Published online Dec 28, 2012. doi: 10.3748/wjg.v18.i48.7341
Revised: July 18, 2012
Accepted: July 28, 2012
Published online: December 28, 2012
AIM: To compare early use of transjugular intrahepatic portosystemic shunt (TIPS) with endoscopic treatment (ET) for the prophylaxis of recurrent variceal bleeding.
METHODS: In-patient data were collected from 190 patients between January 2007 and June 2010 who suffured from variceal bleeding. Patients who were older than 75 years; previously received surgical treatment or endoscopic therapy for variceal bleeding; and complicated with hepatic encephalopathy or hepatic cancer, were excluded from this research. Thirty-five cases lost to follow-up were also excluded. Retrospective analysis was done in 126 eligible cases. Among them, 64 patients received TIPS (TIPS group) while 62 patients received endoscopic therapy (ET group). The relevant data were collected by patient review or telephone calls. The occurrence of rebleeding, hepatic encephalopathy or other complications, survival rate and cost of treatment were compared between the two groups.
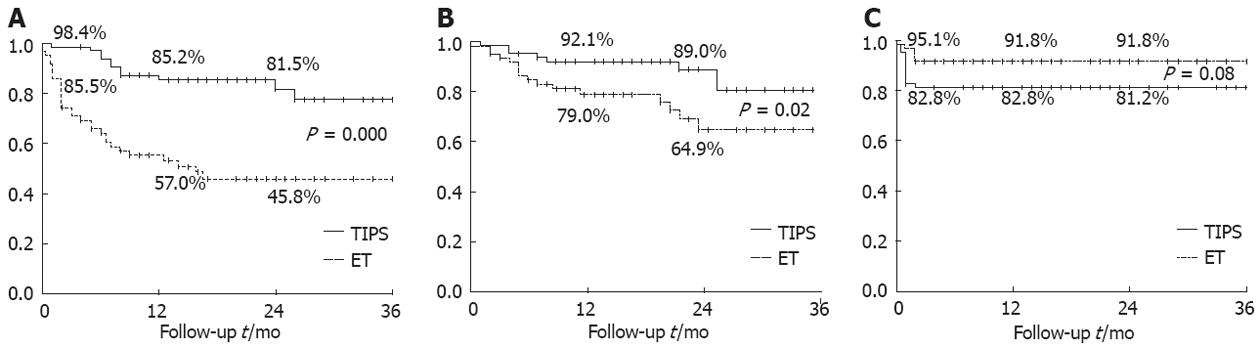
RESULTS: During the follow-up period (median, 20.7 and 18.7 mo in TIPS and ET groups, respectively), rebleeding from any source occurred in 11 patients in the TIPS group as compared with 31 patients in the ET group (Kaplan-Meier analysis and log-rank test, P = 0.000). Rebleeding rates at any time point (6 wk, 1 year and 2 year) in the TIPS group were lower than in the ET group (Bonferroni correction α’ = α/3). Eight patients in the TIPS group and 16 in the ET group died with the cumulative survival rates of 80.6% and 64.9% (Kaplan-Meier analysis and log-rank test χ2 = 4.864, P = 0.02), respectively. There was no significant difference between the two groups with respect to 6-wk survival rates (Bonferroni correction α’ = α/3). However, significant differences were observed between the two groups in the 1-year survival rates (92% and 79%) and the 2-year survival rates (89% and 64.9%) (Bonferroni correction α’ = α/3). No significant differences were observed between the two treatment groups in the occurrence of hepatic encephalopathy (12 patients in TIPS group and 5 in ET group, Kaplan-Meier analysis and log-rank test, χ2 = 3.103, P = 0.08). The average total cost for the TIPS group was higher than for ET group (Wilcxon-Mann Whitney test, 52 678 RMB vs 38 844 RMB, P < 0.05), but hospitalization frequency and hospital stay during follow-up period were lower (Wilcxon-Mann Whitney test, 0.4 d vs 1.3 d, P = 0.01; 5 d vs 19 d, P < 0.05).
CONCLUSION: Early use of TIPS is more effective than endoscopic treatment in preventing variceal rebleeding and improving survival rate, and does not increase occurrence of hepatic encephalopathy.
-
Citation: Xue H, Zhang M, Pang JX, Yan F, Li YC, Lv LS, Yuan J, Palikhe M, Li WZ, Wang ZL. Transjugular intrahepatic portosystemic shunt
vs endoscopic therapy in preventing variceal rebleeding. World J Gastroenterol 2012; 18(48): 7341-7347 - URL: https://www.wjgnet.com/1007-9327/full/v18/i48/7341.htm
- DOI: https://dx.doi.org/10.3748/wjg.v18.i48.7341
Esophagogastric varices bleeding (EGVB) is prone to be fatal, and often induces deterioration of liver function and may lead to bacterial infection, hepatorenal syndrome, or other complications.
Currently, the first-line treatments in prevention of variceal rebleeding include medication[1-3] and endoscopic therapy (ET)[4-6]. Transjugular intrahepatic portosystemic shunt (TIPS) is effective in preventing rebleeding, but due to post-operative stent stenosis and a high incidence of hepatic encephalopathy[7-11], this procedure is considered not superior to the conventional treatment in survival rate. Consequently, TIPS has been used only as a rescue approach after first-line treatment fails[12-14]. A large number of studies have shown that although TIPS can effectively control acute bleeding, it has a high mortality rate. Bare stents were used previously, but recently coated stents have been more commonly used, thus the clinical efficacy of TIPS must be re-evalulated[15-19]. Hence, in this study, through out-patient and telephone communication based follow-up, data of patients with upper gastrointestinal bleeding due to varices over the past three years who were managed in the Department of Gastroenterology, First Affiliated Hospital of Xi’an Jiaotong University, were collected. We compared TIPS with endoscopic surgery in the prevention of gastrointestinal rebleeding, improvement of survival rates and other aspects, in order to assess the feasibility, necessity and long-term efficacy of early implementation of the TIPS treatment.
Patients admitted to our hospital between January 2007 and June 2010 due to upper gastrointestinal bleeding resulting from varices who received TIPS or ET for the first time were included.
Inclusion criteria: (1) Age between 18 and 75 years; (2) liver cirrhosis confirmed by medical history, clinical manifestations and diagnostic imaging examinations; (3) liver function < 13 points according to Child score; (4) endoscopy confirmed bleeding due to esophageal varices before treatment; and (5) no endoscopic and interventional therapy or surgical treatment prior to admission.
Exclusion criteria: (1) A history of hepatocellular carcinoma (HCC) or malignant tumors of other organs; (2) severe organ dysfunction [heart failure, respiratory failure, moderate to severe jaundice (serum bilirubin > 3-5 mg/dL), hepatorenal syndrome or chronic renal insufficiency]; (3) hepatic encephalopathy stage ≥ second stage; and (4) ectopic variceal bleeding. The general information of the patients who were eligible for endoscopic therapy was obtained from the database at our endoscopy room. At the same time, the information of patients eligible for TIPS were obtained from the inpatient database.
All patients chose their treatment plans after they were informed of their conditions, and they were required to sign an informed consent for the special treatment they selected. Patients treated with TIPS (TIPS group) received either elective or immediate (in case of acute bleeding phase) interventional treatment. Patients with endoscopic treatment (ET group) were administered with endoscopic band ligation or tissue adhesive agent injection when their acute bleeding was controlled by medication or combined therapy with three-balloon catheters.
TIPS procedure: Catheters commonly used in TIPS included: RUPS-100, balloon dilatation catheter and guide wire, and the metal stent. Stents used in the procedures included bare metal stents (Luminexx, Codis or Zilver stents) of 8 mm and 10 mm in diameter, and coated stent (Fluency coated stent) with an average diameter of 8 mm. The right internal jugular vein was punctured under local anesthesia. Under X-ray monitoring, the guide wire was manipulated to the hepatic vein. A puncture needle was used to establish a pathway to the portal vein, which was then dilated with the balloon catheter. The stent was then put in place to complete the portal systemic shunting. Angiography was performed and if esophageal varice was still present, Corbra 2 cathter was delivered to the varicose vein. Ethanol or stainless steel ring was used to embolize the vein. Postoperative strategies included prevention of hepatic encephalopathy and infection, and heparin treatment for 1 wk, followed by oral intake of aspirin for 1-3 mo after discharge.
Endoscopic treatment: (1) Six-ligation devices (United States Wilson-Cook Company, Model: MBL-6-F) were used in endoscopic variceal ligation. Ligation started at the dentate line near the cardia (varicose vein bulging site) with a high density and a large number of ligating points. All varicose veins should be ligated. For some varicose veins, 2-3 ligations were done at different locations with bands. The procedure was repeated every two weeks until the varices disappeared or almost disappeared; (2) Endoscopic tissue adhesive injection was administered with the endoscopic sclerosis needle (Germany Ahmed Walker Medical Products Service Co., Ltd; Model: INJ1-A1-10.220), tissue adhesive [α-butyl cyanoacrylate ester; Kang Pat medical glue (embolic)], using sandwich technique.
Postoperative follow-up. All the patients were followed up by the outpatient department through telephone calls. Patients in the TIPS group were scheduled for check-ups at the outpatient department with portal vein Doppler ultrasound at 1 wk, 1 mo and 3 mo, and then every 6-12 mo after the surgery. Patients in the ET group received gastroscopy one mo after treatment, and then once every 3 mo until the 4th one was done. Follow-up continued for 3 years until February 2011. The goal of the follow-up was to check for rebleeding, and check for death, hepatic encephalopathy, and treatment-related complications. Data of repeated treatment, causes and frequency of re-hospitalization, and hospital costs were also evaluated at follow-up .
SPSS 13.0 software was used for statistical analysis. Continuous normally distributed variables were analyzed using two independent samples t test. Continuous non-normally distributed variables were analyzed using Wilcxon-Mann Whitney test. χ2 test or Fisher exact test was used for data measurement. Kaplan-Meier curve analysis was used analyze the occurence of rebleeding, hepatic encephalopathy as well as incidence of death. Log-rank test was used to compare the two methods of treatment regarding the differences in prognosis and outcome. Other prognostic variables, after being assigned by grading or quantification, were analyzed by Cox regression to evaluate the impact of covariates on the prognosis. P values were two-sided, and P < 0.05 was considered as statistically significant.
There was no significant difference in gender, age, cause of disease, clinical manifestations, liver function, endoscopic examination and laboratory indicators between the two groups, thus making the sample statistically comparable (Table 1).
| Characteristics | TIPS group | ET group | P value |
| (64 patients) | (62 patients) | ||
| Sex (n) | 0.80 | ||
| Male | 42 | 42 | |
| Female | 22 | 20 | |
| Age (yr) | 51 (± 13) | 54 (± 12 ) | 0.96 |
| Cases of disease (n) | 0.16 | ||
| HBV | 38 | 27 | |
| HCV | 8 | 10 | |
| Alcohol | 2 | 7 | |
| Other | 16 | 18 | |
| Endoscopic manifestions (n) | |||
| Varices classification | 1.00 | ||
| Severe | 62 | 61 | |
| Moderate | 2 | 1 | |
| Complicated with peptic unlcer | 4 | 3 | 1.00 |
| Complicated with gastric dieorders due to portal hypertension | 23 | 28 | 0.29 |
| Child classification (n) | 0.40 | ||
| A | 23 | 17 | |
| B | 30 | 29 | |
| C | 11 | 16 | |
| Child score | 7.0 (± 2.0 ) | 8.0 (± 2.0 ) | 0.99 |
| Preoperative manifestations (n) | |||
| Complicated with hepatic encephalopathy | 1 | 5 | 0.20 |
| Complicated with ascites | 39 | 38 | 0.97 |
| Compression using Sengstaken-Blakemore tube | 2 | 2 | 1.00 |
| Pre-operative laboratory parameters | |||
| Bilirubin (μmol/L) | 24.03 (± 12.71) | 27.94 (± 13.75) | 0.19 |
| Albumin (g/L) | 32.25 (± 5.03) | 30.85 (± 5.31) | 0.65 |
| PT (s) | 15.80 (± 3.80) | 16.30 (± 4.20) | 0.40 |
| Creatinine (μmol/L) | 72.80 (± 14.8) | 81.50 (± 31.00) | 0.21 |
In the TIPS group, 15 patients used 10-mm internal diameter stents, and the rest used 8 mm. Twenty-four patients used the Fluency coated stents, and the rest with bare stents. Thirty-three patients also underwent interventional embolization of esophageal varices during TIPS procedure. In the ET group, 44 patients were subjected to simple routine endoscopic variceal ligation, 13 were treated with endoscopic tissue adhesive injection, and the rest 5 patients were treated with the combined therapy. Ligations were made about 1-3 times per person (on average, 1.2 times per person); and one tissue adhesive injection was used on average.
The average follow-up was 20.7 ± 1.3 mo for the TIPS group, and 18.7 ± 1.3 mo for the ET group. Eleven cases in the TIPS group and 31 cases in ET group had gastrointestinal rebleeding. Kaplan-Meier analysis showed that there were significant differences in the overall rebleeding rates between the two groups (P = 0.000) (Figure 1A). Bonferroni correction showed that at week 6, month 12 and month 24 after operation, the occurrence of rebleeding was significantly lower in TIPS group than in ET group. Cox multivariate regression analysis showed that among the covariates (grouping variables, combined portal hypertensive gastropathy, gastroesophageal varice 2/isolated gastric varice 1, liver function with B/C grade, prothrombin time > 16 s and cirrhosis due to viral hepatitis), only grouping variable with TIPS therapy was a factor affecting the rate of rebleeding [TIPS treatment: B = -1.41; Exp (B) = 0.24, 95% confidence interval (CI) (0.12, 0.50); P = 0.001]. Of the 31 patients in ET group, 8 rebleeding patients received rescue TIPS treatment. Of those 8 patients, one patient, who used a bare stent, had rebleeding 10 mo later. Examination showed stent stenosis, and the patient received conservative treatment. One patient had massive gastrointestinal bleeding, resulting in death 14 mo after operation. No rebleeding occurred in the remaining 6 patients.
There were 8 deaths in TIPS group and 16 deaths in ET group. Kaplan-Meier survival analysis showed that the cumulative survival rate was significantly higher in the TIPS group than in the ET group (80.6% vs 64.9%, Kaplan-Meier analysis and log-rank test χ2 = 4.864, P = 0.02) (Figure 1B). Individual time point comparison showed that there was no significant difference 6 wk after operation between the two groups in survival rate; after 12 mo and 24 mo, the survival rate was significantly higher in the TIPS group than in the ET group (92% vs 79%; 89% vs 64.9%). Cox regression curves showed that the covariates [age > 53 years, with ascites, cirrhosis due to hepatitis, liver function with total bilirubin > 34 μmol/L, creatinine (CRE) > 77 μmol/L] age > 53 years, viral hepatitis (hepatitis B virus and hepatitis C virus) resulting in cirrhosis, as well as CRE > 77 μmol/L were predictable factors affecting survival. Wald test revealed that after adjusting these risk factors, TIPS therapy was more beneficial for improving survival [B = -0.89; Exp (B) = 0.41, 95%CI (0.16, 1.00); P = 0.04]. Comparison in the cause of death between the two groups is shown in Table 2.
| TIPS group | ET group | |
| Cause of death | ||
| Gastrointestinal bleeding | 3 | 9 |
| Liver failure | 4 | 6 |
| Hepatic encephalopathy | 0 | 1 |
| Infection | 1 | 0 |
| Post-operative severe complications | ||
| Fever | 2 | 2 |
| Spontaneous peritonitis | 0 | 2 |
| Hepatorenal syndrome | 0 | 1 |
| Acute peritonitis | 0 | 1 |
Twelve of the postoperative TIPS patients had newly onset of hepatic encephalopathy (Child A grade 4, Child B grade 8), and 5 in ET (Child A grade 2, Child B grade 3). Kaplan-Meier curve analysis showed that there was no statistically significant difference between the two groups in the non-occurrence of hepatic encephalopathy (TIPS group 81.2% vs ET group 91.8%, P = 0.08) (Figure 1C). Individual time point comparison showed that the non-occurrence of hepatic encephalopathy 6 wk after operation in the ET group was higher than in the TIPS group, the difference being statistically significant (TIPS group 82.8% vs ET group 95.1%), and after 12 mo and 24 mo, the difference was no longer statistically significant (TIPS group 82.8% vs ET group 91.8%, TIPS group 81.2% vs ET group 91.8%). Cox regression analysis showed that all selected covariates (age > 53 years, ascites, cirrhosis due to hepatitis, liver function grade with Tbil > 34 μmol/L, CRE > 77 μmol/L) had no significant effect on the occurrence of hepatic encephalopathy [grouping variable for TIPS treatment: B = 0.94; Exp (B) = 2.56, 95%CI (0.86, 7.62); P = 0.09]. Other complications are shown in Table 2.
Hospitalization cost was compared between the two groups (Table 3). The cumulative total cost of hospitalization was 52 678 RMB/person in TIPS group and 38 844 RMB/person in ET group; the cost in the TIPS group was significantly higher than in the ET group (P < 0.05). In the follow-up period, the average hospitalization frequency for the TIPS group was 0.4 times/person and 1.3 times/person for the ET group; ET group had a significantly higher frequency of hospitalization than the TIPS group (P = 0.01). The average length of hospital stay during the follow-up for TIPS group was 5 d/person and 19 d/person for ET group; the ET group had significantly longer hospital stay than the TIPS group (P < 0.05). The patients in the ET group who received TIPS treatment after the failure of endoscopic treatment were included into rescue TIPS group, and comparative results are shown in Table 3.
| Initial TIPS | Rescue TIPS | Rest of ET | |
| (64 cases) | (8 cases) | (54 cases) | |
| Average total expense (RMB) | 52 678 | 63 003 | 35 298 |
| Average length of hospital stay during follow-up (d) | 5 | 20 | 18 |
| Average number of hospitalization during follow-up | 0.4 | 2.1 | 1.2 |
Currently, the endoscopic variceal treatment remains a predominant method for prevention and treatment of recurrent gastrointestinal bleeding[19]. However, endoscopic therapy cannot fundamentally solve the problem of portal hypertension, and patients often cannot tolerate repeated therapies, therefore leading to a high rate of rebleeding. The TIPS procedure, through reducing portal pressure, serves to prevent and control esophageal and gastric variceal bleeding, and alleviate ascites as well. Therefore, with respect to preventing recurrent gastroesophageal bleeding, TIPS is better than endoscopic therapy.
For the TIPS procedure, stenosis of the stent is an important cause of postoperative recurrent bleeding. Previous studies have shown that the rate of stent stenosis is about 30%-70%[20] with the use of bare stent in TIPS whereas the postoperative patency rate is up to 100% with the use of coated stents and Viatorr stent grafts[21-23], and compared with bare stents, they did not increase the incidence of hepatic encephalopathy. This study showed that in the TIPS group, five cases had postoperative stenosis. Of the five cases, only one used the coated stent, and this patient did not follow doctor’s orders to take aspirin for anticoagulation after being discharged from hospital. This further confirms that the use of coated stent can significantly lower the incidence of postoperative stent stenosis, and anticoagulation therapy can further reduce postoperative stent stenosis.
It has been confirmed that with respect to prevention of recurrent bleeding, TIPS is better than medication therapy[13] and endoscopic therapy[14]. The postoperative rebleeding rate was 12%-22% in TIPS, and it is even lower with the use of coated stent. For endoscopic therapy, however, the rebleeding rate is much higher (20%-43%)[15]. Recently, a study by García-Pagán et al[24], comparing the use of Viatorr stent graft TIPS with drug combined endoscopic variceal ligation treatment, showed that in the 16 mo follow-up, only one case of recurrent bleeding occurred in the TIPS group as opposed to 14 cases in the other groups (3.1% vs 45.2%, P = 0.001). In this study, 17.2% of patients in the TIPS group had recurrent bleeding. Cases of rebleeding caused by stenosis of the stent were mostly seen in patients with bare stents. In the ET group, 50% of the patients had recurrent bleeding. This further confirmed that TIPS is superior to endoscopic therapy in prevention of recurrent bleeding and coated stents can further reduce the incidence of recurrent bleeding by lowering the rate of stent stenosis.
It has been shown that TIPS can effectively reduce refractory ascites (RA). It can also lower the incidences of hepatorenal syndrome (HRS), hepatic hydrothorax and other portal hypertension syndromes that are closely related to refractory ascites[24]. In this study, serious postoperative complications associated with portal hypertension, such as RA, HRS and spontaneous bacterial peritonitis, mainly occurred in the ET group, possibly due to increased portal pressure acting as a common mechanism resulting in the above syndromes, whereas TIPS can effectively reduce portal pressure[25].
A large number of clinical studies[13,14] and meta-analyses[15,25,26] indicate that TIPS procedure is not superior to endoscopic therapy with respect to improvement of survival time. This is the main reason why TIPS is used as a rescue option after the failure of the traditional therapeutic method. However, although rescue TIPS procedure can effectlively control acute bleeding, the postoperative one-year survival rate is only 27%-55%[27]. Most of the previous studies on TIPS procedure were based on the use of bare stents, and most patients chose TIPS 2-3 years after traditional treatment, thus making TIPS appear to be not superior to ET in survival rates.
In the study by García-Pagán et al[24], the patients in the TIPS group received TIPS with coated stent at the first incidence of bleeding during the early stages. Results showed that early and middle stage survival rates were much higher in TIPS group than in drug combined endoscopic group (post-operative 6 wk rate for TIPS group was 97% and combined therapy group 67%; post-operative 1 year rate for TIPS group was 86% and combined therapy group 61%), and the middle to long-term efficacy was similar to this study. As for the combined endoscopic group, of the 7 patients who received rescue TIPS due to recurrent bleeding, 4 died within 36 d. Another five patients died due to recurrent bleeding that led to liver failure and incapability to undergo remedy TIPS. Therefore, early implementation of TIPS after the first bleeding may raise the long-term survival rate better than endoscopic therapy. To use TIPS only after the failure of the traditional method may cause the patient to lose the opportunity for the TIPS procedure, thus delaying the illness and lowering survival rate.
Previous studies indicate that the incidence rate of hepatic encephalopathy, 1 year after TIPS was 30%-55%[8,9]. Most cases occur in the early post-operative stage, and are transient in nature. As the brain adapts and adjusts to the increase in ammonia toxins brought by the redistribution of intestinal blood flow, the symptoms disappear[8]. The incidence rate of persistent hepatic encephalopathy that respond poorly to medication was low, 3%-7%[10] for bare stent and 8%[9] for coated stent. García-Pagán et al[24] showed that early TIPS treatment did not increase the incidence rate of hepatic encephalopathy (TIPS 28% and combined endoscopic therapy 40%, P = 0.13). This study demonstrated similar findings. Although in the early post-operative stage, more cases of hepatic encephalopathy occurred in TIPS group than in the ET group, these were mostly transient, and can quickly be controlled through timely administration of anti-hepatic encephalopathy medication.
In this study, although in the early stage, the average overall time spent in the TIPS group is longer than in the ET group, it significantly reduced re-hospitalization and the length of hospital stay. It also decreased incidences of RA, HRS and other portal hypertension related complications. In the ET group in this study, patients who underwent EBL had an average of 1.2 ligations per person. If following the regular course of treatment, the average total cost in the ET group may not be lower than that in the TIPS group. Also, after the failure of the endoscopic therapy, rescue TIPS increases the total cost. This does not comply with the principles of health economics and may cause the patient to lose the opportunity for the TIPS procedure, thus delaying their treatment of illness and lowering the survival rate.
Variceal bleeding is a severe complication of portal hypertension and a major cause of death in patients with cirrhosis. Combined treatment with vasoactive drugs and endoscopic techniques is the recommended standard of care for patients with acute variceal bleeding. However, treatment failure occurs in about 10% - 20% of patients requiring treatment with a transjugular intrahepatic portosystemic shunt (TIPS) as rescue therapy. TIPS is highly effective in controlling bleeding in such patients, but mortality is still very high. The authors conducted a study to determine whether early treatment with TIPS can improve outcomes in patients with cirrhosis and variceal bleeding compared with endoscopic therapy.
TIPS has been used for more than 20 years to treat the complications of portal hypertension. Previous studies evaluating the role of TIPS in the prevention of recurrent variceal bleeding showed that TIPS reduces the rebleeding rate but increases hepatic encephalopathy without improving survival. TIPS is currently recommended only as a rescue therapy. Current practice guidelines for treating patients with acute variceal bleeding recommend fluid resuscitation, antibiotic prophylaxis, and vasoactive drugs such as glypressin or somatostatin analogues, followed by early endoscopy and either ligation or sclerosis of the varicesi.
In this study, early treatment with TIPS, as compared with medical treatment, was associated with an improved prognosis among patients at high risk for uncontrolled bleeding or rebleeding on the basis of a hepatic venous pressure gradient of 20 mmHg or higher. The results of a randomized, multi-center study that compared early TIPS with optimal medical therapy (endoscopic therapy plus vasoactive drugs) in patients at high risk for rebleeding who were either in Child-Pugh class B with active bleeding at endoscopy or in Child-Pugh class C. This study shows the benefit of early TIPS in patients with Child-Pugh class B or C disease who are at high risk for uncontrolled bleeding with standard therapy.
The study re-evaluated how the authors approach variceal bleeding in patients with Child-Pugh class B or C disease. Physicians should consider the early use of TIPS with an e-PFTE-covered stent as first-line therapy rather than as rescue treatment if rebleeding occurs in high-risk patients with Child-Pugh B or C disease.
TIPS is a technique in which a stent is placed between the portal vein and hepatic vein in the liver to provide a portasystemic shunt to reduce portal hypertension. The procedure is carried out under radiological control through the internal jugular vein. Successful shunt placement will stop/prevent bleeding. Endoscopic variceal ligation is a technique with less trauma and fewer side effects, in which varices were sucked into an endoscope allowing them to be occluded with a tight rubber band.
The main drawbacks of the present study are that it is a retrospective analysis, and the study groups were not randomized. However, this study provides another evidence that early TIPS is associated with significant advantages over endoscopic therapy in terms of rebleeding rates, survival and length of hospital stay.
Peer reviewers: Dr. Bhupinder S Anand, Professor, Digestive Diseases Section (111D), VA Medical Center, 2002 Holcombe Blvd., Houston, TX 77030, United States; Vezali Elena, MD, Department of Hepatology,“Hygeia” Diagnostic and Therpaeutic Center of Athens, Eruthrou Staurou 4, 15123 Marousi, Greece
S- Editor Gou SX L- Editor Ma JY E- Editor Lu YJ
| 1. | Garcia-Tsao G, Sanyal AJ, Grace ND, Carey W. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Hepatology. 2007;46:922-938. [PubMed] |
| 2. | Chen MJ, Lin YC, Wu MS. Optimization of timing of endoscopic variceal ligation of esophageal varices. Am J Gastroenterol. 2006;101:908. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 3. | Villanueva C, Miñana J, Ortiz J, Gallego A, Soriano G, Torras X, Sáinz S, Boadas J, Cussó X, Guarner C. Endoscopic ligation compared with combined treatment with nadolol and isosorbide mononitrate to prevent recurrent variceal bleeding. N Engl J Med. 2001;345:647-655. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 261] [Cited by in RCA: 206] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 4. | Patch D, Sabin CA, Goulis J, Gerunda G, Greenslade L, Merkel C, Burroughs AK. A randomized, controlled trial of medical therapy versus endoscopic ligation for the prevention of variceal rebleeding in patients with cirrhosis. Gastroenterology. 2002;123:1013-1019. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 175] [Cited by in RCA: 147] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 5. | Lo GH, Chen WC, Chen MH, Hsu PI, Lin CK, Tsai WL, Lai KH. Banding ligation versus nadolol and isosorbide mononitrate for the prevention of esophageal variceal rebleeding. Gastroenterology. 2002;123:728-734. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 99] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 6. | Kumar A, Jha SK, Sharma P, Dubey S, Tyagi P, Sharma BC, Sarin SK. Addition of propranolol and isosorbide mononitrate to endoscopic variceal ligation does not reduce variceal rebleeding incidence. Gastroenterology. 2009;137:892-901, 901.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 44] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 7. | Rössle M, Siegerstetter V, Huber M, Ochs A. The first decade of the transjugular intrahepatic portosystemic shunt (TIPS): state of the art. Liver. 1998;18:73-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 130] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 8. | Nolte W, Wiltfang J, Schindler C, Münke H, Unterberg K, Zumhasch U, Figulla HR, Werner G, Hartmann H, Ramadori G. Portosystemic hepatic encephalopathy after transjugular intrahepatic portosystemic shunt in patients with cirrhosis: clinical, laboratory, psychometric, and electroencephalographic investigations. Hepatology. 1998;28:1215-1225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 114] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 9. | Riggio O, Angeloni S, Salvatori FM, De Santis A, Cerini F, Farcomeni A, Attili AF, Merli M. Incidence, natural history, and risk factors of hepatic encephalopathy after transjugular intrahepatic portosystemic shunt with polytetrafluoroethylene-covered stent grafts. Am J Gastroenterol. 2008;103:2738-2746. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 174] [Cited by in RCA: 205] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 10. | Salerno F, Cammà C, Enea M, Rössle M, Wong F. Transjugular intrahepatic portosystemic shunt for refractory ascites: a meta-analysis of individual patient data. Gastroenterology. 2007;133:825-834. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 396] [Cited by in RCA: 366] [Article Influence: 20.3] [Reference Citation Analysis (0)] |
| 11. | Ducoin H, El-Khoury J, Rousseau H, Barange K, Peron JM, Pierragi MT, Rumeau JL, Pascal JP, Vinel JP, Joffre F. Histopathologic analysis of transjugular intrahepatic portosystemic shunts. Hepatology. 1997;25:1064-1069. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 60] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 12. | Forauer AR, McLean GK. Transjugular intrahepatic portosystemic shunt constraining stent for the treatment of refractory postprocedural encephalopathy: a simple design utilizing a Palmaz stent and Wallstent. J Vasc Interv Radiol. 1998;9:443-446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 39] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 13. | Escorsell A, Bañares R, García-Pagán JC, Gilabert R, Moitinho E, Piqueras B, Bru C, Echenagusia A, Granados A, Bosch J. TIPS versus drug therapy in preventing variceal rebleeding in advanced cirrhosis: a randomized controlled trial. Hepatology. 2002;35:385-392. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 167] [Cited by in RCA: 148] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 14. | Burroughs AK, Vangeli M. Transjugular intrahepatic portosystemic shunt versus endoscopic therapy: randomized trials for secondary prophylaxis of variceal bleeding: an updated meta-analysis. Scand J Gastroenterol. 2002;37:249-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 87] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 15. | Bosch J, García-Pagán JC. Prevention of variceal rebleeding. Lancet. 2003;361:952-954. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 309] [Cited by in RCA: 288] [Article Influence: 13.1] [Reference Citation Analysis (2)] |
| 16. | Perz JF, Armstrong GL, Farrington LA, Hutin YJ, Bell BP. The contributions of hepatitis B virus and hepatitis C virus infections to cirrhosis and primary liver cancer worldwide. J Hepatol. 2006;45:529-538. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1764] [Cited by in RCA: 1843] [Article Influence: 97.0] [Reference Citation Analysis (0)] |
| 17. | Charon JP, Alaeddin FH, Pimpalwar SA, Fay DM, Olliff SP, Jackson RW, Edwards RD, Robertson IR, Rose JD, Moss JG. Results of a retrospective multicenter trial of the Viatorr expanded polytetrafluoroethylene-covered stent-graft for transjugular intrahepatic portosystemic shunt creation. J Vasc Interv Radiol. 2004;15:1219-1230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 90] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 18. | Rossi P, Salvatori FM, Fanelli F, Bezzi M, Rossi M, Marcelli G, Pepino D, Riggio O, Passariello R. Polytetrafluoroethylene-covered nitinol stent-graft for transjugular intrahepatic portosystemic shunt creation: 3-year experience. Radiology. 2004;231:820-830. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 110] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 19. | Fleming KM, Aithal GP, Solaymani-Dodaran M, Card TR, West J. Incidence and prevalence of cirrhosis in the United Kingdom, 1992-2001: a general population-based study. J Hepatol. 2008;49:732-738. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 127] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 20. | Merli M, Salerno F, Riggio O, de Franchis R, Fiaccadori F, Meddi P, Primignani M, Pedretti G, Maggi A, Capocaccia L. Transjugular intrahepatic portosystemic shunt versus endoscopic sclerotherapy for the prevention of variceal bleeding in cirrhosis: a randomized multicenter trial. Gruppo Italiano Studio TIPS (G.I.S.T.). Hepatology. 1998;27:48-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 125] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 21. | Latimer J, Bawa SM, Rees CJ, Hudson M, Rose JD. Patency and reintervention rates during routine TIPSS surveillance. Cardiovasc Intervent Radiol. 1998;21:234-239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 37] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 22. | Bureau C, Garcia-Pagan JC, Otal P, Pomier-Layrargues G, Chabbert V, Cortez C, Perreault P, Péron JM, Abraldes JG, Bouchard L, Bilbao JI, Bosch J, Rousseau H, Vinel JP. Improved clinical outcome using polytetrafluoroethylene-coated stents for TIPS: results of a randomized study. Gastroenterology. 2004;126:469-475. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 370] [Cited by in RCA: 338] [Article Influence: 16.1] [Reference Citation Analysis (0)] |
| 23. | Angeloni S, Merli M, Salvatori FM, De Santis A, Fanelli F, Pepino D, Attili AF, Rossi P, Riggio O. Polytetrafluoroethylene-covered stent grafts for TIPS procedure: 1-year patency and clinical results. Am J Gastroenterol. 2004;99:280-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 63] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 24. | García-Pagán JC, Caca K, Bureau C, Laleman W, Appenrodt B, Luca A, Abraldes JG, Nevens F, Vinel JP, Mössner J, Bosch J. Early use of TIPS in patients with cirrhosis and variceal bleeding. N Engl J Med. 2010;362:2370-2379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 826] [Cited by in RCA: 842] [Article Influence: 56.1] [Reference Citation Analysis (0)] |
| 25. | Rössle M, Gerbes AL. TIPS for the treatment of refractory ascites, hepatorenal syndrome and hepatic hydrothorax: a critical update. Gut. 2010;59:988-1000. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 160] [Cited by in RCA: 164] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 26. | Khan S, Tudur Smith C, Williamson P, Sutton R. Portosystemic shunts versus endoscopic therapy for variceal rebleeding in patients with cirrhosis. Cochrane Database Syst Rev. 2006;CD000553. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 27. | Zheng M, Chen Y, Bai J, Zeng Q, You J, Jin R, Zhou X, Shen H, Zheng Y, Du Z. Transjugular intrahepatic portosystemic shunt versus endoscopic therapy in the secondary prophylaxis of variceal rebleeding in cirrhotic patients: meta-analysis update. J Clin Gastroenterol. 2008;42:507-516. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 94] [Article Influence: 5.5] [Reference Citation Analysis (0)] |