Published online Jul 28, 2013. doi: 10.3748/wjg.v19.i28.4526
Revised: March 19, 2013
Accepted: April 28, 2013
Published online: July 28, 2013
Processing time: 160 Days and 13.6 Hours
AIM: To determine the factors affecting the decision to perform surgery, and the efficiency of ultrasonography (USG) in detecting gallbladder polyps (GP).
METHODS: Data for 138 patients who underwent cholecystectomy between 1996 and 2012 in our clinic with a diagnosis of GP were retrospectively analyzed. Demographic data, clinical presentation, principal symptoms, ultrasonographic and histopathological findings were evaluated. Patients were evaluated in individual groups according to the age of the patients (older or younger than 50 years old) and polyp size (bigger or smaller than 10 mm) and characteristics of the polyps (pseudopolyp or real polyps). χ2 tests were used for the statistical evaluation of the data.
RESULTS: The median age was 50 (26-85) years and 91 of patients were female. Of 138 patients who underwent cholecystectomy with GP diagnosis, only 99 had a histopathologically defined polyp; 77 of them had pseudopolyps and 22 had true polyps. Twenty-one patients had adenocarcinoma. Of these 21 patients, 11 were male, their median age was 61 (40-85) years and all malignant polyps had diameters > 10 mm (P < 0.0001). Of 138 patients in whom surgery were performed, 112 had ultrasonographic polyps with diameters < 10 mm. Of the other 26 patients who also had polyps with diameters > 10 mm, 22 had true polyps. The sensitivity of USG was 84.6% for polyps with diameters > 10 mm (P < 0.0001); however it was only 66% in polyps with diameters < 10 mm.
CONCLUSION: The risk of malignancy was high in the patients over 50 years old who had single polyps with diameters > 10 mm.
Core tip: Early stage gallbladder cancers can often be detected as polyps in imaging studies. The aim of this study was to determine the factors affecting surgery by analyzing the incidence of malignancy of gallbladder polyps (GP) and the efficiency of ultrasonography in detecting GP. Of 138 patients with GP on imaging, 99 had polyps and 21 had histopathologically confirmed adenocarcınoma. Of these 21 patients, all malignant polyps were solitary and had a diameter > 10 mm. In our study, the risk of malignancy correlated wıth age over 50 years old, solitary polyp and polyp diameter > 10 mm.
- Citation: Sarkut P, Kilicturgay S, Ozer A, Ozturk E, Yilmazlar T. Gallbladder polyps: Factors affecting surgical decision. World J Gastroenterol 2013; 19(28): 4526-4530
- URL: https://www.wjgnet.com/1007-9327/full/v19/i28/4526.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i28.4526
Gallbladder polyps (GP) present as masses protruding from the gallbladder mucosa. They are found in 0.3% to 12% of healthy individuals[1]. The actual prevalence is unknown; however, at present, GPs are diagnosed more frequently because of the widespread use of abdominal imaging techniques. GPs are usually asymptomatic and are diagnosed incidentally during radiological examinations done for other reasons. GPs are classified as pseudopolyps or true polyps. Pseudopolyps consist of cholesterol polyps/cholesterolosis, adenomatous polyps, adenomyoma, inflammatory polyps and hyperplastic polyps; these are all benign lesions. True polyps are grouped into benign (adenoma), premalignant (dysplastic polyps) and malignant (adenocarcinoma)[2]. Cholesterol polyps are the most frequently observed GPs. Therefore, most GPs are benign lesions. Occasionally, early stage gallbladder cancers can be detected as a polyp in imaging studies.The prevalence of malignant polyps of GPs can reach 27%[3]. In patients older than 50 years old, the presence of polyps larger than 10 mm has been reported as a risk factor for malignancy[3-8]. The most commonly used imaging modality for diagnosis is ultrasonography (USG). However, USG is poor at differentiating benign and malignant polyps. Additional diagnostic tools comprise computed tomography and endoscopic USG.
In this study, patients in our clinic diagnosed withGPs who had surgery were examined; and indication for surgery, frequency of polyp types, malignancy rates of polyps and reliability of USG in identification and differentiation of polyps were investigated.
Age, sex, clinical signs and symptoms, preoperative ultrasound and histopathological diagnoses of patients were analyzed retrospectively in patients admitted to our clinic with GP and underwent cholecystectomy from 1996-2012. All the patients were evaluated with USG before surgery in the Radiology Department of Uludag University Faculty of Medicine. Hyperechoic lesions that had no acoustic shadowing and didnot move with position change represented a confirmed diagnosis of GP[8].Detection of polyps > 10 mm, suspicious findings in USG (such as a vascularization pattern, Figure 1), growth during follow-up, and personal request of the patient were indications for surgery.
