Published online Dec 21, 2012. doi: 10.3748/wjg.v18.i47.7100
Revised: October 30, 2012
Accepted: November 14, 2012
Published online: December 21, 2012
Processing time: 320 Days and 2.5 Hours
Inflammatory myofibroblastic tumor (IMT) occurring at retroperitoneal sites has rarely been reported. We report the case of a previously well 14-year-old girl with no history of abdominal disease whose past medical history and family tumor history were unremarkable. She complained of intermittent abdominal pain for one month. An abdominal mass was found on physical examination and abdominal contrast-enhanced computed tomography (CT) showed a hypodense soft mass, the size and location of which suggested a well delineated retroperitoneal tumor surrounding the superior mesenteric vessels measuring 3.3 cm × 4.5 cm × 4.5 cm with enlarged lymph nodes. The patient underwent an exploratory laparotomy followed by biopsy and was subsequently diagnosed with retroperitoneal IMT. She was successfully treated with postoperative chemotherapy and oral diclofenac sodium. Following completion of therapy the mass was no longer palpable and no longer visible on CT scanning. The use of methotrexate and cisplatin for aggressive myofibroblastic tumors is also reviewed.
- Citation: Tao YL, Wang ZJ, Han JG, Wei P. Inflammatory myofibroblastic tumor successfully treated with chemotherapy and nonsteroidals: A case report. World J Gastroenterol 2012; 18(47): 7100-7103
- URL: https://www.wjgnet.com/1007-9327/full/v18/i47/7100.htm
- DOI: https://dx.doi.org/10.3748/wjg.v18.i47.7100
Inflammatory myofibroblastic tumor (IMT) is a rare soft-tissue tumor with a clinical resemblance to malignant neoplasm[1]. It is an unusual solid tumor commonly seen in children and young adults, and can occur at any site in the body, the lung being the most common site[2]. Extrapulmonary IMTs account for 5% of all IMTs and retroperitoneal IMTs are relatively rare[3]. The retroperitoneum is an unusual site of presentation in these rare tumors, which share the neoplastic characteristics of aggressive local tissue infiltration, recurrence after resection, and occasionally distant metastasis[2,4]. Due to disease progression, lack of alternative therapeutic regimens, recurrence and poor prognosis, almost all patients with IMT have been treated with radical surgical resection or single nonsteroidal anti-inflammatory drugs. Herein, we present a patient with a retroperitoneal IMT, who was successfully treated with chemotherapy and oral diclofenac sodium.
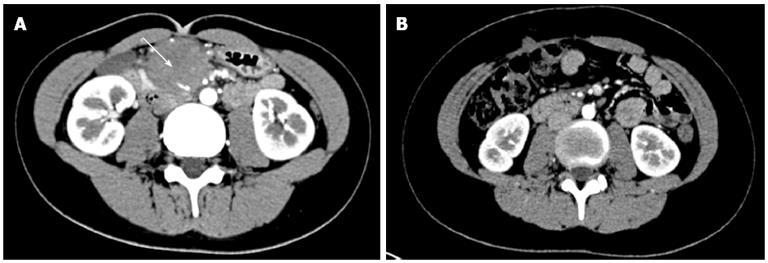
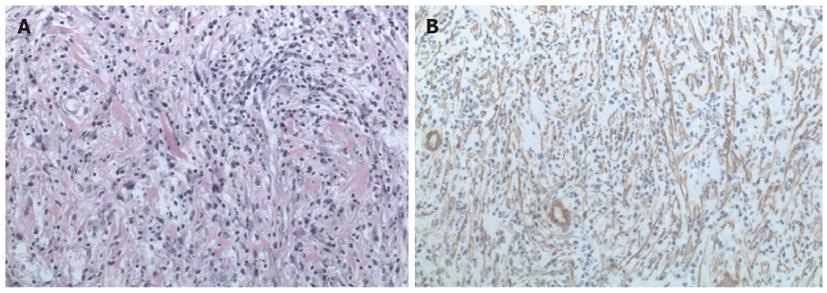
A 14-year-old girl was admitted to our hospital in June 2009 with the chief complaint of intermittent abdominal pain for one month. She experienced intermittent abdominal pain without bloating every two days and all symptoms were in remission after she buckled both legs, however, the pain returned a few minutes later. The patient did not have symptoms of fever, nausea, vomiting, weight loss, bowel obstruction or other discomfort and she did not receive treatment to relieve these symptoms prior to admission. This 14-year-old girl was previously well with no history of abdominal disease, and her past medical history and family tumor history were unremarkable. Physical examinations showed a 7 cm abdominal mass in the right side of the umbilicus, which was hard, without tenderness and firm but mobile on palpation. Blood count analysis and tumor markers such as carcinoembryonic antigen and CA19-9 were negative. Abdominal contrast-enhanced computed tomography showed a hypodense soft mass, the size and location of which suggested a well delineated retroperitoneal tumor surrounding the superior mesenteric vessels which measured 3.3 cm × 4.5 cm × 4.5 cm with enlargement of the surrounding lymph nodes (Figure 1A). Given that the preoperative diagnosis was unconfirmed and radical surgery was the most efficient therapeutic option, after a multidisciplinary discussion, an exploratory laparotomy was performed. During the operation, a 10 cm round solid mass was found at the root of the mesentery. The tumor reached the uncinate process of the pancreas and the horizontal section of the duodenum. Complete excision of the mass was difficult, because the tumor surrounded most of the superior mesenteric artery branches. Therefore, biopsy of the mass was undertaken. Pathologic examination confirmed the diagnosis of IMT with a proliferation of spindle cells and dense polymorphic infiltration of mononuclear inflammatory cells (Figure 2A). On immunohistochemical staining, spindle cells were positive for vimentin, smooth muscle actin (Figure 2B) and CD68, but negative for Cluster of differentiation 34 (CD34), Cluster of differentiation 117 (CD117) and anaplastic lymphoma kinase-1 (ALK-1).
The postoperative course was uneventful and the patient was discharged from the hospital without complications. Three weeks after surgery, the patient received chemotherapy which consisted of 6 courses of middle dose methotrexate (20 mg/m2) and cisplatinum (30 mg/m2) administered once a month, associated with oral administration of slow-release diclofenac sodium until cessation of chemotherapy. The patient was re-examined after completing chemotherapy; the mass was no longer palpable and was no longer visible on (computer tomography) CT scanning (Figure 1B). Currently, the patient is alive without recurrence after 3 years of follow-up.
IMT was originally described in the lungs in 1937, and since then has been reported to occur throughout the body including the mesentery, stomach, abdomen, liver, mediastinum, retroperitoneum, omentum and bladder of children and adolescents[5]. Retroperitoneal IMTs are extremely rare. This tumor was previously described as an inflammatory pseudotumor, inflammatory myofibroblastoma, lymphoplasmacytic, histiocytoma, and fibrous pseudotumor until 1994 when myofibroblastic tumor was established as a distinct low grade malignancy by the World Health Organization classification[6-8]. The exact etiology of the disease is still not completely known. In a review of the medical literature, researchers have suggested that trauma, surgery, inflammation and infection by the Epstein-Barr virus or Human Herpes virus could result in the development of IMT[9]. Others have insisted that a chromosomal rearrangement involving the ALK gene results in the activation of a tyrosine kinase receptor and could lead to abnormal expression[10]. In the present case, the patient had no past medical history related to this disease, therefore, there is no evidence of a direct relationship between the development of the disease and susceptible factors.
The clinical presentation of the tumor often depends on its anatomical site. Retroperitoneal tumors usually grow slowly and always present as a solid abdominal palpable mass, accompanied by abdominal pain or weight loss. It is only when the retroperitoneal tumor increases in size resulting in obstructive symptoms, that intestinal obstruction may be diagnosed. As shown in our report, the patient presented with an atypical clinical manifestation of intermittent abdominal pain accompanied by a localized mass and no significant abnormal laboratory tests. The CT features in our patient showed varied degrees of enhancement on the complex soft tissue involving the mesenteric vessels with nonspecific findings, which was mostly indistinguishable from a malignant process. It is difficult to confirm this disease using these atypical clinical manifestations pre- or intra-operatively. A definite diagnosis therefore depends on histopathological evaluation after biopsy or resection.
When necessary, surgical resection could be considered the preferred treatment for IMT, which can also be used to confirm this disease. The recurrence rate has been reported to range from 18% to 40%, and only precise removal of the tumor will avoid recurrence[11]. In our patient, the location of the tumor made it difficult to cure by means of a complete radical resection which may have led to intestinal ischemia and even postoperative short bowel syndrome. Steroids and radiotherapy as well as chemotherapy as adjuvant therapy are feasible alternatives to surgery. Chemotherapy, radiotherapy, and even immunomodulation have not been reported to be consistently effective against this aggressive tumor[12]. No other efficient treatment regimens have been reported for this tumor. Consequently, in patients with unresectable IMTs, treatment options are limited, and better recommendations have not been defined.
Nonsteroidal anti-inflammatory drugs (NSAIDs) have been successful in the treatment of IMTs when resectability is limited due to the tumor invading vital structures[13]. Przkora et al[14] reported that two patients with nonresectable intra-abdominal IMTs had a satisfactory outcome after receiving treatment with nonsteroidal anti-inflammatory drugs. There is no evidence to prove that chemotherapy is effective when used singly, however, it may play a role following complete resection. As shown in our case, patients with unresectable retroperitoneal IMTs receiving conventional-dose methotrexate/cisplatin chemotherapy and oral NSAIDs can be symptom-free after 3 years of follow-up without relapse or metastasis and achieve a favorable prognosis. Therefore, chemotherapy combined with oral NSAIDs may be an effective therapeutic option for patients with unresectable IMT.
Our experience with the patient in this report might provide another treatment choice for patients with unresectable, residual or recurrent IMT.
In summary, our findings suggest that middle-dose chemotherapy and NSAIDs may be a feasible therapeutic choice in patients with unresectable retroperitoneal IMT.
Peer reviewer: Dr. Elpek GO, School of Medicine, Department of Pathology, Akdeniz University, TR-07070 Antalya, Turkey
S- Editor Jiang L L- Editor A E- Editor Zhang DN
| 1. | Wani I. Inflammatory myofibroblastic tumor of mesentery: a case report. J Gastrointest Cancer. 2007;38:115-118. [PubMed] |
| 2. | Koirala R, Shakya VC, Agrawal CS, Khaniya S, Pandey SR, Adhikary S, Pathania OP. Retroperitoneal inflammatory myofibroblastic tumor. Am J Surg. 2010;199:e17-e19. [PubMed] |
| 3. | Soga H, Yao A, Matsushita K, Shimogaki H, Kawabata G. Inflammatory pseudotumor of the retroperitoneum removed via a retroperitoneoscopic approach. JSLS. 2011;15:272-274. [PubMed] |
| 4. | Diop B, Konate I, Ka S, Sall I, Fall D, Dieng M, Wone Y. Mesenteric myofibroblastic tumor: NSAID therapy after incomplete resection. J Visc Surg. 2011;148:e311-e314. [PubMed] |
| 5. | Mattei P, Barnaby K. Rapid regression of duodenal inflammatory myofibroblastic tumor after intravenous ketorolac: case report and review of the literature. J Pediatr Surg. 2008;43:1196-1199. [PubMed] |
| 7. | Cerfolio RJ, Allen MS, Nascimento AG, Deschamps C, Trastek VF, Miller DL, Pairolero PC. Inflammatory pseudotumors of the lung. Ann Thorac Surg. 1999;67:933-936. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 206] [Cited by in RCA: 174] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 8. | Leon CJ, Castillo J, Mebold J, Cortez L, Felmer R. Inflammatory myofibroblastic tumor of the stomach: an unusual complication after gastrectomy. Gastrointest Endosc. 2006;63:347-349. [PubMed] |
| 9. | Xiang J, Liu X, Wu S, Lv Y, Wang H. Multiple inflammatory myofibroblastic tumor of the duodenum: case report and literature review. J Gastrointest Surg. 2012;16:1442-1445. [PubMed] |
| 10. | Choi AH, Bohn OL, Beddow TD, McHenry CR. Inflammatory myofibroblastic tumor of the small bowel mesentery: an unusual cause of abdominal pain and uveitis. J Gastrointest Surg. 2011;15:584-588. [PubMed] |
| 11. | Bertocchini A, Lo Zupone C, Callea F, Gennari F, Serra A, Monti L, de Ville de Goyet J. Unresectable multifocal omental and peritoneal inflammatory myofibroblastic tumor in a child: revisiting the role of adjuvant therapy. J Pediatr Surg. 2011;46:e17-e21. [PubMed] |
| 12. | Lu CH, Huang HY, Chen HK, Chuang JH, Ng SH, Ko SF. Huge pelvi-abdominal malignant inflammatory myofibroblastic tumor with rapid recurrence in a 14-year-old boy. World J Gastroenterol. 2010;16:2698-2701. [PubMed] |
| 13. | Su W, Ko A, O'Connell T, Applebaum H. Treatment of pseudotumors with nonsteroidal antiinflammatory drugs. J Pediatr Surg. 2000;35:1635-1637. [PubMed] |
| 14. | Przkora R, Bolder U, Schwarz S, Jauch KW, Spes J, Andreesen R, Mackensen A. Regression of nonresectable inflammatory myofibroblastic tumours after treatment with nonsteroidal anti-inflammatory drugs. Eur J Clin Invest. 2004;34:320-321. [PubMed] |