Published online Dec 21, 2012. doi: 10.3748/wjg.v18.i47.7109
Revised: September 10, 2012
Accepted: September 28, 2012
Published online: December 21, 2012
Processing time: 346 Days and 19.8 Hours
This case reports an application of conventional duodenoscope in a post pancreaticoduodenectomy patient with the help of retrieval balloon assisted enterography. The 56-year-old woman had pancreaticoduodenectomy with Child reconstruction 9 mo ago because of pancreatic adenocarcinoma and now there are recurrent enlarged lymph nodes in the anastomotic stoma of hepaticojejunostomy. Considering the patient’s late-stage cancer, a plastic stent was then successfully placed there to drainage. The main challenge in this case was the extremely long afferent loop and blind cannulation through the anastomotic stoma of hepaticojejunostomy. Retrieval balloon assisted enterography is very helpful for duodenoscope going through the reconstructed intestinal tract and for the cannulation. After two weeks, the patient remained free of painful symptoms and free of fever. Liver function improved well. Four months after the placement of stent, the patient died of cachexia without jaundice, fever and abdominal pain according to her daughter’s statement.
- Citation: Zhuang M, Zhang WJ, Gu J, Liu YB, Wang XF. Retrieval-balloon-assisted enterography in post-pancreaticoduodenectomy endoscopic retrograde cholangiopancreatography. World J Gastroenterol 2012; 18(47): 7109-7112
- URL: https://www.wjgnet.com/1007-9327/full/v18/i47/7109.htm
- DOI: https://dx.doi.org/10.3748/wjg.v18.i47.7109
Endoscopic interventions are usually very challenging in patients with anatomic changes caused by previous gastrointestinal surgery. Methods using front view endoscopy, single-balloon enteroscopy (SBE) and double-balloon enteroscopy (DBE) systems may aid in cholangiopancreatography in postsurgical conditions. In this case, an endoscopic retrograde cholangiopancreatography (ERCP) procedure was successfully performed using a conventional duodenoscope on a post-pancreaticoduodenectomy patient with the help of retrieval-balloon-assisted enterography. The patient was a 56-year-old woman who had undergone a pancreaticoduodenectomy 9 mo previously in another hospital because of pancreatic adenocarcinoma. Recurrent enlarged lymph nodes were found 9 mo after surgery in the anastomotic stoma of the hepaticojejunostomy. A plastic stent was placed in the stenosis and resulted in improved liver function.
A 56-year-old woman presented complaining of abdominal pain, fever and jaundice for two weeks. She had pancreaticoduodenectomy 9 mo previously in another hospital, and the pathological diagnosis was pancreatic adenocarcinoma. Two weeks before this admission, she began to feel abdominal distension and intermittent pain, accompanied by jaundice and fever. The highest fever was 38.6 °C.
Magnetic resonance imaging (MRI) showed that the lymph nodes of the hepatoduodenal ligament were enlarged and causing compression of the anastomotic stoma of hepaticojejunostomy (Figure 1). The intrahepatic duct was markedly expanded. The lymph nodes near the aorta were also enlarged.
Laboratory tests revealed: total white cells 5.9 × 109/L, neutrophilic granulocyte (%) 71.9%, total bilirubin 104 μmol/L, direct bilirubin 81.6 μmol/L, glutamate pyruvate transaminase 34 U/L, glutamic-oxal(o) acetic transaminase 25 U/L.
We performed ERCP using a conventional duodenoscope on this patient, which showed compressed stenosis of the anastomotic stoma of hepaticojejunostomy consistent with the MRI. We then successfully placed a plastic stent in the anastomotic stoma.
Within a few days after placement of the biliary stent, the fever resolved and there was no complaint of abdominal pain. Serum bilirubin levels also went down. Five days later, X-ray of the biliary system showed that no contrast remained in the bile duct and the patient was discharged. Two weeks after discharge, there was still no complaint of abdominal illness or fever. Laboratory tests showed: total white cells 5.9 × 109/L, neutrophilic granulocyte (%) 63.1%, total bilirubin 49.7 μmol/L, direct bilirubin 33.0 μmol/L, glutamate pyruvate transaminase 31 U/L, glutamic-oxal(o) acetic transaminase 55 U/L.
The procedure was performed with the patient under pharyngeal anesthesia and sedation (intramuscular 10 mg diazepam injection). The patient was placed in the left lateral decubitus position. ERCP was performed under fluoroscopic control using a therapeutic duodenoscope with a total length of 120 cm, and a working channel of 3.7-mm diameter (Olympus V260). The duodenoscope was advanced into the stomach and then the afferent jejunal loop through the gastrojejunal anastomosis. The afferent loop after pancreaticoduodenectomy is always longer compared to that after a Billroth II gastrectomy. In this case, after arriving at the afferent loop and pushing the whole duodenoscope into the patient’s stomach and afferent loop by retrieval-balloon-assisted enterography, we realized we were a long way (approximately 30 cm) from the anastomotic stoma of the hepaticojejunostomy (Figure 2A).
The position of the anastomotic stoma of hepaticojejunostomy after pancreaticoduodenectomy was actually invariably near the porta hepatis opening downward to the afferent limb. After using contrast to see the whole picture of the afferent loop, we inserted the wire-guided retrieval-balloon catheter to the extremity of the afferent limb, then inflated the balloon and drew back the catheter slowly. We focused on the possible position of the anastomotic stoma of the hepaticojejunostomy and tried to cannulate the intrahepatic bile duct using a guide wire and finally succeeded. It took only 9 min from when we saw the whole picture of afferent loop to successful cannulation (Figure 2B).
Consistent with the MRI, cholangiography showed the compressed anastomotic stoma of hepaticojejunostomy and expanded intrahepatic duct. We left the guide wire in the intrahepatic duct and removed the retrieval-balloon catheter. Because of the patient’s late-stage cancer, we put a plastic stent through the stenosis of the anastomotic stoma. The stent went along the guide wire and was pushed by a long catheter to the proper site. Contrast came out of the intrahepatic duct into the afferent loop (Figure 2C). Five days later, X-ray showed that the stent remained in the correct position (Figure 3).
Four months later, the patient died of cachexia. According to a statement from her daughter, there was no jaundice, fever or abdominal pain during that time.
ERCP on patients with postsurgical anatomy changes, such as subtotal gastrectomy of Billroth II, Roux-en-Y hepaticojejunostomy and pancreaticoduodenectomy, is difficult to perform. Some case reports describe successful cannulation through front-viewing endoscopes[1], SBE or DBE[2-7]. However, rare cases of use of a conventional duodenoscope have been reported[8-10].
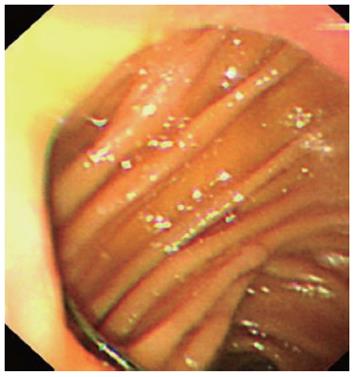
One difficulty in ERCP with postsurgical anatomy changes is how to gain access to the right afferent loop. In our experience, for post-pancreaticoduodenectomy ERCP, the afferent loop was usually at the lesser curvature of stomach, so when we saw the gastrojejunal anastomosis after walking the duodenoscope along the greater curvature of stomach, the “upper tunnel” was the right afferent loop (Figure 4). Sometimes, it was difficult to get into the “upper tunnel” because of the relatively sharp angle. If it was hard to distinguish which was the upper, we would draw back the duodenoscope a little to “relax” the gastrojejunal anastomosis, making it easier to see distinguish the upper. Sometimes, we would also use a catheter (usually the wire-guided retrieval balloon that was used to remove the common bile duct stone) to explore into each limb, injecting contrast into the loop, followed by the scope advancing, and then found the afferent loop. It should be emphasized that in the ERCP with postsurgical anatomy changes, we could rely not only on what was visible through the endoscope, but also the X-ray images from enterology.
The main challenge in this case was the extremely long afferent loop. In an ordinary pancreaticoduodenectomy, the distance from the gastrojejunal anastomosis and the anastomotic stoma of hepaticojejunostomy is at least 60 cm. In theory, the duodenoscope could reach the anastomotic stoma, however, in this case the afferent loop was too long to reach. By using the retrieval balloon catheter and injecting contrast through it, we were able to see how much further we needed to go. The other key point to success in this case was that the surgeons knew the post-pancreaticoduodenectomy anatomy well and, as a result, knew where to cannulate. The retrieval-balloon catheter aided in approaching the anastomotic stoma of the hepaticojejunostomy and served as a sustainer to achieve cannulation successfully.
