Published online Jan 14, 2014. doi: 10.3748/wjg.v20.i2.578
Revised: October 18, 2013
Accepted: October 19, 2013
Published online: January 14, 2014
Processing time: 216 Days and 1.3 Hours
AIM: To systematically review the evidence for the effectiveness of fast-track program vs traditional care in laparoscopic or open surgery for gastric cancer.
METHODS: PubMed, Embase and the Cochrane library databases were electronically searched for published studies between January 1995 and April 2013, and only randomized trials were included. The references of relevant studies were manually searched for further studies that may have been missed. Search terms included “gastric cancer”, “fast track” and “enhanced recovery”. Five outcome variables were considered most suitable for analysis: postoperative hospital stay, medical cost, duration to first flatus, C-reactive protein (CRP) level and complications. Postoperative hospital stay was calculated from the date of operation to the date of discharge. Fixed effects model was used for meta-analysis.
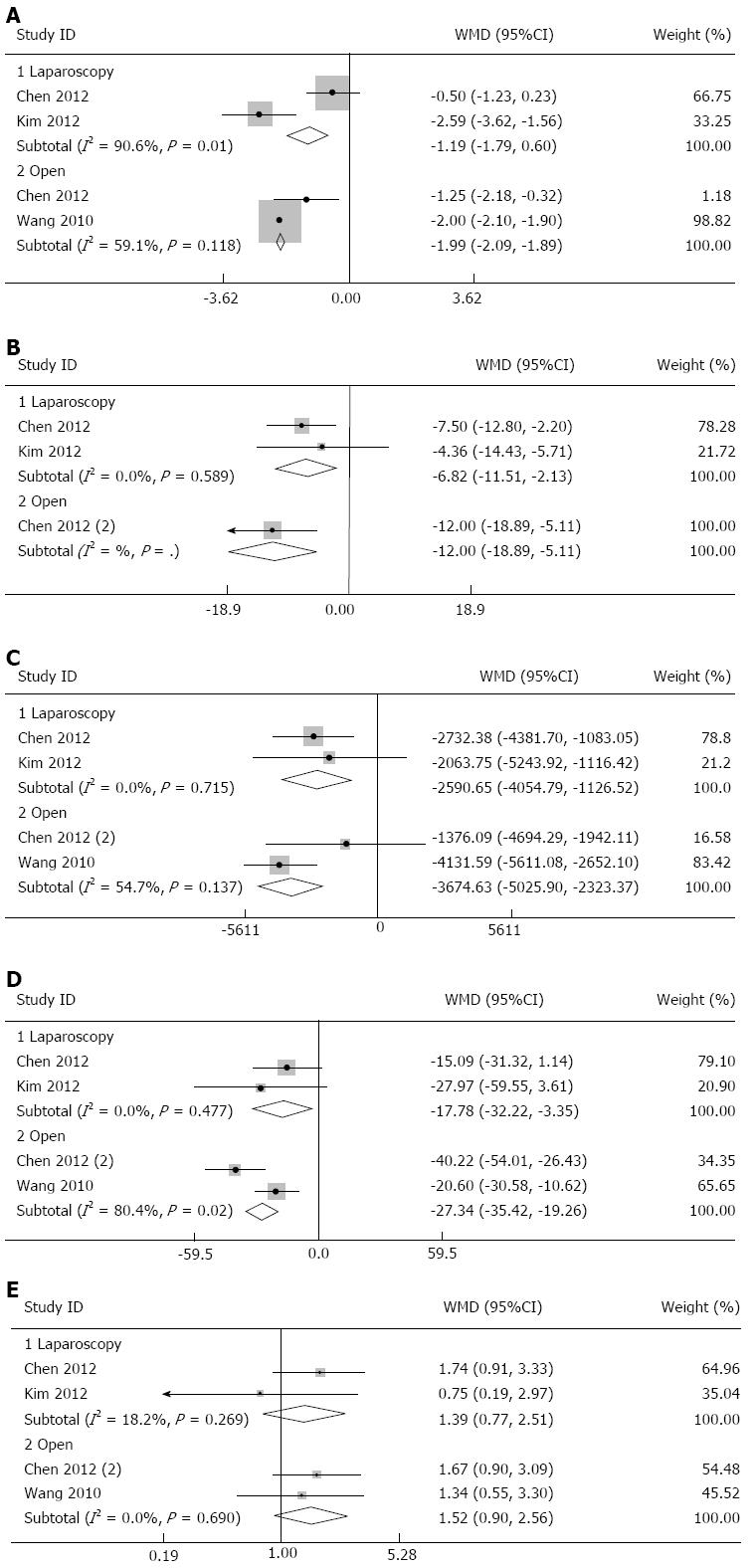
RESULTS: Compared with traditional care, fast-track program could significantly decrease the postoperative hospital stay [weighted mean difference (WMD) = -1.19, 95%CI: -1.79--0.60, P = 0.0001, fixed model], duration to first flatus (WMD = -6.82, 95%CI: -11.51--2.13, P = 0.004), medical costs (WMD = -2590, 95%CI: -4054--1126, P = 0.001), and the level of CRP (WMD = -17.78, 95%CI: -32.22--3.35, P = 0.0001) in laparoscopic surgery for gastric cancer. In open surgery for gastric cancer, fast-track program could also significantly decrease the postoperative hospital stay (WMD = -1.99, 95%CI: -2.09--1.89, P = 0.0001), duration to first flatus (WMD = -12.0, 95%CI: -18.89--5.11, P = 0.001), medical cost (WMD = -3674, 95%CI: -5025--2323, P = 0.0001), and the level of CRP (WMD = -27.34, 95%CI: -35.42--19.26, P = 0.0001). Furthermore, fast-track program did not significantly increase the incidence of complication (RR = 1.39, 95%CI: 0.77-2.51, P = 0.27, for laparoscopic surgery; and RR = 1.52, 95%CI: 0.90-2.56, P = 0.12, for open surgery).
CONCLUSION: Our overall results suggested that compared with traditional care, fast-track program could result in shorter postoperative hospital stay, less medical costs, and lower level of CRP, with no more complications occurring in both laparoscopic and open surgery for gastric cancer.
Core tip: Our overall results suggested that compared with traditional care, fast-track program could result in shorter postoperative hospital stay, less medical cost, and lower level of C-reactive protein, with no more complications occurring in both laparoscopic and open surgery for gastric cancer.
-
Citation: Chen ZX, Liu AHJ, Cen Y. Fast-track program
vs traditional care in surgery for gastric cancer. World J Gastroenterol 2014; 20(2): 578-583 - URL: https://www.wjgnet.com/1007-9327/full/v20/i2/578.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i2.578
China, Japan, South America, Eastern Europe and parts of the Middle East are reported with the highest incidence of gastric cancer[1]. Over the past 20 years, there have been two important developments in elective major abdominal surgery; the introduction of laparoscopic surgery and the implementation of an enhanced recovery after surgery program, also referred to as “fast track” (FT) perioperative care, both focusing on accelerated recovery resulting in shorter hospital stay.
Laparoscopic surgery has definite advantages and has been used widely since its advent. And it is well known to be associated with less postoperative pain than open surgery and postoperative pain can be controlled without opioids[2]. In recent years, the advantages of laparoscopic surgery have been recognized in gastric cancer[3-6].
FT surgery is an integrated application of various medical interventions that can enhance recovery after surgery. The FT perioperative care, or the enhanced recovery program after surgery, initiated by Bardram et al[7] in 1995, consists of a multidisciplinary approach, including preoperative counseling, no bowel preparation, perioperative high oxygen concentrations, active prevention of hypothermia, and no routine use of nasogastric tubes or drains. In recent years, FT surgery has been successfully applied to general[8], urological[9], cardiovascular[10], gynecological[11], orthopedic[12] and thoracic surgery[13].
This study aims to systematically review the evidence for the effectiveness of FT program vs traditional care in surgery for gastric cancer.
PubMed, Embase and the Cochrane library databases were electronically searched for published studies between January 1995 and April 2013. The references of relevant studies were manually searched for further studies that may have been missed. Search terms included “gastric cancer,”“FT” and “enhanced recovery”. No language restriction was applied.
Randomized controlled trials (RCTs) comparing FT program with traditional care in adult patients (aged > 18 years) undergoing laparoscopic or open surgery for gastric cancer were eligible for inclusion. Excluded studies (1) were not RCTs (such as nonrandomized, quasi-randomized, pseudorandomized, or controlled clinical trials or cohort or retrospective studies); (2) had no documentation of individual items of the FT programs; or (3) had no data available for the present meta-analysis.
Each article was critically reviewed by two researchers independently using the double-extraction method for eligibility. Any conflict was resolved before final analysis. Five outcome variables were considered most suitable for analysis: postoperative hospital stay, medical costs, duration to first flatus, C-reactive protein (CRP) level, and complications. Postoperative hospital stay was calculated from the date of operation to the date of discharge. The quality of the RCTs was assessed with the Jadad scoring system by two authors[14].
Weighted mean differences (WMDs) and their 95%CIs were used for analyzing continuous variables presented in the same scale (postoperative hospital stay, medical costs, duration to first flatus, and CRP level). Data reported as medians and ranges or medians and interquartile ranges were converted to means and standard deviation (SD)[15]. We calculated the lower and upper ends of the range by multiplying the difference between the median and upper and lower ends of the interquartile range by 2 and adding or subtracting the product from the median[16]. For dichotomous data (complications), relative risk (RR) with 95%CI was calculated. The effect measures were pooled using the fixed-effects model. Level of statistical significance was set at P < 0.05. Heterogeneity was quantified by calculating I2 where P < 0.10 was deemed significant. Publication bias was not evaluated by a funnel plot, because the number of included trials in the present review was limited. All statistical analyses were executed using STATA version 11. Some outcomes were not analyzed but presented in a descriptive way.
According to the searching strategy, three trials were included in our study. We divided the Chen’s study into two comparisons, i.e., FT program vs conventional care in laparoscopic surgery (Chen 2012), and FT program vs conventional care in open surgery [Chen 2012 (2)]. Two trials evaluated the effectiveness of FT program vs traditional care in laparoscopic surgery for gastric cancer[17,18], while two trials assessed the effectiveness of FT program vs traditional care in open surgery for gastric cancer[17,19]. The sample size was small in all trials, ranging from 41 to 92. All studies were conducted in Asia, including China and Korea. Detailed characteristics of each trial are given in Table 1.
| Ref. | Location | Sample size | Age (yr) | BMI (kg/m2) | Intervention group | Control group | Follow-up (wk) | Jadad score |
| Chen et al[17] | China | 19/22 | 59/63 | 22.9/22.9 | FT + LADG | LADG | 4 | 2 |
| Kim et al[18] | South Korea | 22/22 | 53/57 | 23.4/23.8 | FT + LADG | LADG | 2 | 2 |
| Chen et al[17] | China | 21/20 | 64/64 | 23.5/23.5 | FT + ODG | ODG | 4 | 2 |
| Wang et al[19] | China | 45/47 | 59/57 | 23.8/23.2 | FT + OG | OG | 4 | 2 |
No trials described the detailed methods of randomization, and allocation concealment was not performed in all trials. The incidence of withdrawal and dropouts was low, and the reasons were clearly reported. Blinding design was not applied in any trial. The methodological assessment by Jadad scale suggested that all trials were considered to be of moderate risk of bias.
In 2012, Chen et al[17] reported one RCT that evaluated the safety and effectiveness of FT program combined with laparoscopy-assisted radical distal gastrectomy for gastric cancer. They found that combination of FT with laparoscopy in gastric cancer is safe, feasible, and efficient and can improve nutritional status, lessen postoperative stress, and accelerate postoperative rehabilitation. Meanwhile, Kim and colleagues published another trial which also evaluated the safety and efficacy of FT in laparoscopic distal gastrectomy. They also found that FT surgery could enhance postoperative recovery and improve immediate postoperative quality of life, and was safe in laparoscopic distal gastrectomy. We made a meta-analysis for the following outcomes in these two trials.
Our overall results showed that compared with traditional care, FT program could significantly decrease the postoperative hospital stay (WMD = -1.19, 95%CI: -1.79--0.60, P = 0.0001, Figure 1A), duration to first flatus (WMD = -6.82, 95%CI: -11.51--2.13, P = 0.004, Figure 1B), medical cost (WMD = -2590, 95% CI: -4054--1126, P = 0.001, Figure 1C), and the level of CRP (WMD = -17.78, 95%CI: -32.22--3.35, P = 0.0001, Figure 1D) in laparoscopic surgery for gastric cancer. Furthermore, FT did not significantly increase the incidence of complications (RR = 1.39, 95%CI: 0.77-2.51, P = 0.27, Figure 1E). Additionally, there was no significant difference between the two groups for length of operative time and intraoperative blood loss. Most of the heterogeneity tests for those outcomes did not detect significant heterogeneity, which is detailed in Table 2.
| Gastric cancer | WMD/RR (95%CI) | Pvalue | Heterogeneity | |
| χ2(Pvalue) | I2(%) | |||
| Outcomes for laparoscopy surgery | ||||
| Postoperative hospital stay | WMD -1.19 (-1.79--0.60) | 0.000 | 10.60 (0.001) | 90.6 |
| Medical cost | WMD -2590 (-4054--1126) | 0.001 | 0.13 (0.72) | 0.0 |
| CRP | WMD -17.78 (-32.22--3.35) | 0.016 | 0.51 (0.48) | 0.0 |
| Duration to first flatus | WMD -6.82 (-11.51--2.13) | 0.004 | 0.29 (0.59) | 0.0 |
| Complication | RR 1.39 (0.77-2.51) | 0.270 | 1.22 (0.27) | 18.2 |
| Outcomes for open surgery | ||||
| Postoperative hospital stay | WMD -1.99 (-2.09--1.89) | 0.000 | 2.44 (0.12) | 59.1 |
| Medical cost | WMD -3674 (-5025--2323) | 0.000 | 2.21 (0.14) | 54.7 |
| CRP | WMD -27.34 (-35.42--19.26) | 0.000 | 5.10 (0.02) | 80.4 |
| Duration to first flatus | WMD -12.0 (-18.89--5.11) | 0.001 | - | - |
| Complication | RR 1.52 (0.90-2.56) | 0.120 | 0.16 (0.69) | 0.0 |
In 2010, Wang et al[19] reported a trial which evaluated the feasibility and safety of FT program in patients with gastric cancer during the perioperative period. They suggested that FT open surgery could lessen postoperative stress reactions and accelerate rehabilitation in patients with gastric cancer. In 2012, Chen and colleagues also found that compared with conventional care in open distal gastrectomy, FT program could reduce postoperative stress and accelerate postoperative rehabilitation.
Our overall results found that compared with traditional care, FT program could significantly decrease the postoperative hospital stay (WMD = -1.99, 95%CI: -2.09--1.89, P = 0.0001, Figure 1A), duration to first flatus (WMD = -12.0, 95%CI: -18.89--5.11, P = 0.001, Figure 1B), medical cost (WMD = -3674, 95%CI: -5025--2323, P = 0.0001, Figure 1C), and the level of CRP (WMD = -27.34, 95%CI: -35.42--19.26, P = 0.0001, Figure 1D) in open surgery for gastric cancer. Furthermore, FT program did not increase the incidence of complications (RR = 1.52, 95%CI: 0.90-2.56, P = 0.12, Figure 1E). Additionally, there was no significant difference between the two groups for operative time and intraoperative blood loss. Most of the heterogeneity tests for those outcomes did not detect significant heterogeneity, which is detailed in Table 2.
There have been a lot of studies and systematic reviews which evaluated the safety, feasibility, efficacy of FT program in colorectal surgery, and they found that compared with traditional care, FT program is safe and effective, justifying perioperative care in colorectal surgery[8,20-26]. However, until recently, only several trials evaluated the feasibility of FT program in surgery for gastric cancer.
Our present work is to systematically review the evidence for the effectiveness of FT program vs traditional care in laparoscopic or open surgery for gastric cancer. Our results showed that compared with traditional care, FT program resulted in more rapid postoperative recovery, less medical cost, and earlier discharge from hospital, with no more complications occurring.
There was significant heterogeneity for the outcome of postoperative hospital stay between the two laparoscopy trials. FT program did not decrease the postoperative hospital stay in Chen’s study. In contrast, Kim’s study suggested that FT could significantly decrease the postoperative hospital stay. Causes of the heterogeneity may result from the differences in population, surgeon, sampling, FT program or traditional care. However, we could not be sure which factor was the main source of heterogeneity. The FT program in these two laparoscopy trials was similar in most items, such as normal diet in the preoperative stage, and no opioid analgesics by intramuscular injection or patient-controlled analgesia in the postoperative period. There was some difference in the surgery day. In Chen’s study, there was no routine use of abdominal cavity drainage in the FT program, while in the Kim’s study, routine use of abdominal cavity drainage were applied. Additionally, the necessary data of mean ± SD in Chen’s study were imputed according to the method described by Hozo et al[15], and it could introduce some heterogeneity. No significant heterogeneity was found for the outcome of postoperative hospital stay between the two open trials.
The duration to first flatus in the FT program group was also found to be shorter, which implied that the bowel function recovered faster. The medical cost was significantly less in the FT program group, which may be explained by shorter postoperative hospital stay in this group. The incidence rate of complications was more frequent in Chen’s study than in Kim’s study, which can be explained by the fact that the duration of follow-up in Chen’s study was longer. However, there was no significant difference in the incidence rate of complications between the FT program and traditional care. Several cytokines such as interleukin-6, tumor necrosis factor-α, and CRP have been demonstrated to be involved in the response to surgical stress and therefore considered useful serum markers for evaluating the severity of surgery-induced stress. CRP was chosen as a serum marker in our study, and the overall results showed that the level of CRP was significantly lower in the FT program group than in the traditional group.
Our work is the first systematic review to discuss the FT surgery for gastric cancer. However, there were several main limitations in our study. First, the sample size was relatively small. Second, the number of included studies was limited. Third, the methodological assessment showed that all trials were of moderate risk of bias, because no trial described the details of randomization and allocation concealment. Finally, all trials were single-center studies.
In conclusion, our overall results suggested that compared with traditional care, FT program could result in shorter postoperative hospital stay, less medical cost, and lower level of CRP, with no more complications in both laparoscopic and open surgery for gastric cancer. Future trials need to include more participants in multiple centers to assess the effect of FT surgery for gastric cancer.
Fast-track (FT) surgery is an integrated application of various medical interventions that can enhance recovery after surgery. It has been applied in the surgery for gastric cancer.
Several trials evaluated the effectiveness of FT program vs traditional care in surgery for gastric cancer.
Authors’ overall results suggested that compared with traditional care, FT program could result in shorter postoperative hospital stay, less medical cost, and lower level of C-reactive protein, with no more complications occurring in both laparoscopic and open surgery for gastric cancer.
FT program can be applied in surgery for gastric cancer to enhance postoperative recovery.
The manuscript was well written and concise. The title and abstract explain the manuscript very well. Their results suggested that FT program can be used in surgery for gastric cancer.
P- Reviewer: Pradhan A S- Editor: Wen LL L- Editor: Wang TQ E- Editor: Wu HL
| 1. | Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA Cancer J Clin. 2005;55:74-108. [PubMed] |
| 2. | Kawamura H, Homma S, Yokota R, Watarai H, Yokota K, Kondo Y. Assessment of pain by face scales after gastrectomy: comparison of laparoscopically assisted gastrectomy and open gastrectomy. Surg Endosc. 2009;23:991-995. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 3. | Kitano S, Shiraishi N, Fujii K, Yasuda K, Inomata M, Adachi Y. A randomized controlled trial comparing open vs laparoscopy-assisted distal gastrectomy for the treatment of early gastric cancer: an interim report. Surgery. 2002;131:S306-S311. [PubMed] |
| 4. | Yakoub D, Athanasiou T, Tekkis P, Hanna GB. Laparoscopic assisted distal gastrectomy for early gastric cancer: is it an alternative to the open approach? Surg Oncol. 2009;18:322-333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 82] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 5. | Lee SE, Ryu KW, Nam BH, Lee JH, Kim YW, Yu JS, Cho SJ, Lee JY, Kim CG, Choi IJ. Technical feasibility and safety of laparoscopy-assisted total gastrectomy in gastric cancer: a comparative study with laparoscopy-assisted distal gastrectomy. J Surg Oncol. 2009;100:392-395. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 89] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 6. | Kawamura H, Okada K, Isizu H, Masuko H, Yamagami H, Honma S, Ueki S, Noguchi K, Kondo Y. Laparoscopic gastrectomy for early gastric cancer targeting as a less invasive procedure. Surg Endosc. 2008;22:81-85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 38] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 7. | Bardram L, Funch-Jensen P, Jensen P, Crawford ME, Kehlet H. Recovery after laparoscopic colonic surgery with epidural analgesia, and early oral nutrition and mobilisation. Lancet. 1995;345:763-764. [PubMed] |
| 8. | Zhuang CL, Ye XZ, Zhang XD, Chen BC, Yu Z. Enhanced recovery after surgery programs versus traditional care for colorectal surgery: a meta-analysis of randomized controlled trials. Dis Colon Rectum. 2013;56:667-678. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 340] [Cited by in RCA: 341] [Article Influence: 28.4] [Reference Citation Analysis (0)] |
| 9. | Pruthi RS, Nielsen M, Smith A, Nix J, Schultz H, Wallen EM. Fast track program in patients undergoing radical cystectomy: results in 362 consecutive patients. J Am Coll Surg. 2010;210:93-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 117] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 10. | Barletta JF, Miedema SL, Wiseman D, Heiser JC, McAllen KJ. Impact of dexmedetomidine on analgesic requirements in patients after cardiac surgery in a fast-track recovery room setting. Pharmacotherapy. 2009;29:1427-1432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 44] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 11. | Kroon UB, Rådström M, Hjelthe C, Dahlin C, Kroon L. Fast-track hysterectomy: a randomised, controlled study. Eur J Obstet Gynecol Reprod Biol. 2010;151:203-207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 41] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 12. | Andersen LØ, Gaarn-Larsen L, Kristensen BB, Husted H, Otte KS, Kehlet H. Subacute pain and function after fast-track hip and knee arthroplasty. Anaesthesia. 2009;64:508-513. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 139] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 13. | Das-Neves-Pereira JC, Bagan P, Coimbra-Israel AP, Grimaillof-Junior A, Cesar-Lopez G, Milanez-de-Campos JR, Riquet M, Biscegli-Jatene F. Fast-track rehabilitation for lung cancer lobectomy: a five-year experience. Eur J Cardiothorac Surg. 2009;36:383-391; discussion 391-392. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 96] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 14. | Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, McQuay HJ. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17:1-12. [PubMed] |
| 15. | Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5:13. [PubMed] |
| 16. | Liu T, Li G, Li L, Korantzopoulos P. Association between C-reactive protein and recurrence of atrial fibrillation after successful electrical cardioversion: a meta-analysis. J Am Coll Cardiol. 2007;49:1642-1648. [PubMed] |
| 17. | Chen Hu J, Xin Jiang L, Cai L, Tao Zheng H, Yuan Hu S, Bing Chen H, Chang Wu G, Fei Zhang Y, Chuan Lv Z. Preliminary experience of fast-track surgery combined with laparoscopy-assisted radical distal gastrectomy for gastric cancer. J Gastrointest Surg. 2012;16:1830-1839. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 81] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 18. | Kim JW, Kim WS, Cheong JH, Hyung WJ, Choi SH, Noh SH. Safety and efficacy of fast-track surgery in laparoscopic distal gastrectomy for gastric cancer: a randomized clinical trial. World J Surg. 2012;36:2879-2887. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 117] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 19. | Wang D, Kong Y, Zhong B, Zhou X, Zhou Y. Fast-track surgery improves postoperative recovery in patients with gastric cancer: a randomized comparison with conventional postoperative care. J Gastrointest Surg. 2010;14:620-627. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 138] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 20. | Li MZ, Xiao LB, Wu WH, Yang SB, Li SZ. Meta-analysis of laparoscopic vs open colorectal surgery within fast-track perioperative care. Dis Colon Rectum. 2012;55:821-827. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 35] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 21. | Abraham N, Albayati S. Enhanced recovery after surgery programs hasten recovery after colorectal resections. World J Gastrointest Surg. 2011;3:1-6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 28] [Cited by in RCA: 28] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 22. | Baird G, Maxson P, Wrobleski D, Luna BS. Fast-track colorectal surgery program reduces hospital length of stay. Clin Nurse Spec. 2010;24:202-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 23. | Scatizzi M, Kröning KC, Boddi V, De Prizio M, Feroci F. Fast-track surgery after laparoscopic colorectal surgery: is it feasible in a general surgery unit? Surgery. 2010;147:219-226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 27] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 24. | Wang Q, Suo J, Jiang J, Wang C, Zhao YQ, Cao X. Effectiveness of fast-track rehabilitation vs conventional care in laparoscopic colorectal resection for elderly patients: a randomized trial. Colorectal Dis. 2012;14:1009-1013. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 122] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 25. | van Bree SH, Vlug MS, Bemelman WA, Hollmann MW, Ubbink DT, Zwinderman AH, de Jonge WJ, Snoek SA, Bolhuis K, van der Zanden E. Faster recovery of gastrointestinal transit after laparoscopy and fast-track care in patients undergoing colonic surgery. Gastroenterology. 2011;141:872-880.e1-e4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 92] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 26. | Vlug MS, Wind J, Hollmann MW, Ubbink DT, Cense HA, Engel AF, Gerhards MF, van Wagensveld BA, van der Zaag ES, van Geloven AA. Laparoscopy in combination with fast track multimodal management is the best perioperative strategy in patients undergoing colonic surgery: a randomized clinical trial (LAFA-study). Ann Surg. 2011;254:868-875. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 571] [Cited by in RCA: 583] [Article Influence: 44.8] [Reference Citation Analysis (0)] |