Published online Feb 14, 2012. doi: 10.3748/wjg.v18.i6.583
Revised: September 12, 2011
Accepted: October 27, 2011
Published online: February 14, 2012
Acute pancreatitis is an inflammatory disease characterized by local tissue injury which can trigger a systemic inflammatory response. So vascular complications of pancreatitis are a major cause of morbidity and mortality. Pulmonary embolism in acute pancreatitis has been reported to be very rare. We reported a case of pulmonary embolism with acute pancreatitis. A 38-year-old woman broke out upper abdomen pain without definite inducement. She had no nausea and vomiting, fever, dyspnea, cough and expectoration, chest pain. The patient had been diagnosed with acute pancreatitis in local hospital. The patient was treated with antibiotics and proton pump inhibitors, and the abdomen pain was alleviated slightly. But the patient came forth cough and expectoration with a little blood, progressive dyspnea. A computed tomographic scan of the abdomen revealed pancreatitis. Subsequent computer tomography angiography of chest revealed pulmonary embolism (both down pulmonary arteries, left pulmonary artery and branch of right pulmonary artery). Dyspnea of the patient got well with thrombolytic treatment and anticoagulation therapy. Pulmonary embolism is a rare but potentially lethal complication of pancreatitis. Familiarity with this complication will aid in its early diagnosis, therapy and prevent pulmonary embolism, a rare but catastrophic phenomenon.
- Citation: Zhang Q, Zhang QX, Tan XP, Wang WZ, He CH, Xu L, Huang XX. Pulmonary embolism with acute pancreatitis: A case report and literature review. World J Gastroenterol 2012; 18(6): 583-586
- URL: https://www.wjgnet.com/1007-9327/full/v18/i6/583.htm
- DOI: https://dx.doi.org/10.3748/wjg.v18.i6.583
Pulmonary embolism (PE) is a blockage of the main artery of the lung or one of its branches by a substance that has travelled from elsewhere in the body through the bloodstream (embolism). Usually this is due to embolism of a thrombus (blood clot) from the deep veins in the legs, a process termed venous thromboembolism. A small proportion is due to the embolization of air, fat, talc in drugs of intravenous drug abusers or amniotic fluid. Untreated, PE has a mortality rate of approximately 30%.
Vascular complications of pancreatitis are a major cause of morbidity and mortality and are related to haemorrhage resulting from arterial erosion or pseudoaneurysms, ischaemic complications (either “local” or related to remote vascular events) and venous or arterial complications - specifically splanchnic thrombosis and associated varices[1-3]. The frequency of pulmonary embolism in acute pancreatitis has been reported to be very rare. The thrombohemorrhagic complications in pancreatitis are playing a tremendous part in the development of its most severe forms and fatal outcome. So we described a case of pulmonary embolism with acute pancreatitis and reviewed the literature for the occurrence of this complication.
A 38-year-old woman broke out upper abdomen pain after engorgement. She had no nausea and vomiting, fever, dyspnea, cough and expectoration, chest pain. The patient had been diagnosed with acute pancreatitis in local hospital. The relevant laboratory findings on admission were: white blood cell (WBC) 12.71 × 109/L, red blood cell 3.65 × 1012/L, hemoglobin 109 g/L, platelets 100 × 109/L, blood amylase 1130 U/L, alanine aminotransferase 261 U/L, total bilirubin 33.9 μmol/L, lactate dehydrogenase 614 U/L, urea nitrogen 10.26 mmol/L, serum creatinine 149.3 mmol/L, serum potassium 3.9 mmol/L, serum calcium 1.89 mmol/L, fasting blood glucose 12.1 mmol/L, c-reactive protein 162 mg/L. The patient was treated with antibiotics and proton pump inhibitors, and the abdomen pain was alleviated slightly. But the patient came forth cough and expectoration with a little blood, progressive dyspnea. So the patient was transferred to our institution. We found the following signs with physical examination: The temperature was 36 °C, the breath rate was 30 breaths per minute, the heart rate was 120 beats per minute, the blood pressure was 90/60 mmHg. The patient had cyanopathy of lip, breathed rapidly. Coarse breath sounds were heard in whole lung, breath sounds were decreased in the bilateral low lung fields, moist rales were heard in bilateral lung. Cardiac examination revealed tachycardia of 120 beats per minute without pathological murmur. Abdomen was flat and soft. Tenderness was obvious in upper abdomen. There was no rebound tenderness on abdomen. Liver and spleen were untouched below the costal margin. Shifting dullness was negative. The remainder of the examination was unremarkable, with no clinical evidence of deep venous thrombosis.
Oxygen saturation of blood was 78% on room air, 82% on 4 L/min oxygen nasal cannula, and 89% with noninvasive ventilator. Laboratory evaluation showed a WBC count of 13.4 × 109/L, with otherwise normal complete blood count; normal basic metabolic panel results; and arterial blood gas measurements showed a pH of 7.30, PCO2 43.6 mmHg, PO2 68.4 mmHg, and bicarbonate 20.8 mEq/L on oxygen flow rate of 6 L/min face mask. Plasma dimerized plasmin fragment D (D-dimer) assay was > 500 μg/L. blood amylase was 850 U/L.
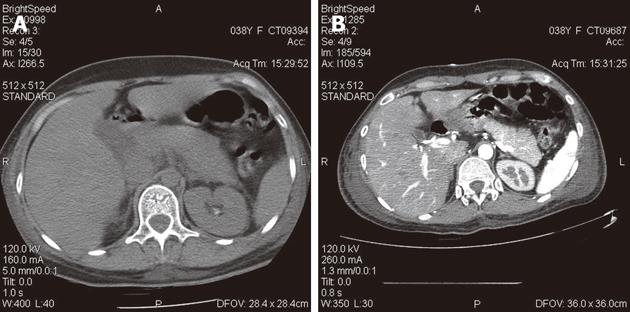
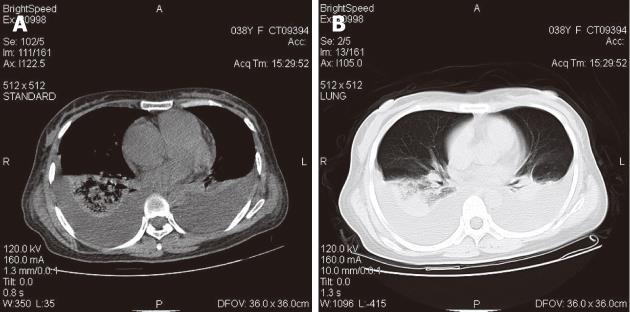
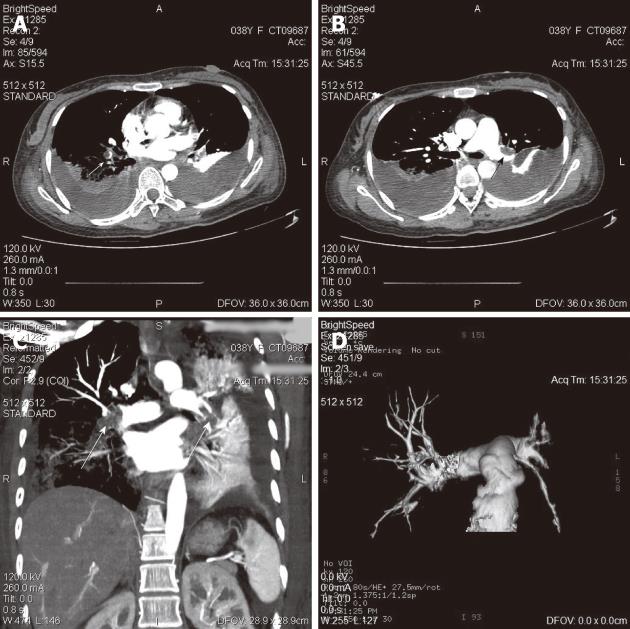
Electrocardiogram of the patient showed the sinus tachycardia and T-wave change. Doppler echocardiography revealed that right atrial was enlarged. There were no signs of celiac and pelvic vein thrombosis or proximal leg deep venous thrombosis with venous ultrasonography. A computed tomographic (CT) scan of the abdomen revealed pancreatitis (Figure 1). A CT scan of the chest revealed bilateral pleural effusion, lung infection and pulmonary hypertension (Figure 2). Subsequent computer tomography angiography of chest revealed pulmonary embolism (both down pulmonary arteries, left pulmonary artery and branch of right pulmonary artery) (Figure 3). Dyspnea of the patient got well with thrombolytic treatment and anticoagulation therapy.
Acute pancreatitis is an inflammatory disease characterized by local tissue injury which can trigger a systemic inflammatory response. There is increasing evidence that endothelial dysfunction is one of the critical pathophysiologic manifestations in patients with severe form of acute pancreatitis[1-4]. In keeping with this, we report the case of pulmonary embolism with acute pancreatitis. The case was reported for the reason: because pulmonary thrombus is a rare complication of pancreatitis.
Pulmonary embolism is a rare complication of pancreatitis, and there have been very few descriptions of it. Vascular thrombosis and hypercoagulable states complicating pancreatitis are thought to due to release of proteolytic enzymes from the pancreas and direct vasculitis. So some researchers consider the mechanism of formation of the pulmonary thrombus in the present case to be as follows: (1) a cyst communicating with the pancreatic duct penetrates into the vascular; (2) pancreatic juice enters the vascular and triggers the formation of a thrombus secondary to vasculitis; (3) hypercoagulability complicates pancreatitis and is thought due to a combination of hepatic dysfunction and hypertrypsinaemia (resulting in raised fibrinogen and Factor VIII concentrations) and cachexia; (4) vascular changes, due to proteolytic damage or inflammation, may also play a significant part; and (5) the acute pancreatitis provokes deleterious effects in endothelium-dependent relaxing response for ACh in isolated mesenteric rings that were strongly associated with high plasma NOx-levels as consequence of intense inflammatory responses. Furthermore, the subsensitivity of contractile response to phenylephrine in both mesenteric and pulmonary rings might be due to the complications of this pathological condition in the early stage of pancreatitis[5-7].
Pulmonary thromboembolism is a dreadful complication of vascular thrombosis in acute pancreatitis. Symptoms of pulmonary embolism include difficulty breathing, chest pain on inspiration, and palpitations. Clinical signs include low blood oxygen saturation and cyanosis, rapid breathing, and a rapid heart rate. Severe cases of PE can lead to collapse, abnormally low blood pressure, and sudden death. Diagnosis is based on these clinical findings in combination with laboratory tests (such as the D-dimer test) and imaging studies. So virtually all radiological modalities have been applied to the diagnosis of vascular thrombosis in acute pancreatitis. Contrast venography, ultrasonography, contrast-enhanced CT scan and magnetic resonance imaging (MRI) all have defined roles in the diagnosis of vascular thrombosis. Radionuclide 99mTc-venography and lung perfusion scintigraphy are useful in diagnosing pulmonary thromboembolism secondary to vascular thrombosis in pancreatitis, showing abnormal large hot spots at the level of the pancreas and pulmonary embolism[2,8,9].
Early recognition and investigation of thromboembolism is imperative because accurate diagnosis and timely radiological interventional procedures can reduce mortality. Early treatment with intravenous heparin is effective. A vascular filter is sometimes used in the management of vascular thrombosis in acute pancreatitis to prevent pulmonary thromboembolism[10-13].
This case report describes a rare complication of acute pancreatitis. Familiarity with this complication will aid in its early diagnosis, therapy and prevent pulmonary embolism, a rare but catastrophic phenomenon.
In conclusions, pulmonary thrombosis is a rare but potentially lethal complication of pancreatitis. Where the patient developing acute shortness of breath, or leg edema, superficial thrombophlebitis or thromboembolic events arouse clinical suspicion of vascular thrombosis, evaluation by CT scanning, MRI, radionuclide 99mTc-venography and lung perfusion scintigraphy is required. Early recognition and investigation of thromboembolism is imperative because accurate diagnosis and timely radiological interventional procedures can reduce mortality. Early treatment with intravenous heparin or thrombolysis is effective. Vascular filter insertion may be a life-saving measure for such patients.
Peer reviewers: Parimal Chowdhury, PhD, Professor, Department of Physiology and Biophysics, College of Medicine University of Arkansas for Medical Sciences, 4301 W Markham Street Little Rock, Arkansas 72205, United States; Seng-Kee Chuah, MD, Division of Hepatogastroenterology, Chang Kaohsiung Gang Memorial Hospital, 123, Ta-Pei Road, Niaosung Hsiang, Kaohsiung 833, Taiwan, China; Barjesh Chander Sharma, Professor, Department of Gastroenterology, G B Pant Hospital, New Delhi 110002, India
S- Editor Tian L L- Editor Ma JY E- Editor Xiong L
| 1. | Mendelson RM, Anderson J, Marshall M, Ramsay D. Vascular complications of pancreatitis. ANZ J Surg. 2005;75:1073-1079. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 89] [Article Influence: 4.7] [Reference Citation Analysis (1)] |
| 2. | Kirby JM, Vora P, Midia M, Rawlinson J. Vascular complications of pancreatitis: imaging and intervention. Cardiovasc Intervent Radiol. 2008;31:957-970. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 44] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 4. | Pastor CM, Matthay MA, Frossard JL. Pancreatitis-associated acute lung injury: new insights. Chest. 2003;124:2341-2351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 127] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 5. | Camargo EA, Delbin MA, Ferreira T, Landucci EC, Antunes E, Zanesco A. Influence of acute pancreatitis on the in vitro responsiveness of rat mesenteric and pulmonary arteries. BMC Gastroenterol. 2008;8:19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Piercy KT, Ayerdi J, Geary RL, Hansen KJ, Edwards MS. Acute pancreatitis: A complication associated with rheolytic mechanical thrombectomy of deep venous thrombosis. J Vasc Surg. 2006;44:1110-1113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Lungarella G, Gardi C, de Santi MM, Luzi P. Pulmonary vascular injury in pancreatitis: evidence for a major role played by pancreatic elastase. Exp Mol Pathol. 1985;42:44-59. [PubMed] |
| 8. | Ohta H, Hachiya T. A case of inferior vena cava thrombosis and pulmonary embolism secondary to acute exacerbation of chronic pancreatitis: a rare finding in radionuclide venography. Ann Nucl Med. 2002;16:147-149. [PubMed] |
| 9. | Ma SK, Kim SW, Kim NH, Choi KC. Renal vein and inferior vena cava thrombosis associated with acute pancreatitis. Nephron. 2002;92:475-477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Asanuma Y, Furuya T, Shibata S, Shioya T, Miura M, Koyama K. Postoperative acute pulmonary thromboembolism in patients with acute necrotizing pancreatitis with special reference to apheresis therapy. Ther Apher. 1998;2:199-204. [PubMed] |
| 11. | Balachandra S, Siriwardena AK. Systematic appraisal of the management of the major vascular complications of pancreatitis. Am J Surg. 2005;190:489-495. [PubMed] |
| 12. | Beattie GC, Hardman JG, Redhead D, Siriwardena AK. Evidence for a central role for selective mesenteric angiography in the management of the major vascular complications of pancreatitis. Am J Surg. 2003;185:96-102. [PubMed] |
| 13. | Jones AL, Ojar D, Redhead D, Proudfoot AT. Case report: Use of an IVC filter in the management of IVC thrombosis occurring as a complication of acute pancreatitis. Clin Radiol. 1998;53:462-464. [PubMed] |