Published online Feb 21, 2012. doi: 10.3748/wjg.v18.i7.692
Revised: April 26, 2011
Accepted: May 2, 2011
Published online: February 21, 2012
AIM: To evaluate the clinical impact of multidetector computed tomography (MDCT) before double-balloon endoscopy (DBE) for patients with obscure gastrointestinal bleeding (OGIB).
METHODS: A retrospective analysis of prospectively collected cases with DBE and MDCT for overt OGIB was conducted from April 2004 to April 2010 at Changhua Christian Hospital. We evaluated the clinical impact of MDCT on the subsequent DBE examinations and the diagnostic yields of both MDCT and DBE respectively.
RESULTS: From April 2004 to April 2010, a total of 75 patients underwent DBE for overt OGIB. Thirty one cases received MDCT followed by DBE for OGIB. The overall diagnostic yields of DBE and MDCT was 93.5% and 45.2%. The MDCT had a high diagnostic yield of tumor vs non-tumor etiology of OGIB (85.7% vs 33.3%, P = 0.014). Additionally, the choice of initial route of DBE was correct in those with a positive MDCT vs negative MDCT (100% vs 52.9%, P = 0.003).
CONCLUSION: This study suggests MDCT as a triage tool may identify patients who will benefit from DBE and aid the endoscopist in choosing the most efficient route.
- Citation: Yen HH, Chen YY, Yang CW, Liu CK, Soon MS. Clinical impact of multidetector computed tomography before double-balloon enteroscopy for obscure gastrointestinal bleeding. World J Gastroenterol 2012; 18(7): 692-697
- URL: https://www.wjgnet.com/1007-9327/full/v18/i7/692.htm
- DOI: https://dx.doi.org/10.3748/wjg.v18.i7.692
Obscure gastrointestinal bleeding (OGIB) is defined by the American Gastroenterological Association (AGA)[1] as bleeding of unknown cause after upper or lower endoscopy. OGIB constitutes approximately 5% of patients evaluated for gastrointestinal hemorrhage[2]. OGIB can be further classified into two clinical forms: (1) obscure-occult bleeding; and (2) obscure-overt type bleeding (those with hematochezia or melena). The management of overt OGIB is clinically challenging for the gastroenterologist. With the introduction of high yield diagnostic tools such as capsule endoscopy (CE) and double-balloon endoscopy (DBE) since the year 2000, the AGA recommended the use of CE followed by DBE as the first line diagnostic tool in 2007[2]. CE has exhibited some limitations, such as capsule retention, incomplete examination, inability to provide therapy, and high cost[3]. Compared with CE, DBE offered a therapeutic ability which is more useful in the setting of overt OGIB and is cost-effective compared with CE[4]. Multidetector computed tomography (MDCT) is a non-invasive tool and some recent reports have used it to investigate OGIB[3,5-7]. The clinical impact of MDCT prior to DBE for OGIB has not been evaluated. Thus, we performed this study to evaluate, retrospectively, the role of MDCT and DBE in patients with OGIB.
A retrospective review of the medical records of Changhua Christian hospital from April 2004 to April 2010 identified 75 patients who underwent DBE for OGIB. A retrospective analysis of this prospectively collected database of DBE identified 31 patients who received MDCT within one month prior to DBE for obscure overt gastrointestinal (GI) bleeding and were included for this analysis. OGIB was defined as gastrointestinal bleeding after a non-diagnostic upper and lower endoscopy. All patients provided written consent to undergo MDCT and endoscopy, including endoscopic treatments, such as hemoclip and argon plasma coagulation. All patients were informed that endoscopic examination and treatment are involved in the current standard therapeutic approach used in the evaluation of OGIB. The primary end point of the study was to evaluate the clinical impact of MDCT on the subsequent DBE examinations. The secondary end point of the study was the diagnostic yield for MDCT and DBE for the diagnosis of OGIB.
All the patients received MDCT with non-enhanced and triphasic helical computed tomography (CT) scanning[8]. No oral contrast material was given before the examination. First, patients were imaged with a MDCT scanner (LightSpeed Ultra 16, GE Medical Systems, Milwaukee, WI) in a craniocaudal direction beginning at the dome of the liver. A nonionic contrast medium (Optiray 350, Tyco Healthcare, Mansfield, MA) was then administered at a total dose of 100 to 120 mL with an injection rate of 3 mL/s through an antecubital vein. For triphasic acquisitions, scanning was started with a 10 s scan delay for the hepatic arterial phase after the attenuation value of the aorta reached 120 HU. Fifteen seconds after the end point of the hepatic arterial phase, the scans for the portal venous phase were acquired. Delayed-phase images were acquired 80 s after the end of the acquisition of the portal venous phase. Whole scanning was completed in 4 to 8 s with the patients holding their breath.
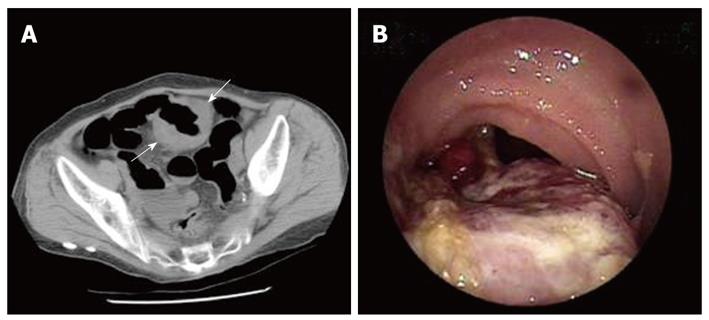
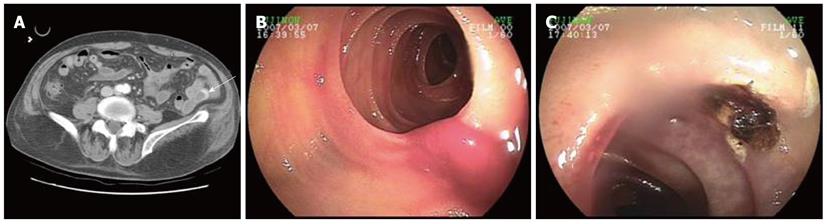
The MDCT was reviewed by one radiologist (Dr. Liu) with 10 years of experience with abdominal imaging. The finding of the presence of small intestinal neoplasm (Figure 1), active contrast extravasation (Figure 2) or hyperdense fluid accumulation was considered to be diagnostic of GI bleeding[9].
The double-balloon method was developed as described by Yamamoto et al[10]. Briefly, the double-balloon endoscope (EN-450P5 or EN-450T5, Fujinon Co., Japan) had two balloons, one attached to the distal end of the scope and the other attached to a transparent overtube (length 140 cm). Through a technique of inflating and deflating the balloons, the 7 m long small intestine can be shrunk to less than 2 m. Therefore, the entire small intestine could be theoretically examined. Fluoroscopy was required to guide the insertion or withdrawal of the endoscope. An oral route or anal route was chosen depending on clinical suspicion of the lesion. The endoscopic examination was stopped when (1) a lesion was found; (2) the endoscope was unable to be inserted or (3) due to patient intolerance. All the patients were admitted and received conscious sedation with intravenous midazolam and meperidine. During the procedure, the patients were monitored with an oximeter, EKG, and blood pressure monitor. Oxygen via nasal cannula was provided, as necessary.
All data were analyzed with SPSS 16.0. All quantitative data were expressed as mean ± SD. The χ2 test was used to compare two categorical data with P < 0.05 being considered statistically significant.
From 2004 to 2010, a total of 75 patients underwent DBE for OGIB and, of these, 31 patients were included in this analysis. These patients had a mean age of 68.6 years. Their mean hemoglobin levels were of 7.95 g/dL. Fourteen patients exhibited shock (defined as systolic blood pressure < 90 mmHg or drop of systolic pressure > 40 mmHg) during the presentation. The median time between the MDCT and DBE procedures was 2 d (range from 0 d to 12 d). The source attributed to OGIB was found in 93.5% of these 31 patients. Two patients had no diagnosis made after both DBE and CT examination and had no further bleeding during the follow-up period (Table 1).
| Item | Value |
| Sex (M/F) | 13/18 |
| Age (yr) | 68.6 ± 11.3 |
| Underlying diseases | |
| Hypertension | 23 (74.2) |
| DM | 4 (12.9) |
| Chronic renal failure | 5 (16.1) |
| Cirrhosis | 2 (6.5) |
| Abdominal operation | 1 (3.2) |
| NSAID/aspirin use | 9 (29.0) |
| Hemoglobin level (g/dL) | 7.95 ± 1.62 |
| Hospital stay (d) | 12.8 ± 10.8 |
| Shock at presentation | 14 (45.2) |
| Median time between DBE and MDCT (d) | 2 (0-12) |
| Final diagnosis | |
| Ulcers | 7 |
| Tumors | 7 |
| Angiodysplasia | 2 |
| Diverticulosis | 10 |
| Lymphangiectasia | 1 |
| Undiagnosed | 2 |
The overall diagnostic yield of DBE was 93.5% and CT was 45.2%. The diagnostic yield of CT depends on the etiology: 100% (2/2) of bleeding angiodysplasia, 85.7% (6/7) of those had bleeding from tumors, 41.7% (5/12) of those from diverticulosis, 14.3% (1/7) of those from ulcers and 0% of those from lymphangiectasia (0/1). One patient had early colon cancer diagnosed by DBE, though missed by CT. The MDCT diagnostic yields were not different according to the hospital stay, shock status, hemoglobin levels and timeframe between presentations to MDCT. The diagnostic yield of MDCT is high compared to the bleeders from tumor vs non-tumor (ulcerative or angiogenic cause) origin (85.7% vs 33.3%, P = 0.014) (Table 2).
| Final diagnosis | DBE positive | MDCT positive | Total |
| Ulcers | 7 | 1 | 7 |
| Tumors | 7 | 6 | 7 |
| Angiodysplasia | 2 | 2 | 2 |
| Diverticulosis | 12 | 5 | 12 |
| Lymphangiectasia | 1 | 0 | 1 |
| Undiagnosed | 0 | 0 | 2 |
| Diagnostic yield | 29 (93.5) | 14 (45.2) | 31 |
The choice of initial route of DBE examination (for example, oral route or anal route) depended on the clinical suspicion of the lesion by the endoscopist. If previous imaging studies suggested the location of bleeding, the nearest route was chosen; if the patient had a history of hematemesis or tarry stool passage, the oral route was chosen; if the patient had bloody stool passage, the anal route was chosen. Our patients received DBE via oral route only (n = 18), anal route only (n = 4), and both routes (n = 9). Among the 14 cases with a positive CT, the initial route of DBE was correct in all 14 cases. Among those 17 patients with a negative CT, the initial route of DBE was correct in 9 cases. A positive CT led to a correct choice of the route of DBE compared with a negative CT (100% vs 52.9%, P = 0.003) (Table 3).
| Route choice right | Route choice wrong | |
| Positive CT | 14 | 0 |
| Negative CT | 9 | 8 |
| Pearson’s χ2 = 8.88, P = 0.003 |
The current suggested investigation into OGIB includes CE and DBE by the AGA in 2007[2]. Both methods have a variable diagnostic yield from 36% to 80%[2]. CE is non-invasive but has some limitations, such as capsule retention and incomplete examination[3]. Compared with CE, DBE is more invasive but offers therapeutic ability[4]. Unlike routine endoscopy, performing DBE is technically demanding and usually requires a two-physician team[11]. An initial approach with CE followed by DBE is ideal for patients with OGIB, but is not cost-effective[12]. Both procedures are expensive and not reimbursed by insurance in Taiwan. By contrast, MDCT is a non-invasive tool and had been used to evaluate OGIB[3,5-7]. In our previous reports[9,13,14], we determined that MDCT is particularly useful to localize the bleeding for subsequent endoscopy in the setting of active GI bleeding. MDCT is reimbursed by our insurance and is more readily available; therefore, approaching OGIB patients with initial MDCT followed by DBE was suggested as an alternative to the current AGA recommendation[2] in our institution since the introduction of DBE[15]. There are few studies that compare CE and MDCT in the management of OGIB[6,16]. In Zhang’s report[16], the combination of MDCT with CE was not superior to CE alone in the diagnosis of OGIB. However, data regarding the role of MDCT before DBE in the setting of OGIB is lacking. Only one study from Chen et al[17] involving 70 patients suggested the usefulness of MDCT combined with DBE in the assessment of small bowel diseases. Thus, we performed this study to evaluate the role of MDCT prior to DBE in our institution during a 6-year-period.
In our study, we found DBE had higher diagnostic yield compared with MDCT (93.5% vs 45.2%) for OGIB. Both the diagnostic yield of DBE[2] and MDCT[3,5-7] are comparable to previous literature. Most of our patients exhibited severe GI bleeding (45.2% of shock at presentation), accounting for our high diagnostic yield. In this study, we discovered that MDCT is useful in two ways. Firstly, MDCT has a high diagnostic yield of small intestinal neoplasm compared with other non-tumor origins (ulcerative or angiogenic cause). Among seven patients with a tumor origin accounting for their OGIB, six patients were finally diagnosed to have small bowel tumors and all were diagnosed by MDCT prior to DBE procedure. The failure to diagnose one case of early colon cancer in the study can be explained by the fact that our MDCT protocol did not involve bowel preparation or optimal for colonic examination. The reported diagnostic rate of MDCT for small bowel neoplasm ranges from 67.4%[16] to 100%[5]. This is particularly useful in the management of patients with OGIB. In two recent large DBE series[18,19], patients with diagnosed neoplasm mostly benefited from the DBE due to the ability for long-term control of bleeding either endoscopically or surgically. By contrast, while a diagnosis of ulcer or vascular lesion was identified, only 40%[18,19] of the patients remained free of recurrent bleeding. Thus, the high diagnostic yield of MDCT for small bowel neoplasm allowed the clinician to identify patients that would most benefit from subsequent DBE procedures.
Secondly, in patients with positive MDCT, the choice of initial route of DBE examination was more likely to be correct compared to a negative MDCT (100% vs 52.9%, P = 0.003). As DBE usually requires examination via either the oral or anal route, the choice of correct insertion route of DBE is critical for allowing rapid approaches to the bleeding[20]. No recommended standard for selection of the insertion route of DBE currently exists. Although clinical presentation such as hematesis and stool color are useful for the endoscopist to choose the route of insertion, the initial route of DBE is not reliable, especially in the setting of massive bleeding[20]. Few studies[20,21] have utilized the finding of CE to guide the insertion route of subsequent DBE. In our study, we demonstrated that a positive MDCT is useful for guiding the insertion route of subsequent DBE.
Several methods of MDCT are described in the literature, including MDCT with oral saline as a contrast[16,22] or multi-phase CT-enterography[3,5,7]. The reported diagnostic yield for OGIB ranges from 30%[16] to 83%[22] with different MDCT protocols. No comparative study comparing the diagnostic yield of different CT protocols exists. In our institution, the triphasic MDCT protocol without oral contrast[8] utilized in our institution demonstrates a similar diagnostic yield as compared with previous reports. Although the use of fluid contrast can distend the intestinal lumen effectively and increase the diagnostic ability, especially for mucosal lesions[3,16,22], this may delay the subsequent DBE examination. In our institution, an emergent MDCT can be arranged as quickly as 2 h after a non-diagnostic endoscopy. If previous endoscopic studies suggested bleeding in the small bowel, the endoscopist would withdraw the endoscope without air suction, which leaves air in the bowel as a contrast (Figure 1). This approach is simple and similar to the recently described virtual enteroscopy[23]. Via this approach, once MDCT is positive, a DBE can be arranged early without the need to wait for gastric emptying due to the use of an oral fluid contrast.
This study has some limitations. The first is in the retrospective nature of the study. Although CE or DBE are recommended for the diagnosis of OGIB[24], both of these procedures are expensive and neither is covered by health insurance providers in our region. In addition, MDCT is more readily available compared with CE and DBE and less invasive than conventional angiography. Thus, MDCT is used as the diagnostic and triage tool of choice for OGIB at our institution[9]. Therefore, our findings of the high diagnostic yields of both DBE and MDCT may be an overestimation because some patients with small intestinal tumors or those who have self-limited bleeding may not undergo subsequent DBE and were not included in this analysis. Secondly, the use of MDCT still has some disadvantages[4]. The procedure results in substantial radiation exposure and carries the risk of contrast nephrotoxicity that may limit its use in elderly patients, who constitute the main population of OGIB patients.
Our study demonstrates that MDCT provides a reasonable diagnostic yield for OGIB in comparison with previous reports[3,7,16,22]. The use of MDCT as a triage tool prior to DBE may aid the endoscopist in identifying patients who will benefit from the examination, and may aid the endoscopist in choosing the most efficient route of DBE examination. However, our study is limited to a retrospective nature and only a small number of patients were enrolled in this study. Further prospective studies with more patients are required to confirm our observation.
Capsule endoscopy followed by double-balloon endoscopy is the current standard approach for obscure gastrointestinal bleeding. Multidetector computed tomography (MDCT) has been used recently to investigate obscure gastrointestinal bleeding, but its role in current standard approach to obscure gastrointestinal bleeding (OGIB) has not been evaluated.
This study analyzed the clinical impact of MDCT in a subset of patients with OGIB in a single medical center.
This study is novel in that the researchers analyzed the clinical utility of MDCT before double-balloon enteroscopy (DBE) for the indication of OGIB.
MDCT provides a reasonable diagnostic yield in this study. The use of MDCT as a triage tool prior to DBE may aid the endoscopist in identifying patients who will benefit from the examination and may aid the endoscopist in choosing the most efficient route of DBE examination.
The authors demonstrated that MDCT may provide a reasonable diagnostic yield in a select group of patients with OGIB by a retrospective study.
Peer reviewer: Yuji Naito, Professor, Kyoto Prefectural University of Medicine, Kamigyo-ku, Kyoto 602-8566, Japan
S- Editor Sun H L- Editor Rutherford A E- Editor Zheng XM
| 1. | Zuckerman GR, Prakash C, Askin MP, Lewis BS. AGA technical review on the evaluation and management of occult and obscure gastrointestinal bleeding. Gastroenterology. 2000;118:201-221. [PubMed] |
| 2. | Raju GS, Gerson L, Das A, Lewis B. American Gastroenterological Association (AGA) Institute medical position statement on obscure gastrointestinal bleeding. Gastroenterology. 2007;133:1694-1696. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 159] [Cited by in RCA: 160] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 3. | Huprich JE. Multi-phase CT enterography in obscure GI bleeding. Abdom Imaging. 2009;34:303-309. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 19] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 4. | Graça BM, Freire PA, Brito JB, Ilharco JM, Carvalheiro VM, Caseiro-Alves F. Gastroenterologic and radiologic approach to obscure gastrointestinal bleeding: how, why, and when? Radiographics. 2010;30:235-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 58] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 5. | Huprich JE, Fletcher JG, Alexander JA, Fidler JL, Burton SS, McCullough CH. Obscure gastrointestinal bleeding: evaluation with 64-section multiphase CT enterography--initial experience. Radiology. 2008;246:562-571. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 110] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 6. | Filippone A, Cianci R, Milano A, Valeriano S, Di Mizio V, Storto ML. Obscure gastrointestinal bleeding and small bowel pathology: comparison between wireless capsule endoscopy and multidetector-row CT enteroclysis. Abdom Imaging. 2008;33:398-406. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 36] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 7. | Hara AK, Walker FB, Silva AC, Leighton JA. Preliminary estimate of triphasic CT enterography performance in hemodynamically stable patients with suspected gastrointestinal bleeding. AJR Am J Roentgenol. 2009;193:1252-1260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 47] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 8. | Liu CK, Chou CT, Tung TH, Li MC, Wu HK, Lee KW. The role of multi-detector CT as preoperative assessment of hypervascular hepatocellular carcinoma compared with digital subtraction angiography. Zhonghua Fangshexue Zazhi. 2006;31:215-220. |
| 9. | Yen HH, Chen YY, Yang CW, Soon MS. The clinical significance of jejunal diverticular disease diagnosed by double-balloon enteroscopy for obscure gastrointestinal bleeding. Dig Dis Sci. 2010;55:3473-3478. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | Yamamoto H, Sekine Y, Sato Y, Higashizawa T, Miyata T, Iino S, Ido K, Sugano K. Total enteroscopy with a nonsurgical steerable double-balloon method. Gastrointest Endosc. 2001;53:216-220 doi: S0016510701525390 [pii]]. |
| 11. | Mehdizadeh S, Ross A, Gerson L, Leighton J, Chen A, Schembre D, Chen G, Semrad C, Kamal A, Harrison EM. What is the learning curve associated with double-balloon enteroscopy? Technical details and early experience in 6 U.S. tertiary care centers. Gastrointest Endosc. 2006;64:740-750. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 207] [Cited by in RCA: 198] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 12. | Gerson L, Kamal A. Cost-effectiveness analysis of management strategies for obscure GI bleeding. Gastrointest Endosc. 2008;68:920-936. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 88] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 13. | Chen YY, Soon MS, Yen HH, Wu HK. A life-threatening complication of a life-saving manoeuvre. Gut. 2007;56:364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 14. | Yen HH, Chen YY, Soon MS. Double-balloon enteroscopic treatment for bleeding jejunal diverticulum. Gastrointest Endosc. 2008;68:371-32; discussion 372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | Su WW, Yen HH, Chen YY, Hsu YC, Soon MS. Double-balloon enteroscopy: one year experience. Taiwan Xiaohuaxue Zazhi. 2005;22:310-315. |
| 16. | Zhang BL, Jiang LL, Chen CX, Zhong BS, Li YM. Diagnosis of obscure gastrointestinal hemorrhage with capsule endoscopy in combination with multiple-detector computed tomography. J Gastroenterol Hepatol. 2010;25:75-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 27] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 17. | Chen LH, Cao HJ, Zhang H, Shan GD, Zhang BL, Jiang LL, Li L, Chen HT, Fang Y, Cheng Y. [Diagnostic values of double-balloon enteroscopy and abdominal computed tomography in small bowel disease]. Zhonghua Yi Xue Za Zhi. 2008;88:3305-3308. [PubMed] |
| 18. | Gerson LB, Batenic MA, Newsom SL, Ross A, Semrad CE. Long-term outcomes after double-balloon enteroscopy for obscure gastrointestinal bleeding. Clin Gastroenterol Hepatol. 2009;7:664-669. [PubMed] |
| 19. | Shinozaki S, Yamamoto H, Yano T, Sunada K, Miyata T, Hayashi Y, Arashiro M, Sugano K. Long-term outcome of patients with obscure gastrointestinal bleeding investigated by double-balloon endoscopy. Clin Gastroenterol Hepatol. 2010;8:151-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 97] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 20. | Nakamura M, Ohmiya N, Shirai O, Takenaka H, Morishima K, Miyahara R, Ando T, Watanabe O, Kawashima H, Itoh A. Route selection for double-balloon endoscopy, based on capsule transit time, in obscure gastrointestinal bleeding. J Gastroenterol. 2010;45:592-599. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 31] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 21. | Gay G, Delvaux M, Fassler I. Outcome of capsule endoscopy in determining indication and route for push-and-pull enteroscopy. Endoscopy. 2006;38:49-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 168] [Cited by in RCA: 150] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 22. | Heiss P, Zorger N, Hamer OW, Seitz J, Müller-Wille R, Koller M, Herold T, Schölmerich J, Feuerbach S, Wrede CE. Optimized multidetector computed tomographic protocol for the diagnosis of active obscure gastrointestinal bleeding: a feasibility study. J Comput Assist Tomogr. 2009;33:698-704. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 23. | Endo K, Utano K, Togashi K, Yano T, Lefor AT, Yamamoto H, Yasuda Y, Sugimoto H. Virtual enteroscopy using air as the contrast material: a preliminary feasibility study. Dig Endosc. 2010;22:205-210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 24. | Yano T, Yamamoto H. Current state of double balloon endoscopy: the latest approach to small intestinal diseases. J Gastroenterol Hepatol. 2009;24:185-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 29] [Article Influence: 1.8] [Reference Citation Analysis (0)] |