Polyp size, number and presence of stones were evaluated in preoperative USG reports, and compatibility of these findings with histopathological data was analyzed.
According to histopathological diagnoses, cholesterol polyps/cholesterolosis, hyperplastic and adenomatous polyps were assembled under the title of “pseudopolyp”; adenoma and adenocarcinoma were assembled under the title of “real polyps”. In addition, patients were evaluated in individual groups according to the age of the patients (older or younger than 50 years old) and polyp size (bigger or smaller than 10 mm).
The χ2 test was used, when appropriate, to calculate the statistical significance of the different demographic and clinical variables. P values of < 0.05 were deemed significant.
Cholecystectomy was performed in 5832 patients between 1996-2012 and surgical indication of 138 patients (2.3%) was GPs. Ninety-one of the patients were female and 47 of them were male, with a median age of 55 (26-85) years. Polyps were detected in 99 of the 138 patients (71.7%) undergoing surgery for GPs; gallbladder stones were detected in the remaining 39. Thus, the false positive rate was 28% in ultrasound evaluation of polyps. Remarkably, the polyps in all of these cases were < 10 mm.
Sixty-six patients (66.6%) did not have any symptoms at the time of presentation; however, 33 patients with polyps were symptomatic. Sixty-two of 66 asymptomatic patients elected to have surgical treatment because of possible future risks. Three of four asymptomatic patients had a cholecystectomy because their polyp increased to > 10 mm in 6 mo; the remaining patient had a cholecystectomy because of their age and sex (65 years old male). On pathological examination, the polyps of these four patients were detected as cholesterol polyps and adenomatous polyps. The 33 symptomatic patients presented with complaints of right upper quadrant pain and dyspepsia, and had surgery upon detection of polyps in USG (Table 1). Gallstones were accompanied with polyps in 18 (54.5%) of these symptomatic patients. Only in two of the malignant cases was a polypoid structure accompanied by gallstones.
| Characteristics | Pseudopolyp | True polyp (n = 22) | P value1 | ||
| Pathology result | (n = 77) | Adenocarcinoma | Adenoma | ||
| Sex | Woman | 51 | 10 | 1 | 0.33 |
| Man | 26 | 11 | 0 | ||
| Age (yr) | < 50 | 52 | 1 | 1 | < 0.0001 |
| ≥ 50 | 25 | 20 | 0 | ||
| Symptoms | Yes | 24 | 9 | 0 | 0.62 |
| No | 53 | 12 | 1 | ||
| Number | Multiple | 23 | 0 | 0 | 0.01 |
| Single | 54 | 21 | 1 | ||
| Size (mm) | ≤ 10 | 73 | 0 | 1 | < 0.0001 |
| > 10 | 4 | 21 | 0 | ||
As shown in Table 1, 54.5% of patients were under the age of 50 and 90% of true polyps were seen in patients over 50 years old. In addition, the incidence of polyps was 3.7% under 50 years of age, rising to 44% in patients over 50 years of age (P < 0.0001).
While gallstones were detected only in 1 of 26 patients who had lesions of 10 mm diameter in preoperative USG, postoperative diagnoses was true gallbladder polyp in 21 (84.6%) of the remaining 25 patients. The other four patients were reported to have pseudopolyps. Pre-operative USG diagnosed 96% of lesions over 10 mm accurately and 84% of them were found to be true polyps (adenoma/adenocarcinoma). Histopathological diagnoses reported polyps only in 74 of 112 patients who had lesions < 10 mm. Thus, the accuracy of USG for polyps < 10 mm decreased to 66% and only one of these 74 cases was a true polyp (adenoma). There was a statistically significant difference in the diagnosis of true polyps between polyps < 10 mm or > 10 mm (P < 0.0001).
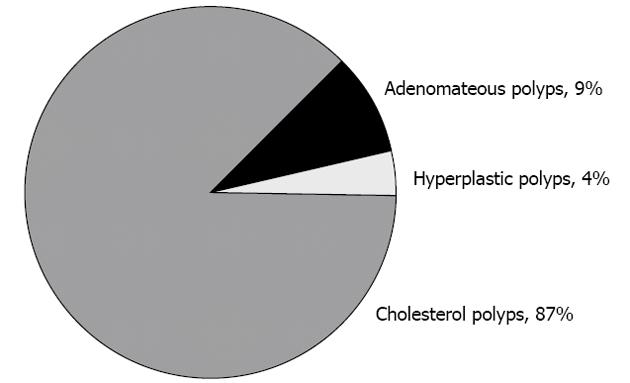
The mean polyp diameter of the polyps from 99 patients (histopathologically defined as 77 pseudopolyps and 22 true polyps) was 8.8 mm (range 3-19 mm). The most commonly seen GP was a cholesterol polyp (Figure 2). Twenty-one of 22 patients with true polyps were diagnosed with adenocarcinoma, and the other one was adenoma. All the malignant polyps were > 10 mm and solitary. Eleven patients with malignancy were male and the median age was 61 (40-85) years. In our series, the incidence of malignant GP was 21.2% (21 of 99 cases). The incidence dropped to 15.2% when all 138 patients with preoperative diagnoses of polyps were taken into consideration.
Cholecystectomy only was performed in 16 of 21 patients with malignancy, and cholecystectomy with liver S-5 resection and lymph node dissection was performed in the remaining five patients. No additional treatment other than cholecystectomy was performed in 10 patients with T1 tumors limited to the mucosa and submucosa.The other 7 patients did not accept additional treatment. Eight patients received chemotherapy treatment after surgery. Ten of these patients were still alive and 11 of them died. Survival was 14.8 mo (range 4-38 mo).
GPs are common gallbladder lesions and should not be ignored because of their association with malignancy. In the literature, the incidence of GP has been reported as between 0.3% and 12.0%[9,10]. In our clinical series of 5832 patients undergoing cholecystectomy, GPs were an indication for cholecystectomy in 2.3% (138 patients) of cases. Thirty-nine of these patients were diagnosed with only cholelithiasis; therefore, the true incidence of GPs was 1.7%.
There are different concepts about the effect of demographic factors such as age and gender on the incidence of GPs. Some studies reported that GPs are more frequently seen in males[2,11-14] or females[9-15], and some studies even suggest that there is no effect of gender on GPs[14-21]. Approximately 2/3 of cases in our study werewomen and the true polyp ratio was 29.7% in men and 17.7% in women (Table 1). Ito et al[17] reported that the mean age was 59 years in their 417 patients series. Although 53% of patients in our study were under the age of 50, 90% of true polyps were detected in patients over 50 years old. As demonstrated in Table 1, the incidence of true polyps was 3.8% under the age of 50 years and 44% over the age of 50 years (P < 0.05).
Ultrasonography is the most frequently used and most valuable diagnostic tool for preoperative evaluation of gallbladder pathologies[8]. One hundred thirty eight patients in our series were diagnosed with GP using USG. Considering that 39% of them were also diagnosed with cholelithiasis, the accurate diagnosis rate of USG was 71.7%. The sensitivity of USG for GPs has beenreported to be between 32% and 90%[5,18]. While USG can usually detect polyps > 5 mm, it becomes more accurate if the polyp is > 10 mm[19]. Indeed, USG detected almost all polyps > 10 mm accurately (25 of 26 cases) and these polyps were true polyps (adenoma/adenocarcinoma).However, the accuracy of USG diagnosis lesions < 10 mm was 66%. In addition, GPs were detected as < 10 mm in 39 patients who were thought to have GPs preoperatively but in whom no polyps were detected postoperatively. Postoperatively, the pathological diagnoses of these 39 patients were chronic cholecystitis and cholelithiasis. Cholesterolosis occurs as a result of accumulation of esterified cholesterol and triglycerides in macrophages of the lamina propria, and they are often mistaken as small polyps in USG[17]. Gallbladder stones attached to the wall of the gallbladder can easily be interpreted as a polyp in USG[18]. The presence of stones in the gallbladder reduces the success rate of USG in the diagnosis of GPs; USG diagnosis of GPs is to 99% accurate in the absence of any stones. On the other hand, in our patients, GPs did not usually cause any symptoms. Association of stones with GPs may cause symptoms and prompts the patient to consult a doctor, making the diagnosis easier. In our study, gallstones accompanied GPs in only 18.1% (18 patients) of patients. All patients with stones were symptomatic. However, there were no stones in 15 of the 33 symptomatic patients and GPs caused the symptoms in these patients. In our series of patients, being symptomatic did not have any impact on detection of true polyps (P = 0.71).
Another important factor associated with malignancy in GPs is the diameter of the polyps[6,20]. Kozuka et al[21] reported that the critical limit for differentiation of benign and malignant GPs was 12 mm and suggested cholecystectomy for GPs larger than 12 mm. Kubota et al[22] compared postoperative pathological data of 72 patients with GPs and preoperative ultrasound. They reported 22% of neoplastic polyps of the gallbladder as > 10 mm. They also reported that evaluation of the polyp shape may be beneficial, but it is not enough to distinguish cholesterol polyps from adenoma and cancer. Sugiyama et al[23] tried to make a distinction between benign and malignant polyps using preoperative USG and endoscopic USG. They detected adenoma or cancer in 14% of polyps with diameters of 6-10 mm in preoperative USG. Zielinski et al[2] emphasized that there is a significant increase in the risk of neoplasia in polypoid lesions > 6 mm; they suggest performing cholecystectomy in these patients. In our study, the majority of polyps (73 of 74 cases) < 10 mm were pseudopolyps, and the remaining polyps were adenomas. None of the malignant polypswere < 10 mm. Eight-four percent of polyps > 10 mm were true polyps (adenoma/adenocarcinoma) and all of the these true polyps were found to be adenocarcinoma.This suggests that a limit of 10 mm is very important (P = 0.0001). Similarly, no true polyps were detected in the setting of multiple polyps. Remarkably, 28% of single polyps were diagnosed as adenocarcinoma.
The literature suggests that patients over 50 years old, polyps > 10 mm, polyps with a broad base or long pedicle, polyps associated with cholecystitis or cholelithiasis, or irregular thickening of the gallbladder in the setting of biliary colic are indications for cholecystectomy[4,23,24]. In our study, 21 (21.2%) of 99 patients with GPs were diagnosed with malignancy, all of whom were older than 50 years with single polyps > 10 mm. In addition, the success rate of USG for diagnosing GPs > 10 mm was more evident and an important point. Patients had surgery mostly because of their extreme sensitivity and anxiety.We found that surgery was not beneficial in patients with multiple polypoid lesions or polyps < 10 mm. For this reason, the surgical team should reassure and relax the patients and avoid unnecessary cholecystectomies.
In conclusion, being male and over 50 years old with a solitary polyp > 10 mm benefited most from cholecystectomy.
Gallbladder polyps (GP) are frequently detected incidentally. They are usually misdiagnosed as gallstones in sonographic examinations. There is no consensus for treatment and follow-up of GP because of its particularly rare incidence of malignancy. There are some risk factors associated with high risk of malignancy. Early diagnosis and surgical treatment of GP affects survival of gallbladder carcinomas.
Many studies have investigated risk factors that increase the incidence of malignancy of GP. Age, gender, polyp size, polyp number, accompanying gallstones and the inflammatory status of the gallbladder are significant risk factors.
In this study, all the malignant polyps were solitary and over 10 mm in size. Malignant polypsweredetermined in 44% of the patients aged over 50. The authors failed to show an association between gender and malignancy for GP. Ultrasonography (US) was more sensitive for polyps over 10 mm. US was more helpful in showing malignancy for cases with polyps under 10 mm.
This study will facilitate surgeons’ decision making for treatment and follow-up of patients with GP.
Histopathologically, cholesterol polyps/colestherolosis, hyperplastic and adenomateous polyps are defined as pseudopolyps, while adenomas and adenocarcinomas are defined as true polyps.
This manuscript, which was written on a subject of considerable controversy in general surgery, has been generally well designed.
P- Reviewers Nikolaos GS, Sari YS, Vettoretto N S- Editor Wen LL L- Editor Stewart GJ E- Editor Li JY
| 1. | Cha BH, Hwang JH, Lee SH, Kim JE, Cho JY, Kim H, Kim SY. Pre-operative factors that can predict neoplastic polypoid lesions of the gallbladder. World J Gastroenterol. 2011;17:2216-2222. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 57] [Cited by in RCA: 70] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 2. | Zielinski MD, Atwell TD, Davis PW, Kendrick ML, Que FG. Comparison of surgically resected polypoid lesions of the gallbladder to their pre-operative ultrasound characteristics. J Gastrointest Surg. 2009;13:19-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 76] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 3. | Lee KF, Wong J, Li JC, Lai PB. Polypoid lesions of the gallbladder. Am J Surg. 2004;188:186-190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 142] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 4. | Terzi C, Sökmen S, Seçkin S, Albayrak L, Uğurlu M. Polypoid lesions of the gallbladder: report of 100 cases with special reference to operative indications. Surgery. 2000;127:622-627. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 159] [Cited by in RCA: 128] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 5. | Yang HL, Sun YG, Wang Z. Polypoid lesions of the gallbladder: diagnosis and indications for surgery. Br J Surg. 1992;79:227-229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 180] [Cited by in RCA: 146] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 6. | Koga A, Watanabe K, Fukuyama T, Takiguchi S, Nakayama F. Diagnosis and operative indications for polypoid lesions of the gallbladder. Arch Surg. 1988;123:26-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 118] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 7. | Shinkai H, Kimura W, Muto T. Surgical indications for small polypoid lesions of the gallbladder. Am J Surg. 1998;175:114-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 59] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 8. | Yang HL, Kong L, Hou LL, Shen HF, Wang Y, Gu XG, Qin JM, Yin PH, Li Q. Analysis of risk factors for polypoid lesions of gallbladder among health examinees. World J Gastroenterol. 2012;18:3015-3019. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 23] [Cited by in RCA: 34] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 9. | Jørgensen T, Jensen KH. Polyps in the gallbladder. A prevalence study. Scand J Gastroenterol. 1990;25:281-286. [PubMed] |
| 10. | Lin WR, Lin DY, Tai DI, Hsieh SY, Lin CY, Sheen IS, Chiu CT. Prevalence of and risk factors for gallbladder polyps detected by ultrasonography among healthy Chinese: analysis of 34 669 cases. J Gastroenterol Hepatol. 2008;23:965-969. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 80] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 11. | Chen CY, Lu CL, Chang FY, Lee SD. Risk factors for gallbladder polyps in the Chinese population. Am J Gastroenterol. 1997;92:2066-2068. [PubMed] |
| 12. | Segawa K, Arisawa T, Niwa Y, Suzuki T, Tsukamoto Y, Goto H, Hamajima E, Shimodaira M, Ohmiya N. Prevalence of gallbladder polyps among apparently healthy Japanese: ultrasonographic study. Am J Gastroenterol. 1992;87:630-633. [PubMed] |
| 13. | Heyder N, Günter E, Giedl J, Obenauf A, Hahn EG. Polypoid lesions of the gallbladder. Dtsch Med Wochenschr. 1990;115:243-247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 12] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Collett JA, Allan RB, Chisholm RJ, Wilson IR, Burt MJ, Chapman BA. Gallbladder polyps: prospective study. J Ultrasound Med. 1998;17:207-211. [PubMed] |
| 15. | Farinon AM, Pacella A, Cetta F, Sianesi M. “Adenomatous polyps of the gallbladder” adenomas of the gallbladder. HPB Surg. 1991;3:251-258. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 18] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 16. | Moriguchi H, Tazawa J, Hayashi Y, Takenawa H, Nakayama E, Marumo F, Sato C. Natural history of polypoid lesions in the gall bladder. Gut. 1996;39:860-862. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 51] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 17. | Ito H, Hann LE, D’Angelica M, Allen P, Fong Y, Dematteo RP, Klimstra DS, Blumgart LH, Jarnagin WR. Polypoid lesions of the gallbladder: diagnosis and followup. J Am Coll Surg. 2009;208:570-575. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 79] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 18. | Berk RN, van der Vegt JH, Lichtenstein JE. The hyperplastic cholecystoses: cholesterolosis and adenomyomatosis. Radiology. 1983;146:593-601. [PubMed] |
| 19. | Mainprize KS, Gould SW, Gilbert JM. Surgical management of polypoid lesions of the gallbladder. Br J Surg. 2000;87:414-417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 83] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 20. | Shoup M, Fong Y. Surgical indications and extent of resection in gallbladder cancer. Surg Oncol Clin N Am. 2002;11:985-994. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 38] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 21. | Kozuka S, Tsubone N, Yasui A, Hachisuka K. Relation of adenoma to carcinoma in the gallbladder. Cancer. 1982;50:2226-2234. [PubMed] |
| 22. | Kubota K, Bandai Y, Noie T, Ishizaki Y, Teruya M, Makuuchi M. How should polypoid lesions of the gallbladder be treated in the era of laparoscopic cholecystectomy? Surgery. 1995;117:481-487. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 126] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 23. | Sugiyama M, Atomi Y, Kuroda A, Muto T, Wada N. Large cholesterol polyps of the gallbladder: diagnosis by means of US and endoscopic US. Radiology. 1995;196:493-497. [PubMed] |
| 24. | Gouma DJ. When are gallbladder polyps malignant? HPB Surg. 2000;11:428-430. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |