Published online Apr 28, 2014. doi: 10.3748/wjg.v20.i16.4835
Revised: December 28, 2013
Accepted: March 5, 2014
Published online: April 28, 2014
Processing time: 192 Days and 17.7 Hours
Splenic artery aneurysm is one of the most common visceral aneurysms, and patients with this type of aneurysm often present without symptoms. However, when rupture occurs, it can be a catastrophic event. Although most of these aneurysms can be treated with percutaneous embolization, some located in uncommon parts of the splenic artery may make this approach impossible. We present a patient with an aneurysm in the proximal splenic artery, close to the celiac trunk, which was treated by laparoscopic ligation only, without resection of the aneurysm, and with long-term preservation of splenic function.
Core tip: An aneurysm in the proximal splenic artery is rare. Few cases of an aneurysm in the proximal splenic artery treated by laparoscopic techniques have been reported in the literature. We present a case of splenic artery aneurysm located in the proximal splenic artery which was treated by laparoscopic ligation with long-term preservation of splenic function. This is the first case of laparoscopic ligation of a proximal artery aneurysm with preservation of splenic function to be reported in the English literature.
- Citation: Wei YH, Xu JW, Shen HP, Zhang GL, Ajoodhea H, Zhang RC, Mou YP. Laparoscopic ligation of proximal splenic artery aneurysm with splenic function preservation. World J Gastroenterol 2014; 20(16): 4835-4838
- URL: https://www.wjgnet.com/1007-9327/full/v20/i16/4835.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i16.4835
Splenic artery aneurysms (SAAs) account for 46%-60% of all visceral artery aneurysms[1]. Most occur in the distal third of the splenic artery (75%) followed by the middle third (20%)[2]. Aneurysms in the proximal splenic artery are uncommon. Treatment of a SAA includes laparotomy, laparoscopy or endovascular techniques. In recent years, open aneurysm repair of SAAs has been largely replaced by minimally invasive surgery, such as endovascular procedures, which result in less surgical trauma and faster postoperative recovery. However, only selected aneurysms are suitable for these procedures, as marked tortuosity of the artery or SAA in the proximal splenic artery may not be suitable for endovascular management. Thus, in these rare cases, laparoscopy may be a challenging alternative, not only to open surgery, but also to endovascular procedures.
To our knowledge, few cases of SAA in the proximal splenic artery treated by laparoscopic techniques have been reported in the literature. The authors present a patient with an aneurysm located in the proximal splenic artery, which was treated by laparoscopic ligation with long-term preservation of splenic function.
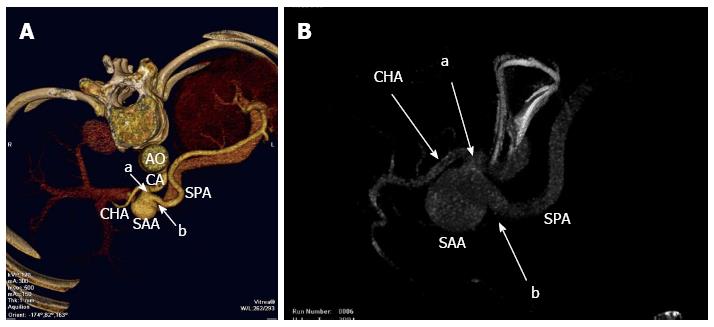
An asymptomatic 49-year-old woman was found to have a splenic artery aneurysm on medical examination. Computed tomography scan revealed a 3 cm SAA. Both three-dimensional reconstruction and angiography demonstrated the presence of a 3 cm aneurysm in the proximal splenic artery, approximately 0.8 cm from the celiac trunk (Figure 1). Considering the anatomic location of the aneurysm, endovascular treatment was not proposed due to recanalization and coil migration. Thus, laparoscopic surgery was deemed the optimal treatment option. It was decided to attempt simple laparoscopic ligation without resecting the aneurysm.
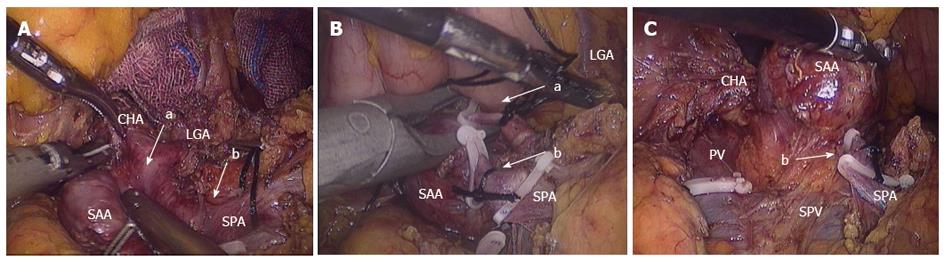
The patient was placed in the supine position. Five ports were inserted and a pneumoperitoneum was created. First, we divided the gastrocolic ligament, revealing the pancreatic edge, then identified the splenic artery and exposed the aneurysm. We separated its proximal and distal parts, and clips were used to ligate the aneurysm proximally and distally (Figure 2). The collateral vessels of the aneurysm were also completely dissected, thus isolating the aneurysm with no retrograde filling. The whole spleen appeared dusky, but returned to normal at the end of the procedure. The abdominal cavity was irrigated with normal saline and a drain was placed under the aneurysm to drain the fluid and prevent contingent complications caused by pancreatic leakage.
The operative time was 50 min and blood loss was 10 mL. Three days later, abdominal vascular ultrasound showed a hypoechoic mass between the proximal part of the splenic artery and celiac trunk with no color flow signals (Figure 3A), and the blood flow into the splenic vein was affluent (Figure 3B). The patient had a smooth recovery with no complications and was discharged on postoperative day 5. During the postoperative follow-up period, she recovered very well with no abdominal pain or pancreatic insufficiency. The three-dimensional computed tomography reconstruction (two months after surgery) revealed no recurrence of the aneurysm and her splenic function was well maintained (Figure 3C).
Despite an extremely low incidence and almost no symptoms of SAA, death can occur if the aneurysm ruptures[3]. The available evidence suggests that active treatment should be initiated if the aneurysm is larger than 2 cm in patients at high risk of rupture, such as during pregnancy, patients of childbearing age or following liver transplantation.
Transcatheter embolization is currently considered to be the first-line treatment in most patients with SAAs, since the procedure can be carried out under local anesthesia with minimal trauma to the patient[4]. However, this technique may not be proposed if the SAA is located at the hilum of the spleen or if the splenic artery is particularly tortuous. In addition, it presents some critical points: recanalization, coil migration and distal infarction with abscess formation, and the post-treatment splenic flow can be compromised due to related splenic malfunction and infarction[5].
Stent grafting also requires careful patient selection as the size and tortuosity of the splenic artery as well as the location of the aneurysm may have limitations in the deployment of the stent graft[6]. Furthermore, complications related to stent migration and arterial occlusion also have to be considered[7]. Moreover, following stent grafting, life-long oral antiplatelet drugs are required and the long-term durability and patency of these grafts are unknown.
In the present case, the SAA was in the proximal splenic artery, close to the celiac trunk, and the splenic artery was tortuous in this location. Thus, transcatheter embolization and stent grafting were considered inappropriate treatment choices. Laparoscopic management was deemed to be the best treatment option, and was to include either resection of the SAA or just simple ligation of the SAA. Laparoscopic resection of orthotopic SAAs has been espoused by a number of authors as a less invasive alternative to open surgery[8]. However, it was performed only for aneurysms of small diameter, 2-2.5 cm, affecting the middle or distal third of the artery. In addition, this technique is controversial as it leaves a vascular stump exposing it to pulsatile arterial pressure and the possibility of recurrence[9].
To date, laparoscopic ligation of aneurysms has only been reported in two cases, and both were located in the middle or distal third of the splenic artery[10,11]. An SAA in the proximal splenic artery treated by laparoscopic ligation has not yet been reported. In our case, the location of the SAA was in the proximal part of the splenic artery, close to the celiac trunk, and the splenic artery was tortuous in this location. Therefore, we chose laparoscopy as the optimal treatment. As an SAA is a non-solid tumor, it was not necessary to resect the aneurysm. Preoperative evaluation is essential and blocking the collateral circulation of the SAA is the most important step in the procedure, which ultimately leads to no retrograde filling of the SAA. The risk associated with laparoscopic ligation of the SAA was deficient residual blood flow to the spleen, thus leading to splenic infarction and possible evolution into a splenic abscess. Therefore, intraoperative ultrasound may contribute to determination of the residual blood flow. To the best of our knowledge, this is the first case of laparoscopic ligation of a splenic artery aneurysm in the proximal part of the splenic artery. This approach greatly reduces blood loss and results in a shorter operative time compared to laparoscopic resection. In addition, spleen function was completely preserved. The patient had a faster postoperative recovery and a good long-term outcome associated with preservation of splenic function. Therefore, we believe that laparoscopic ligation is suitable for aneurysms located in the proximal splenic artery.
In conclusion, laparoscopic ligation of a SAA in the proximal splenic artery is safe and effective. It offers good postoperative recovery with a good long-term outcome due to preservation of splenic function. Therefore, laparoscopic ligation may be the preferred treatment in cases in which other treatments are unfeasible.
Incidental finding of a 3-cm aneurysm in the proximal splenic artery in an asymptomatic 49-year-old female patient on routine medical examination.
Incidental finding of a 3-cm aneurysm in the proximal splenic artery on computed tomography (CT).
To exclude a tortuous splenic artery and calcified lymph nodes, three-dimensional CT reconstruction and angiography were performed.
The laboratory tests were all within normal ranges.
Three-dimensional CT reconstruction and angiography revealed a 3-cm aneurysm in the proximal splenic artery, 0.8 cm from the celiac trunk.
Laparoscopic ligation of the proximal splenic artery aneurysm, without resection of the aneurysm.
To date, laparoscopic ligation of aneurysms has only been reported in two cases, and both were located in the middle or distal third of the splenic artery.
Laparoscopic ligation of a splenic artery aneurysm is safe and effective, and should be considered when other treatment modalities are not feasible.
The authors presented their successful experience of laparoscopic ligation of asymptomatic proximal splenic artery aneurysm in 49-year-old woman. The paper is very well presented with very nice intraoperative figures. It is an interesting rare case report with nice laparoscopic views.
P- Reviewers: Pavlidis TE, Pogorelic Z, Yokoyama N S- Editor: Ma YJ L- Editor: A E- Editor: Wu HL
| 1. | Trastek VF, Pairolero PC, Joyce JW, Hollier LH, Bernatz PE. Splenic artery aneurysms. Surgery. 1982;91:694-699. [PubMed] |
| 2. | Al-Habbal Y, Christophi C, Muralidharan V. Aneurysms of the splenic artery - a review. Surgeon. 2010;8:223-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 119] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 3. | Hunsaker DM, Turner S, Hunsaker JC. Sudden and unexpected death resulting from splenic artery aneurysm rupture: two case reports of pregnancy-related fatal rupture of splenic artery aneurysm. Am J Forensic Med Pathol. 2002;23:338-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 29] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 4. | Tulsyan N, Kashyap VS, Greenberg RK, Sarac TP, Clair DG, Pierce G, Ouriel K. The endovascular management of visceral artery aneurysms and pseudoaneurysms. J Vasc Surg. 2007;45:276-283; discussion 283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 399] [Cited by in RCA: 425] [Article Influence: 23.6] [Reference Citation Analysis (1)] |
| 5. | Tiberio GA, Bonardelli S, Gheza F, Arru L, Cervi E, Giulini SM. Prospective randomized comparison of open versus laparoscopic management of splenic artery aneurysms: a 10-year study. Surg Endosc. 2012;Jun 30; Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 6. | Karaman K, Onat L, Sirvanci M, Olga R. Endovascular stent graft treatment in a patient with splenic artery aneurysm. Diagn Interv Radiol. 2005;11:119-121. [PubMed] |
| 7. | Góes Junior AM, Góes AS, de Albuquerque PC, Palácios RM, Abib Sde C. Endovascular treatment of giant splenic artery aneurysm. Case Rep Surg. 2012;2012:964093. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Arca MJ, Gagner M, Heniford BT, Sullivan TM, Beven EG. Splenic artery aneurysms: methods of laparoscopic repair. J Vasc Surg. 1999;30:184-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 62] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 9. | Reardon PR, Otah E, Craig ES, Matthews BD, Reardon MJ. Laparoscopic resection of splenic artery aneurysms. Surg Endosc. 2005;19:488-493. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 38] [Article Influence: 1.9] [Reference Citation Analysis (2)] |
| 10. | Sandford RM, Lloyd DM, Ross Naylor A. Laparoscopic ligation of splenic artery aneurysm. Surg Laparosc Endosc Percutan Tech. 2006;16:102-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |