Published online Jul 28, 2012. doi: 10.3748/wjg.v18.i28.3761
Revised: January 18, 2011
Accepted: May 12, 2012
Published online: July 28, 2012
Type IV-A choledochal cysts (CCs) are a congenital biliary anomaly which involve dilatation of the extrahepatic and intrahepatic bile ducts. We present the case of a 30-year-old woman with type IV-A CC, on whom three-dimensional computed tomography (3D CT) and virtual endoscopy were performed. 3D CT revealed partial dilatation in the posterior branch of the intrahepatic bile duct and a relative stricture between it and the extrahepatic bile duct. Virtual endoscopy showed that this stricture was membrane-like and separated from the surrounding blood vessels. Based on these image findings, complete cyst resection, bile duct plasty for the stricture, and hepaticojejunostomy were safely performed. To the best of our knowledge, there are no reports of imaging by virtual endoscopy of the biliary tract which show the surrounding blood vessels running along the bile duct.
- Citation: Tsuchida A, Nagakawa Y, Kasuya K, Kyo B, Ikeda T, Suzuki Y, Aoki T, Itoi T. Computed tomography virtual endoscopy with angiographic imaging for the treatment of type IV-A choledochal cyst. World J Gastroenterol 2012; 18(28): 3761-3764
- URL: https://www.wjgnet.com/1007-9327/full/v18/i28/3761.htm
- DOI: https://dx.doi.org/10.3748/wjg.v18.i28.3761
Choledochal cysts (CCs), namely, congenital bile duct dilatation, are high-risk factors for biliary tract cancer[1,2]. Almost all cases of type I and type IV-A CCs are associated with pancreaticobiliary maljunction, and preventative diversion surgery is performed even without the presence of cancer[3]. Type IV-A CCs involve dilatation of the extrahepatic and intrahepatic bile ducts, and relative stricture at the junction of both is often observed. If this stricture is left alone, several complications, including cholangitis, hepatolithiasis, and cholangiocarcinoma may occur after surgery. Therefore, bile duct plasty for stricture or bile duct resection which includes the stricture site is required[4,5]. Moreover, if the stricture or cyst is present in the intrahepatic bile duct, hepatectomy is required to remove these lesions[4,6]. Accordingly, for type IV-A CCs, a thorough examination of the biliary tract is necessary before surgery. Recently, three-dimensional (3D) imaging and virtual endoscopy based on computed tomography (CT) or magnetic resonance images have often been used for the evaluation of biliary tract anatomy and disease detection[7-10]. Here, we report a case of type IV-A CC in which the condition of the bile duct stricture and blood vessels running along the CC were confirmed by 3D CT imaging and virtual endoscopy, and surgery was safely performed.
A 30-year-old woman was admitted to a local hospital because of cholangitis during late pregnancy. Since marked dilatation of the common bile duct and jaundice were observed, she underwent percutaneous transhepatic bile duct drainage (PTCD). She was given a diagnosis of type IV-A CC with pancreaticobiliary maljunction and was transferred to our department for surgery. We performed cholangiography by injecting a contrast medium via a PTCD tube, and imaging data at 1 mm intervals obtained by multislice CT was evaluated using a 3D image analytic system (Synapse Vincent FN-7941; Fuji Film Medical Co., Ltd., Tokyo, Japan).
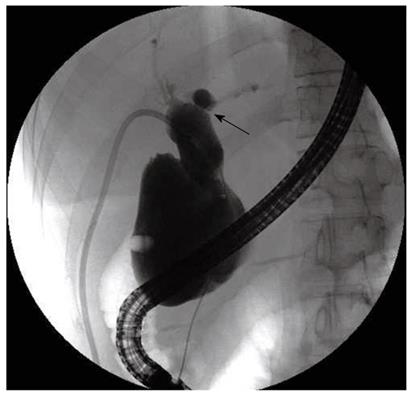
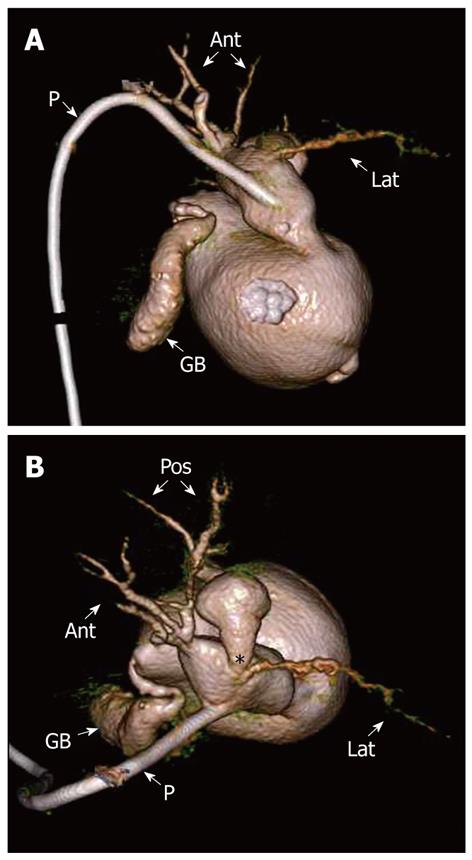
PTCD cholangiography and endoscopic retrograde cholangiopancreatography (ERCP) revealed marked cystic dilatation in the common bile duct (Figure 1). The end of the common bile duct was obstructed, and communication between the bile duct and the side of the papilla was not observed. Moreover, stricture was found in the transition site, which was assumed to be between the left hepatic duct and the intrahepatic bile duct. On a 3D image of the biliary tract, no dilatation in the anterior branch or the lateral branch of the intrahepatic bile duct, and no relative stricture of the extrahepatic bile duct were observed. However, the posterior branch showed partial dilatation in the transition site from the extrahepatic bile duct, and relative stricture was observed in the transition site, but with no stricture or dilatation in the peripheral bile duct (Figure 2).
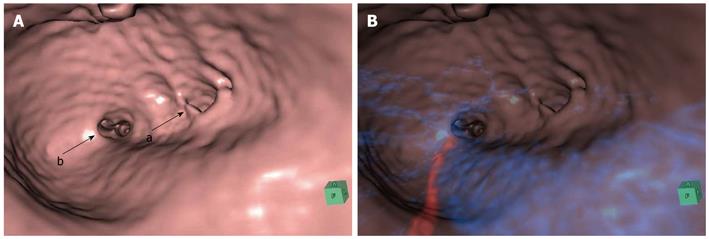
A virtual endoscopic image of the biliary tract showed no stricture in the orifice of the anterior branch, but the presence of a membrane-like stricture in the orifice of the posterior branch was confirmed (Figure 3A). Furthermore, when this image was overlapped with blood vessel images obtained by 3D imaging, the distribution of a blood vessel system around the biliary tract was clearly observed. This image showed that blood vessels did not run in the membrane-like stricture (Figure 3B).
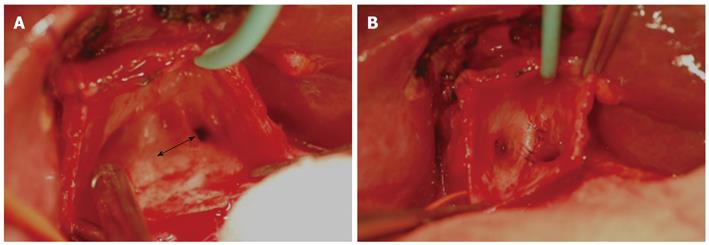
During surgery, the gallbladder and dilated extrahepatic bile duct were removed. Next, the membrane-like stricture of the posterior branch was cut by several mm, and each cut end was sutured with 2 stitches of 5-0 absorbable sutures. This alleviated the relative stricture, and the orifice of the posterior branch expanded sufficiently (Figure 4). Finally, the bile ducts on the hepatic side and jejunum were anastomosed. In the histopathological findings of the resected specimen, chronic inflammation and hyperplasia of the gallbladder and bile duct were observed, but no malignancy was observed. One year after surgery, no complications, including cholangitis or hepatolithiasis, have been observed.
3D imaging and virtual endoscopy based on reconstructed CT images have been performed since the early 1990s, and have been applied in various fields. Initially, the images obtained were comparatively rough because they were taken from helical CT[7], but with the introduction of multislice CT, it has become possible to obtain images almost as clear as those obtained in cholangioscopy[8]. This imaging modality has 93% sensitivity in visualizing the biliary tract, 90% sensitivity in visualizing CCs, and 93% sensitivity in the diagnosis of lithiasis[11]. Conventionally, ERCP is considered to be the best imaging modality for CCs, but its application has become less with the appearance of virtual endoscopy[11]. One reason for this is that ERCP is invasive and poses the risk of complications including bleeding, cholangitis or pancreatitis. Moreover, if there is partial or complete obstruction of the bile duct, imaging of the peripheral bile duct may also be poor. Furthermore, since a high volume of contrast medium is needed to visualize CCs, there is a risk of missing small lesions in the biliary mucosa. In the present case, since the end of the common bile duct was completely obstructed, neither ERCP nor direct cholangioscopy could be performed. PTCD cholangiography revealed that there was a relative stricture in the transition site, which was assumed to be present between the left hepatic duct and the intrahepatic bile duct, but was clearly shown in the posterior branch of the bile duct by 3D imaging and virtual endoscopy. These results indicate that 3D imaging and virtual endoscopy can be very useful in understanding the anatomy of the biliary tract.
The basic surgical treatment for type IV-A CCs is as follows[4,12]: (1) the gallbladder and extrahepatic bile duct portions with high carcinogenetic risk are completely removed; (2) if the transition site of the extrahepatic bile duct and intrahepatic bile duct is narrow, bile duct plasty for stricture is performed; (3) if stricture or dilatation is observed in the intrahepatic bile duct, hepatectomy is also performed; and (4) during hepaticoenterostomy, a wide anastomotic stoma is formed to prevent cholangitis due to anastomotic stricture. In the present case, the posterior branch of the bile duct showed partial dilatation from the transition site from the extrahepatic bile duct, and a relative stricture was observed in the transition site. Moreover, according to the virtual endoscopic findings, this was a membrane-like stricture, and bile duct plasty was performed. There was no other stricture or dilatation in the intrahepatic bile duct, thus hepatectomy was not required. In the present case, by confirming blood vessels running around the bile duct using virtual endoscopy, the risk of mistakenly cutting the blood vessels by bile duct plasty could be avoided. To the best of our knowledge, there are no reports considering the overlapping of surrounding blood vessels running on the same image through observation of the bile duct by virtual endoscopy. Since the hepatic artery, and often the portal vein, may become displaced by a dilated cyst, caution is required in performing surgery of CCs. The present results clearly show that CT virtual endoscopy greatly contributes to the diagnosis and treatment of CCs.
The authors are indebted to Mr. Roderick J Turner, Assistant Professor Edward F Barroga and Professor J Patrick Barron of the Department of International Medical Communications of Tokyo Medical University for their review of this manuscript.
Peer reviewer: Michael Leitman, MD, FACS, Chief of General Surgery, Beth Israel Medical Center, 10 Union Square East, Suite 2M, New York, NY 10003, United States
S- Editor Sun H L- Editor Cant MR E- Editor Zheng XM
| 1. | Tashiro S, Imaizumi T, Ohkawa H, Okada A, Katoh T, Kawaharada Y, Shimada H, Takamatsu H, Miyake H, Todani T. Pancreaticobiliary maljunction: retrospective and nationwide survey in Japan. J Hepatobiliary Pancreat Surg. 2003;10:345-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 143] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 2. | Tsuchida A, Kasuya K, Endo M, Saito H, Inoue K, Nagae I, Aoki T, Koyanagi Y. High risk of bile duct carcinogenesis after primary resection of a congenital biliary dilatation. Oncol Rep. 2003;10:1183-1187. [PubMed] |
| 3. | Tsuchida A, Itoi T. Carcinogenesis and chemoprevention of biliary tract cancer in pancreaticobiliary maljunction. World J Gastrointest Oncol. 2010;2:130-135. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 47] [Cited by in RCA: 37] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 4. | Todani T, Narusue M, Watanabe Y, Tabuchi K, Okajima K. Management of congenital choledochal cyst with intrahepatic involvement. Ann Surg. 1978;187:272-280. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 80] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 5. | Singham J, Schaeffer D, Yoshida E, Scudamore C. Choledochal cysts: analysis of disease pattern and optimal treatment in adult and paediatric patients. HPB (Oxford). 2007;9:383-387. [PubMed] |
| 6. | Kawarada Y, Das BC, Tabata M, Isaji S. Surgical treatment of type IV choledochal cysts. J Hepatobiliary Pancreat Surg. 2009;16:684-687. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Saing H, Chan JK, Lam WW, Chan KL. Virtual intraluminal endoscopy: a new method for evaluation and management of choledochal cyst. J Pediatr Surg. 1998;33:1686-1689. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Guo ZJ, Chen YF, Zhang YH, Meng FJ, Lin Q, Cao B, Zi XR, Lu JY, An MH, Wang YJ. CT virtual endoscopy of the ampulla of Vater: preliminary report. Abdom Imaging. 2011;36:514-519. [PubMed] |
| 9. | Simone M, Mutter D, Rubino F, Dutson E, Roy C, Soler L, Marescaux J. Three-dimensional virtual cholangioscopy: a reliable tool for the diagnosis of common bile duct stones. Ann Surg. 2004;240:82-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 27] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 10. | Azuma T, Yamaguchi K, Iida T, Oouhida J, Suzuki M. MR virtual endoscopy for biliary tract and pancreatic duct. Magn Reson Med Sci. 2007;6:249-257. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Singham J, Yoshida EM, Scudamore CH. Choledochal cysts: part 2 of 3: Diagnosis. Can J Surg. 2009;52:506-511. [PubMed] |
| 12. | Singham J, Yoshida EM, Scudamore CH. Choledochal cysts. Part 3 of 3: management. Can J Surg. 2010;53:51-56. [PubMed] |