Published online Jun 28, 2013. doi: 10.3748/wjg.v19.i24.3810
Revised: March 31, 2013
Accepted: April 9, 2013
Published online: June 28, 2013
Processing time: 176 Days and 5.9 Hours
AIM: To investigate the quality of life following laparoscopic Nissen fundoplication by assessing short-term and long-term outcomes.
METHODS: From 1992 to 2005, 249 patients underwent laparoscopic Nissen fundoplication. Short-term outcome data including symptom response, side effects of surgery, endoscopy, and patient’s perception of overall success were collected prospectively. Long-term outcomes were investigated retrospectively in patients with a median follow-up of 10 years by assessment of reflux symptoms, side effects of surgery, durability of antireflux surgery, need for additional treatment, patient’s perception of success, and quality of life. Antireflux surgery was considered a failure based on the following criteria: moderate to severe heartburn or regurgitation; moderate to severe dysphagia reported in combination with heartburn or regurgitation; regular proton pump inhibitor medication use; endoscopic evidence of erosive esophagitis Savary-Miller grade 1-4; pathological 24-h pH monitoring; or necessity to undergo an additional surgery. The main outcome measures were short- and long-term cure rates and quality of life, with patient satisfaction as a secondary outcome measure.
RESULTS: Conversion from laparoscopy to open surgery was necessary in 2.4% of patients. Mortality was zero and the 30-d morbidity was 7.6% (95%CI: 4.7%-11.7%). The median postoperative hospital stay was 2 d [interquartile range (IQR) 2-3 d]. Two hundred and forty-seven patients were interviewed for short-term analysis following endoscopy. Gastroesophageal reflux disease was cured in 98.4% (95%CI: 95.9%-99.6%) of patients three months after surgery. New-onset dysphagia was encountered postoperatively in 13 patients (6.7%); 95% reported that the outcome was better after antireflux surgery than with preoperative medical treatment. One hundred and thirty-nine patients with a median follow-up of 10.2 years (IQR 7.2-11.6 years) were available for a long-term evaluation. Cumulative long-term cure rates were 87.7% (81.0%-92.2%) at 5 years and 72.9% (64.0%-79.9%) at 10 years. Gastrointestinal symptom rating scores and RAND-36 quality of life scores of patients with treatment success were similar to those of the general population but significantly lower in those with failed antireflux surgery. Of the patients available for long-term follow-up, 83% rated their operation a success.
CONCLUSION: For the long-term, our results indicate decreasing effectiveness of laparoscopic antireflux surgery, although most of the patients seem to have an overall quality of life similar to that of the general population.
Core tip: Current evidence suggests that laparoscopic fundoplication is more effective than medical therapy for the short- and medium-term treatment of gastroesophageal reflux disease. This study examined short-term and long-term outcomes after laparoscopic Nissen fundoplication. Short-term outcomes were assessed by symptom response, side effects of surgery, endoscopy and the patient’s perception of overall success. Long-term outcomes were examined by addressing multiple domains affected by the operation including reflux symptoms, side effects of surgery, durability of antireflux surgery, selective objective testing, need for additional medical or surgical treatment, the patient’s perception of overall success, and long-term quality of life.
- Citation: Kellokumpu I, Voutilainen M, Haglund C, Färkkilä M, Roberts PJ, Kautiainen H. Quality of life following laparoscopic Nissen fundoplication: Assessing short-term and long-term outcomes. World J Gastroenterol 2013; 19(24): 3810-3818
- URL: https://www.wjgnet.com/1007-9327/full/v19/i24/3810.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i24.3810
Medical treatment with proton pump inhibitors (PPIs) heals esophagitis and suppresses heartburn in over 90% of patients[1-3]. Despite the fact that effective maintenance therapies do exist, patients often require lifelong medication, and compliance with long-term maintenance therapy is sometimes difficult to achieve[1-3]. Furthermore, concerns exist regarding long-term safety of PPI medication[4]. Current evidence suggests that laparoscopic fundoplication is more effective than medical therapy for the short- and medium-term treatment of gastroesophageal reflux disease[5-10]. In contrast to medical therapy that inhibits only acid reflux, antireflux surgery is designed to prevent reflux of all gastric content. This is achieved by creating a mechanical antireflux valve that increases lower esophageal sphincter pressure and markedly reduces the rate of spontaneous transient relaxations accompanied by reflux[11,12]. Side effects of Nissen fundoplication such as dysphagia, increased bloating and flatulence, and inability to belch or vomit may limit the success of antireflux surgery[12,13]. Patients may also need revision surgery to improve symptom control, or revert to the use of long-term medical therapy following recurrent symptoms.
Optimal management of chronic gastroesophageal reflux disease is uncertain as treatment options include either modern medical therapy using proton pump inhibitors or antireflux surgery[5]. In addition, long-term quality of life studies are limited. This study examined short-term and long-term outcomes after laparoscopic Nissen fundoplication. Short-term outcomes were assessed by symptom response, side effects of surgery, endoscopy and the patient’s perception of overall success. Long-term outcomes were examined by addressing multiple domains affected by the operation including reflux symptoms, side effects of surgery, durability of antireflux surgery, selective objective testing, need for additional medical or surgical treatment, the patient’s perception of overall success, and long-term quality of life.
From 1992 to 2005, a total of 249 patients underwent laparoscopic Nissen fundoplication for gastroesophageal reflux disease at the fourth Department of Surgery, Helsinki University Central Hospital (120 operations done by three surgeons: Kellokumpu I, Haglund C and Roberts PJ from 1992 to 1997) and at the Central Hospital of Central Finland (129 operations done by Kellokumpu I from 1998 to 2005). Indications for antireflux surgery were residual symptoms while on medical therapy or endoscopic esophagitis after at least three months of intensive acid suppression therapy, or both; dependence on continuous medication and expenses; and pathological 24-h esophageal pH monitoring in symptomatic patients without preoperative endoscopic signs of erosive esophagitis. Diagnosis of gastroesophageal reflux disease was based on upper gastrointestinal endoscopy on 24-h ambulatory pH measurement according to standard criteria as established by Johnson et al[14], and on esophageal manometry to evaluate the lower esophageal resting pressure and pre-existing motility disorders[15]. Antisecretory medication was halted 7 d before assessment of esophageal function. Preoperative and short-term outcome data were entered in a prospective database. Long-term outcome data were collected retrospectively.
Laparoscopic floppy Nissen fundoplication was performed by the standard 5-trocar technique as described[16]. Every patient had prophylactic anticoagulation and compressive elastic stockings. The fundus was routinely mobilized by ligating and dividing the short gastric vessels (Kellokumpu I and Haglund C)[16]. The Rossetti-Hell modification[17] with mobilization of the fundus posteriorly to the upper pole of the spleen without division of short gastric vessels was preferred by Roberts PJ. A short (20 mm) fundic wrap was constructed around the distal esophagus with 2-0 non-absorbable sutures. Nasogastric tubes (18 F) and bougies (36 F) allowed calibration of the fundic wrap and closure of the hiatus. A posterior hiatoplasty was performed with 2-0 non-absorbable stitches when the esophageal hiatus was enlarged. The left side of the wrap was anchored to the cardia with an additional 1-2 sutures. A nasogastric tube was left in place until the following morning when intake of liquids was started. Solid intake was usually started on the second or third postoperative day. All patients received dietary instructions before their discharge.
Preoperative and short-term symptom assessment three months after surgery was based on a standardized questionnaire and interview about heartburn, regurgitation, and dysphagia according to the DeMeester-Johnson reflux scale[18]. Regurgitation was graded as: none = 0, mild = 1 (occasional after straining, large meal, or lying down), moderate = 2 (predictable with position change, straining, or lying down), severe = 3 (history of aspiration). Heartburn grades were none = 0, mild = 1 (recognizable symptom, no prior history of medical treatment), moderate = 2 (primary reason for medical visit or medical problem), severe = 3 (constant, marked disability in activities of daily living). Dysphagia grades were none = 0, mild = 1 (occasional with coarse foods), moderate = 2 (require liquids to clear), severe = 3 (history of meat impaction necessitating medical attention)[18]. In addition, the frequency of heartburn, regurgitation and dysphagia was rated as absent = 0, occasional (less than once every two weeks) as 1, frequent symptoms (more than once every two weeks but less than daily) as 2, and daily symptoms (at least one attack/day to constant symptoms) as 3[19].
Side effects of surgery such as disturbed belching ability, bloating (defined as abdominal swelling), and flatulence were analyzed with the patients assessing their degree of disturbance by any postoperative decrease (belching) or increase (flatus, bloating) on a scale where 0 = no change, 1 = mild change, 2 = moderate change, and 3 = severe change.
Upper gastrointestinal endoscopy was routinely performed preoperatively and at three months after surgery. Endoscopic classification of esophagitis was based on the modified Savary-Miller 5-grade classification[20]. The state and localization of the fundic wrap and the presence of paraesophageal hernia were checked postoperatively.
Overall short-term success of the operation was assessed by the patient’s subjective perception of the outcome after surgery compared to that with medical therapy and patient’s willingness to undergo surgery again for similar preoperative conditions.
Long-term outcome was investigated in a subgroup of patients with a median follow-up of 10 years and was based on the same self-completed, standardized questionnaire about heartburn, regurgitation, and dysphagia[18,19], and side effects of surgery as in the short-term. Patients also reported time to symptom recurrence and the use of PPI medication as well as the date of any re-fundoplication. Finally, long-term outcome of surgery was assessed by a self-rated 7-point Likert scale describing outcome as good as expected (0), mildly (+1), moderately (+2) or markedly (+3) better or worse as -1, -2, -3 than expected and by willingness to undergo surgery again under similar preoperative conditions. During the long-term follow-up, objective testing including upper gastrointestinal endoscopy, barium examination, and esophageal function studies was not routinely performed.
Long-term quality of life assessment was done by the self-completed Gastrointestinal Symptom Rating Scale (GSRS)[21,22], and overall quality of life by RAND-36 (SF-36)[23,24]. The GSRS is a disease-specific instrument comprising 15 items, each rated on a 7-point Likert scale from no discomfort to very severe discomfort, and further divided into five dimensions: abdominal pain syndrome (abdominal pain, hunger pain and nausea), reflux syndrome (heartburn and acid regurgitation), diarrhea syndrome (diarrhea, loose stools and urgent need for defecation), indigestion syndrome (borborygmus, abdominal distension, eructation and increased flatus), and constipation syndrome (constipation, hard stools and feeling of incomplete evacuation). The higher the GSRS score, the more the patient suffers from gastrointestinal symptoms. The Finnish RAND-36[23] covers eight areas of health status, including physical functioning, role limitation due to physical health problems, bodily pain, general health, energy, social functioning, role limitation due to personal emotional problems, and emotional well-being. The raw responses were recoded according to the original version of the RAND-36, each item being scored on a 0-to-100 scale with higher scores indicating better quality of life[23,24]. Questionnaires were sent to the patients in May 2006 and returned by November 2006. Incomplete answers were completed by telephone interview.
Consistent with Lundell et al[25], laparoscopic Nissen fundoplication was considered failed if at least one of the following criteria was present: persistence or recurrence of moderate to severe heartburn or regurgitation[18] occurring more than once every two weeks (grade 2) or daily (grade 3)[19] or both; moderate to severe dysphagia[18] reported in combination with heartburn or regurgitation or both; the use of daily or weekly PPI medication; endoscopic evidence of erosive esophagitis Savary-Miller grade 1-4; pathological 24-h pH monitoring; and necessity to undergo redo surgery.
The Central Hospital of Central Finland ethics committee approved this study (K-Sshp Dnro 47/2005). The causes of death were obtained from the National Cause of Death Registry.
The data are presented as mean ± SD, as median with interquartile range (IQR), or as counts with percentages. The 95%CIs are given for the most important outcomes. Groups were compared using the Mann-Whitney U test or the χ2 test. The statistical significance between groups in HRQL measures was evaluated by bootstrap-type analysis of co-variance because of the violation of distribution assumptions. Repeated measures for dichotomous outcomes were analyzed by Cochran’s Q test and the marginal homogeneity test. Time-to-failure analysis was based on the product limit estimate (Kaplan-Meier) of the cumulative “survival” function. The Finnish general population values[23] for the eight Rand-36 domains were weighted to match the gender- and age-distribution of the study population. Statistical analyses were performed with Stata statistical software, release 12.1 (StataCorp, College Station, TX, United States).
Baseline clinical characteristics of the study population are shown in Table 1. Esophageal dilatations up to 18 mm in diameter were performed preoperatively in three of the four patients having esophageal stricture. Frequent or daily heartburn in 89.9% and regurgitation in 87.2% of the patients were the main presenting symptoms. DeMeester-Johnson severity grades are shown in Table 1, and operative data and surgical outcome in Table 2. While major intraoperative complications occurred in three patients, no deaths occurred. A distal esophageal perforation caused by diathermy scissors in one patient and by an inadvertent push of the calibration tube in another patient with esophageal stricture were suture-repaired and covered by the fundic wrap. A small fundic perforation caused by Harmonic scissors-induced thermal injury occurred postoperatively in one patient and necessitated a laparotomy and suture repair. Overall, 30-d morbidity was 7.6% (95%CI: 4.7-11.7) (Table 2). Pleural empyema in one patient with esophageal injury necessitated a thoracotomy and decortication. Comparing the two treatment centers and time periods, 30-d morbidity was similar (10.0% vs 5.4%, P = 0.17), but operation time [median 135 min (IQR 116.3-180 min) vs 75 min (IQR 65-90 min), P < 0.001] and postoperative hospital stay [median 3 d (IQR 2-4 d) vs 2 d (IQR 1-2 d), P < 0.001] were shorter during the latter period.
| Follow-up | Study population (n = 249) | Long-term (n = 139) |
| Age, yr (mean ± SD) | 51.2 ± 11.2 | 51.5 ± 10.6 |
| Sex, male/female | 131/118 | 76/62 |
| ASA classification | ||
| I | 130 (52.0) | 85 (61.2) |
| II | 96 (38.4) | 40 (28.8) |
| III | 23 (9.2) | 14 (10.1) |
| Duration of GERD in years, median (IQR) | 6 (5.0-10.0) | 6 (4.0-10.0) |
| Preoperative medication | ||
| PPI | 222 (89.2) | 120 (86.3) |
| H2-antagonist and/or prokinetic | 27 (10.8) | 19 (13.7) |
| Duration of medical treatment, mo, median (IQR) | 18 (8.0-36.0) | 18 (6.0-36.0) |
| Preoperative Helicobacter pylori eradication | 36 (14.6) | 20 (14.4) |
| Preoperative symptom severity grade 1/2/3 as %1 | ||
| Heartburn | 0/49.8/48.6 | 0/55.4/42.4 |
| Regurgitation | 5.6/87.6/4.4 | 5.0/89.2/4.3 |
| Dysphagia | 12.0/9.2/0 | 12.9/11.5/0 |
| pH < 4 of total time, median (IQR) as %2 | 12.0 (8.0-18.7) | 11.5 (7.4-19.1) |
| DeMeester score, median (IQR) | 42.5 (28.4-71.3) | 41.0 (26.2-69.3) |
| Lower esophageal sphincter pressure in mmHg3, median (IQR) | 11.0 (8.0-16.0) | 11.0 (7.5-17.0) |
| Preoperative grading of esophagitis (Savary-Miller) | ||
| None | 68 (27.3) | 36 (25.9) |
| Grade 1 (single erosive lesion, one longitudinal fold) | 22 (8.8) | 16 (11.5) |
| Grade 2 (multiple erosive lesions, more than one fold) | 98 (39.4) | 57 (41.0) |
| Grade 3 (circumferential lesions) | 13 (5.2) | 3 (2.2) |
| Grade 4 (chronic ulcer or stricture ± Gr. 1-3)4 | 5 (2.0) | 3 (2.2) |
| Grade 5 (Barrett’s esophagus ± Gr. 1-3) | 43 (17.3)5 | 24 (17.2)6 |
| n = 249 | |
| Type of surgery | |
| Floppy Nissen fundoplication | 213 (85.5) |
| Rosetti-Hell fundoplication | 36 (14.5) |
| Hiatoplasty | 235 (94.4) |
| Conversion to open surgery1 | 7 (2.8) |
| Operation time, min, median (IQR) | 90 (70.3-135.0) |
| Mortality (30 d) | 0 (0.0) |
| Intraoperative complications | 3 (1.2) |
| Esophageal perforation | 2 (0.8) |
| Burn injury of the fundus | 1 (0.4) |
| Postoperative morbidity (30 d)2 | 19 (7.6) |
| General | 12 (4.8) |
| Atelectasis + fever | 5 (2.0) |
| Pneumonia | 7 (2.8) |
| Surgical | 9 (3.6) |
| Pleural empyema | 1 (0.4) |
| Fundic perforation (burn injury) | 1 (0.4) |
| Port-site hernia and bowel obstruction | 1 (0.4) |
| Port-site bleeding | 2 (0.8) |
| Excessive pain at port-site | 1 (0.4) |
| Gastric dilatation | 1 (0.4) |
| Wound infection | 1 (0.4) |
| Urinary retention | 1 (0.4) |
| Reoperation rate3 | 5 (2.0) |
| Relaparotomy | 4 (1.6) |
| Thoracotomy and decortication | 1 (0.4) |
| Postoperative hospital stay, d, median (IQR) | 2 (2-3) |
Two of the 249 operated patients could not be contacted 3 mo after surgery, leaving 247 patients for short-term analysis. Based on symptom control and endoscopically-verified healing of erosive esophagitis, gastroesophageal reflux disease was cured in 243 of the 247 patients [98.4% (95%CI: 95.9%-99.6%)]. Only four patients reported short-term failures. Two had persisting reflux symptoms and erosive esophagitis (grade 2) with partly disrupted plication. One had erosive esophagitis (grade 1) and too distally placed and partly disrupted plication. Another one who had an apparently normal fundoplication had persistence of erosive esophagitis (grade 1). Three patients underwent a reoperation, and one was treated with PPI-medication. None of the patients used PPI-medication at three months post-surgery. Barrett’s esophagus without erosive changes was observed in 45 patients 3 mo after surgery and 2 patients had strictures, of which 1 was dilated. No cases of paraesophageal hernia were found. The short-term failure rate was similar between the two centers and time periods (1.7% vs 1.6%, P = 0.94). Two gastric ulcers and one case of acute gastritis were encountered in three patients with ulcer-like dyspepsia within 3-5 mo after surgery. All had biopsy-verified Helicobacter pylori infection and were treated by eradication therapy and followed-up by endoscopy and biopsies.
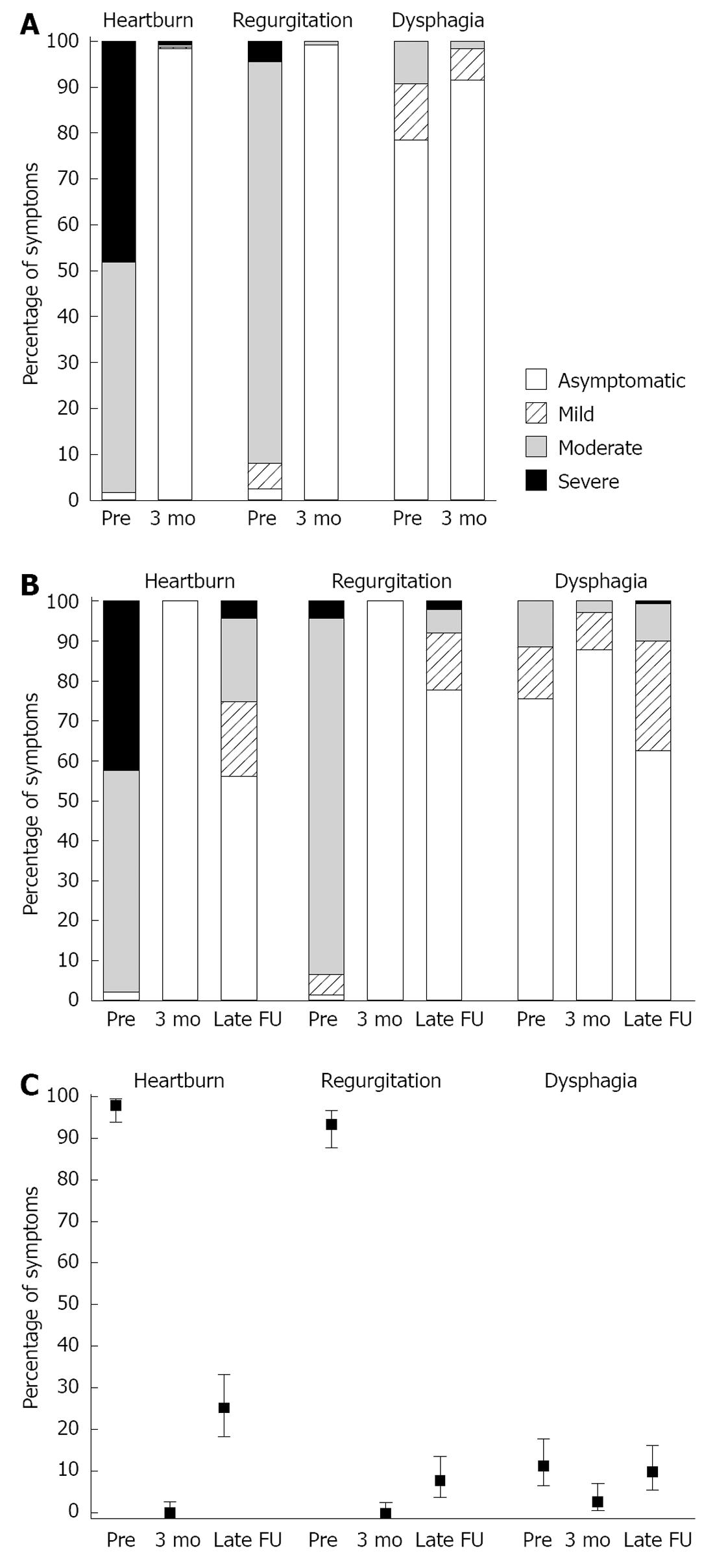
The patients observed typical reflux symptoms, especially heartburn and regurgitation, changed markedly after surgery. While 4 patients were asymptomatic for heartburn before and after surgery, 239 patients with reporting heartburn preoperatively [98.4% (95%CI: 95.8%-99.5%)] were completely symptom free (Figure 1A). Regurgitation was ameliorated in 239 [99.2% (97.0%-99.9%)] of the 241 patients, while 6 were asymptomatic before and after surgery (Figure 1A). Transitory new-onset dysphagia or worsening of preoperative dysphagia within 3 mo after surgery was reported by 176 patients (71.3%), but overall, dysphagia was significantly reduced from baseline. Dysphagia was alleviated in 45 [84.9% (72.4%-92.3%)] of the 53 patients having preoperative dysphagia. New onset dysphagia (grade 1 in all) was reported by 13 of the 194 patients (6.7%) without preoperative dysphagia.
A decreased ability to belch was reported by 164 [66.4% (60.1%-72.3%)], increased flatulence by 183 [74.1% (68.2%-79.4%)] and increased bloating by 61 [24.7% (19.4%-72.3%)] of the 247 patients. The ability to vomit could not be evaluated at three months.
At their first clinical visit, 235 [95.1% (95%CI: 92.7%-98.0%)] patients reported better outcome after antireflux surgery than with preoperative medical treatment and were willing to have the procedure repeated in situations similar to preoperative ones.
A cohort of the first 180 consecutive patients operated on between 1992 and 2002 was selected to obtain a median follow-up time of 10 years until November 2006. Of these, 14 had died of the following non-gastroesophageal reflux disease (GERD), related causes: myocardial infarctions (n = 3), intoxications (n = 2), cerebral infarction, pulmonary embolism, aortic rupture, gastric cancer, pneumonia, necrotizing fasciitis, chemotherapy-related sepsis, cerebral trauma and intracranial hemorrhage, and severe myasthenia gravis. In addition, 1 patient had severe dementia, 1 had undergone esophageal resection for Barrett’s esophagus-related adenocarcinoma, 3 returned incomplete questionnaires, and 22 patients could not be contacted, leaving 139 available for evaluation of late outcomes [median follow-up time 10.2 years (IQR 7.2-11.6 years), response rate 85%]. During the long-term follow-up, 24-h pH monitoring and endoscopy was done in 32 patients; 6 showed endoscopically verified disrupted fundoplication and pH < 4 median 25.1% (IQR 13.0%-42.8%) of total time, and 26 had intact fundoplication and pH median 0.6% (IQR 0.1%-2.4%).
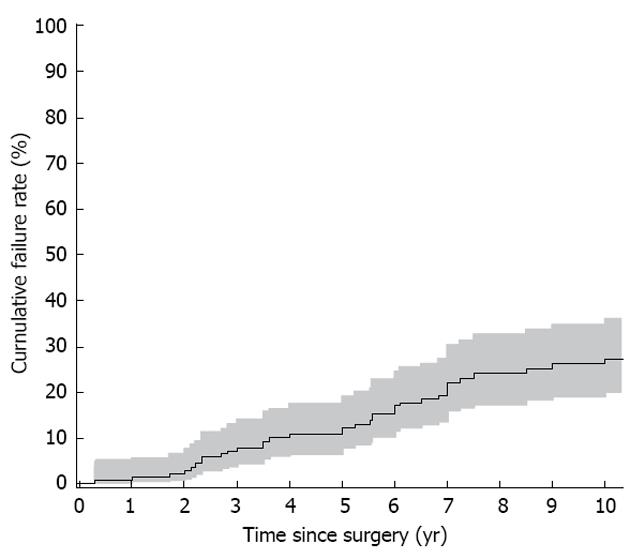
The crude long-term failure rate was 24.5% (34 of 139 patients): 6 patients (4.3%) underwent reoperation for symptomatic and objective recurrence caused by defective plication, 16 (11.5%) had heartburn, regurgitation, dysphagia and PPI medication on a daily/weekly basis, 11 patients (7.9%) not using PPI medication reported frequent/daily symptoms, and 1 was asymptomatic while on medication (Figure 1B and C). The cumulative 5-year failure rate was 12.3% (95%CI: 7.8%-36.0%) and the 10-year failure rate 27.1 % (20.1%-36.0%) (Figure 2), and cure rates 87.7% (81.0%-92.2%) and 72.9% (64.0%-79.9%), respectively. One patient underwent a reoperation for paraesophageal hernia and one for late trocar-site hernia.
Decreased belching ability in the long-term was reported by 61.2% (52.5%-69.3%), increased rectal flatulence by 91.4% (85.4%-95.5%) and bloating by 71.9% (63.7%-79.2%). Total inability to vomit was reported by 43 patients (30.9%).
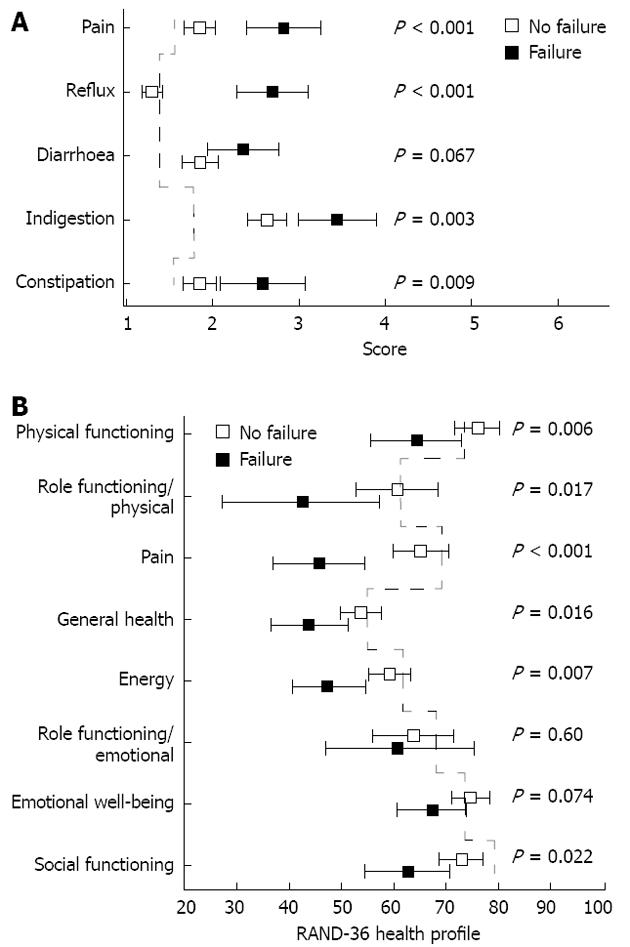
The mean GSRS score describing overall discomfort related to gastrointestinal symptoms was 1.9 (95%CI: 1.8-2.0) in patients cured by antireflux surgery and 2.8 (2.4-3.1) in those with failed antireflux surgery (P < 0.001). Mean scores for all GSRS dimensions in comparison to a healthy control population are shown in Figure 3A. The failure of antireflux surgery and post-fundoplication side effects were reflected in the reflux syndrome score and indigestion syndrome score. Mean values of RAND-36 QoL scores were similar to the scores of the Finnish age- and gender-matched reference population for patients without treatment failure but were significantly impaired for those with failed antireflux surgery (Figure 3B).
Long-term outcomes were subjectively graded as good as expected (0) by 18.0%, moderately better (+2) by 14.4%, markedly better (+3) by 50.4%, and worse (-1) 5.8%, moderately worse (-2) 8.6% and markedly worse (-3) by 2.9%. At the time of this survey, 118 patients [84.9% (95%CI: 77.8%-90.4%)] were willing to undergo surgery again under similar preoperative conditions, whereas 21 patients (15.1%) chose medical treatment as a better initial treatment option.
Laparoscopic Nissen fundoplication has become the method of choice in antireflux surgery providing good short-term outcome in over 90% of patients, an associated morbidity rate of less than 10%, and only a 5% incidence of new-onset dysphagia[5-10,12,13]. Here, we show that laparoscopic Nissen fundoplication effectively abolished heartburn and regurgitation, alleviated most preoperative dysphagia, and cured erosive esophagitis in most patients in the short term. This was achieved with low morbidity, a short hospital stay, a low incidence of new-onset dysphagia, and good patient satisfaction, with approximately 95% of the patients reporting a better outcome after surgery compared with non-surgical medical therapy. Mechanical side effects of total fundoplication may lead to a functional obstruction in the gastroesophageal junction and to an inability to vent air from the stomach[12]. As a result, we observed common postoperative side effects including inability to belch, abdominal bloating, and increased flatulence. However, these mild side effects did not seem to limit the success of antireflux surgery.
Long-term outcomes after laparoscopic antireflux surgery in this study were examined in multiple domains including symptom response, side effects of surgery, durability of the antireflux surgery, patient’s subjective perception of the overall success of the operation, and quality of life. In addition, treatment failure was defined according to composite criteria in contrast to previous studies[26-30] expressing the clinical outcome as the point prevalence of reflux-associated symptoms and patient satisfaction. However, our 5-year (88%) and 10-year (73%) cure rates compare well to previous studies reporting long-term control of reflux in 74%-90% of patients[26-31]. Our results also compare well to the nationwide long-term outcome after laparoscopic antireflux surgery in Sweden demonstrating a treatment failure in 25%-29% of the patients[32]. Only one randomized study comparing medical and surgical therapies for GERD and including patients with good response to PPI therapy, has reported similar remission rates at five years (85% vs 92%) between laparoscopic antireflux surgery and modern antisecretory medication[9]. Similar outcomes after laparoscopic Nissen fundoplication were obtained in our study despite the inclusion of patients reporting residual symptoms while on medical antisecretory treatment.
Patient well-being or quality of life are among the most important outcome measures in the field of functional surgery. The GSRS is a useful patient-related scale for evaluating the outcome of treatment for GERD[21]. In our study, the GSRS reflected well the long-term success of antireflux surgery as well as the side effects of antireflux surgery; it differentiated patients experiencing treatment failure from those being cured and from healthy controls[22]. Certain side effects, including increased bloating and rectal flatulence, manifest as indigestion syndrome and seem to be inevitable for most patients following fundoplication.
