Published online Jan 14, 2014. doi: 10.3748/wjg.v20.i2.607
Revised: November 21, 2013
Accepted: December 3, 2013
Published online: January 14, 2014
Processing time: 128 Days and 0.7 Hours
Endoscopic retrograde cholangiopancreatography (ERCP) is efficacious in patients who have undergone Billroth II gastroenterostomies, but the success rate decreases in patients who also have experienced Braun anastomoses. There are currently no reports describing the preferred enterography route for cannulation in these patients. We first review the patient’s previous surgery records, which most often indicate that the efferent loop is at the greater curvature of the stomach. We recommend extending the duodenoscope along the greater curvature of the stomach and then advancing it through the “lower entrance” at the site of the gastrojejunal anastomosis, along the efferent loop, and through the “middle entrance” at the site of the Braun anastomosis to reach the papilla of Vater. Ten patients who had each undergone Billroth II gastroenterostomy and Braun anastomosis between January 2009 and December 2011 were included in our study. The overall success rate of enterography was 90% for the patients who had undergone Billroth II gastroenterostomy and Braun anastomosis, and the therapeutic success rate was 80%. We believe that this enterography route for ERCP is optimal for a patient who has had Billroth II gastroenterostomy and Braun anastomosis and helps to increase the success rate of the procedure.
Core tip: We recommend extending the duodenoscope along the greater curvature of the stomach and then advancing it through the “lower entrance” at the site of the gastrojejunal anastomosis, along the efferent loop, and through the “middle entrance” at the site of the Braun anastomosis to reach the papilla of Vater. We believe that this enterography route for endoscopic retrograde cholangiopancreatography is optimal for a patient who has undergone Billroth II gastroenterostomy and Braun anastomosis and helps to increase the success rate of the procedure.
- Citation: Wu WG, Gu J, Zhang WJ, Zhao MN, Zhuang M, Tao YJ, Liu YB, Wang XF. ERCP for patients who have undergone Billroth II gastroenterostomy and Braun anastomosis. World J Gastroenterol 2014; 20(2): 607-610
- URL: https://www.wjgnet.com/1007-9327/full/v20/i2/607.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i2.607
Endoscopic retrograde cholangiopancreatography (ERCP) is efficacious in patients having undergone Billroth II gastroenterostomies, but the success rate decreases in patients who also have had Braun anastomoses. A previous study reported success rates of 83% in patients with simple Billroth II gastroenterostomies but only 29% in patients with both a Billroth II gastroenterostomy and an additional Braun anastomosis[1]. ERCP failures in such patients are caused by difficulties entering the afferent loop and accessing the papilla[2-4]. There are currently no reports describing the preferred enterography route for cannulation in these patients. Herein, we describe our method for identifying the optimal enterography route for ERCP in patients with both a Billroth II gastroenterostomy and a Braun anastomosis.
In this study, we included patients who had had Billroth II gastroenterostomies and Braun anastomoses and in whom therapeutic biliary intervention was planned between January 2009 and December 2011 in the ERCP unit in the Department of General Surgery, Xin Hua Hospital, which is affiliated with the Shanghai Jiaotong University School of Medicine. During this period, 1659 ERCP procedures were performed. Patients who had normal anatomies, Billroth I/II gastroenterostomies, Roux-en-Y gastroenterostomies, and choledochoduodenostomies were excluded from the study. A total of 10 patients who had undergone Billroth II gastroenterostomies and Braun anastomoses were included in the study. These 10 patients [2 women and 8 men; mean age: 70.8 years (range: 55-83 years)] were admitted to our hospital as a result of upper right quadrant pain, fever and jaundice. Magnetic resonance cholangiopancreatography revealed intra- and extra-hepatic bile duct dilation (common bile duct stones were presented in all patients).
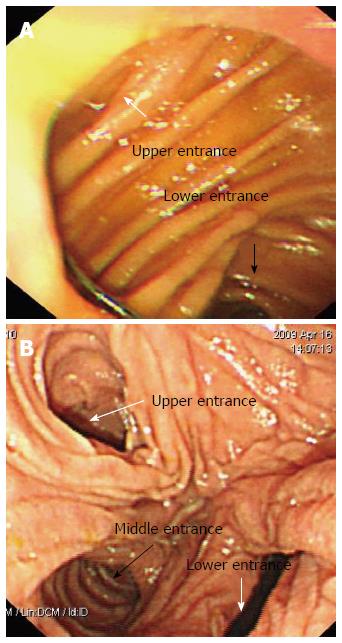
When conducting the procedure, we first review the patient’s previous surgery records, which most often indicate that the efferent loop is at the greater curvature of the stomach. One major challenge is distinguishing between the afferent and efferent loops. Our solution is to extend the duodenoscope along the greater curvature of the stomach until the gastrojejunal anastomosis becomes visible, from which perspective the “lower entrance” is the entrance to the right efferent loop (Figure 1A). We are occasionally able to draw back the duodenoscope to “relax” the gastrojejunal anastomosis and thus differentiate the “upper entrance” from the “lower entrance.” The efferent loop makes a better entrance for the duodenoscope because it is less angulated than the afferent loop. Three stomal openings can be visualized endoscopically, but identifying the correct entrance is a major challenge (Figure 1B). The “middle entrance” is the entrance to the loop that can be used to reach the papilla of Vater when the endoscope is advanced from the efferent loop and is unique irrespective of the endoscopic approach used.
Ten patients who had each undergone a Billroth II gastroenterostomy and a Braun anastomosis were included in our study. The overall success rate of enterography was 90% for the patients who had Billroth II gastroenterostomies and Braun anastomoses, and the therapeutic success rate was 80%. One patient’s procedure was unsuccessful because of a failure to access the papilla (due to a long afferent loop), and cannulation failure occurred another patient.
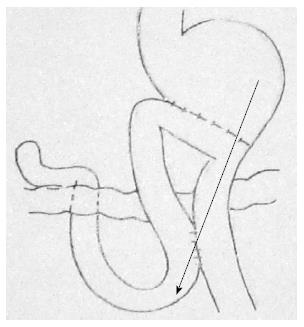
Many endoscopists enter the afferent loop via the site of the gastrojejunal anastomosis, but the sharp angulation caused by adhesions may make it impossible to advance the endoscope into the afferent loop. Premature entry into the afferent loop at the gastrojejunal anastomosis is the main cause of failure to access the papilla. We avoid this by extending the duodenoscope along the efferent loop until the Braun anastomosis is visible. We recommend extending the duodenoscope along the greater curvature of the stomach and then advancing it through the “lower entrance” at the site of the gastrojejunal anastomosis, along the efferent loop, and through the “middle entrance” at the site of the Braun anastomosis to reach the papilla of Vater. We believe that this enterography route for ERCP is optimal for patients with Billroth II gastroenterostomies and Braun anastomoses (Figure 2) and helps to increase the success rate of the procedure. Ten patients who received Billroth II gastroenterostomies and Braun anastomoses were included in our study. The overall success rate of enterography was 90% for the patients who had undergone Billroth II gastroenterostomies and Braun anastomoses, and the therapeutic success rate was 80%.
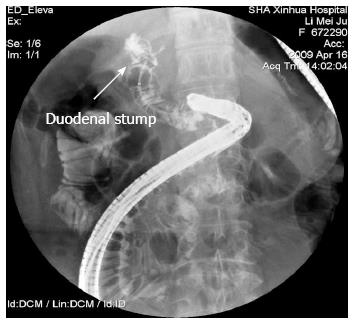
When the efferent loop is located at the lesser curvature of the stomach, we recommend extending the duodenoscope along the greater curvature of the stomach and then advancing it through the “upper entrance” at the site of the gastrojejunal anastomosis, along the efferent loop, and through the “middle entrance” at the site of the Braun anastomosis to reach the papilla of Vater. If the previous surgery records do not specify the location of the efferent loop, we extend the duodenoscope along the greater curvature of the stomach until the gastrojejunal anastomosis is visible and then advance it through the “lower entrance” and along the jejunal loop until it reaches the 3 stomal openings at the site of the Braun anastomosis. We use a catheter (usually the wire-guided retrieval balloon that is used to remove the common bile duct stone) to explore the middle limb and inject contrast into the loop to confirm that the limb is the duodenal stump (Figure 3) and have therefore termed this procedure “retrieval-balloon-assisted enterography”[5,6]. It should be emphasized that when performing ERCP in patients with postsurgical anatomical changes, endoscopic guidance is insufficient and should be supplemented with radiographs. If the middle limb into which the catheter was advanced is the distal jejunum rather than the duodenal stump, the duodenoscope should be retracted to the gastrojejunal anastomosis and then advanced through the “upper entrance,” along the limb, and then into the “middle entrance” at the site of the Braun anastomosis to reach the papilla of Vater.
Ten patients were admitted to their hospital as a result of upper right quadrant pain, fever and jaundice.
Upper right quadrant pain, fever and jaundice.
Magnetic resonance cholangiopancreatography.
Liver function tests were outside normal limits.
Magnetic resonance cholangiopancreatography revealed intra- and extra-hepatic bile duct dilation (common bile duct stones were presented in all patients).
Endoscopic retrograde cholangiopancreatography.
Endoscopic retrograde cholangiopancreatography (ERCP) is efficacious in patients having undergone Billroth II gastroenterostomies, but the success rate decreases in patients who also have had Braun anastomoses.
Braun anastomosis is an anastomosis between the afferent and efferent loops of the jejunum after a loop gastroenterostomy.
The authors recommend extending the duodenoscope along the greater curvature of the stomach and then advancing it through the “lower entrance” at the site of the gastrojejunal anastomosis, along the efferent loop, and through the “middle entrance” at the site of the Braun anastomosis to reach the papilla of Vater. The authors believe that this is the optimal enterography route for ERCP in patients having undergone Billroth II gastroenterostomies and a Braun anastomoses.
In this paper, Wu et al describe a method for identifying the optimal route for ERCP in patients with both a Billroth II gastroenterostomy and a Brown anastomosis. The methods used appear feasible and useful to increase success rate of ERCP in such setting. The figures are a good argument for their methods. The manuscript can be accepted for publication.
P- Reviewers: Mendelsohn RB, Trifan A S- Editor: Song XX L- Editor: A E- Editor: Liu XM
| 1. | Ciçek B, Parlak E, Dişibeyaz S, Koksal AS, Sahin B. Endoscopic retrograde cholangiopancreatography in patients with Billroth II gastroenterostomy. J Gastroenterol Hepatol. 2007;22:1210-1213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 47] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 2. | Hintze RE, Veltzke W, Adler A, Abou-Rebyeh H. Endoscopic sphincterotomy using an S-shaped sphincterotome in patients with a Billroth II or Roux-en-Y gastrojejunostomy. Endoscopy. 1997;29:74-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 48] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 3. | Kim MH, Lee SK, Lee MH, Myung SJ, Yoo BM, Seo DW, Min YI. Endoscopic retrograde cholangiopancreatography and needle-knife sphincterotomy in patients with Billroth II gastrectomy: a comparative study of the forward-viewing endoscope and the side-viewing duodenoscope. Endoscopy. 1997;29:82-85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 81] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 4. | Faylona JM, Qadir A, Chan AC, Lau JY, Chung SC. Small-bowel perforations related to endoscopic retrograde cholangiopancreatography (ERCP) in patients with Billroth II gastrectomy. Endoscopy. 1999;31:546-549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 94] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 5. | Zhuang M, Zhang W, Gu J, Gong W, Wang X. ERCP with retrieval balloon-assisted enterography using traditional duodenoscope in post-GI surgery patients. Gastrointest Endosc. 2013;77:315-316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Zhuang M, Zhang WJ, Gu J, Liu YB, Wang XF. Retrieval-balloon-assisted enterography in post-pancreaticoduodenectomy endoscopic retrograde cholangiopancreatography. World J Gastroenterol. 2012;18:7109-7112. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |