INTRODUCTION
Since its first introduction in the 1990s, transjugular intrahepatic portosystemic shunt (TIPS) has played an increasingly important role in the management and treatment of the complications of portal hypertension (PH). Now, established indications for TIPS include active variceal hemorrhage not controlled by endoscopic and pharmacologic treatment (mainly from gastric and ectopic varices), secondary prevention of bleeding, refractory hydrothorax and ascites, Budd-Chiari and veno-occlusive syndrome, hepatopulmonary syndrome, hepatorenal syndrome, and prophylaxis of complications in patients with cirrhosis who need major abdominal surgery[1-3].
TIPS as a treatment for PH has been performed for > 20 years in our hospital. Five hundred cases of PH have been treated[4,5]. With improvement in the technical skills of interventional radiologists over time, technical complications such as abdominal bleeding, stent migration, hemobilia, and hepatic artery injury have become extremely rare[6,7]. This paper reports a case of delayed liver laceration 8 d after TIPS in a patient with PH.
CASE REPORT
A 45-year-old female patient was admitted to our institution because of hematemesis. She had a few years history of PH due to liver cirrhosis of unclear etiology, and had been hospitalized twice for gastrointestinal bleeding. On examination, she was emaciated and had moderate ascites requiring diuretic treatment. Endoscopy showed severe hypertensive gastropathy with severe esophageal and gastric varices (Figure 1). Abdominal computed tomography demonstrated a classical PH appearance with liver cirrhosis and splenomegaly (Figure 2A). Plain chest film showed left hydrothorax. Abnormal laboratory findings on admission were as follows: hemoglobin concentration, 71 g/L; platelet count, 3 × 1010/L. Child-Pugh class A and normal renal function are not laboratory findings and were not abnormal.
Figure 1 Gastroscopy showing severe esophageal and gastric varices.
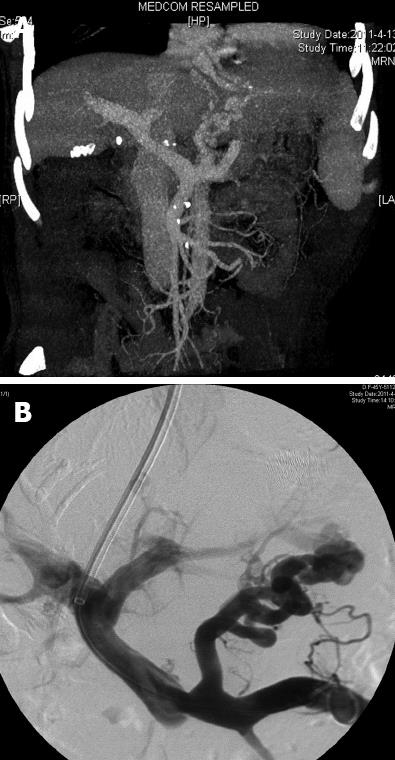
Figure 2 Portal venous-phase computed tomography and portal venography.
A: Portal venous-phase computed tomography showing classical appearance of portal hypertension with liver cirrhosis and splenomegaly; B: Portal venography showing the anatomy and direction of portal flow.
The TIPS procedure was performed according to the standard method under local anesthesia (1% lidocaine hydrochloride). After the right internal jugular vein was percutaneously punctured, a 10-Fr, 41-cm long sheath (Rösch-Uchida TIPS Puncture Set; Cook, Bloomington, IN, United States) was placed in the suprahepatic portion of the inferior vena. After catheterization of the right hepatic vein, measurement of hepatic venous pressure and portal puncture were performed. At no stage during attempted puncture of the portal vein was contrast agent seen to enter the hepatic arterial system, bile ducts, or peritoneal cavity. Portal venography was performed to evaluate the anatomy and determine the direction of portal flow (Figure 2B). With the use of a hydrophylic guide wire (Radiofocus guide wire; Terumo Europe, Leuven, Belgium), the portal vein was catheterized. The dilation of the intrahepatic parenchymal tract was performed using a low-profile balloon with 8 mm diameter. In this particular case with large varices of the gastric coronary vein, embolization using coils and gelatin sponge was performed to reduce the risk of rebleeding. Polytetrafluoroethylene (PTFE)-covered Fluency stent grafts (8 mm × 6 cm, manufactured by Angiomed GmbH Co., subsidiary of C.R. Bard, Murray Hill, NJ, United States) were used. After placement of the stents, portography was performed to ensure no contrast extravasation within the shunt, and the portal pressure was measured (Figure 3). The portosystemic gradient reduced from 50 to 34 cm H2O. The 5-Fr catheter should be routinely retained inside the portal vein through the right internal jugular vein after the procedure for the purpose of postoperative regional anticoagulation (heparin 4000 U/d) and re-examination.
Figure 3 Completion venography of transjugular intrahepatic portosystemic shunt showing good flow and no contrast extravasation.
Doppler ultrasound of the liver on d 1 and 7 following TIPS confirmed shunt patency and showed no evidence of liver parenchymal hemorrhage. The patient was transferred onto low molecular weight heparin (4100 U/d) and hepatoprotective drugs (such as magnesium isoglycyrrhizinate injection 200 mg/d, polyene phosphatidylcholine injection 930 mg/d, and ornithine aspartate injection 20 g/d), and made good clinical progress.
On d 8 following TIPS she developed sudden severe right upper abdominal pain, which did not significantly improve after analgesic treatment. Laboratory findings showed a drop in hemoglobin to 49 g/L, with deterioration of liver and coagulation function: serum alanine aminotransferase (ALT), 202 U/L; serum aspartate aminotransferase (AST), 300 U/L; total bilirubin, 38 μmol/L; prothrombin time, 22 s; and international normalized ratio, 1.8. At the same time, she developed clinical evidence of hypovolemic shock, with confusion, cool periphery, and systemic hypotension. Emergency ultrasound showed massive hemoperitoneum. The patient’s anticoagulation therapy was stopped, and vasoactive drugs were given to maintain blood pressure. The same day the patient was transferred to the intensive care unit due to hemorrhagic shock with an Acute Physiology and Chronic Health Evaluation II score of 17. A large volume of blood (about 1 L) was drained from the abdominal cavity by paracentesis. Exploratory laparotomy revealed massive hemoperitoneum (3 L). The active bleeding source was located in the liver parenchyma behind the gallbladder bed of the right hepatic lobe and was controlled with direct suturing and perihepatic packing. Erythrocyte suspension, 25 U, fresh frozen plasma, 2 L, platelet concentrate, 10 U, and cryoprecipitate, 20 U, were infused during and after surgery. The bleeding had ceased and the packs were removed after 6 d. However, postoperative liver dysfunction gradually appeared. Total bilirubin continued to increase, up to 505 μmol/L, but ALT and AST were normal (cholenzyme separation). Finally, she died of liver failure 23 d after TIPS.
DISCUSSION
Since the first clinical application was presented by Rössle et al[8] in 1989, TIPS has gained widespread popularity and has become the treatment of choice in many clinical scenarios for complications related to PH[9]. TIPS is an interventional radiology procedure that results in decompression of the splanchnic venous system in patients with PH by creating a low-resistance channel between an intrahepatic branch of the portal vein and a main hepatic vein[9]. When compared with endoscopic ligation and sclerotherapy, TIPS shows a significant advantage with respect to hemostasis (87% vs 45%, P = 0.03), rebleeding (31% vs 54%, P = 0.0005) and mortality (29% vs 48%, P = 0.05)[10]. TIPS is as effective as surgical shunting in preventing variceal bleeding and is also more cost-effective[11,12]. Evidence has now been provided that the use of TIPS at an early stage may represent a new perspective and improve the outcome and survival of high-risk bleeding patients selected by simple clinical prognostic indicators[13]. It has been reported that, in patients with Child-Pugh class C disease or class B disease with active bleeding who were admitted for acute variceal bleeding, the early use of TIPS with an e-PTFE covered stent was associated with significant reductions in failure to control bleeding, rebleeding, and mortality, with no increase in the risk of hepatic encephalopathy[14].
TIPS can markedly reduce portal pressure, but associated complications are also common. Direct procedure-related complication rates during TIPS have been reported in up to 20% of procedures[6]. Gaba et al[15] have conducted an in-depth discussion of complications and how to avoid TIPS-related operations in 2010. Freedman et al[6] have described a large series of TIPS complications, after analyzing TIPS procedures and complications at four American centers and reviewing the literature. They have reported that the most dangerous complications were related to transhepatic needle puncture, such as biliary duct injury, hemobilia, transcapsular tearing, arterial puncture, or portal venous rupture. In the event of such complications, direct surgical suture as well as local and perihepatic gauze packing can often effectively stop bleeding. However, if there has been uncontrollable bleeding despite repeated surgical interventions, postoperative evolution toward hepatic insufficiency (acute or progressive), and portal vein injuries that cannot be reconstructed, liver transplantation may be the only option to salvage the patient[16].
The current patient with decompensated liver cirrhosis was admitted to hospital with upper gastrointestinal bleeding. After adjustment of the liver and blood coagulation function, TIPS was performed to prevent variceal rebleeding. Routine anticoagulation with low molecular weight heparin was given in order to prevent early stent thrombosis and improve the stent patency rate. However, delayed liver laceration suddenly occurred 8 d after surgery. We consider that it may have been related to the following factors: (1) patients with liver cirrhosis suffer from coagulation disorders; (2) small blood vessels of liver parenchyma were damaged during the TIPS procedure; and (3) stent anticoagulation was given with low molecular weight heparin when thrombosis had not formed in a timely manner.
To the best of our knowledge, delayed liver laceration after TIPS has not been reported previously. There have been only three previous reports about late intrahepatic hematoma following TIPS, occurring in patients with Budd-Chiari syndrome (BCS). In each case the hematoma resolved with conservative management. It was considered that the cause of hematoma may have been related to the use of postoperative heparin[17].
With the introduction of the e-PTFE covered stent, the long-term patency of shunts has significantly improved[2,4,11,18]. Regular anticoagulation is given to prevent early shunt thrombosis through systemic or local application. A randomized study of anticoagulation following TIPS has reported reduced incidence of early thrombosis but no instances of intrahepatic hemorrhage, although this study comprised only 49 patients, 25 of whom stopped anticoagulation 3 d after TIPS[19].
Advanced cirrhosis is often accompanied by severe liver atrophy, rigidity of the liver, and enlargement of liver fissure. Anatomical variations of intrahepatic branches of the portal and hepatic veins affect the success rate of the puncture. This often requires repeated puncture or appropriate adjustments of the angle[20]. Many candidates for TIPS have cirrhosis and are more prone to arterial injuries because of enlargement and increased flow in the hepatic arteries. Therefore, multiple puncture and early postoperative anticoagulation may be an important risk factor for bleeding. So, early and timely examination has become an effective means of diagnosis and treatment of such complications. Some studies have reported that dynamic gadolinium-enhanced serial magnetic resonance examination may be useful to demonstrate and localize active bleeding, and if performed serially, may have the potential to quantify the rate of bleeding, which may potentially decrease the time needed to identify a site of hemorrhage during surgery[21].
In conclusion, delayed liver laceration is a rare but fatal complication of TIPS, which to date has not been reported in patients with PH. TIPS is increasingly accepted as an important management option for PH and other diseases such as BCS, therefore, this complication must be borne in mind. We advocate that careful attention to technique is vital to avoid complications. However, when complications do arise, the first step to stop bleeding is immediate imaging and secure local hemostasis with direct suturing and perihepatic gauze packing. If the bleeding does not stop, based on the clinical status and concomitant liver failure, liver transplantation may be necessary.
Peer reviewers: Michael A Fink, MBBS, FRACS, Department of Surgery, The University of Melbourne, Austin Hospital, Melbourne, Victoria 3084, Australia; Xiao-Ping Chen, Professor, Institute of Hepato-Pancreato-Biliary Surgery, Tongji Hospital, 1095 Jiefang Dadao, Wuhan 430030, Hubei Province, China
S- Editor Gou SX L- Editor Kerr C E- Editor Li JY