Published online Mar 28, 2013. doi: 10.3748/wjg.v19.i12.1992
Revised: December 25, 2012
Accepted: January 5, 2013
Published online: March 28, 2013
Processing time: 129 Days and 18.7 Hours
Double-balloon enteroscopy (DBE) and video capsule endoscopy are useful for the diagnosis of lymphoma in the small intestine. However, DBE cannot be safely performed in cases with passage disturbance due to wall thickening and stenosis. Additionally, video capsule endoscopy cannot be performed in such cases because of the risk of retention. Here, we report 4 cases of primary follicular lymphoma of the gastrointestinal tract that could be detected using 18F-fluorodeoxyglucose positron emission tomography combined with computed tomography (PET-CT). The endoscopic findings of these 4 cases included lesions with wall thickening, which comprised macroscopically clusters of nodules, dense clusters of whitish granules or small nodules, fold thickening and ulcers with irregular margins that occupied the whole lumen with edematous mucosa. All patients fulfilled the World Health Organization grade 1 criteria. 18F-fluorodeoxyglucose PET-CT can help predict the risks that may result from certain endoscopic examinations, such as DBE and video capsule endoscopy.
- Citation: Tari A, Asaoku H, Kunihiro M, Tanaka S, Yoshino T. Usefulness of positron emission tomography in primary intestinal follicular lymphoma. World J Gastroenterol 2013; 19(12): 1992-1996
- URL: https://www.wjgnet.com/1007-9327/full/v19/i12/1992.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i12.1992
Primary follicular lymphoma of the gastrointestinal tract (FL-GI) is often diagnosed by initially detecting duodenal lesions using esophago-gastro-duodenoscopy (EGD)[1,2]. FL-GI lesions can exist in broad areas, ranging from the descending portion of the duodenum to the ileum, and may include lymph node involvement[1,2]. The correct diagnosis of the locations of lesions is vital to decisions regarding therapeutic plans[3]. Double-balloon enteroscopy (DBE) and video capsule endoscopy (VCE) are useful for the diagnosis of lesions in the small intestine[4]. However, DBE cannot be safely performed in cases with passage disturbance due to wall thickening and stenosis, and VCE cannot be performed in these cases because of the risk of retention[4]. Conversely, 18F-fluorodeoxyglucose (FDG) positron emission tomography combined with computed tomography (PET-CT) has been reported to be useful for detecting lymph node involvement in the diagnosis of the clinical stages of follicular lymphomas[5]. This study reports the cases of 4 patients for whom PET-CT was useful in the detection of FL-GI in the digestive tract, the location of which ranged from the duodenum to the ileocecal valve.
Twenty FL-GI patients (male/female 9/11, age 46-82 years, mean 58 years) consulted the Division of Gastroenterology, Department of Internal Medicine, Hiroshima Red Cross Hospital and Atomic-Bomb Survivors Hospital from December 2004 to May 2010. In 2 of the 18 patients with duodenal lesions, FL-GI lesions were detected using PET-CT. One of the 14 patients with jejunal lesions and 2 of the 12 patients with ileal lesions had abnormal accumulations according to the PET-CT results.
Table 1 shows the 4 FL-GI patients with abnormal accumulations by PET-CT who had gastrointestinal lesions detected from the duodenum to the ileocecal valve. Case 1 had duodenal lesion, case 2 had jejunal lesions, case 3 had lesions from the terminal ileum to the ileocecal valve and case 4 had lesions in broad areas from the duodenum to the ileum. All lesions were diagnosed by endoscopic examination with biopsy.
| Case No. | Age (yr) | Sex | Diagnosis(WHO grade) | Clinical stage(Lugano) | FLIPI | Locations in GI tract | Endoscopic appearances | PET-CT |
| 1 | 52 | M | FL (grade 1) | I | Low | Duodenum descending portion-duodenojejunal flexure | Dense cluster of whitish granules | (+) descending portion and duodenojejunal flexure of duodenum |
| Jejunum | Cluster of whitish granules | (-) | ||||||
| Terminal ileum | Normal lymph follicles | (-) | ||||||
| 2 | 62 | F | FL (grade 1) | II2 | Intermediate | Jejunum | Swelling and thickening of folds | (+) jejunum |
| Ileum | Normal lymph follicles | (-) | ||||||
| 3 | 66 | F | FL (grade 1) | II2 | Intermediate | Papilla vater | Mild swelling and erosion | (-) |
| Jejunum | Sparse cluster of small nodules | (-) | ||||||
| Ileum | Sparse cluster of small nodules | (-) | ||||||
| Terminal ileum-ileocecal valve | Dense cluster of granules and nodules | (+) ileocecal valve | ||||||
| 4 | 61 | F | FL (grade 1) | IV | High | Duodenal bulb | Rough mucosa | (-) |
| Duodenum descending portion-jejunum | Cluster of numerous whitish granules | (+) duodenum-jejunum | ||||||
| Ileum | Multiple ulcers with irregular margin | (+) ileum |
The mandatory examinations included palpation of the superficial lymph nodes, blood tests, urinalysis, chest radiography, abdominal ultrasonography, contrast-enhanced computed tomography (CT) scan (General Electric, Fairfield, CT, United States) (CT/CE+) of the neck, chest, abdomen and pelvis, PET-CT (General Electric, Fairfield, Connecticut, United States), bone marrow aspiration, endoscopy with biopsies [EGD (Olympus, Tokyo, Japan), colonoscopy (Fujinon, Tokyo, Japan), DBE (Fujinon, Tokyo, Japan)] and VCE (Given Imaging, Yoqneam, Israel). Each patient was classified by the location of the lesions, clinical stage (Lugano International classification[6]), FL histological grade (World Health Organization grade)[7] and follicular lymphoma international prognosis index[8]. The macroscopic findings of FL-GI were classified by endoscopy into the following 6 types: whitish granules, multiple small nodules, fold swelling and thickening, mass forming, ulcers with irregular margins and rough mucosa[1].
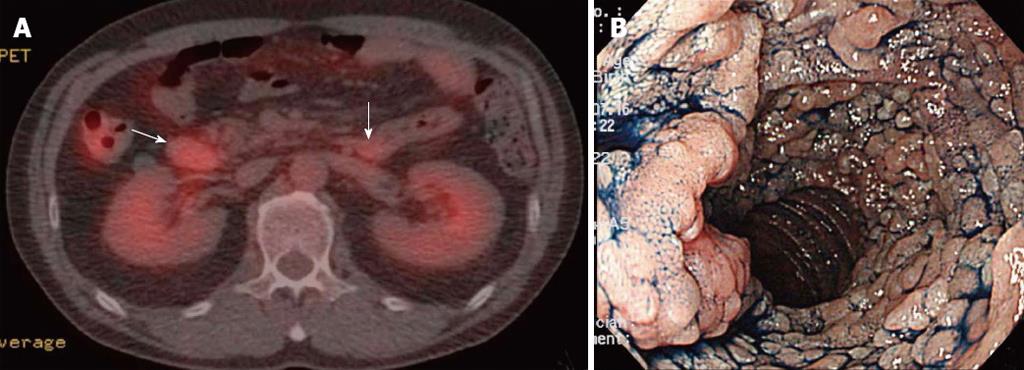
Case 1 is a 52-year-old man who had no symptoms but was diagnosed to have abnormalities in the descending portion of the duodenum by EGD for gastric cancer screening (Table 1). This patient had wall thickening with abnormal accumulation at the descending portion of the duodenum and at the duodenojejunal flexure [maximum standardized uptake value (SUVmax) 6.6 and 5.5, respectively] (Figure 1A) by PET-CT. However, there were no abnormal findings in the small intestine by PET-CT. EGD showed lesions with dense clusters of whitish granules, making it difficult to see the folds in the descending and horizontal portions of duodenum (Figure 1B). The jejunum showed only rough clusters of whitish granules. The terminal ileum of this patient showed mucosa with normal lymphoid tissues.
Case 2 is a 62-year-old woman who presented with swelling of the mesenteric lymph nodes (max, 1.5 cm in diameter) by abdominal ultrasonography and a mild accumulation of FDG (SUVmax, 3.0) by PET-CT. A laparotomic lymph node biopsy led to the diagnosis of FL. Regarding the intestinal lesions, localized accumulation was demonstrated by PET-CT (SUVmax, 3.9) performed in the jejunum 25 mo later. The EGD showed swelling and thickening of the folds that occupied half of the lumen (Table 1).
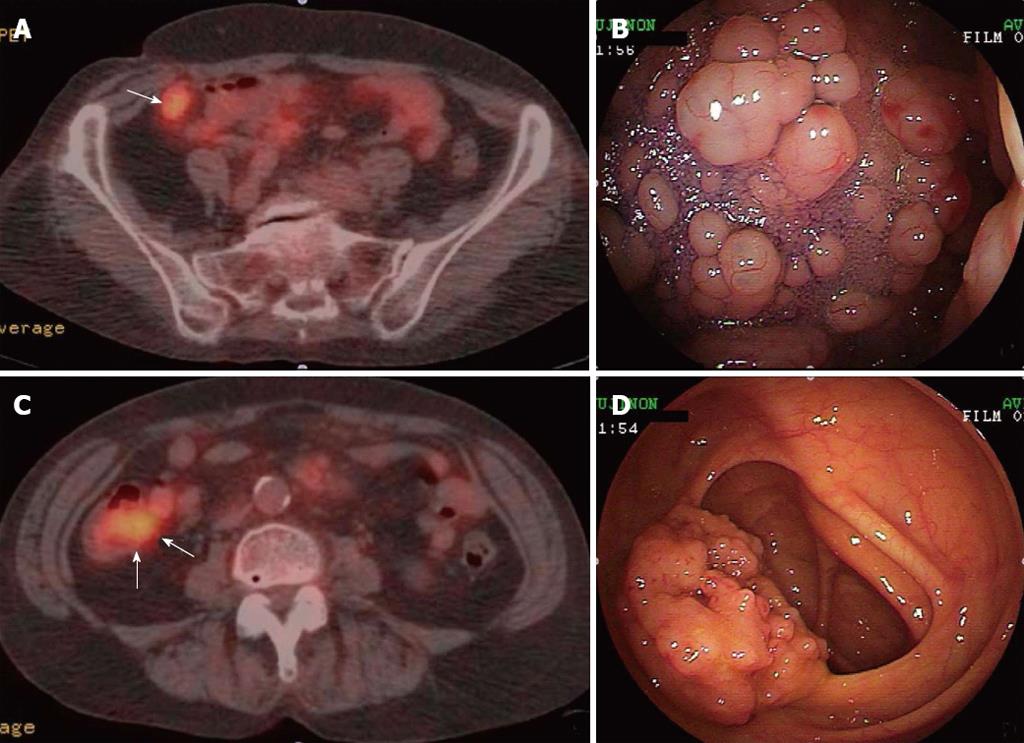
Case 3 is a 66-year-old woman who underwent EGD because of a 1-wk history of postprandial epigastric discomfort and dyspepsia. There were abnormal findings in the papillae of vater (Table 1). This case showed intestinal wall thickening with abnormal accumulation from the terminal ileum to the cecum by PET-CT (SUVmax, 6.73) (Figure 2A and C). The endoscopic findings in the duodenum included eruptions with mild swelling and erosion at the papillae of Vater. The jejunum and the ileum had sparse clusters of small nodules. Portions from the terminal ileum (Figure 2B) to the ileocecal valve (Figure 2D) had dense clusters of granules and nodules.
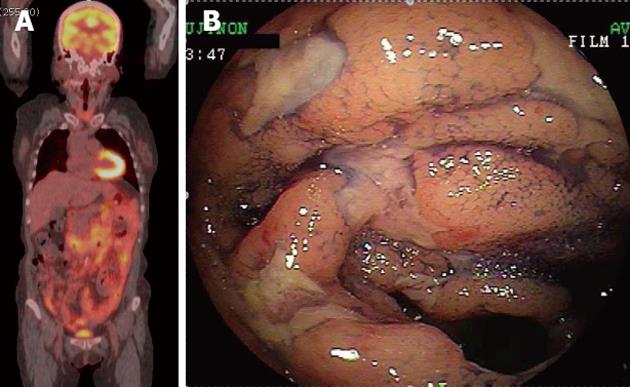
Case 4 is a 61-year-old woman undergoing examinations for leukocytosis (white blood cells, 29 740) (Table 1). The PET-CT of this patient showed abnormal accumulations (SUVmax, 5.6) in broad areas from the descending portion of the duodenum through the jejunum to the ileum (Figure 3A). The color of the duodenal bulb was normal, and the macroscopic finding was rough mucosa. The mucosa of the descending and horizontal portions of the duodenum showed clusters of numerous whitish granules. The jejunum and the ileum had multiple ulcers with irregular margins that occupied the whole lumen, with edematous change in broad areas of the mucosa (Figure 3B).
FL-GI patients frequently have duodenal and small intestinal lesions, as has been already reported[2]. The macroscopic findings of patient endoscopies that were also detected using PET-CT were clusters of numerous whitish granules spreading over the mucosa, concealing the folds, obvious swelling and thickening of folds and dense clusters of granules and nodules (Cases 1-3). PET-CT could detect lesions of ulcers with irregular margins that occupied the whole lumen with edematous mucosa as well as lesions with clusters of numerous whitish granules (Case 4). Lesions with a scattered distribution of whitish granules and small nodules were not shown as abnormal accumulations by PET-CT (Cases 1 and 3). It is assumed that a greater wall thickness of a GI lesion results in a greater possibility of abnormal accumulation according to the PET-CT results.
There were 2 FL-GI patients with small intestinal tumors whose initial symptom was ileus (4.3% of FL-GI at our division in April 2012). PET-CT is a valuable tool for the detection of the lesions in these patients (PET-CT findings not shown). The detection rate of the GI lesions of FL by PET-CT is generally reported to be rather low[9,10]. However, among the gastrointestinal lesions that were detected by PET-CT were cases with wall thickening and macroscopic clusters of nodules, dense clusters of whitish granules or small nodules, fold thickening or ulcers that showed irregular margins and occupied the whole lumen with edematous mucosa. Therefore, PET-CT is useful in cases with lesions that are difficult to approach using DBE and in cases that have a risk of retention with VCE because of stenosis due to tumors or wall thickening of the deep portion of small intestine. PET-CT is a useful tool for detecting the involvement of lymph nodes and other organs in follicular lymphoma[3]. It is not only useful for deciding whether VCE should be performed, but also for deciding the method by which lesions in the small intestine are approached using DBE, which is necessary for the pathological diagnosis of the biopsy.
P- Reviewers Bendandi M, Seto M S- Editor Gou SX L- Editor A E- Editor Xiong L
| 1. | Tari A, Asaoku H, Kunihiro M, Tanaka S, Fujihara M, Yoshino T. Clinical features of gastrointestinal follicular lymphoma: comparison with nodal follicular lymphoma and gastrointestinal MALT lymphoma. Digestion. 2011;83:191-197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 2. | Takata K, Okada H, Ohmiya N, Nakamura S, Kitadai Y, Tari A, Akamatsu T, Kawai H, Tanaka S, Araki H. Primary gastrointestinal follicular lymphoma involving the duodenal second portion is a distinct entity: a multicenter, retrospective analysis in Japan. Cancer Sci. 2011;102:1532-1536. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 109] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 3. | Bendandi M. Aiming at a curative strategy for follicular lymphoma. CA Cancer J Clin. 2008;58:305-317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 30] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 4. | Akamatsu T, Kaneko Y, Ota H, Miyabayashi H, Arakura N, Tanaka E. Usefulness of double balloon enteroscopy and video capsule endoscopy for the diagnosis and management of primary follicular lymphoma of the gastrointestinal tract in its early stages. Dig Endosc. 2010;22:33-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 24] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 5. | Hofman MS, Hicks RJ. Imaging in follicular NHL. Best Pract Res Clin Haematol. 2011;24:165-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 6. | Rohatiner A, d’Amore F, Coiffier B, Crowther D, Gospodarowicz M, Isaacson P, Lister TA, Norton A, Salem P, Shipp M. Report on a workshop convened to discuss the pathological and staging classifications of gastrointestinal tract lymphoma. Ann Oncol. 1994;5:397-400. [PubMed] |
| 7. | Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, Thiele J, Vardiman JW. WHO classifications of tumors of Haematopoietic and Lymphoid Tissues. Lyon: IARC Press 2008; . |
| 8. | Solal-Céligny P, Roy P, Colombat P, White J, Armitage JO, Arranz-Saez R, Au WY, Bellei M, Brice P, Caballero D. Follicular lymphoma international prognostic index. Blood. 2004;104:1258-1265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1289] [Cited by in RCA: 1294] [Article Influence: 61.6] [Reference Citation Analysis (0)] |
| 9. | Hoffmann M, Chott A, Püspök A, Jäger U, Kletter K, Raderer M. 18F-fluorodeoxyglucose positron emission tomography (18F-FDG-PET) does not visualize follicular lymphoma of the duodenum. Ann Hematol. 2004;83:276-278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | Higuchi N, Sumida Y, Nakamura K, Itaba S, Yoshinaga S, Mizutani T, Honda K, Taki K, Murao H, Ogino H. Impact of double-balloon endoscopy on the diagnosis of jejunoileal involvement in primary intestinal follicular lymphomas: a case series. Endoscopy. 2009;41:175-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 27] [Article Influence: 1.7] [Reference Citation Analysis (1)] |