INTRODUCTION
A gastric diverticulum is a pouch protruding from the gastric wall and has similar characteristics to duodenal, jejunal and colonic diverticula[1]. Generally it is a very rare and uncommon condition with a prevalence of 0.04% in contrast radiographs and 0.01%-0.11% in upper gastrointestinal endoscopies[2,3]. It occurs equally in men and women, typically in the fifth and sixth decades. Although most patients are asymptomatic, occasionally abdominal symptoms occur, including vague pain, epigastric fullness, bleeding or perforation[4-6]. Gastric diverticula are usually 1-3 cm in diameter and can be divided into true diverticula comprising all gastrointestinal layers and pseudodiverticula which are often found in the antrum[7,8]. We present two cases of uncommon large symptomatic gastric diverticula with discussion of the cornerstones in management, and report a minimally invasive solution, with a brief review of literature.
CASE REPORT
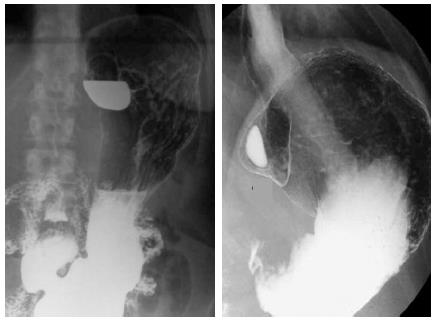
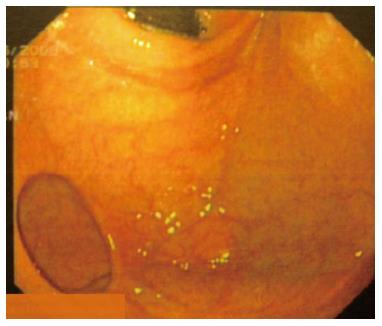
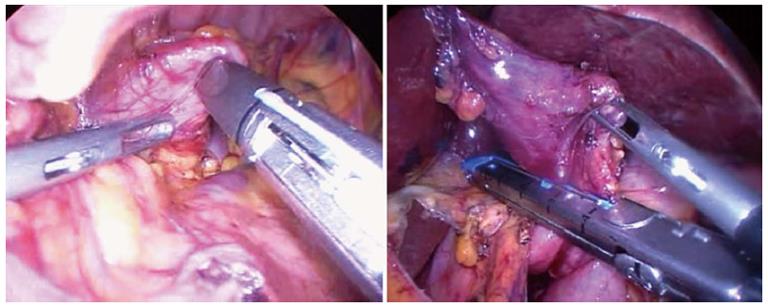
Two 51-year-old and 49-year-old women were referred to our Department for evaluation of symptoms of epigastralgy and upper abdomen tenderness, respectively. They denied weight loss, hematemesis and melena. The patients did not complain of vomiting or any abnormal bowel function. Abdominal examinations revealed no masses or other abnormalities. A barium esophagogastric study was performed, which showed an image of a protruding pouch in the upper gastric region (Figure 1). To confirm the diagnosis, an upper endoscopy was conducted, demonstrating diverticula directed posteriorly off the fundus of the stomach that measured 5 cm and 8 cm in diameter, respectively (Figure 2). The diverticula had a narrow neck but no ulcer was identified. Functional examination with esophageal stationary manometry and 24-h esophagogastric pH-multichannel intraluminal impedance monitoring showed normal values. The electrogastrography monitoring showed an increase in bradyarrhythmic gastric activity in both patients. Patients were presented for surgery and the operations were performed laparoscopically. The interventions were substantially the same for both patients. Because inspection of the stomach did not show a diverticulum at the anterior surface, the bursa omentalis was opened by dividing the gastrocolic omentum. Under endoscopic control, the diverticula were resected at the neck with EndoGIA (Universal, US Surgical Corporation, Norwalk, CO, United States) and then successfully retrieved with a laparoscopic pouch (Figure 3). Then, the staple lines were carefully examined and tested by submerging insufflated stomach under sterile irrigation to observe bubbles and there was no evidence of a leak. Histology confirmed a gastric diverticula of 5 cm and 8 cm, respectively, with normal mucosa in both cases. The procedures were uneventful. Patients were placed on a regular diet on postoperative day 3 and discharged 5 d later. Patients did not show any complications after surgery. On their first 6-mo follow-up visit, neither patient complained of any symptoms, while normal radiographic and endoscopic examinations, and regular values of esophageal manometry and 24-h esophagogastric pH-multichannel intraluminal impedance were found.
Figure 1 A barium study reveals diverticula directed posteriorly off the fundus of the stomach that measured 5 cm and 8 cm in diameter in 51-year-old and 49-year-old women, respectively.
Figure 2 Endoscopic view of gastric diverticulum with a narrow neck.
Figure 3 Exposure of the neck of the diverticulum for preparation of diverticulectomy and resection at the neck with a linear stapler.
DISCUSSION
Moebius in 1661 and later Roax in 1774 first described gastric diverticula[9]. The literature suggests that most symptomatic diverticula are found in patients between 20 and 60 years of age[10-12], while a unique study showed that only 4% of gastric diverticula occurred in patients younger than 20 years[11] and no differences in incidence between sexes have been described[4]. Two types of gastric diverticula are recognized according to Akerlund[13] and Schmidt et al[14]: congenital (true) and acquired (false) diverticula, with congenital types being more common[2,15-17]. True diverticula have all layers of the gastric wall, and it is believed that these congenital diverticula occur as a result of splitting of the longitudinal muscular fibers at the cardia level, leaving only circular muscle fibers in the gastric wall and creating a weakening to allow a diverticulum to form during the fetal period. This hypothesis is supported by Reich[18] who reported fetal gastric diverticula and by Lewis, which described gastrointestinal diverticula in embryos in 1908[19]. False diverticula, also classified as pulsation and traction diverticula, do not carry all layers of the gastric wall[20]. Pulsation diverticula are those arising from increased intraluminal pressure, such as chronic coughing, obesity and pregnancy. Traction diverticula arise from perigastric adhesions from concurrent diseases, such as peptic ulcer disease, pancreatitis, malignancy, gastroesophageal reflux and cholecystitis[11,12]. Gastric traction diverticula have been reported after surgical procedures on the stomach, including Roux-en-Y gastric bypass[12,21,22]. Even if gastric diverticula can arise virtually anywhere along stomach, most congenital diverticula (70%) are typically located on the posterior wall of the stomach just below the gastroesophageal junction[2], while acquired diverticula are usually situated near the gastric antrum. Typical diverticula are 1-3 cm in diameter but large diverticula as demonstrated above can occur[2,15].
Most gastric diverticula are asymptomatic[22], however when symptoms arise, depending on the size of the diverticular neck, they are most commonly upper abdominal pain, nausea, and emesis, and are described in 18%-30% of cases[2,21]. Wide-neck diverticula often go unnoticed perhaps because food and digestive juices are less likely to become trapped. It has been suggested that food retention with subsequent distension of the gastric diverticulum may cause pain[23,24]. Dyspepsia and vomiting are less common[21,25]. Occasionally, patients with gastric diverticula can have dramatic presentations related to massive bleeding or perforation[26] due to food retention with subsequent release of gastric juices within the mucosal sac, causing diverticulitis and possibly ulceration or hemorrhage. There are two reports of invasion with adenocarcinoma[27,28]. The diagnosis may be difficult, as complaints can be caused by more common gastrointestinal pathologies and only be aggravated by diverticula. Methods of detection can fail, therefore, a combined approach should be used[8]. The presence of a mucosal sac can be confirmed with upper gastrointestinal contrast studies and endoscopies. These are the most reliable diagnostic tests but reports in the literature confirm that they can still miss the lesion if it has a narrow neck that precludes entry of the contrast or scope, giving false negative results[2,11,29]. In a large review, Palmer[11] reported that 5% of gastric diverticula are missed during upper gastrointestinal investigation. Other reports recommend the use of upper endoscopy[22,30] for diagnosis, as this modality easily confirms the location and size of the diverticulum and provides the opportunity to biopsy any concurrent pathology. This diagnostic tool can rule out associated pathology and may be able to reproduce symptoms with distention of the diverticulum, indicating which patients would benefit from resection[15,22]. Computerized tomography scans are also used to diagnose diverticula; however, these have also mistaken diverticula for adrenal masses[31].
Appropriate management of a diverticulum depends mainly on the symptoms as well as on the diverticulum size. There is no specific therapeutic strategy for an asymptomatic diverticulum[5,18]. However, routine surveillance with a periodic physical examination is recommended, given the potential onset of complications[20]. Diverticula exceeding 4 cm are more prone to produce complications and tend to respond less favorably to medications. Although some authors support conservative therapy with antacids, this provides only temporary symptom relief and is not able to resolve the underlying pathology[20]. A necessity for successful treatment with complete relief of symptoms is the association of the symptoms with the diverticulum. Palmer[11] found that in 30 of 49 symptomatic patients with a gastric diverticulum, symptoms were attributable to other gastrointestinal diseases, and 6 of 9 patients with symptoms caused by a gastric diverticulum who underwent open surgery showed excellent outcomes. Resection of gastric diverticula in all patients will lead to unsatisfactory results[22]. Surgical resection is the mainstay of treatment when the diverticulum is large, symptomatic or complicated by bleeding, perforation or malignancy, with over two-thirds of patients remaining symptom-free after surgery[11]. Several surgical approaches have been described including invagination of the diverticulum as well as partial gastrectomy[32,33], however, since the first successful laparoscopic resection of a gastric diverticulum in the late 1990s, this approach is now considered safe and feasible[34]. The most favorable approach providing better exposure is by placing a, right upper quadrant port, and 2 left upper quadrant ports. Laparoscopic dissection has been performed by either releasing the gastrocolic ligament, thus allowing exposure of the superior posterior wall of the stomach[5,34-36]. Simple diverticulum resection with a laparoscopic cutting stapler has been reported to be successful[37]. In some cases the surgical approach can be challenging because the diverticulum is often collapsed and hidden in the splenic bed. Sometimes, a resection of the wrong part of the stomach has also been described[22]. For this reason the surgical procedure should be combined with intraoperative endoscopy to find an elusive diverticula by stretching the diverticular sac[4,34-36].
In conclusion, laparoscopic resection is a safe and feasible surgical approach with excellent outcomes and is strongly indicated for symptomatic gastric diverticula.