Published online Jan 21, 2012. doi: 10.3748/wjg.v18.i3.275
Revised: August 18, 2011
Accepted: August 27, 2011
Published online: January 21, 2012
AIM: To evaluate the efficacy of intraductal ultrasonography (IDUS) in the diagnosis of non-opaque, common bile duct stones.
METHODS: A total of 183 patients (102 males, mean age 73 years; 81 females, mean age 70 years) with suspected common bile duct stones diagnosed through abdominal computed tomography (CT), magnetic resonance imaging (MRI), and abdominal Type-B ultrasound were included in the study. The diagnosis was confirmed through endoscopic retrograde cholangiopancreatography (ERCP) followed by IDUS.
RESULTS: A total of 183 patients with suspected common bile duct (CBD) stones were included in the study as follows: 36 patients with high-density CBD stones, 68 patients with sand-like stones, 44 patients with low-density stones, 21 patients with ampullary cancer, and 14 patients with pancreatic cancer. Conventional imaging revealed 124 cases of choledochectasia, and only 36 cases of suspected CBD stones; ERCP revealed 145 cases of CBD stones with three missed diagnoses. IDUS revealed 148 cases of CBD stones, 21 cases of ampullary tumors, and 14 cases of pancreatic cancer.
CONCLUSION: IDUS was more effective in the diagnosis of bile duct stones than ERCP, upper abdominal CT or upper abdominal MRI.
- Citation: Lu J, Guo CY, Xu XF, Wang XP, Wan R. Efficacy of intraductal ultrasonography in the diagnosis of non-opaque choledocholith. World J Gastroenterol 2012; 18(3): 275-278
- URL: https://www.wjgnet.com/1007-9327/full/v18/i3/275.htm
- DOI: https://dx.doi.org/10.3748/wjg.v18.i3.275
Common bile duct (CBD) stones can cause a range of serious complications such as obstructive jaundice, biliary tract infection, and pancreatitis. These stones may even cause severe septic shock and lead to life-threatening conditions[1]. With the continuous development of endoscopic technology, endoscopic treatment has now become a standard diagnostic procedure for bile duct stones. Endoscopic retrograde cholangiopancreatography (ERCP) has long been considered the gold standard for the diagnosis of CBD stones because it can accurately image the pancreatic duct system. With diagnostic accuracy higher than 90%, ECRP is significantly more effective in the diagnosis of extra-hepatic bile duct stones than computed tomography (CT), or magnetic resonance imaging (MRI). However, misdiagnoses and missed diagnoses still occur due to operator error and variations in the contrast agent concentration and stone density[2]. Biliary intraductal ultrasonography (IDUS), which has emerged as a safe and effective new method for the diagnosis of CBD stones in recent years, combines high-resolution ultrasound imaging with endoscopy, thereby preventing imaging of the pancreatic duct system from being affected by intestinal gas. It is accurate in the diagnosis of smaller non-opaque stones and low-density stones, i.e., stones with density similar to that of the contrast agent. Through the IDUS examination of ERCP surgery patients between January 2009 and August 2010, in this study we investigated the efficacy of IDUS combined with ERCP in the diagnosis of bile duct stones.
A total of 183 ERCP surgery patients treated between January 2009 and August 2010 were retrospectively analyzed. The patient population was as follows: 102 males, mean age 69 years; 81 females, mean age 71 years. All patients exhibited upper abdominal pain, nausea, vomiting, chills, fever and jaundice. The preoperative imaging studies included abdominal CT or upper abdominal enhanced MRI + magnetic resonance cholangiopancreatography (slice thickness of 7 mm, plane scanning with layer gap of 3 mm, cross section T1W1/T2W1), and these examinations were done at the Radiology Department of Shanghai Tenth Hospital, revealing 124 patients with suspected choledochectasia, 36 patients with suspected common bile duct stones, and 23 patients with negative imaging but suspicious clinical presentation and laboratory test results.
IDUS surgery was performed in all cases. First, we conducted preoperative preparations for conventional ERCP. Next, ERCP was carried out with inclusion of the following three procedures: cholangiography after successful wire-guided bile duct intubation; a partial intraoperative duodenal papillotomy based on the specific circumstances; and biliary tract imaging to determine whether a stone or a stenosis was the cause of the clinical findings. This was followed by the insertion of an ultrasound scanning probe along the guide wire to observe the bile ducts. The ultrasound probe was removed after the IDUS examination was completed, and the subsequent stages of the ECRP procedure, which included biliary stent placement and nasal biliary drainage, were determined from the specifics of the clinical situation, e.g., the presence of bile duct stones. The criteria for IDUS diagnosis of bile duct stones were evaluated by experts who were experienced in IDUS imaging.
The sensitivity, specificity, negative predictive value, positive predictive value, and diagnostic accuracy of the comparisons were calculated. The SPSS13 statistical package was used for the statistical analysis. The χ2 test was used to compare rates, and the Scheffé method was used for pairwise comparisons among groups. P values < 0.05 were considered statistically significant.
A total of 183 patients with suspected CBD stones were included in the study as follows: 36 patients with high-density CBD stones, 68 patients with sand-like stones, 44 patients with low-density stones, 21 patients with ampullary cancer, and 14 patients with pancreatic cancer.
Conventional imaging revealed 124 cases of choledochectasia, and only 36 cases of suspected CBD stones in the 148 confirmed cases; this represents a diagnosis rate of 24.3%, sensitivity of 24.3%, specificity of 100%, and diagnostic accuracy of 38.3%.
ERCP revealed 145 cases of CBD stones with three missed diagnoses, which resulted in a diagnostic accuracy of 98%. The remaining 35 cases that did not involve CBD stones comprised 21 cases of ampullary tumors and 14 cases of pancreatic cancer; all were diagnosed with an accuracy of 100%. The sensitivity, specificity, and accuracy of ERCP were 98%, 100% and 98.4%, respectively.
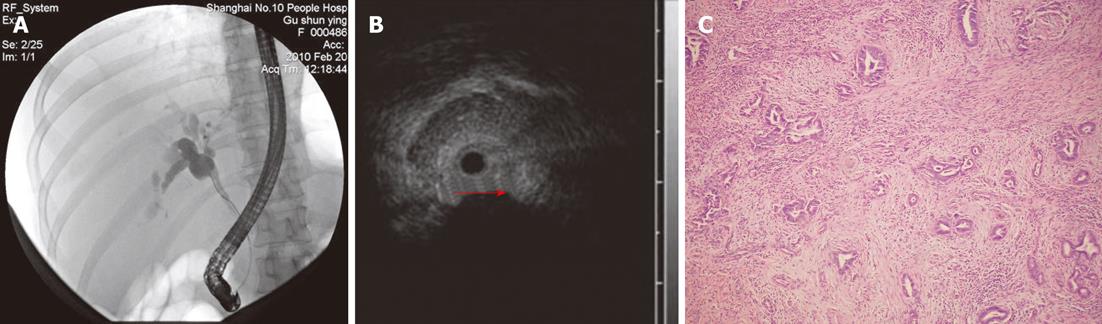
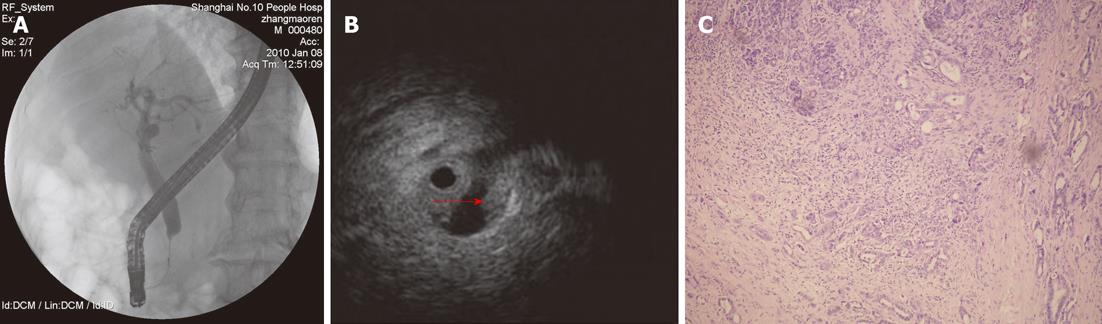
IDUS revealed 148 cases of CBD stones, 21 cases of ampullary tumors (Figure 1), and 14 cases of pancreatic cancer (Figure 2), which resulted in a specificity of 100%, sensitivity of 100%, and accuracy of 100%. Of the 148 cases of CBD stones, 27 patients underwent cholecystectomy and CBD stones were intraoperatively confirmed in all cases.
