscopy based colorectal screening programmes where the invasive nature of colonoscopy limits patient uptake. Indeed Hassan et al[47] calculated that if a colon capsule based screening programme were associated with a 30% better compliance rate, it would be as equally cost-effective as faecal occult blood screening. The study was performed using the data from trials of the original colon capsule model, which had a much reduced sensitivity of 64% in detecting polyps of over 6 mm.
Relentless technical progression has allowed considerable improvements to capsule endoscopes. Superior quality multi-element lenses and adaptive illumination allow a wider angle of view and enhanced picture clarity. Power management strategies have increased the duration and performance of capsule endoscopes and are imperative to facilitate other capsule technological advancements. The CapsoCam SV1 (Capso Vision Inc, Saratoga, United States) has four side-viewing (as opposed to end-viewing) lenses allowing a 360° panoramic view to improve mucosal visualisation. In the first study of this new capsule, 100% of small bowel examinations were complete. The duodenal papilla, identified in only 18%-43% of conventional CE due to its’ angular position, was visualised in 70% of examinations using CapsoCam SV1[48-50].
Software and data analysis: Accurate reporting of a CE examination is time consuming and requires focussed attention since abnormalities may be evident in only a small number of frames[51]. This has prompted attempts to produce software tools to enable a shorter capsule reading time while maintaining diagnostic accuracy. The Suspected Blood Indicator automatically highlights frames containing multiple red pixels as a marker of bleeding or vascular abnormalities. However, with a reported sensitivity of < 60% in the presence of active bleeding it cannot be recommended as anything more than a supportive tool[52,53]. Quick View allows time efficient capsule reading by selecting 2%-80% of frames (as set by the reader), producing a condensed video for review. Results are promising with excellent lesion detection rates and significantly shorter reading times[54,55]. Fujinon intelligent chromoendoscopy enhances surface contrast in three specific wavelengths (red, green and blue) and appears to improve the definition and surface texture of small bowel lesions already detected with white light. Whether this actually influences detection rates or clinical outcomes still remains uncertain[56,57].
3-Dimensional reconstruction of the GI tract seems to assist diagnosis at conventional endoscopy by enhancing mucosal textural features and abnormalities[58-60]. A version for small bowel CE using a software-enabled technique to convert a 2-D CE image to a 3-D representation has been trialled. It improved visualisation of a significant proportion of vascular lesions but, surprisingly, was less beneficial for inflammatory and protruding lesions[61]. Encouraging early results have also been reported from automated tumour recognition software algorithms[62,63]. Such innovations are not isolated to small bowel CE. Ankri et al[64] recently reported a new optical detection method specifically designed for colorectal cancer. The technique uses immune-conjugated gold nanorods to differentiate between normal and cancerous tissue and could be integrated into standard colon capsule endoscopy systems. Further research is required to define the utility of these advances in clinical practice.
Manoeuverability: The development of steerable capsules represents a major leap in the evolution of capsule technology. If the capsule motion through the gut was an active process, areas of interest could be inspected carefully, while interaction with the capsule could allow targeted biopsy or even drug delivery. Furthermore, a steerable capsule could overcome the problems encountered examining the capacious stomach allowing accurate pan-enteric examination to become a reality.
Remote manipulation: Swain et al[65] first reported this novel technology in 2010, using a modified Pillcam Colon with one camera replaced by magnets. The magnetically manoeuvrable capsule appeared to be easily manipulated in the oesophagus and stomach using a handheld external magnet. A second study found encouraging results with > 75% of gastric mucosa visualised in 7 out of 10 patients undergoing the examination and no adverse events reported[66].
Further studies using a magnetically steerable capsule with a magnetic guidance system similar to standard magnetic resonance imagers have been reported. In this case the capsule is manipulated using a joystick rather than a hand held paddle. Promising results were also achieved with all major areas of the stomach identified in > 85% of examinations. Comparison with conventional upper GI endoscopy was also encouraging with 58.3% of gastric lesions detected by both modalities, while 14 lesions were missed by MSCE and 31 lesions missed by OGD (that were seen on MSCE)[67]. The relative high cost of installing such a system is a major drawback to this technique.
Self-propelling capsules: Self-locomotion strategies using paddling, legs, fish-like movement and external magnets have been tried on in vivo models of the stomach and colon with some element of success. However, extensive work is required for these to become clinical reality. Most utilise internal actuation mechanisms to mobilise attached legs or paddles. An externally connected cable allows a continuous power supply, steering mechanisms and retrieval of data images[68,69].
Obtaining a tissue sample is the next logical step once the capsule can be accurately manoeuvred around a lesion and thus would prevent the need for a flexible endoscopy and biopsy when an abnormality is noted at CE reporting. The Nano-based capsule-Endoscopy with Molecular imaging and Optical biopsy (NEMO) project is a collaboration between academic and industry pioneers to produce a capsule with recognition, anchoring and bio-sensing capabilities to enable accurate pathology detection and diagnosis. Similarly the Versatile Endoscopic Capsule for gastrointestinal TumOr Recognition and therapy (VECTOR) project, funded by the European Commission, is developing a mini-robot comprising sensors, controls, and a human-machine interface aiming to detect and intervene in early GI cancer. Other capsules using “micro-grippers” to fold and grab tissue samples are also being prototyped[70].
With the advent of real-time viewing and external manipulation the notion of targeted drug delivery becomes feasible. Potentially this could be applied to a number of clinical situations; localised application of steroid or immunomodulation for isolated CD for instance or targeted use of haemostatic spray to an actively bleeding lesion. One prototype can deliver an injection of 1 mL of targeted medication while using a holding mechanism to resist movement by peristalsis[71]. Whereas the iPill (Phillips Research, Eindhoven, The Netherlands) uses bowel transit time and pH sensors to gauge gut location before drug delivery and is being trialled in CD and colorectal cancer[72].
Capsule endoscopy is now an invaluable tool for investigating the small bowel since it outperforms other investigation modalities while remaining acceptable to patients. Oesophageal, colon and potentially gastric capsule examination have some way to go in order to challenge their traditional investigational counterparts. Ultimately underlying these issues, the fact remains that intubational endoscopy is uncomfortable for patients and incurs risk. Despite having good patient tolerability and safety profiles capsule examination outside of the small bowel will need to match these conventional tests in both diagnostic yields and cost-effectiveness in order to compete. Technology is swiftly advancing and therefore if these standards can be met CE would have a clear advantage over conventional endoscopy particularly in the context of screening.
P- Reviewers: El-Salhy M, Kopacova M, Maehata Y S- Editor: Ma YJ L- Editor: A E- Editor: Zhang DN
| 1. | McAlindon ME, Parker CE, Hendy P, Mosea H, Panter S, Dabvison C, Fraser C, Despott EJ, Sidhu R, Sanders DS. Provision of service and training for small bowel endoscopy in the UK. Frontline Gastroenterol. 2012;2:98-103. [RCA] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 17] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 2. | Ho KK, Joyce AM. Complications of capsule endoscopy. Gastrointest Endosc Clin N Am. 2007;17:169-178, viii-ix. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 49] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 3. | Liao Z, Gao R, Xu C, Li ZS. Indications and detection, completion, and retention rates of small-bowel capsule endoscopy: a systematic review. Gastrointest Endosc. 2010;71:280-286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 4. | Carey EJ, Heigh RI, Fleischer DE. Endoscopic capsule endoscope delivery for patients with dysphagia, anatomical abnormalities, or gastroparesis. Gastrointest Endosc. 2004;59:423-426. [PubMed] |
| 5. | Cheifetz AS, Lewis BS. Capsule endoscopy retention: is it a complication? J Clin Gastroenterol. 2006;40:688-691. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 75] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 6. | Li F, Gurudu SR, De Petris G, Sharma VK, Shiff AD, Heigh RI, Fleischer DE, Post J, Erickson P, Leighton JA. Retention of the capsule endoscope: a single-center experience of 1000 capsule endoscopy procedures. Gastrointest Endosc. 2008;68:174-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 168] [Cited by in RCA: 155] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 7. | Boysen M, Ritter M. Small bowel obstruction from capsule endoscopy. West J Emerg Med. 2010;11:71-73. [PubMed] |
| 8. | Cheon JH, Kim YS, Lee IS, Chang DK, Ryu JK, Lee KJ, Moon JS, Park CH, Kim JO, Shim KN. Can we predict spontaneous capsule passage after retention? A nationwide study to evaluate the incidence and clinical outcomes of capsule retention. Endoscopy. 2007;39:1046-1052. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 93] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 9. | Baichi MM, Arifuddin RM, Mantry PS. What we have learned from 5 cases of permanent capsule retention. Gastrointest Endosc. 2006;64:283-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 35] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 10. | Payeras G, Piqueras J, Moreno VJ, Cabrera A, Menéndez D, Jiménez R. Effects of capsule endoscopy on cardiac pacemakers. Endoscopy. 2005;37:1181-1185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 46] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 11. | Harris LA, Hansel SL, Rajan E, Srivathsan K, Rea R, Crowell MD, Fleischer DE, Pasha SF, Gurudu SR, Heigh RI. Capsule Endoscopy in Patients with Implantable Electromedical Devices is Safe. Gastroenterol Res Pract. 2013;2013:959234. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 33] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 12. | Bandorski D, Stunder D, Höltgen R, Jakobs R, Keuchel M. [Capsule Endoscopy in Patients with Cardiac Pacemakers and Implantable Cardioverter Defibrillators - Is the Formal Contraindication still Justified?]. Z Gastroenterol. 2013;51:747-752. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 13. | Triester SL, Leighton JA, Leontiadis GI, Fleischer DE, Hara AK, Heigh RI, Shiff AD, Sharma VK. A meta-analysis of the yield of capsule endoscopy compared to other diagnostic modalities in patients with obscure gastrointestinal bleeding. Am J Gastroenterol. 2005;100:2407-2418. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 433] [Cited by in RCA: 419] [Article Influence: 21.0] [Reference Citation Analysis (0)] |
| 14. | Ladas SD, Triantafyllou K, Spada C, Riccioni ME, Rey JF, Niv Y, Delvaux M, de Franchis R, Costamagna G. European Society of Gastrointestinal Endoscopy (ESGE): recommendations (2009) on clinical use of video capsule endoscopy to investigate small-bowel, esophageal and colonic diseases. Endoscopy. 2010;42:220-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 173] [Cited by in RCA: 172] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 15. | Hadithi M, Heine GD, Jacobs MA, van Bodegraven AA, Mulder CJ. A prospective study comparing video capsule endoscopy with double-balloon enteroscopy in patients with obscure gastrointestinal bleeding. Am J Gastroenterol. 2006;101:52-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 182] [Cited by in RCA: 184] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 16. | Nakamura M, Niwa Y, Ohmiya N, Miyahara R, Ohashi A, Itoh A, Hirooka Y, Goto H. Preliminary comparison of capsule endoscopy and double-balloon enteroscopy in patients with suspected small-bowel bleeding. Endoscopy. 2006;38:59-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 171] [Cited by in RCA: 166] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 17. | Teshima CW, Kuipers EJ, van Zanten SV, Mensink PB. Double balloon enteroscopy and capsule endoscopy for obscure gastrointestinal bleeding: an updated meta-analysis. J Gastroenterol Hepatol. 2011;26:796-801. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 173] [Cited by in RCA: 208] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 18. | Liu K, Kaffes AJ. Review article: the diagnosis and investigation of obscure gastrointestinal bleeding. Aliment Pharmacol Ther. 2011;34:416-423. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 51] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 19. | Yamada A, Watabe H, Kobayashi Y, Yamaji Y, Yoshida H, Koike K. Timing of capsule endoscopy influences the diagnosis and outcome in obscure-overt gastrointestinal bleeding. Hepatogastroenterology. 2012;59:676-679. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 23] [Reference Citation Analysis (0)] |
| 20. | Carey EJ, Leighton JA, Heigh RI, Shiff AD, Sharma VK, Post JK, Fleischer DE. A single-center experience of 260 consecutive patients undergoing capsule endoscopy for obscure gastrointestinal bleeding. Am J Gastroenterol. 2007;102:89-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 214] [Cited by in RCA: 212] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 21. | May A, Wardak A, Nachbar L, Remke S, Ell C. Influence of patient selection on the outcome of capsule endoscopy in patients with chronic gastrointestinal bleeding. J Clin Gastroenterol. 2005;39:684-688. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 31] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 22. | Sidhu R, Sanders DS, Sakellariou VP, McAlindon ME. Capsule endoscopy and obscure gastrointestinal bleeding: are transfusion dependence and comorbidity further risk factors to predict a diagnosis? Am J Gastroenterol. 2007;102:1329-1330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 23. | Triester SL, Leighton JA, Leontiadis GI, Gurudu SR, Fleischer DE, Hara AK, Heigh RI, Shiff AD, Sharma VK. A meta-analysis of the yield of capsule endoscopy compared to other diagnostic modalities in patients with non-stricturing small bowel Crohn’s disease. Am J Gastroenterol. 2006;101:954-964. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 392] [Cited by in RCA: 368] [Article Influence: 19.4] [Reference Citation Analysis (1)] |
| 24. | Dionisio PM, Gurudu SR, Leighton JA, Leontiadis GI, Fleischer DE, Hara AK, Heigh RI, Shiff AD, Sharma VK. Capsule endoscopy has a significantly higher diagnostic yield in patients with suspected and established small-bowel Crohn’s disease: a meta-analysis. Am J Gastroenterol. 2010;105:1240-1248; quiz 1249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 262] [Cited by in RCA: 278] [Article Influence: 18.5] [Reference Citation Analysis (36)] |
| 25. | Chong AK, Taylor A, Miller A, Hennessy O, Connell W, Desmond P. Capsule endoscopy vs. push enteroscopy and enteroclysis in suspected small-bowel Crohn’s disease. Gastrointest Endosc. 2005;61:255-261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 121] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 26. | Crook DW, Knuesel PR, Froehlich JM, Eigenmann F, Unterweger M, Beer HJ, Kubik-Huch RA. Comparison of magnetic resonance enterography and video capsule endoscopy in evaluating small bowel disease. Eur J Gastroenterol Hepatol. 2009;21:54-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 36] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 27. | Tillack C, Seiderer J, Brand S, Göke B, Reiser MF, Schaefer C, Diepolder H, Ochsenkühn T, Herrmann KA. Correlation of magnetic resonance enteroclysis (MRE) and wireless capsule endoscopy (CE) in the diagnosis of small bowel lesions in Crohn’s disease. Inflamm Bowel Dis. 2008;14:1219-1228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 91] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 28. | Rondonotti E, Herrerias JM, Pennazio M, Caunedo A, Mascarenhas-Saraiva M, de Franchis R. Complications, limitations, and failures of capsule endoscopy: a review of 733 cases. Gastrointest Endosc. 2005;62:712-76; quiz 752, 754. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 195] [Cited by in RCA: 196] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 29. | Caunedo-Alvarez A, Romero-Vazquez J, Herrerias-Gutierrez JM. Patency and Agile capsules. World J Gastroenterol. 2008;14:5269-5273. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 65] [Cited by in RCA: 60] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 30. | Sidhu R, Brunt LK, Morley SR, Sanders DS, McAlindon ME. Undisclosed use of nonsteroidal anti-inflammatory drugs may underlie small-bowel injury observed by capsule endoscopy. Clin Gastroenterol Hepatol. 2010;8:992-995. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 32] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 31. | Endo H, Hosono K, Inamori M, Nozaki Y, Yoneda K, Fujita K, Takahashi H, Yoneda M, Abe Y, Kirikoshi H. Characteristics of small bowel injury in symptomatic chronic low-dose aspirin users: the experience of two medical centers in capsule endoscopy. J Gastroenterol. 2009;44:544-549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 60] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 32. | Lang J, Price AB, Levi AJ, Burke M, Gumpel JM, Bjarnason I. Diaphragm disease: pathology of disease of the small intestine induced by non-steroidal anti-inflammatory drugs. J Clin Pathol. 1988;41:516-526. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 230] [Cited by in RCA: 217] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 33. | Hayashi Y, Yamamoto H, Taguchi H, Sunada K, Miyata T, Yano T, Arashiro M, Sugano K. Nonsteroidal anti-inflammatory drug-induced small-bowel lesions identified by double-balloon endoscopy: endoscopic features of the lesions and endoscopic treatments for diaphragm disease. J Gastroenterol. 2009;44 Suppl 19:57-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 42] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 34. | Rokkas T, Niv Y. The role of video capsule endoscopy in the diagnosis of celiac disease: a meta-analysis. Eur J Gastroenterol Hepatol. 2012;24:303-308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 82] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 35. | Kurien M, Evans KE, Aziz I, Sidhu R, Drew K, Rogers TL, McAlindon ME, Sanders DS. Capsule endoscopy in adult celiac disease: a potential role in equivocal cases of celiac disease? Gastrointest Endosc. 2013;77:227-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 43] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 36. | Atlas DS, Rubio-Tapia A, Van Dyke CT, Lahr BD, Murray JA. Capsule endoscopy in nonresponsive celiac disease. Gastrointest Endosc. 2011;74:1315-1322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 57] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 37. | Culliford A, Daly J, Diamond B, Rubin M, Green PH. The value of wireless capsule endoscopy in patients with complicated celiac disease. Gastrointest Endosc. 2005;62:55-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 132] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 38. | Chen WG, Shan GD, Zhang H, Li L, Yue M, Xiang Z, Cheng Y, Wu CJ, Fang Y, Chen LH. Double-balloon enteroscopy in small bowel tumors: a Chinese single-center study. World J Gastroenterol. 2013;19:3665-3671. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 26] [Cited by in RCA: 44] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 39. | Talamonti MS, Goetz LH, Rao S, Joehl RJ. Primary cancers of the small bowel: analysis of prognostic factors and results of surgical management. Arch Surg. 2002;137:564-70; discussion 570-1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 148] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 40. | Baichi MM, Arifuddin RM, Mantry PS. Small-bowel masses found and missed on capsule endoscopy for obscure bleeding. Scand J Gastroenterol. 2007;42:1127-1132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 45] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 41. | Postgate A, Despott E, Burling D, Gupta A, Phillips R, O’Beirne J, Patch D, Fraser C. Significant small-bowel lesions detected by alternative diagnostic modalities after negative capsule endoscopy. Gastrointest Endosc. 2008;68:1209-1214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 111] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 42. | Gralnek IM, Adler SN, Yassin K, Koslowsky B, Metzger Y, Eliakim R. Detecting esophageal disease with second-generation capsule endoscopy: initial evaluation of the PillCam ESO 2. Endoscopy. 2008;40:275-279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 44] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 43. | Guturu P, Sagi SV, Ahn D, Jaganmohan S, Kuo YF, Sood GK. Capsule endoscopy with PILLCAM ESO for detecting esophageal varices: a meta-analysis. Minerva Gastroenterol Dietol. 2011;57:1-11. [PubMed] |
| 44. | Sánchez-Yagüe A, Caunedo-Alvarez A, García-Montes JM, Romero-Vázquez J, Pellicer-Bautista FJ, Herrerías-Gutiérrez JM. Esophageal capsule endoscopy in patients refusing conventional endoscopy for the study of suspected esophageal pathology. Eur J Gastroenterol Hepatol. 2006;18:977-983. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 45. | Spada C, De Vincentis F, Cesaro P, Hassan C, Riccioni ME, Minelli Grazioli L, Bolivar S, Zurita A, Costamagna G. Accuracy and safety of second-generation PillCam COLON capsule for colorectal polyp detection. Therap Adv Gastroenterol. 2012;5:173-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 34] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 46. | Heresbach D, Barrioz T, Lapalus MG, Coumaros D, Bauret P, Potier P, Sautereau D, Boustière C, Grimaud JC, Barthélémy C. Miss rate for colorectal neoplastic polyps: a prospective multicenter study of back-to-back video colonoscopies. Endoscopy. 2008;40:284-290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 351] [Cited by in RCA: 370] [Article Influence: 21.8] [Reference Citation Analysis (0)] |
| 47. | Hassan C, Zullo A, Winn S, Morini S. Cost-effectiveness of capsule endoscopy in screening for colorectal cancer. Endoscopy. 2008;40:414-421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 72] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 48. | Friedrich K, Gehrke S, Stremmel W, Sieg A. First clinical trial of a newly developed capsule endoscope with panoramic side view for small bowel: a pilot study. J Gastroenterol Hepatol. 2013;28:1496-1501. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 40] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 49. | Nakamura M, Ohmiya N, Shirai O, Takenaka H, Kenji R, Ando T, Watanabe O, Kawashima H, Itoh A, Hirooka Y. Advance of video capsule endoscopy and the detection of anatomic landmarks. Hepatogastroenterology. 2009;56:1600-1605. [PubMed] |
| 50. | Park S, Chun HJ, Keum B, Seo YS, Kim YS, Jeen YT, Lee HS, Um SH, Kim CD, Ryu HS. Capsule Endoscopy to Detect Normally Positioned Duodenal Papilla: Performance Comparison of SB and SB2. Gastroenterol Res Pract. 2012;2012:202935. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 51. | Lo SK. How should we do capsule reading? Tech Gastrointest Endosc. 2006;8:146-148. [RCA] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 52. | Liangpunsakul S, Mays L, Rex DK. Performance of Given suspected blood indicator. Am J Gastroenterol. 2003;98:2676-2678. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 47] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 53. | Buscaglia JM, Giday SA, Kantsevoy SV, Clarke JO, Magno P, Yong E, Mullin GE. Performance characteristics of the suspected blood indicator feature in capsule endoscopy according to indication for study. Clin Gastroenterol Hepatol. 2008;6:298-301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 41] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 54. | Saurin JC, Lapalus MG, Cholet F, D’Halluin PN, Filoche B, Gaudric M, Sacher-Huvelin S, Savalle C, Frederic M, Lamarre PA. Can we shorten the small-bowel capsule reading time with the “Quick-view” image detection system? Dig Liver Dis. 2012;44:477-481. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 46] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 55. | Koulaouzidis A, Smirnidis A, Douglas S, Plevris JN. QuickView in small-bowel capsule endoscopy is useful in certain clinical settings, but QuickView with Blue Mode is of no additional benefit. Eur J Gastroenterol Hepatol. 2012;24:1099-1104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 33] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 56. | Spada C, Hassan C, Costamagna G. Virtual chromoendoscopy: will it play a role in capsule endoscopy? Dig Liver Dis. 2011;43:927-928. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 57. | Gupta T, Ibrahim M, Deviere J, Van Gossum A. Evaluation of Fujinon intelligent chromo endoscopy-assisted capsule endoscopy in patients with obscure gastroenterology bleeding. World J Gastroenterol. 2011;17:4590-4595. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 22] [Cited by in RCA: 30] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 58. | Tsutsui A, Okamura S, Muguruma N, Tsujigami K, Ichikawa S, Ito S, Umino K. Three-dimensional reconstruction of endosonographic images of gastric lesions: preliminary experience. J Clin Ultrasound. 2005;33:112-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 59. | Bhandari S, Shim CS, Kim JH, Jung IS, Cho JY, Lee JS, Lee MS, Kim BS. Usefulness of three-dimensional, multidetector row CT (virtual gastroscopy and multiplanar reconstruction) in the evaluation of gastric cancer: a comparison with conventional endoscopy, EUS, and histopathology. Gastrointest Endosc. 2004;59:619-626. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 118] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 60. | Taylor SA, Halligan S, Slater A, Goh V, Burling DN, Roddie ME, Honeyfield L, McQuillan J, Amin H, Dehmeshki J. Polyp detection with CT colonography: primary 3D endoluminal analysis versus primary 2D transverse analysis with computer-assisted reader software. Radiology. 2006;239:759-767. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 37] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 61. | Koulaouzidis A, Karargyris A, Rondonotti E, Noble CL, Douglas S, Alexandridis E, Zahid AM, Bathgate AJ, Trimble KC, Plevris JN. Three-dimensional representation software as image enhancement tool in small-bowel capsule endoscopy: a feasibility study. Dig Liver Dis. 2013;45:909-914. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 23] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 62. | Barbosa DJ, Ramos J, Lima CS. Detection of small bowel tumors in capsule endoscopy frames using texture analysis based on the discrete wavelet transform. Conf Proc IEEE Eng Med Biol Soc. 2008;2008:3012-3015. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 63. | Li B, Meng MQ. Tumor recognition in wireless capsule endoscopy images using textural features and SVM-based feature selection. IEEE Trans Inf Technol Biomed. 2012;16:323-329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 82] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 64. | Ankri R, Peretz D, Motiei M, Sella-Tavor O, Popovtzer R. New optical method for enhanced detection of colon cancer by capsule endoscopy. Nanoscale. 2013;5:9806-9811. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 65. | Swain P, Toor A, Volke F, Keller J, Gerber J, Rabinovitz E, Rothstein RI. Remote magnetic manipulation of a wireless capsule endoscope in the esophagus and stomach of humans (with videos). Gastrointest Endosc. 2010;71:1290-1293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 113] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 66. | Keller J, Fibbe C, Volke F, Gerber J, Mosse AC, Reimann-Zawadzki M, Rabinovitz E, Layer P, Schmitt D, Andresen V. Inspection of the human stomach using remote-controlled capsule endoscopy: a feasibility study in healthy volunteers (with videos). Gastrointest Endosc. 2011;73:22-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 89] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 67. | Rey JF, Ogata H, Hosoe N, Ohtsuka K, Ogata N, Ikeda K, Aihara H, Pangtay I, Hibi T, Kudo SE. Blinded nonrandomized comparative study of gastric examination with a magnetically guided capsule endoscope and standard videoendoscope. Gastrointest Endosc. 2012;75:373-381. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 113] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 68. | Quirini M, Menciassi A, Scapellato S, Dario P, Rieber F, Ho CN, Schostek S, Schurr MO. Feasibility proof of a legged locomotion capsule for the GI tract. Gastrointest Endosc. 2008;67:1153-1158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 56] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 69. | Kim HM, Yang S, Kim J, Park S, Cho JH, Park JY, Kim TS, Yoon ES, Song SY, Bang S. Active locomotion of a paddling-based capsule endoscope in an in vitro and in vivo experiment (with videos). Gastrointest Endosc. 2010;72:381-387. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 66] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 70. | Yim S, Gultepe E, Gracias DH, Sitti M. Biopsy using a magnetic capsule endoscope carrying, releasing, and retrieving untethered microgrippers. IEEE Trans Biomed Eng. 2014;61:513-521. [PubMed] |
| 71. | Woods SP, Constandinou TG. Wireless capsule endoscope for targeted drug delivery: mechanics and design considerations. IEEE Trans Biomed Eng. 2013;60:945-953. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 75] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 72. | Phillips Technology. Phillips Intelligent Pill Technology. Available from: http://www.research.philips.com/newscenter/backgrounders/081111-ipill.html. |