The retrieval balloon could be used to explore the intestinal tract by injecting contrast through it under X-ray, especially in patients with postsurgical anatomy changes. We termed it retrieval-balloon-assisted enterography. It not only showed us the direction of the tract in order to guide the endoscope forward, but also facilitated forward movement of the endoscope with fewer injuries to the intestinal wall. In a subtotal gastrectomy of Billroth II with side-to-side jejunojejunostomy of afferent and efferent loops, the retrieval-balloon catheter could also be used, by lying in the right limb, as a guide to prevent the duodenoscope from sliding out of the right limb into another upon forward motion. Upon successful accessing of the right limb, the retrieval balloon is visible in the tract ahead, instead of jumping out of it.
Peer reviewer: Guido Costamagna, Professor, Digest Endoscopy Unit, University Sacred Heart, Largo A Gemelli 8, 00168 Rome, Italy
S- Editor Song XX L- Editor A E- Editor Zhang DN
| 1. | Matsushita M, Takakuwa H, Uchida K, Nishio A, Okazaki K. Techniques to facilitate ERCP with a conventional endoscope in patients with previous pancreatoduodenectomy. Endoscopy. 2009;41:902-906. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 2. | Neumann H, Fry LC, Meyer F, Malfertheiner P, Monkemuller K. Endoscopic retrograde cholangiopancreatography using the single balloon enteroscope technique in patients with Roux-en-Y anastomosis. Digestion. 2009;80:52-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 61] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 3. | Mönkemüller K, Fry LC, Bellutti M, Neumann H, Malfertheiner P. ERCP with the double balloon enteroscope in patients with Roux-en-Y anastomosis. Surg Endosc. 2009;23:1961-1967. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 61] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 4. | Cho S, Kamalaporn P, Kandel G, Kortan P, Marcon N, May G. 'Short' double-balloon enteroscope endoscopic retrograde cholangiopancreatography in patients with a surgically altered upper gastrointestinal tract. Can J Gastroenterol. 2011;25:615-619. [PubMed] |
| 5. | Itoi T, Ishii K, Sofuni A, Itokawa F, Kurihara T, Tsuchiya T, Tsuji S, Ikeuchi N, Moriyasu F. Ultraslim endoscope-assisted therapeutic ERCP for inaccessible papilla by a double-balloon enteroscope in patients with Roux-en-Y anastomosis. Endoscopy. 2011;43 Suppl 2 UCTN:E36-E37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | Moreels TG, Pelckmans PA. Comparison between double-balloon and single-balloon enteroscopy in therapeutic ERC after Roux-en-Y entero-enteric anastomosis. World J Gastrointest Endosc. 2010;2:314-317. [PubMed] |
| 7. | Itoi T, Ishii K, Sofuni A, Itokawa F, Tsuchiya T, Kurihara T, Tsuji S, Ikeuchi N, Umeda J, Moriyasu F. Single-balloon enteroscopy-assisted ERCP in patients with Billroth II gastrectomy or Roux-en-Y anastomosis (with video). Am J Gastroenterol. 2010;105:93-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 124] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 8. | Lin LF, Siauw CP, Ho KS, Tung JC. ERCP in post-Billroth II gastrectomy patients: emphasis on technique. Am J Gastroenterol. 1999;94:144-148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 74] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 9. | Nakahara K, Horaguchi J, Fujita N, Noda Y, Kobayashi G, Ito K, Obana T, Takasawa O. Therapeutic endoscopic retrograde cholangiopancreatography using an anterior oblique-viewing endoscope for bile duct stones in patients with prior Billroth II gastrectomy. J Gastroenterol. 2009;44:212-217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 35] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 10. | Wang XF, Mei JW, Zhang WJ, Gu J, Zhuang M, Shi WB, Zhang Y, Gong W. Endoscopic retrograde cholangiopancreatography after Billroth II gastrectomy. Zhonghua Xiaohua Neijing Zazhi. 2010;27:451-453. |