Of the 183 cases included in the study, 3 patients showed pancreatitis after ERCP, which represents an incidence rate of 1.64% (3/183). The pancreatitis complications improved after conservative treatment that included fasting, acid-suppression, inhibition of enzymes, and anti-inflammatory drugs. No other complications such as bleeding or perforation were observed (Table 1).
| Diagnosis | Missed diagnosis | Accuracy (%) | |
| Common imaging (n = 148) | 36 | 112 | 24.3 |
| ERCP (n = 148) | 145 | 3 | 98 |
| ERCP + IDUS (n = 148) | 148 | 0 | 100 |
CBD stones are commonly encountered in clinical settings, and jaundice is usually observed as the first symptom[3]. Although the diagnosis of such a disease using surface ultrasonography, CT and MRI has been greatly improved, their diagnostic accuracy is still not ideal[4]. In this study, conventional imaging showed an accurate preoperative diagnosis rate of 24.3%.
In ERCP images, opaque CBD stones clearly appear as round or crescent shaped objects. Although cholangiectasis is also typically observed, other low-density and sand-like stones are not visible[5]. ERCP, as a direct biliary imaging method, exhibits high resolution, which not only helps in further clarifying the location and number of stones, but also facilitates further interventions. Therefore, since the 1970s, ERCP has been the gold standard for the diagnosis of extrahepatic bile duct stones[6]. However, the evaluation of biliary pathological changes through ERCP is evaluated by contrast agent and image shapes of X-ray. Therefore, several factors may contribute to misdiagnosis and missed diagnoses using ERCP, such as the nature and size of the stones, air bubbles in the bile duct, variations in contrast agent concentration, and the injection rate[7]. The diagnostic accuracy of ERCP in this study was 98%. Endo-ultrasonography (EUS), which is a technological combination of ultrasonography and direct endoscopic visual inspection, was introduced in the 1980s. After years of technological development, EUS now plays an important role in the diagnosis and treatment of digestive diseases[8]. Miniature ultrasonic probes exhibit small diameters and high frequencies. In this manner, IDUS can be used to explore the pancreatic duct via the guide wire during ERCP. When used in the bile duct, IDUS repeatedly scans the involved anatomy and generates cross-sectional images of the bile duct wall and the lesion, which clearly show the inner structures with reduced interference. Lesions that are at least 0.5 cm in diameter, as well as the structure of adjacent organs such as the liver, portal vein, pancreas and portions of the pancreatic duct, can be clearly observed. Determining the specific causes of obstructive jaundice and evaluating the severity of such lesions is valuable[9]. In this study, based on the previously reported criteria for the diagnosis of CBD stones, IDUS showed a diagnostic accuracy of 100%, which is significantly higher than that of ERCP and other imaging methods. For the diagnosis of CBD malignant strictures, IDUS is also more accurate than surface imaging and ERCP. In this study, no malignant lesions were diagnosed prior to the ERCP procedures; however, with the use of IDUS, 21 cases of ampullary cancer and 14 cases of pancreatic cancer were found. Therefore, IDUS is useful in the early diagnosis of bile duct or ampullary tumors[10].
Bleeding, perforation, and acute pancreatitis are major complications of ERCP[11]. In this study, severe pancreatitis and gastrointestinal perforation did not occur in any of the cases; however, there were three cases of pancreatitis after ERCP with minimal edema that improved after conservative treatment such as enzyme inhibition, acid-suppression, and anti-inflammatory drug administration. In conclusion, the use of IDUS in combination with ERCP is a safe and reliable method of increasing the diagnostic accuracy of ERCP.
The incidence of choledocholith is currently rising with the improvement of living standards and changes in food habits. Common bile duct (CBD) stones can cause a range of serious complications such as obstructive jaundice, biliary tract infection, and pancreatitis. A safe and accurate method to diagnosis CBD stones is urgently needed.
Endoscopic retrograde cholangiopancreatography (ERCP) is a significant method in the diagnosis of CBD stones. However, misdiagnoses still occur. IDUS is a new, safe method for the diagnosis of bile duct pathological changes.
This is the first research to report the outcome of intraductal ultrasonography (IDUS) in the diagnosis of non-opaque stones. IDUS showed a diagnostic accuracy of 100%.
IDUS is useful in the diagnosis of non-opaque, common bile duct stones and early diagnosis of bile duct or ampullary tumors.
The paper evaluates the efficacy of intraductal ultrasonography (IDUS) in the diagnosis of non-opaque, common bile duct stones. The study is very interesting.
Peer reviewer: Herwig R Cerwenka, Professor, Department of Surgery, Medical University of Graz, Auenbruggerplatz 29, A-8036 Graz, Austria
S- Editor Tian L L- Editor Logan S E- Editor Xiong L
| 1. | Chen WX, Zhang Y, Li YM, Xu GQ, Fang Y, Cai SP. Endoscopic retrograde cholangiopancreatography in evaluation of choledochal dilatation in patients with obstructive jaundice. Hepatobiliary Pancreat Dis Int. 2002;1:111-113. [PubMed] |
| 2. | Xu AM, Cheng HY, Jiang WB, Chen D, Jia YC, Wu MC. Multi-slice three-dimensional spiral CT cholangiography: a new technique for diagnosis of biliary diseases. Hepatobiliary Pancreat Dis Int. 2002;1:595-603. [PubMed] |
| 3. | Moghimi M, Marashi SA, Salehian MT, Sheikhvatan M. Obstructive jaundice in Iran: factors affecting early outcome. Hepatobiliary Pancreat Dis Int. 2008;7:515-519. [PubMed] |
| 4. | Holm AN, Gerke H. What should be done with a dilated bile duct? Curr Gastroenterol Rep. 2010;12:150-156. [PubMed] |
| 5. | Tang LJ, Tian FZ, Cai ZH. Cholecysto-choledochostomy plus construction of subcutaneous cholecystic tunnel in treatment of choledocholith. Hepatobiliary Pancreat Dis Int. 2003;2:114-116. [PubMed] |
| 6. | Mosler P, Fogel EL. Massive subcutaneous emphysema after attempted endoscopic retrograde cholangiopancreatography in a patient with a history of bariatric gastric bypass surgery. Endoscopy. 2007;39 Suppl 1:E155. [PubMed] [DOI] [Full Text] |
| 7. | Wilcox CM. Endoscopic examination with the duodenoscope at ERCP: frequency of lesions and accuracy of detection. Gastrointest Endosc. 2002;55:538-542. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Malik S, Kaushik N, Khalid A, Bauer K, Brody D, Slivka A, McGrath K. EUS yield in evaluating biliary dilatation in patients with normal serum liver enzymes. Dig Dis Sci. 2007;52:508-512. [PubMed] [DOI] [Full Text] |
| 9. | Stavropoulos S, Larghi A, Verna E, Battezzati P, Stevens P. Intraductal ultrasound for the evaluation of patients with biliary strictures and no abdominal mass on computed tomography. Endoscopy. 2005;37:715-721. [PubMed] |
| 10. | Inui K, Yoshino J, Miyoshi H. Differential diagnosis and treatment of biliary strictures. Clin Gastroenterol Hepatol. 2009;7:S79-S83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 11. | Rácz I, Rejchrt S, Hassan M. Complications of ERCP: ethical obligations and legal consequences. Dig Dis. 2008;26:49-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |