Published online Jan 14, 2014. doi: 10.3748/wjg.v20.i2.555
Revised: November 10, 2013
Accepted: November 28, 2013
Published online: January 14, 2014
Processing time: 100 Days and 16.4 Hours
AIM: To evaluate total embolization of the main splenic artery in patients with splenic artery aneurysms (SAAs) and normal spleen.
METHODS: Thirty-five consecutive patients with SAAs were referred for treatment with coil embolization. Patients were classified into two groups: coil embolization of the main splenic artery with complete occlusion of the artery and aneurysms (group A, n = 16), and coil embolization of the aneurysmal sac with patency of the splenic artery (group B, n = 19). Data on white blood cell (WBC) and platelet counts, liver function, and complications were collected on days 7 and 30, and subsequently at a 6-mo interval postoperatively. Abdominal computed tomography was routinely performed to calculate the splenic volume before and 1 mo after the procedure, and subsequently every 6 mo during follow-up.
RESULTS: Coil embolization of the SAAs was technically successful in all 35 patients, with no procedure-related complications. The post-embolization syndrome, including abdominal pain, fever and vomiting, occurred in six patients (37.5%) in group A and three patients in group B (15.8%). There were no significant differences in WBC and platelet counts between preoperatively and at each follow-up point after the procedures. There were also no significant differences in average WBC and platelet counts between the two groups at each follow-up point. There were significant differences in splenic volume in group A between preoperatively and at each follow-up point, and there were also significant differences in splenic volume between the two groups at each follow-up point.
CONCLUSION: Total embolization of the main splenic artery was a safe and feasible procedure for patients with SAAs and normal spleen.
Core tip: Total embolization of the splenic artery sometime must be performed to achieve complete occlusion of large or multiple aneurysms. Thirty-five patients were classified into two groups: coil embolization of the splenic artery with complete occlusion of the artery and aneurysms, and coil embolization of the aneurysmal sac with patency of the splenic artery. Except for shrinkage of splenic volume, no changes in white blood cell and platelet counts or liver function were found in the former group. These results suggest that total embolization of the splenic artery is a safe and feasible procedure for patients with splenic artery aneurysm and normal spleen.
- Citation: Li ES, Mu JX, Ji SM, Li XM, Xu LB, Chai TC, Liu JX. Total splenic artery embolization for splenic artery aneurysms in patients with normal spleen. World J Gastroenterol 2014; 20(2): 555-560
- URL: https://www.wjgnet.com/1007-9327/full/v20/i2/555.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i2.555
Splenic artery aneurysms (SAAs) are the second most common abdominal aneurysm with a reported prevalence of 0.8% at arteriography and 0.04%-0.10% at autopsy. SAAs are usually small (< 2 cm in diameter), circular, and located at a bifurcation in a middle or distal segment of the splenic artery. Most SAAs are detected incidentally without symptoms during diagnostic imaging for other indications. Rupture of SAAs is rare, with the rate of potential rupture ranging from 3% to 9.6%[1], but is associated with a high mortality rate (10%-25%) if left untreated[2-4].
Coil embolization is now a widely accepted treatment for SAAs; however, for patients with large or multiple SAAs, total embolization of the splenic artery must be performed to produce complete occlusion of the SAAs. Nowadays, total embolization of the splenic artery has been shown to be a safe and effective method for the treatment of SAAs[1,5-8], but the changes in splenic function and morphology after embolization have rarely been reported, especially in patients with SAAs and normal spleen.
In this study, we retrospectively reviewed patients with SAAs treated by transcatheter embolization in our institution, evaluated the clinical outcomes of total embolization of the main splenic artery for patients with SAAs and normal spleen, and compared the results with coil embolization of the aneurysmal sac with patency of the splenic artery.
The protocol was approved by the institutional ethics committee, and all the patients provided written informed consent. From January 2007 to June 2013, 35 consecutive patients with SAAs referred for the treatment with coil embolization were screened for enrollment in this retrospective study, and subsequently underwent computed tomography (CT) follow-up at our hospital. Diagnosis of SAAs was established in all patients by CT with contrast medium injection and multiplanar reconstructions.
Patients were eligible for enrollment if they met the following criteria: (1) definite SAAs of the main splenic arteries with normal spleen; (2) transcatheter coil embolization; and (3) at least one CT and clinical follow-up ≥ 1 year after initial treatment. Patients were excluded if any of the followings were present: (1) severe cardiopulmonary comorbidity; (2) untreatable coagulopathy; (3) hypersplenism; (4) SAA at the branch of the splenic arteries or splenic parenchyma; or (5) contraindication for contrast medium.
A total of 48 patients with SAAs were enrolled in this study. SAAs were located in the proximal (n = 10), middle (n = 17), or distal (n = 21) segment of the main splenic artery. Thirty-eight patients had asymptomatic lesions that were discovered incidentally, and the remaining 10 patients presented with isolated abdominal pain. Forty-one of the 48 patients had a single aneurysm, and seven had multiple aneurysms. None of the patients experienced rupture of their lesions.
Patients were classified into two groups according to two embolization techniques: coil embolization of the main splenic artery with complete occlusion of the artery and aneurysms (group A), and coil embolization of the aneurysmal sac with patency of the splenic artery (group B). Initially, 21 and 27 patients were assigned to groups A and B, respectively. Of these, 13 patients did not meet the inclusion criteria, with CT and clinical follow-up < 1 year in eight patients and loss to follow-up in five patients (3 in group A and 2 in group B). The remaining 35 patients were enrolled. There were 21 men and 14 women with a mean age of 49.51 ± 7.0 years (range, 34-60 years). Demographic features and clinical presentations are summarized in Table 1.
| Group A (n = 16) | Group B (n = 19) | P value | |
| Age (yr, mean ± SD) | 50.81 ± 7.66 | 48.42 ± 6.37 | 0.320 |
| Female/male | 6/10 | 8/11 | 0.782 |
| SAA size (mm) | 16.43 ± 3.59 | 10.14 ± 2.07 | < 0.001 |
| SAAs | 0.156 | ||
| Single | 12 | 18 | |
| Multiple | 4 | 1 | |
| Technical success | 16 (100) | 19 (100) | 0.999 |
| Hospital stay (d) | 9.25 ± 2.84 | 8.52 ± 1.74 | 0.320 |
| Complications | |||
| Post-embolization syndrome | 6 (37.5) | 3 (15.8) | 0.245 |
| Major complications | 2 (12.5 ) | 0 (0) | 0.202 |
| Splenic abscess | 1 | 0 | |
| Pleural effusion | 1 | 0 | |
| Ascites | 0 | 0 | |
| CT follow-up (mo) | 38.69 ± 15.66 | 32.84 ± 15.02 | 0.269 |
| Clinical follow-up (mo) | 39.94 ± 14.90 | 35.16 ± 16.01 | 0.370 |
There are two embolization techniques: endovascular ligation that requires the positioning of the coils on either side of the aneurysm (“sandwich technique”) in order to attain complete occlusion[1,5,9,10], and embolization using coils limited to the aneurysmal sac with patency of the splenic artery. In general, the former technique was used for large or multiple SAAs, and the latter for small or single SAA. All embolization procedures were performed by two experienced interventional radiologists on a single plane angiography system under fluoroscopic guidance.
Prior to embolization, selective angiography of the celiac trunk, splenic artery, and superior mesenteric artery was performed in all patients via the right femoral artery with a 5-Fr diagnostic catheter. To avoid total splenic infarction, we confirmed patency of the collateral arteries, which were shown to be connected to the hilar splenic artery from the left gastric artery or from the gastroepiploic artery on a celiac arteriogram.
Coil embolization of the SAAs was performed after confirmation of these connections, and details of the coiling procedures were described previously[1,5,9-11]. Coils and/or gelfoam were used as embolization material either alone or in combination. In general, the embolization coils used in this series were standard 0.089-cm (0.035-in) fibered microcoils (Tornado; Cook, Bloomington, IN, United States). Post-embolization checks were performed with selective splenic, celiac and superior mesenteric artery angiograms to confirm occlusion of the main splenic artery and patency of the collateral arteries. Preoperative antibiotic prophylaxis was used routinely for 3 d. Following embolization, patients were monitored clinically, and antibiotics were administered after the procedure for several days to avoid infectious complications.
All the patients were followed at our outpatient clinic. Peripheral blood cell parameters, including white blood cell (WBC), red blood cell and platelet counts, were monitored at different time points prior to the procedure, on days 7 and 30, and subsequently at a 6-mo interval during follow-up. To determine a possible effect on liver function, aspartate aminotransferase (AST), alanine aminotransferase (ALT), total bilirubin (TB), albumin, and prothrombin time (PT) in serum were measured before and after the procedure at the same follow-up time point as evaluating the peripheral blood cells.
Abdominal CT scans were routinely performed before and 1 mo after the procedure, and subsequently every 6 mo during follow-up. CT images were obtained using a multislice GE Pro Speed machine (GE Medical Systems, Milwaukee, WI, United States) and included unenhanced and enhanced images (arterial phase, parenchymatous phase) with multiplanar 3D reconstruction. Based on enhanced CT images, we measured and compared the pretreatment splenic volume and the post-embolization residual splenic volume on a 3.1 workstation (GE Medical Systems) using volumetric analysis software. The infarcted splenic volume (mL) was calculated by subtracting the noninfarcted splenic volume from the pretreatment splenic volume. The splenic infarction rate was calculated by dividing the infarcted splenic volume by the pretreatment splenic volume (× 100%).
Data regarding (1) technical success; (2) liver function; (3) changes in splenic volume and (4) complications were evaluated at the time of the report or patient death. Technical success was defined as complete exclusion of the aneurysm on the post-embolization arteriogram, without major complications. Post-embolization syndrome was defined as fever, abdominal pain, or elevation of pancreatic enzymes over preprocedural values after splenic infarction.
Any potential complications following coil embolization, such as splenic abscess, splenic rupture, pneumonia, refractory ascites or pleural effusion, gastrointestinal bleeding, post-embolization syndrome, abdominal fullness, or appetite loss, were recorded.
All the data are expressed as mean ± SD. Dichotomous and categorical data are reported as numbers and percentages. The end points were determined technically and clinically. The technical end point was failed performance of the procedures. The clinical end points were loss to follow-up or death during or after the procedures. Comparisons of the variables between the two groups were performed using the Mann-Whitney test, χ2 test or Fisher’s exact test as appropriate. All statistical analyses were performed using SPSS version 13.0 (SPSS, Chicago, IL, United States).
The technical and initial clinical outcomes of the two groups are shown in Table 1. Coil embolization of the SAAs was technically successful in all 35 patients, with no procedure-related complications. The 30-d mortality rate was zero.
Complications after the procedures are listed in Table 1. The post-embolization syndrome, including abdominal pain, fever and vomiting, occurred in six patients (37.5%) in group A and three in group B (15.8%). One patient in group A had pleural effusion, which was resolved by thoracocentesis. One patient in group A suffered from persistent high fever, and was found to have splenic abscess on abdominal CT scan. The abscess was drained with a catheter and absorbed within 1 mo. There was no significant difference in hospital stays between the two groups (Table 1).
At the time of writing this manuscript, all patients were followed and assessed at 1 wk, 1 mo, 6 mo, and 1 year; 28 were assessed for 2 years and 13 were assessed for ≥ 4 years, prospectively, with a mean follow-up of 37.34 ± 15.47 mo (range, 13-66 mo). There were no significant differences in the number of patients in each follow-up period between the two groups.
Table 2 summarizes the follow-up clinical outcome between the two groups. In comparison with pre-procedural level of peripheral blood cell counts, including WBC and platelet counts in each of the two groups, there were no significant differences at each follow-up point after the procedures. There were also no significant differences in average WBC and platelet counts between the two groups at each follow-up point.
| Evaluation | Initial | 1 mo | 6 mo | 1 yr | 2 yr | ≥4 yr | ||||||
| Group A | Group B | Group A | Group B | Group A | Group B | Group A | Group B | Group A | Group B | Group A | Group B | |
| WBC count (× 109) | 6.1 ± 0.9 | 6.2 ± 1.0 | 6.2 ± 1.2 | 6.2 ± 1.1 | 6.2 ± 0.7 | 6.3 ± 1.0 | 6.0 ± 0.9 | 5.8 ± 0.8 | 5.9 ± 1.0 | 5.9 ± 1.0 | 5.9 ± 0.9 | 5.9 ± 1.1 |
| PLT count (× 109) | 172.1 ± 52.9 | 178.7 ± 48.4 | 190.3 ± 28.3 | 198.9 ± 28.2 | 191.2 ± 23.7 | 194.3 ± 27.8 | 191.2 ± 31.6 | 196.5 ± 29.3 | 196.6 ± 28.6 | 190.1 ± 34.1 | 180.6 ± 3-6.6 | 192.8 ± 27.8 |
| Splenic volume (cm3) | 289.8 ± 28.2 | 290.5 ± 26.5 | 222.3 ± 47.9a | 285.2 ± 29.2c | 202.3 ± 43.0a | 283.6 ± 30.5c | 199.1 ± 40.9a | 275.4 ± 38.2c | 197.7 ± 40.9a | 276.4 ± 43.0c | 201.3 ± 25.1a | 281.7 ± 42.1c |
In comparison with pre-procedural level of liver function parameters values, including AST, ALT, TB, albumin and PT, in each of the two groups, there were no significant differences at each follow-up point after the procedures. There were also no significant differences in average AST, ALT, TB, albumin and PT between the two groups at each follow-up point.
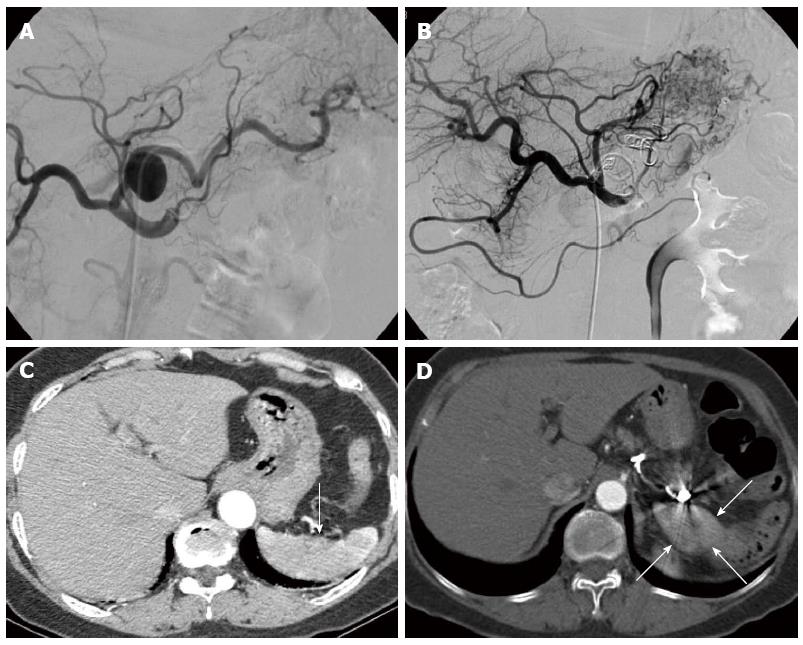
All patients were followed and assessed at 6 mo and 1 year; 28 were assessed for 2 years and 13 were assessed for ≥ 4 years, with a mean follow-up of 35.5 ± 15.4 mo (range, 12-66 mo). After the procedures, splenic volume decreased significantly in group A, peaked at 1 mo after the procedures, and was then maintained at about the same size during follow-up (Table 2). In group B, there was no obvious decrease in splenic volume after the procedures. There were significant differences in splenic volume at each follow-up point between the two groups. In addition, there were also significant differences in splenic volume in group A between preoperatively and at each follow-up point (Table 2, Figure 1).
There are three main findings from this study: (1) no significant differences were found in peripheral blood cell counts, including WBCs and platelets, between preoperatively and at each follow-up point after the procedures, and between the two groups at each follow-up point; (2) no significant differences were found in liver function between preoperatively and at each follow-up point after the procedures and between the two groups at each follow-up point; and (3) splenic volume in group A was significantly smaller after embolization. To the best of our knowledge, this is the first report to evaluate the clinical outcome of total embolization of the main splenic artery for patients with SAAs and normal spleen.
Therapeutic options available for patients with SAAs include conventional open surgery, endovascular treatment, and the more recently introduced technique of laparoscopic surgery. The traditional treatment was ligation of the artery or aneurysm or excision of the lesion, with or without partial or total splenectomy, and occasionally with distal pancreatectomy[12,13]. However, the mortality rate associated with this procedure was approximately 1.3% and the morbidity rate was 9% for aneurysms[12].
During the past decade, endovascular techniques including transcatheter embolization and covered stent placement were introduced as alternatives to conventional surgery[2,12,14,15]. These techniques can be used to treat most SAAs regardless of clinical presentation, etiology, and location. Endovascular treatment is also indicated for ruptured SAAs, especially when the site is difficult to access during conventional surgery or when the operative risk is high because the patient is in poor general health[3,16]. Advantages over surgery include accurate localization of the aneurysm, assessment of collateral flow, low risk for patients who are poor surgical candidates[17], and easier approach to aneurysms whose surgical exposure is difficult.
Nowadays, transcatheter coil embolization is the commonly used method and has been shown to be safe and effective for the treatment of the SAAs[1,4-8,18-23]. Although percutaneous treatment with covered stents has produced favorable results[24,25] with main splenic arterial patency, they are difficult to deploy in tortuous vessels, and thrombosis may occur after stenting.
There are two embolization techniques: coil embolization of the aneurysmal sac with patency of the splenic artery, and embolization of the main splenic artery with complete occlusion of the artery and the SAAs[1,5,9,10]. The former technique was often used for single and small SAAs, and the latter was often applied for large or multiple SAAs. In this study, although shrinkage of the splenic volume in group A was obtained after total embolization of the main splenic artery, no mortality occurred, and the complications were under control, which was confirmed by the patency of the collateral arteries.
In addition, an increase in WBC and platelet counts after total embolization of the main splenic artery for patients with hypersplenism has been reported by He et al[26,27] and Gu et al[28]. In the present study, there were no significant differences in WBC and platelet counts between preoperatively and at each follow-up point. In other words, there was no increase or decrease in WBC and platelet counts in group A after embolization. Furthermore, there were no differences in liver function parameters between preoperatively and at each follow-up point, which was in agreement with He et al[26,27] and Gu et al[28]. These results indicated that total embolization of the main splenic artery is a safe procedure for patients with SAAs and normal spleen.
In this study, we found that the splenic volume in three patients in group A did not decrease after total embolization of the main splenic artery. We thought that the main reason may be the recanalization of the splenic artery. Another possible reason was that there was sufficient blood supply for the spleen from these connections.
Our study had the following limitations. First, the study was retrospective, and the patient population was small, which may prevent generalization of our results. Second, severe complications may occur when the collateral arteries are lacking or not consummate. Confirmation of the patency of the collateral arteries, which connected to the hilar splenic artery from the left gastric artery or from the gastroepiploic artery, was a necessary step prior to total embolization of the main splenic artery for SAAs. Third, CT angiography involves exposure of the patients to ionizing radiation and the administration of intravenous contrast material. Lastly, follow-up angiography was not performed in this study, thus, the possibility of recanalization of the main splenic artery or the SAAs could not be determined.
In conclusion, in this retrospective study, except for shrinkage of splenic volume in patients undergoing total embolization of the main splenic artery, no changes in WBC and platelet counts and liver function parameters were found. These results indicated that total embolization of the main splenic artery is a safe and feasible procedure for patients with SAAs and normal spleen. Further clinical trials and extended follow-up studies are needed.
Coil embolization is now a widely accepted treatment for splenic artery aneurysms (SAAs); however, for patents with large or multiple SAAs, total embolization of the splenic artery sometime must be performed to achieve complete occlusion of the SAAs.
Total embolization of the splenic artery has been shown to be a safe and effective method for the treatment of SAAs, but the changes in splenic function and morphology after embolization have rarely been reported, especially in patients with SAAs and normal spleen. We retrospectively evaluated the clinical outcomes of total embolization of the main splenic artery for patients with SAAs and normal spleen.
The use of total embolization of the splenic artery was devised for the management of patients with SAAs and normal spleen. All procedures were performed under fluoroscopic control. This is believed to be the first report to evaluate the clinical outcomes of total embolization of the main splenic artery for patients with SAAs and normal spleen.
Total embolization of the main splenic artery is a safe and feasible procedure for the patients with SAAs and normal spleen.
Total embolization of the main splenic artery is the technique of embolization of the main splenic artery with complete occlusion of the artery and SAAs.
The authors reported total embolization of the main splenic artery for patients with SAAs and normal spleen. Thirty-five consecutive patients with SAAs were classified into two groups: coil embolization of the main splenic artery with complete occlusion of the artery and aneurysms (group A), and coil embolization of the aneurysmal sac with patency of the splenic artery (group B). The results reveal that except for shrinkage of splenic volume in patients with total embolization of the main splenic artery, no changes in white blood cell and platelet counts or liver function parameters were found. These results suggest that total embolization of the main splenic artery is a safe and feasible procedure for the patients with SAAs and normal spleen.
P- Reviewers: Murata S, Said SAM, Wu HP S- Editor: Cui XM L- Editor: Wang TQ E- Editor: Zhang DN
| 1. | Laganà D, Carrafiello G, Mangini M, Fontana F, Dizonno M, Castelli P, Fugazzola C. Endovascular treatment of splenic artery aneurysms. Radiol Med. 2005;110:77-87. [PubMed] |
| 2. | Carr SC, Pearce WH, Vogelzang RL, McCarthy WJ, Nemcek AA, Yao JS. Current management of visceral artery aneurysms. Surgery. 1996;120:627-33; discussion 633-4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 194] [Cited by in RCA: 163] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 3. | Gabelmann A, Görich J, Merkle EM. Endovascular treatment of visceral artery aneurysms. J Endovasc Ther. 2002;9:38-47. [PubMed] |
| 4. | Trastek VF, Pairolero PC, Joyce JW, Hollier LH, Bernatz PE. Splenic artery aneurysms. Surgery. 1982;91:694-699. [PubMed] |
| 5. | Loffroy R, Guiu B, Cercueil JP, Lepage C, Cheynel N, Steinmetz E, Ricolfi F, Krausé D. Transcatheter arterial embolization of splenic artery aneurysms and pseudoaneurysms: short- and long-term results. Ann Vasc Surg. 2008;22:618-626. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 83] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 6. | Venkatesh SK, Kumar S, Baijal SS, Phadke RV, Kathuria MK, Gujral RB. Endovascular management of pseudoaneurysms of the splenic artery: experience with six patients. Australas Radiol. 2005;49:283-288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 7. | Piffaretti G, Tozzi M, Lomazzi C, Rivolta N, Riva F, Caronno R, Castelli P. Splenic artery aneurysms: postembolization syndrome and surgical complications. Am J Surg. 2007;193:166-170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 57] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 8. | Laganà D, Carrafiello G, Mangini M, Dionigi G, Caronno R, Castelli P, Fugazzola C. Multimodal approach to endovascular treatment of visceral artery aneurysms and pseudoaneurysms. Eur J Radiol. 2006;59:104-111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 117] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 9. | Guillon R, Garcier JM, Abergel A, Mofid R, Garcia V, Chahid T, Ravel A, Pezet D, Boyer L. Management of splenic artery aneurysms and false aneurysms with endovascular treatment in 12 patients. Cardiovasc Intervent Radiol. 2003;26:256-260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 139] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 10. | Probst P, Castañeda-Zuñiga WR, Gomes AS, Yonehiro EG, Delaney JP, Amplatz K. Nonsurgical treatment of splenic-artery aneurysms. Radiology. 1978;128:619-623. [PubMed] |
| 11. | Takahashi T, Arima Y, Yokomuro S, Yoshida H, Mamada Y, Taniai N, Kawano Y, Mizuguchi Y, Shimizu T, Akimaru K. Splenic artery embolization before laparoscopic splenectomy in children. Surg Endosc. 2005;19:1345-1348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 25] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 12. | McDermott VG, Shlansky-Goldberg R, Cope C. Endovascular management of splenic artery aneurysms and pseudoaneurysms. Cardiovasc Intervent Radiol. 1994;17:179-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 121] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 13. | Busuttil RW, Brin BJ. The diagnosis and management of visceral artery aneurysms. Surgery. 1980;88:619-624. [PubMed] |
| 14. | Sessa C, Tinelli G, Porcu P, Aubert A, Thony F, Magne JL. Treatment of visceral artery aneurysms: description of a retrospective series of 42 aneurysms in 34 patients. Ann Vasc Surg. 2004;18:695-703. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 171] [Cited by in RCA: 157] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 15. | Varnagy D, Sendzischew M, Hertz JA, Sendzischew H. Endovascular management of a ruptured splenic artery aneurysm. Vasc Endovascular Surg. 2007;41:68-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 16. | Kasirajan K, Greenberg RK, Clair D, Ouriel K. Endovascular management of visceral artery aneurysm. J Endovasc Ther. 2001;8:150-155. [PubMed] |
| 17. | Huang YK, Hsieh HC, Tsai FC, Chang SH, Lu MS, Ko PJ. Visceral artery aneurysm: risk factor analysis and therapeutic opinion. Eur J Vasc Endovasc Surg. 2007;33:293-301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 92] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 18. | Yamamoto S, Hirota S, Maeda H, Achiwa S, Arai K, Kobayashi K, Nakao N. Transcatheter coil embolization of splenic artery aneurysm. Cardiovasc Intervent Radiol. 2008;31:527-534. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 61] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 19. | Tulsyan N, Kashyap VS, Greenberg RK, Sarac TP, Clair DG, Pierce G, Ouriel K. The endovascular management of visceral artery aneurysms and pseudoaneurysms. J Vasc Surg. 2007;45:276-283; discussion 283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 399] [Cited by in RCA: 425] [Article Influence: 23.6] [Reference Citation Analysis (1)] |
| 20. | Ikeda O, Tamura Y, Nakasone Y, Iryou Y, Yamashita Y. Nonoperative management of unruptured visceral artery aneurysms: treatment by transcatheter coil embolization. J Vasc Surg. 2008;47:1212-1219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 87] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 21. | Roland J, Brody F, Venbrux A. Endovascular management of a splenic artery aneurysm. Surg Laparosc Endosc Percutan Tech. 2007;17:459-461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 22. | Schmittling ZC, McLafferty R. Transcatheter embolization of a splenic artery aneurysm. J Vasc Surg. 2004;40:1049. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 23. | Kramann B, Daoyu H, Kubale R, Schneider G. [Experiences with the endovascular embolization therapy of aneurysms of the splanchnic arteries--a report on 13 cases]. Rofo. 1995;163:417-423. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 24. | Carrafiello G, Laganà D, Dizonno M, Mangini M, Fugazzola C. Endovascular ligature of splenic artery aneurysm with Amplatzer Vascular Plug: a case report. Cardiovasc Revasc Med. 2007;8:203-206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 25. | Larson RA, Solomon J, Carpenter JP. Stent graft repair of visceral artery aneurysms. J Vasc Surg. 2002;36:1260-1263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 112] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 26. | He XH, Gu JJ, Li WT, Peng WJ, Li GD, Wang SP, Xu LC, Ji J. Comparison of total splenic artery embolization and partial splenic embolization for hypersplenism. World J Gastroenterol. 2012;18:3138-3144. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 26] [Cited by in RCA: 34] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 27. | He XH, Li WT, Peng WJ, Li GD, Wang SP, Xu LC. Total embolization of the main splenic artery as a supplemental treatment modality for hypersplenism. World J Gastroenterol. 2011;17:2953-2957. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 10] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 28. | Gu JJ, He XH, Li WT, Ji J, Peng WJ, Li GD, Wang SP, Xu LC. Safety and efficacy of splenic artery coil embolization for hypersplenism in liver cirrhosis. Acta Radiol. 2012;53:862-867. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 25] [Article Influence: 1.9] [Reference Citation Analysis (0)] |