Overall quality of life was evaluated with RAND-36 (SF-36) because it is well validated in Finnish[23]. Consistent with previous studies[26,30] our results revealed that the quality of life of patients with long-term treatment success is similar to that of an age- and sex-matched general population. On the other hand, failed antireflux surgery and symptom recurrence significantly worsened quality of life in most dimensions.
Patients were also given a chance to evaluate the result of their surgery in the long-term. Here, 83% of the patients rated their surgical result to be as good as or better than expected, while only 17% felt that their surgical result was only fair or poor. Similarly, 118 patients (85%) were willing to undergo surgery again under similar preoperative conditions.
A major challenge with this study and other similar studies was its retrospective nature and the lack of systematic long-term assessment by endoscopy and ambulatory 24-h pH monitoring[31]. The significance of the use of antireflux medication in the long term is also debatable without objective measurements and may not be a reliable marker of surgical failure. On the other hand, we used standardized symptom questionnaires, composite criteria, and quality of life assessment to define treatment failures. Furthermore, it is the symptom response experienced by patients that ultimately determines the success or failure of antireflux surgery and quality of life, not the change in objective measurements. It is also well known that the outcome after antireflux surgery is dependent on surgeon’s experience and quality of the surgery. Satisfactory short-term outcomes indicate, however, that the quality of surgery has been as good in this study as elsewhere. The long-term outcome was investigated in 139 of the first 180 consecutive patients selected for the 10-year follow-up. The compliance in this study compares favorably with that in earlier studies with 85% of the eligible patients returning the questionnaires for long-term evaluation.
In the short-term, laparoscopic antireflux surgery effectively alleviated symptoms of gastroesophageal reflux disease and cured erosive esophagitis. Postoperative adverse effects were usually mild and patient satisfaction was good. For the long-term, our results indicate decreasing effectiveness of laparoscopic antireflux surgery, although most of the patients seem to have an overall quality of life similar to that of the general population.
Optimal management of chronic gastroesophageal reflux disease (GERD) is uncertain because treatment options can include either modern medical therapy that uses proton pump inhibitors or antireflux surgery.
Only one randomized study comparing medical and surgical therapies for GERD, has reported similar remission rates at 5 years. Data on long-term (10-year) cures and quality of life after antireflux surgery vs medical therapy are limited.
To assess long-term outcomes, the authors examined several domains affected by the operation and defined treatment failures based on composite criteria and quality of life assessment. The results show that the excellent short-term results after laparoscopic Nissen fundoplication deteriorate over time. Quality of life analysis with the Gastrointestinal Symptom Rating Scale reflected well the side effects of antireflux surgery and differentiated patients having treatment failure from those being cured and from healthy controls. Overall quality of life (RAND-36) of patients with long-term treatment success was similar to that of an age- and sex-matched general population. Failed antireflux surgery and symptom recurrence significantly worsened the quality of life in most dimensions.
By defining treatment outcomes with composite criteria and understanding how quality of life is affected by failed antireflux surgery, this study represents a potential new strategy for assessment of the long-term outcome after antireflux surgery.
The authors examined the short- and long-term outcome and quality of life after laparoscopic fundoplication. By addressing several domains affected by the operation and using composite criteria to define treatment failure, they show the excellent short-term results after laparoscopic Nissen fundoplication deteriorate over time. They also show failed antireflux surgery is associated with reduced quality of life. Use of composite criteria and quality of life assessment to define treatment failure represents a potential new strategy for the assessment of long-term outcomes following antireflux surgery.
P- Reviewers Clark J, Detry O S- Editor Wen LL L- Editor A E- Editor Li JY
| 1. | Dent J. Controversies in long-term management of reflux disease. Baillieres Best Pract Res Clin Gastroenterol. 2000;14:811-826. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 2. | An evidence-based appraisal of reflux disease management--the Genval Workshop Report. Gut. 1999;44 Suppl 2:S1-16. [PubMed] |
| 3. | Dellon ES, Shaheen NJ. Persistent reflux symptoms in the proton pump inhibitor era: the changing face of gastroesophageal reflux disease. Gastroenterology. 2010;139:7-13.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 4. | Nealis TB, Howden CW. Is there a dark side to long-term proton pump inhibitor therapy? Am J Ther. 2008;15:536-542. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 28] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 5. | Wileman SM, McCann S, Grant AM, Krukowski ZH, Bruce J. Medical versus surgical management for gastro-oesophageal reflux disease (GORD) in adults. Cochrane Database Syst Rev. 2010;CD003243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 67] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 6. | Mahon D, Rhodes M, Decadt B, Hindmarsh A, Lowndes R, Beckingham I, Koo B, Newcombe RG. Randomized clinical trial of laparoscopic Nissen fundoplication compared with proton-pump inhibitors for treatment of chronic gastro-oesophageal reflux. Br J Surg. 2005;92:695-699. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 117] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 7. | Mehta S, Bennett J, Mahon D, Rhodes M. Prospective trial of laparoscopic nissen fundoplication versus proton pump inhibitor therapy for gastroesophageal reflux disease: Seven-year follow-up. J Gastrointest Surg. 2006;10:1312-1316; discussion 1316-1317. [PubMed] |
| 8. | Grant A, Wileman S, Ramsay C, Bojke L, Epstein D, Sculpher M, Macran S, Kilonzo M, Vale L, Francis J. The effectiveness and cost-effectiveness of minimal access surgery amongst people with gastro-oesophageal reflux disease - a UK collaborative study. The REFLUX trial. Health Technol Assess. 2008;12:1-181, iii-iv. [PubMed] |
| 9. | Galmiche JP, Hatlebakk J, Attwood S, Ell C, Fiocca R, Eklund S, Långström G, Lind T, Lundell L. Laparoscopic antireflux surgery vs esomeprazole treatment for chronic GERD: the LOTUS randomized clinical trial. JAMA. 2011;305:1969-1977. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 315] [Cited by in RCA: 300] [Article Influence: 21.4] [Reference Citation Analysis (0)] |
| 10. | Anvari M, Allen C, Marshall J, Armstrong D, Goeree R, Ungar W, Goldsmith C. A randomized controlled trial of laparoscopic Nissen fundoplication versus proton pump inhibitors for the treatment of patients with chronic gastroesophageal reflux disease (GERD): 3-year outcomes. Surg Endosc. 2011;25:2547-2554. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 62] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 11. | Ireland AC, Holloway RH, Toouli J, Dent J. Mechanisms underlying the antireflux action of fundoplication. Gut. 1993;34:303-308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 132] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 12. | Lundell L. Therapy of gastroesophageal reflux: evidence-based approach to antireflux surgery. Dig Dis. 2007;25:188-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Catarci M, Gentileschi P, Papi C, Carrara A, Marrese R, Gaspari AL, Grassi GB. Evidence-based appraisal of antireflux fundoplication. Ann Surg. 2004;239:325-337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 238] [Cited by in RCA: 204] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 14. | Johnson LF, Demeester TR. Twenty-four-hour pH monitoring of the distal esophagus. A quantitative measure of gastroesophageal reflux. Am J Gastroenterol. 1974;62:325-332. [PubMed] |
| 15. | McLauchlan G. Oesophageal function testing and antireflux surgery. Br J Surg. 1996;83:1684-1688. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 16. | Dallemagne B, Perretta S. Twenty years of laparoscopic fundoplication for GERD. World J Surg. 2011;35:1428-1435. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 25] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 17. | Rossetti M, Hell K. Fundoplication for the treatment of gastroesophageal reflux in hiatal hernia. World J Surg. 1977;1:439-443. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 122] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 18. | Demeester TR, Johnson LF, Joseph GJ, Toscano MS, Hall AW, Skinner DB. Patterns of gastroesophageal reflux in health and disease. Ann Surg. 1976;184:459-470. [PubMed] |
| 19. | Pope CE. Acid-reflux disorders. N Engl J Med. 1994;331:656-660. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 70] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 20. | Nayar DS, Vaezi MF. Classifications of esophagitis: who needs them? Gastrointest Endosc. 2004;60:253-257. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 21. | Revicki DA, Wood M, Wiklund I, Crawley J. Reliability and validity of the Gastrointestinal Symptom Rating Scale in patients with gastroesophageal reflux disease. Qual Life Res. 1998;7:75-83. [PubMed] |
| 22. | Dimenäs E, Carlsson G, Glise H, Israelsson B, Wiklund I. Relevance of norm values as part of the documentation of quality of life instruments for use in upper gastrointestinal disease. Scand J Gastroenterol Suppl. 1996;221:8-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 229] [Cited by in RCA: 265] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 24. | Hays RD, Sherbourne CD, Mazel RM. The RAND 36-Item Health Survey 1.0. Health Econ. 1993;2:217-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1804] [Cited by in RCA: 2011] [Article Influence: 62.8] [Reference Citation Analysis (0)] |
| 25. | Lundell L, Miettinen P, Myrvold HE, Pedersen SA, Liedman B, Hatlebakk JG, Julkonen R, Levander K, Carlsson J, Lamm M. Continued (5-year) followup of a randomized clinical study comparing antireflux surgery and omeprazole in gastroesophageal reflux disease. J Am Coll Surg. 2001;192:172-179; discussion 179-181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 255] [Cited by in RCA: 220] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 26. | Dallemagne B, Weerts J, Markiewicz S, Dewandre JM, Wahlen C, Monami B, Jehaes C. Clinical results of laparoscopic fundoplication at ten years after surgery. Surg Endosc. 2006;20:159-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 256] [Cited by in RCA: 235] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 27. | Salminen PT, Hiekkanen HI, Rantala AP, Ovaska JT. Comparison of long-term outcome of laparoscopic and conventional nissen fundoplication: a prospective randomized study with an 11-year follow-up. Ann Surg. 2007;246:201-206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 94] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 28. | Kelly JJ, Watson DI, Chin KF, Devitt PG, Game PA, Jamieson GG. Laparoscopic Nissen fundoplication: clinical outcomes at 10 years. J Am Coll Surg. 2007;205:570-575. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 77] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 29. | Yang H, Watson DI, Lally CJ, Devitt PG, Game PA, Jamieson GG. Randomized trial of division versus nondivision of the short gastric vessels during laparoscopic Nissen fundoplication: 10-year outcomes. Ann Surg. 2008;247:38-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 48] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 30. | Broeders JA, Rijnhart-de Jong HG, Draaisma WA, Bredenoord AJ, Smout AJ, Gooszen HG. Ten-year outcome of laparoscopic and conventional nissen fundoplication: randomized clinical trial. Ann Surg. 2009;250:698-706. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 122] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 31. | Oelschlager BK, Ma KC, Soares RV, Montenovo MI, Munoz Oca JE, Pellegrini CA. A broad assessment of clinical outcomes after laparoscopic antireflux surgery. Ann Surg. 2012;256:87-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 32. | Sandbu R, Sundbom M. Nationwide survey of long-term results of laparoscopic antireflux surgery in Sweden. Scand J Gastroenterol. 2010;45:15-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |