Published online Jul 28, 2013. doi: 10.3748/wjg.v19.i28.4531
Revised: April 24, 2013
Accepted: May 9, 2013
Published online: July 28, 2013
Processing time: 199 Days and 15.5 Hours
AIM: To perform wire-guided cannulation using a newly designed J-shaped tip guidewire, and to verify feasibility and safety for use.
METHODS: The study was conducted on endoscopic retrograde cholangiopancreatography (ERCP) patients with naïve papilla undergoing diagnosis and treatment of biliary diseases between September 2011 and July 2012. We performed ERCP in a succession of 50 cases with a J-shaped tip guidewire. The first insertion attempt began with a trainee who had 5 min to complete cannulation, followed if necessary by the trainer for another 5 min. We assessed the primary success rate of selective biliary cannulation within 10 min and adverse events such as post-ERCP pancreatitis (PEP), bleeding or perforation.
RESULTS: The primary success rate was 90% (45/50) within 10 min, the initial success rate within 5 min by trainee staff was 76% (38/50). The rate of PEP was 6% (3/50), but all 3 cases were mild pancreatitis. All patients were managed successfully with conservative treatment. There was no bleeding or perforation.
CONCLUSION: A newly designed J-shaped tip guide-wire has the possibility to facilitate selective biliary cannulation for ERCP and appears to be safe.
Core tip: We conducted a feasibility study that performed endoscopic retrograde cholangiopancreatography (ERCP) with a newly designed J-shaped tip guidewire. This new guidewire has a strongly-flexed atraumatic tip with hydrophilic coating; therefore, it may contribute to the improvement of the passage through the intra-duodenal biliary segment and to the decrease of adverse events such as post-ERCP pancreatitis. We assessed the primary success rate of selective biliary cannulation within 10 min and rate of post-ERCP pancreatitis. The primary success rate was 90% (45/50); the rate of post-ERCP pancreatitis was 6% (3/50), but all 3 cases were mild. The J-shaped tip guidewire may facilitate selective biliary cannulation in ERCP.
- Citation: Omuta S, Maetani I, Shigoka H, Gon K, Saito M, Tokuhisa J, Naruki M. Newly designed J-shaped tip guidewire: A preliminary feasibility study in wire-guided cannulation. World J Gastroenterol 2013; 19(28): 4531-4536
- URL: https://www.wjgnet.com/1007-9327/full/v19/i28/4531.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i28.4531
Endoscopic retrograde cholangiopancreatography (ERCP) is used to diagnose and treat biliary disease. Deep cannulation of the common bile duct is required for this procedure, and the current success rate for the relatively difficult conventional contrast-guided cannulation (CGC) technique ranges from 50%-90%[1-5]. Wire-guided cannulation (WGC) is a recently developed alternative to CGC that has been shown to increase primary biliary cannulation rate[6-11], chiefly by reducing incidence of post-ERCP pancreatitis (PEP)[12-20]. However, despite efficiency improvements, the sharp tips of guidewires are sometimes associated with perforation[21-23]. Even without perforation, complications can occur when the guidewire tip hits the fold and flexion of the intra-duodenal biliary segment. While a looped tip guidewire has been developed, its utility in avoiding perforation has not sufficiently been evaluated[24].
Here, we assessed the efficiency of ERCP using a newly designed J-shaped tip guidewire with a strongly flexed atraumatic tip and hydrophilic coating designed to improve passage through intra-duodenal biliary segments and decrease the adverse events, such as PEP, bleeding or perforation.
Fifty patients with naïve papilla undergoing diagnosis and treatment for biliary diseases between September 2011 and July 2012 received ERCP using J-shaped tip guidewires. Patients were excluded if only their pancreatic ducts were diagnosed or treated, if they had previously undergone endoscopic sphincteroplasty, or if they had duodenal stenosis or Billroth II or Roux-en-Y anastomosis, or refused to provide informed consent.
Patients were sedated via intravenous administration of midazolam (5-10 mg) and buprenorphine (0.2 mg). Scopolamine butylbromide (20 mg) or glucagon (1 mg) was injected intravenously to inhibit gastrointestinal peristalsis, and each patient received nafamostat mesilate (20 mg/d) prior to ERCP. Blood samples collected 2 h after ERCP were used to determine complete blood counts and serum amylase levels, and those collected after 18-24 h also measured hepatobiliary enzymes and C-reactive protein. We did not place a pancreatic duct stent for the prevention of pancreatitis in either procedure.
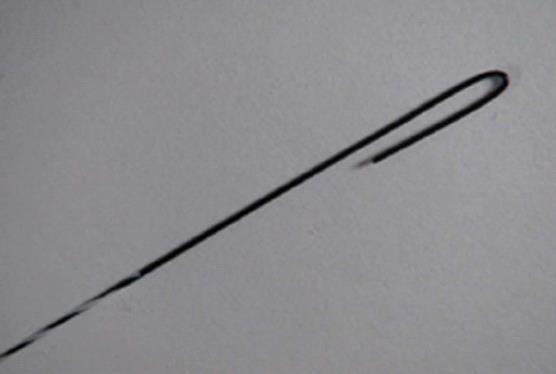
The guidewire (RWHJ-2545A, 0.025-inch; Paiolax Medical Devices, Inc., Kanagawa, Japan) tip was bent to attain a 1-mm radius, and a hydrophilic coating was applied starting 50 mm from the tip. The shaft was covered by a sheath and the jacket coated with water-repellent material (Figure 1).
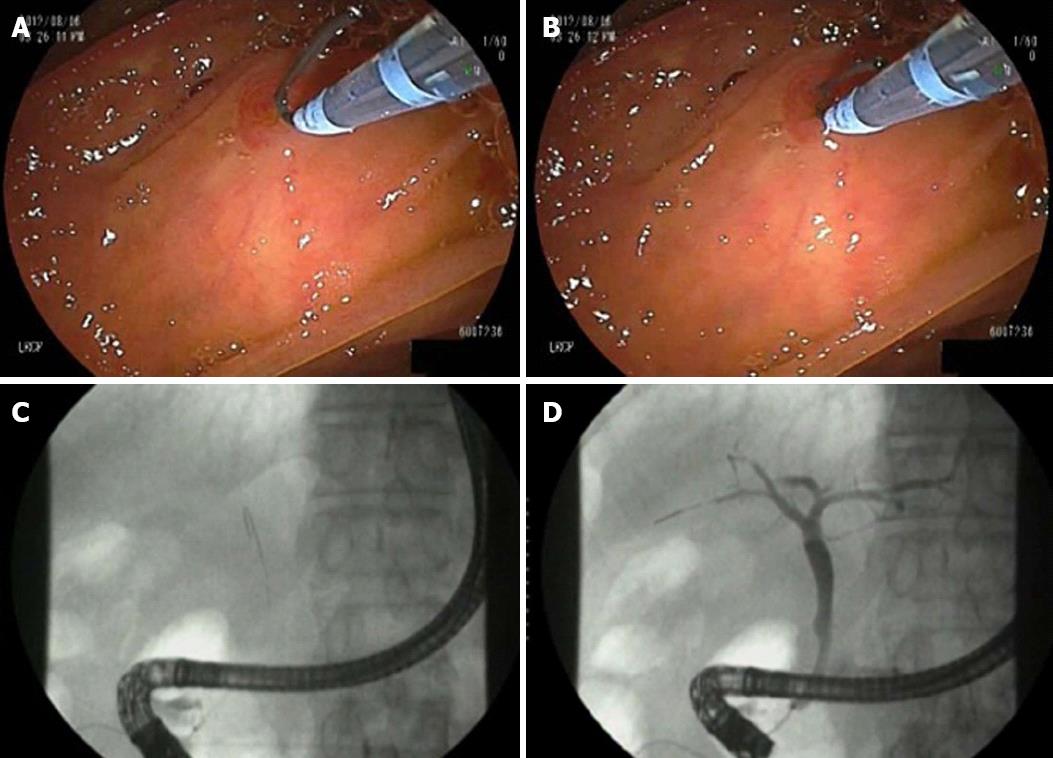
Endoscopy was performed with JF-260V (Olympus, Tokyo, Japan) or ED-530XT8 (Fujinon, Tokyo, Japan) endoscopes, after catheters were preloaded with guidewires. In the present study, in general, a regular catheter was chosen except for the case undergoing sphincterotomy. First, catheters (CleverCut3 V, Olympus, Tokyo, Japan; Tamdem XL, Boston Scientific, Natick, MA, United States) were preloaded with guidewires, the guidewire tip was extended 5 mm from the catheter, bent into a “J” shape, and then the guidewire was pulled back into a stand-by position (Figure 2A). Endoscopists controlled the direction parallel to the axis of bile duct of the catheter by inches. Assisting endoscopists participated in the guidewire manipulation in all cases. An assisting endoscopist moved the guidewire back and forth in small motions by using a tactile feedback (in-and-out movement method). No fluoroscope was used during attempts of insertion, but once the guidewire was inserted without resistance then fluoroscopy was used only after insertion to confirm success (Figure 2B). The catheter was then inserted into the biliary system along the guidewire, and contrast medium was injected (Figure 2C). No test injection was performed before successful cannulation.
The first insertion attempt began with a trainee who had 5 min to complete cannulation, followed if necessary by a trainer with career experience of over 500 ERCPs (Maetani I or Shigoka H or Omuta S) for another 5 min. If both attempts failed, efforts continued with a standard biliary guidewire (Jagwire 0.035 angle type, Boston Scientific) for another 10 min (second attempt) and were repeated as necessary according to the trainers’ recommendations (exchange of endoscopist or guidewire, pancreatic duct guidewire placement method, or pre-cutting sphincterotomy).
Success was defined as completing cannulation with the J-shaped tip guidewire and obtaining a cholangiogram within 10 min. Cannulation time was defined as from when a tip of the guidewire first touched the orifice of the papilla to the obtainment of cholangiogram. PEP was defined as continued abdominal pain ≥ 24 h after ERCP, with more than 3 times the normal (upper limit) serum-amylase level[25]. Pancreatitis severity was classified using the Atlanta International Symposium criteria[26]. Suspected sphincter of Oddi dysfunction was defined according to the revised Milwaukee classification[27]. Sphincter of Oddi manometory was not performed. Hyperamylasemia was defined as 3 times the normal (upper limit) amylase level 18-24 h after ERCP.
The protocol adhered to the Helsinki Declaration and was approved in advance by the Institutional Ethical Review Board. The trial was registered with the University hospital Medical Information Network Clinical Trials Registry (UMIN000007526). All participants gave written informed consent beforehand.
The primary study endpoint was the success rate of cannulation with the J-shaped tip guidewire performed within 10 min. The secondary endpoints were as follows: (1) the rate of the occurrence of PEP; (2) time to selective biliary cannulation; (3) number of attempts for selective biliary cannulation; and (4) number of accidental pancreatic duct insertions. Data are presented as median and interquartile ranges (IQR).
Baseline characteristics and indications are summarized in Table 1, and details of the endoscopic procedure are given in Table 2.
| Item (n = 50) | Value |
| Age, yr [median (IQR)] | 75.3 (68-83) |
| Sex (male) | 24 |
| Periampullary diverticulum, n (%) | 22 (44) |
| Indications | |
| Choledocolithiasis (including suspicion) | 27 |
| Cholangiocarcinoma | 7 |
| Pancreatic cancer | 6 |
| Gallbladder cancer | 4 |
| Other malignant disease | 2 |
| Cholangiocellular carcinoma | 1 |
| Suspected biliary SOD | 1 |
| Mirrizi syndrome | 1 |
| Biliary leak after cholecystectomy | 1 |
| Procedure | n |
| Endoscopic papillary (large) balloon dilation | 24 |
| Endoscopic sphincterotomy | 19 |
| Endoscopic nasobiliary drainage | 20 |
| Endoscopic nasobiliary gallbladder drainage | 2 |
| Placement of biliary stent (plastic or metal) | 18 |
| Intraductal ultrasonography | 7 |
| Aspiration, biopsy | 12 |
| Only cholangiogram | 0 |
The overall success rate of endoscopy was 90% (45/50, Table 3), with cannulation achieved within the first 5 min in 38 patients (76%). Cannulation was achieved on the second attempt in 3 patients. The median time to cannulation for these 48 patients was 42.5 s (IQR: 5-262 s). Of the remaining two patients, one required pancreatic duct guidewire placement and the other a pre-cutting sphincterotomy. The median number of attempts was 2.0 (IQR: 1.0-6.0), and the median number of accidental pancreatic duct insertions was 1.0 (IQR: 0.0-3.0). The median serum-amylase level was 148 IU/L (IQR: 94-331 IU/L), and hyperamylasemia occurred in 4 patients.
| Item (n = 50) | Value |
| Success, n (%) | 45 (90) |
| < 5 min | 38 (76) |
| 5-10 min | 7 (14) |
| Time to selective biliary cannulation1, s | 42.5 (5.0-262.0) |
| No. of attempts1 | 2.0 (1.0-6.0) |
| No. of accidental pancreatic duct insertion1 | 1.0 (0.0-3.0) |
| Amylase level1, IU/L | 148 (94-331) |
| Post-ERCP pancreatitis, n (%) | 3 (6) |
| Mild | 3 |
| Severe | 0 |
| Hyperamylasemia, n (%) | 4 (8) |
Mild PEP occurred in 3 patients (6%); in 2 of these, success was achieved within 5 min after endoscopic papillary large balloon dilation, while the third patient received the pre-cutting sphincterotomy mentioned above. All patients were managed successfully with conservative treatment. There were no other adverse events including bleeding or perforation.
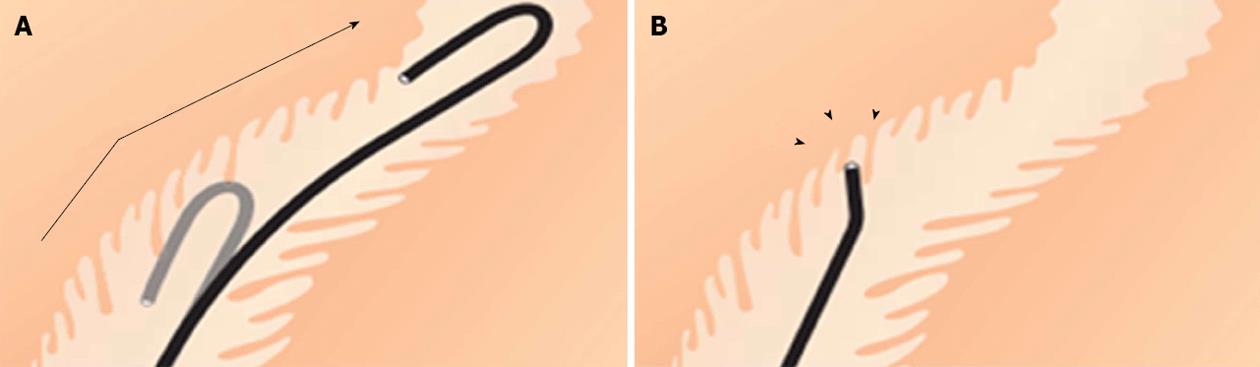
The success rate for selective biliary cannulation using a J-shaped tip guidewire was comparable to that found in previous studies[6-16,28,29], and no guidewire-related adverse events such as bleeding or perforation occurred. Although ours was a preliminary study, the atraumatic and blunt tip of the new guidewire may facilitate selective biliary cannulation (Figure 3A) and reduce instances of perforation and bleeding.
Although straight and angled tips are the most common types used in WGC[1-20,28,29], these sharp tips often stick in the intra-duodenal biliary segment (Figure 3B). While the superiority of the J-shaped tip cannot be definitively shown without controls, the success rate, speed of cannulation, and facility of use appear improved compared to other studies. While similar procedures using standard guidewires resulted in a 77.9% overall success rate (trainees and trainer combined)[28], here we achieved a 76% success rate with trainees, and an overall success rate of 90%. Additionally, the 6% PEP rate is similar to that of other studies[14,18,19,20].
WGC was first introduced by Siegel et al[30]. Meta-analysis has shown that the reduction of pancreatic duct opacification is another possible advantage over CGC[14,18,19]. Further, WGC has been suggested to decrease the risk of PEP[14,18,19], facilitating its spread across the globe as a potential first-line method.
Usually, when guidewires are extended from the tip of a catheter without enough space for advancement, the wire may act like a needle and pierce the epithelium. The J-shape of the guidewire protrudes from the catheter before approaching the biliary orifice, and reduces this likelihood. We therefore believe our J-shaped design to be the aspect that improved insertion into the biliary system. Limitations to this study include small sample size, no controls, a single institution, and involvement of multiple endoscopists. A randomized comparison is warranted for objective evaluation of its performance. One drawback of the J-shaped tip guidewire is the 1-mm radius, which is wider than a standard guidewire and may hamper selective cannulation through a narrow orifice.
In conclusion, a newly designed guidewire with a J-shaped tip may facilitate selective biliary cannulation in ERCP. However, a large prospective randomized control trial is necessary to verify the performance of this guidewire in comparison with standard guidewires.
Selective biliary cannulation is essential for diagnosis and therapeutic endoscopic retrograde retrograde cholangiopancreatography (ERCP) in biliary diseases. Wire-guided cannulation (WGC) increases the primary biliary cannulation rate and decreases the risk of post-ERCP pancreatitis (PEP). Therefore, WGC is now widely performed. However, even experts meet with difficulty and the possible risk of bleeding and perforation due to the guidewire.
The authors performed ERCP using a newly designed J-shaped tip guidewire. A J-shaped tip guidewire with a strongly flexed atraumatic tip and hydrophilic coating was designed to improve passage through intra-duodenal biliary segments and decrease the adverse events, such as PEP, bleeding and perforation. The authors conducted a feasible study.
This is a single center pilot study. The primary success rate was 90% (45/50) within 10 min. The rate of PEP was 6% (3/50), but all 3 cases were mild pancreatitis. All patients were managed successfully with conservative treatment. There was no bleeding or perforation.
A newly designed J-shaped tip guidewire may facilitate selective biliary cannulation and the structure of the tip may contribute to decrease PEP and bleeding, or perforation. However, it is necessary to conduct a large prospective randomized control trial to verify the performance.
This is a single center pilot study of a newly designed J-shaped tip guidewire for wire-guided cannulation. The authors hypothesized that the J-shaped tip prevented perforation or PEP during cannulation. The limitation of this study is a small sample size without a control group as the authors discussed.
P- Reviewers Dormann AJ, Gassler N, Nakai Y S- Editor Zhai HH L- Editor Logan S E- Editor Li JY
| 1. | Kumar S, Sherman S, Hawes RH, Lehman GA. Success and yield of second attempt ERCP. Gastrointest Endosc. 1995;41:445-447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 37] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 2. | Maydeo A, Borkar D. Techniques of selective cannulation and sphincterotomy. Endoscopy. 2003;35:S19-S23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 38] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 3. | Cotton PB. Income and outcome metrics for the objective evaluation of ERCP and alternative methods. Gastrointest Endosc. 2002;56:S283-S290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 43] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 4. | Lehman GA. What are the determinants of success in utilization of ERCP in the setting of pancreatic and biliary diseases? Gastrointest Endosc. 2002;56:S291-S293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Kowalski T, Kanchana T, Pungpapong S. Perceptions of gastroenterology fellows regarding ERCP competency and training. Gastrointest Endosc. 2003;58:345-349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 57] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 6. | Schwacha H, Allgaier HP, Deibert P, Olschewski M, Allgaier U, Blum HE. A sphincterotome-based technique for selective transpapillary common bile duct cannulation. Gastrointest Endosc. 2000;52:387-391. [PubMed] |
| 7. | Artifon EL, Sakai P, Cunha JE, Halwan B, Ishioka S, Kumar A. Guidewire cannulation reduces risk of post-ERCP pancreatitis and facilitates bile duct cannulation. Am J Gastroenterol. 2007;102:2147-2153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 125] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 8. | Bailey AA, Bourke MJ, Williams SJ, Walsh PR, Murray MA, Lee EY, Kwan V, Lynch PM. A prospective randomized trial of cannulation technique in ERCP: effects on technical success and post-ERCP pancreatitis. Endoscopy. 2008;40:296-301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 164] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 9. | Katsinelos P, Paroutoglou G, Kountouras J, Chatzimavroudis G, Zavos C, Pilpilidis I, Tzelas G, Tzovaras G. A comparative study of standard ERCP catheter and hydrophilic guide wire in the selective cannulation of the common bile duct. Endoscopy. 2008;40:302-307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 72] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 10. | Bourke MJ, Costamagna G, Freeman ML. Biliary cannulation during endoscopic retrograde cholangiopancreatography: core technique and recent innovations. Endoscopy. 2009;41:612-617. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 34] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 11. | Halttunen J, Kylänpää L. A prospective randomized study of thin versus regular-sized guide wire in wire-guided cannulation. Surg Endosc. 2013;27:1662-1667. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 23] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 12. | Lella F, Bagnolo F, Colombo E, Bonassi U. A simple way of avoiding post-ERCP pancreatitis. Gastrointest Endosc. 2004;59:830-834. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 129] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 13. | Lee TH, Park do H, Park JY, Kim EO, Lee YS, Park JH, Lee SH, Chung IK, Kim HS, Park SH. Can wire-guided cannulation prevent post-ERCP pancreatitis? A prospective randomized trial. Gastrointest Endosc. 2009;69:444-449. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 105] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 14. | Cennamo V, Fuccio L, Zagari RM, Eusebi LH, Ceroni L, Laterza L, Fabbri C, Bazzoli F. Can a wire-guided cannulation technique increase bile duct cannulation rate and prevent post-ERCP pancreatitis?: A meta-analysis of randomized controlled trials. Am J Gastroenterol. 2009;104:2343-2350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 109] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 15. | Hisa T, Matsumoto R, Takamatsu M, Furutake M. Impact of changing our cannulation method on the incidence of post-endoscopic retrograde cholangiopancreatography pancreatitis after pancreatic guidewire placement. World J Gastroenterol. 2011;17:5289-5294. [PubMed] |
| 16. | Karamanolis G, Katsikani A, Viazis N, Stefanidis G, Manolakopoulos S, Sgouros S, Papadopoulou E, Mantides A. A prospective cross-over study using a sphincterotome and a guidewire to increase the success rate of common bile duct cannulation. World J Gastroenterol. 2005;11:1649-1652. [PubMed] |
| 17. | Freeman ML, Guda NM. ERCP cannulation: a review of reported techniques. Gastrointest Endosc. 2005;61:112-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 215] [Cited by in RCA: 224] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 18. | Cheung J, Tsoi KK, Quan WL, Lau JY, Sung JJ. Guidewire versus conventional contrast cannulation of the common bile duct for the prevention of post-ERCP pancreatitis: a systematic review and meta-analysis. Gastrointest Endosc. 2009;70:1211-1219. [PubMed] |
| 19. | Eachus P. Multidimensional health locus of control in nurses. J Adv Nurs. 1991;16:165-171. [PubMed] |
| 20. | Cotton PB, Garrow DA, Gallagher J, Romagnuolo J. Risk factors for complications after ERCP: a multivariate analysis of 11,497 procedures over 12 years. Gastrointest Endosc. 2009;70:80-88. [PubMed] |
| 21. | Stapfer M, Selby RR, Stain SC, Katkhouda N, Parekh D, Jabbour N, Garry D. Management of duodenal perforation after endoscopic retrograde cholangiopancreatography and sphincterotomy. Ann Surg. 2000;232:191-198. [PubMed] |
| 22. | Fatima J, Baron TH, Topazian MD, Houghton SG, Iqbal CW, Ott BJ, Farley DR, Farnell MB, Sarr MG. Pancreaticobiliary and duodenal perforations after periampullary endoscopic procedures: diagnosis and management. Arch Surg. 2007;142:448-454; discussion 454-455. [PubMed] |
| 23. | Machado NO. Management of duodenal perforation post-endoscopic retrograde cholangiopancreatography. When and whom to operate and what factors determine the outcome? A review article. JOP. 2012;13:18-25. [PubMed] |
| 24. | Ayala JC, Labbe R, Vera E, Moran M. The loop tip wire guide: A new device to facilitate better access through the papilla. Gastrointest Endosc. 2007;65:AB236. [DOI] [Full Text] |
| 25. | Cotton PB, Lehman G, Vennes J, Geenen JE, Russell RC, Meyers WC, Liguory C, Nickl N. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991;37:383-393. [PubMed] |
| 26. | Bradley EL. A clinically based classification system for acute pancreatitis. Summary of the International Symposium on Acute Pancreatitis, Atlanta, Ga, September 11 through 13, 1992. Arch Surg. 1993;128:586-590. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 27. | Geenen JE, Hogan WJ, Dodds WJ, Toouli J, Venu RP. The efficacy of endoscopic sphincterotomy after cholecystectomy in patients with sphincter-of-Oddi dysfunction. N Engl J Med. 1989;320:82-87. [PubMed] [DOI] [Full Text] |
| 28. | Nambu T, Ukita T, Shigoka H, Omuta S, Maetani I. Wire-guided selective cannulation of the bile duct with a sphincterotome: a prospective randomized comparative study with the standard method. Scand J Gastroenterol. 2011;46:109-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 42] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 29. | Nakai Y, Isayama H, Tsujino T, Sasahira N, Hirano K, Kogure H, Sasaki T, Kawakubo K, Yagioka H, Yashima Y. Impact of introduction of wire-guided cannulation in therapeutic biliary endoscopic retrograde cholangiopancreatography. J Gastroenterol Hepatol. 2011;26:1552-1558. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 30. | Siegel JH, Pullano W. Two new methods for selective bile duct cannulation and sphincterotomy. Gastrointest Endosc. 1987;33:438-440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 32] [Article Influence: 0.8] [Reference Citation Analysis (0)] |