Published online Feb 14, 2013. doi: 10.3748/wjg.v19.i6.960
Revised: December 18, 2012
Accepted: January 11, 2013
Published online: February 14, 2013
Processing time: 108 Days and 12 Hours
Left supraclavicular lymph node metastasis is a rare presentation of hepatocellular carcinoma (HCC). This phenomenon is easily neglected in the clinic. A 56-year-old man presented with HCC. On examination, a 1cm long left supraclavicular lymph node was palpated. Auxiliary examination indicated a lesion located in the right lobe of the liver. Fine needle aspiration cytology (FNAC) of the enlarged lymph node was performed; however, only necrosis was found. Hepatectomy was performed and HCC was confirmed by Hematoxylin-Eosin staining. However, 14 d after surgery, significantly enlarged left supraclavicular lymph nodes, a new intrahepatic lesion, and pulmonary and mediastinal metastasis appeared. An excisional biopsy of the left supraclavicular lymph node was performed, and its findings confirmed metastatic HCC. The patient’s HCC rapidly progressed and he died one month later. It is possible for HCC to metastasize to the left supraclavicular lymph node. Surgeons should always consider an overall physical examination. When left supraclavicular lymphadenopathy of unknown origin is encountered, FNAC should be performed initially. If the results are negative, an excisional biopsy and subsequent Positron emission tomography - computed tomography scanning should be performed. These are very important for making the correct diagnosis and for selecting reasonable therapies.
- Citation: Liu T, Gao JF, Yi YX, Ding H, Liu W. Misdiagnosis of left supraclavicular lymph node metastasis of hepatocellular carcinoma: A case report. World J Gastroenterol 2013; 19(6): 960-963
- URL: https://www.wjgnet.com/1007-9327/full/v19/i6/960.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i6.960
Hepatocellular carcinoma (HCC) is a common malignancy of the digestive tract. The main route of spread is hematogenous, that is, by invasion of the portal venous system or hepatic venous system[1]. Lymphatic metastases are uncommon. For patients with HCC larger than 5 cm, tumor-related factors predict outcomes and survival[2]. Left supraclavicular lymphadenopathy may be the sign of a metastatic tumor, mostly from lung cancer, gastric cancer, nasopharyngeal cancer and breast cancer[3]. However, HCC rarely metastasizes to the left supraclavicular lymph node and few relevant reports are available in the literature. Here, we present a case of HCC that manifested as left supraclavicular lymphadenopathy and analyze the reasons for the initial misdiagnosis.
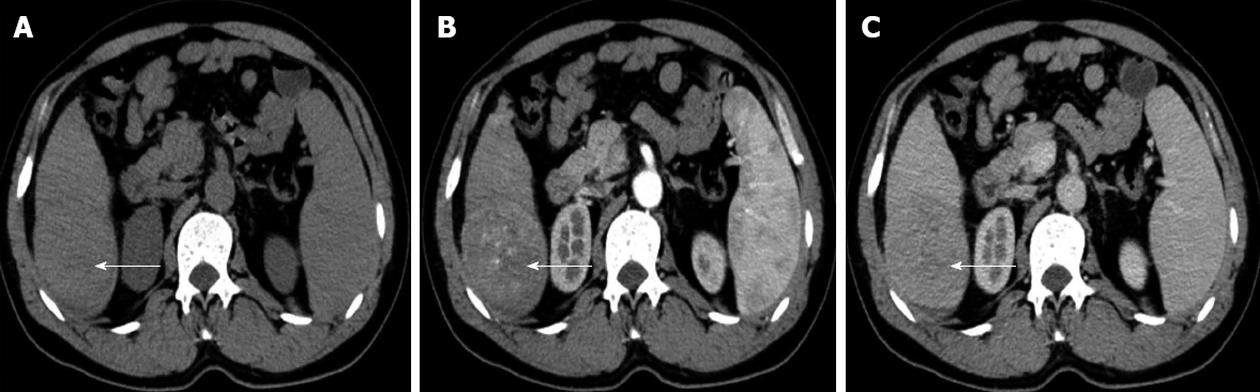
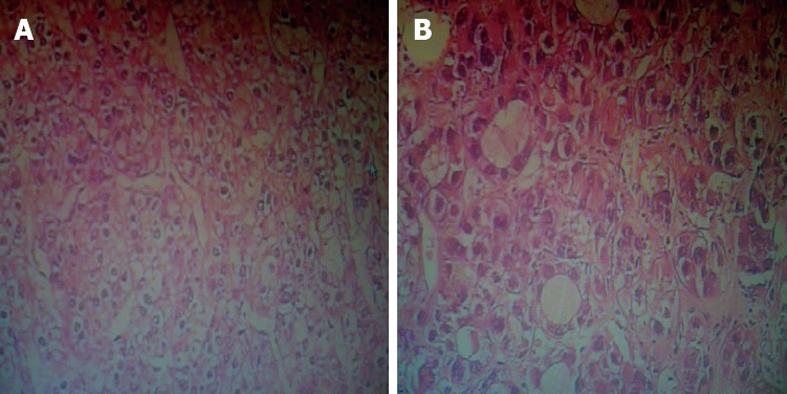
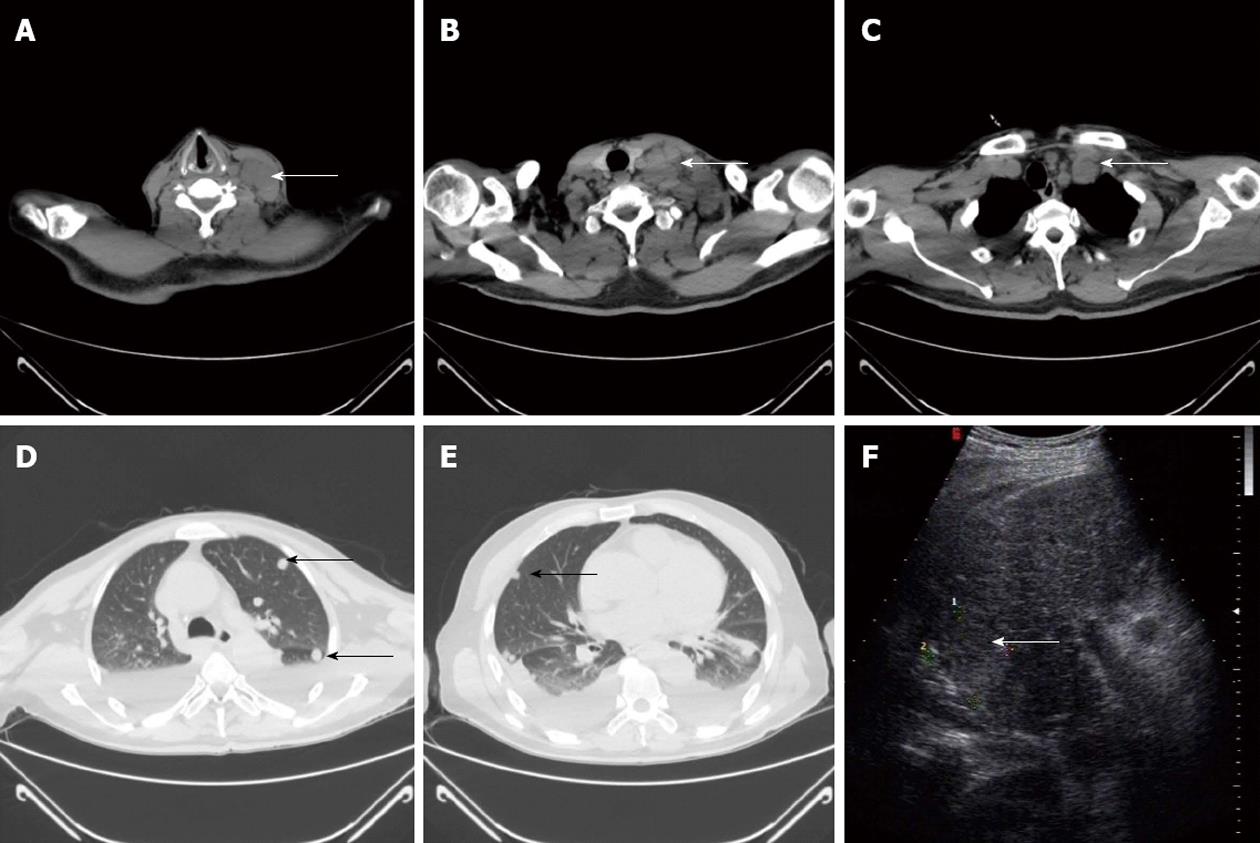
A 56-year-old man suffering from HCC was referred to our hospital. His chief complaint was abdominal pain. He had hypertension that was successfully treated with oral medication. On examination, a 1 cm long left supraclavicular lymph node was palpated and it was slightly tender. Examination of the chest did not reveal any signs of bronchospasm. Varicose veins on the thoracic and abdominal wall were not observed. Neurological examination did not demonstrate any deficit. Laboratory examination revealed a platelet count of 89 × 109/L. His alpha-fetoprotein (AFP) level was 695.4 ng/mL (normal < 10.9 ng/mL). Serum hepatitis B surface antigen was positive. HBV DNA quantification was within normal limits. Renal and liver function tests, coagulation function, electronic laryngoscopy and gastroscopy were also normal. Abdominal computed tomography indicated an 8 cm lesion located in the right lobe of the liver (VI segment) (Figure 1A), which was showed significant enhancement during the hepatic arterial phase (Figure 1B), but no enhancement during the portal phase (Figure 1C). The vascular system was normal, and no enlarged lymph nodes were found. No new lesions were found by contrast-enhanced ultrasound. A chest X-ray revealed no lung metastasis. Fine needle aspiration cytology (FNAC) of the enlarged left supraclavicular lymph node showed only necrosis. A hepatectomy was performed without hepatic hilar occlusion. Doppler ultrasound was used to define the tumor margin during the operation. The dissection line was 1 cm outside the tumor margin. Diagnosis was confirmed as HCC with moderate differentiation by Hematoxylin-Eosin staining (Figure 2A), and the resection margin was negative. Initially, the patient showed a good recovery. However, 14 d after surgery, enlarged left supraclavicular lymph nodes were observed to be firm and fixed. To exclude the possibility of malignant lymphoma, an excisional biopsy of the left supraclavicular lymph node was performed, and its findings confirmed metastatic HCC (Figure 2B). Thoracic computed tomography showed significantly enlarged left supraclavicular lymph nodes (Figure 3A), part of which were fused into masses (Figure 3B). Their diameters ranged from 2 cm to 6 cm. Enlarged lymph nodes appeared in mediastinum (Figure 3C) and round nodules were distributed in both lungs (Figure 3D and E). A new lesion was detected in the liver via Doppler ultrasound (Figure 3F). Laboratory examination revealed an AFP level > 1050 ng/mL. The patient rapidly declined and died one month later.
Distant metastasis of HCC occurs in three main ways: Hematogenous dissemination, lymphatic metastasis and implantation metastasis. Hematogenous dissemination is common, whereas lymphatic metastasis is uncommon. Lymphatic metastasis has been documented in 25.5% of patients at different stages of HCC. Hilar lymph nodes and para-aortic nodes are the major metastatic sites[4]. Nowadays, a hepatectomy has become one of the most popular treatments for HCC, and understanding lymph node metastasis in HCC is indispensable at surgery for improving the patient’s prognosis. A previous study revealed that the incidence of lymph node metastasis in operable HCC patients was low, but patients with lymph node metastasis had a poorer prognosis[5].
HCC metastasis to left supraclavicular lymph nodes, although uncommon, does occur, probably via the hepatic node and then through the thoracic duct[6]. Early discovery of distant metastasis is important for tumor staging, prognosis judgment and therapy determination in those patients with HCC. However, left supraclavicular lymphadenopathy is not the initial presentation in most conditions; therefore, overall physical examination, especially of the supraclavicular fossa, should not be overlooked. When the left supraclavicular lymph node is involved in the tumor, patients already have advanced disease. In this situation, it is more appropriate for patients to adopt non-operative treatment, including hepatic arterial chemoembolization, molecular targeted therapy, chemotherapy and radiotherapy, instead of surgery. For palpable left supraclavicular lymph nodes, FNAC is not only useful for diagnosing various lesions, but also can help in deciding on appropriate management[7]. However, the diagnosis may sometimes be difficult, with the potential for clinically important diagnostic errors. Therefore, FNAC can also show false negative results for positive lesions[8]. It is presumed that multiple factors can result in misdiagnosis[9], including inadequate specimens, poor smears, inaccurate puncture location, and lack of ancillary studies (cell blocks, immunocytochemistry and electron microscopy)[10].
For a patient with left supraclavicular lymphadenopathy who is highly suspected to have a metastatic tumor, FNAC can be used as a first line diagnostic modality in the evaluation of enlarged lymph nodes. If negative findings are obtained, an excisional biopsy is necessary, which is the gold standard for diagnosis, and Positron emission tomography - computed tomography (PET-CT) scanning should be performed, which allows identification of the primary site and metastatic lesions, including bone and soft tissue metastases, in a single examination.
In our case, an enlarged left supraclavicular lymph node was noticed preoperatively. The negative findings of FNAC and no further examination resulted in incorrect tumor staging. The disease progressed rapidly after surgery. Metastatic HCC was not confirmed until an excisional biopsy was performed.
In summary, we have presented an uncommon case of advanced HCC with left supraclavicular lymph node metastasis. When similar cases are encountered, FNAC should be performed initially. When the results of FNAC, are negative, further tests, such as an excisional biopsy and PET-CT scanning will help to achieve a definitive diagnosis. Such diagnoses will help to prioritize the patient’s management protocol.
P- Reviewers Julie NL, Hoogenraad TU S- Editor Huang XZ L- Editor Stewart GJ E- Editor Li JY
| 1. | Kew MC, Paterson AC. Unusual clinical presentations of hepatocellular carcinoma. Trop Gastroenterol. 1985;6:10-22. [PubMed] |
| 2. | Schiffman SC, Woodall CE, Kooby DA, Martin RC, Staley CA, Egnatashvili V, McMasters KM, Scoggins CR. Factors associated with recurrence and survival following hepatectomy for large hepatocellular carcinoma: a multicenter analysis. J Surg Oncol. 2010;101:105-110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 37] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 3. | Gupta N, Rajwanshi A, Srinivasan R, Nijhawan R. Pathology of supraclavicular lymphadenopathy in Chandigarh, north India: an audit of 200 cases diagnosed by needle aspiration. Cytopathology. 2006;17:94-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Watanabe J, Nakashima O, Kojiro M. Clinicopathologic study on lymph node metastasis of hepatocellular carcinoma: a retrospective study of 660 consecutive autopsy cases. Jpn J Clin Oncol. 1994;24:37-41. [PubMed] |
| 5. | Sun HC, Zhuang PY, Qin LX, Ye QH, Wang L, Ren N, Zhang JB, Qian YB, Lu L, Fan J. Incidence and prognostic values of lymph node metastasis in operable hepatocellular carcinoma and evaluation of routine complete lymphadenectomy. J Surg Oncol. 2007;96:37-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 71] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 6. | Selvasekaran R, Cherian JV, Venkataraman J. Metastasis of hepatocellular carcinoma to Virchow’s node: have the tumor cells gone astray? Hepatobiliary Pancreat Dis Int. 2007;6:650-652. [PubMed] |
| 7. | Gupta RK, Naran S, Lallu S, Fauck R. The diagnostic value of fine needle aspiration cytology (FNAC) in the assessment of palpable supraclavicular lymph nodes: a study of 218 cases. Cytopathology. 2003;14:201-207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 36] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 8. | Ellison E, LaPuerta P, Martin SE. Supraclavicular masses: results of a series of 309 cases biopsied by fine needle aspiration. Head Neck. 1999;21:239-246. [PubMed] |
| 9. | Stanley MW. Selected problems in fine needle aspiration of head and neck masses. Mod Pathol. 2002;15:342-350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 42] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 10. | Mutreja D, Nijhawan VS, Srinivasa V, Lakhtakia R, Subramanya H. Value of ancillary studies in the evaluation of fine-needle aspiration specimens: Our experience. J Cytol. 2012;29:103-110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |