Published online Apr 7, 2012. doi: 10.3748/wjg.v18.i13.1438
Revised: September 2, 2011
Accepted: January 22, 2012
Published online: April 7, 2012
Liver hydatidosis is a parasitic endemic disease affecting extensive areas in our planet, a significant stigma within medicine to manage because of its incidence, possible complications, and diagnostic involvements. The diagnosis of liver hydatidosis should be as fast as possible because of the relevant complications that may arise with disease progression, involving multiple organs and neighboring structures causing disruption, migration, contamination. The aim of this essay is to illustrate the role of imaging as ultrasonography (US), multi detector row computed tomography, and magnetic resonance imaging (MRI) in the evaluation of liver hydatidosis: the diagnosis, the assessment of extension, the identification of possible complications and the monitoring the response to therapy. US is the screening method of choice. Computed tomography (CT) is indicated in cases in which US is inadequate and has high sensitivity and specificity for calcified hydatid cysts. Magnetic resonance is the best imaging procedure to demonstrate a cystic component and to show a biliary tree involvement. Diagnostic tests such as CT and MRI are mandatory in liver hydatidosis because they allow thorough knowledge regarding lesion size, location, and relations to intrahepatic vascular and biliary structures, providing useful information for effective treatment and decrease in post-operative morbidity. Hydatid disease is classified into four types on the basis of their radiologic appearance.
- Citation: Marrone G, Crino' F, Caruso S, Mamone G, Carollo V, Milazzo M, Gruttadauria S, Luca A, Gridelli B. Multidisciplinary imaging of liver hydatidosis. World J Gastroenterol 2012; 18(13): 1438-1447
- URL: https://www.wjgnet.com/1007-9327/full/v18/i13/1438.htm
- DOI: https://dx.doi.org/10.3748/wjg.v18.i13.1438
Hydatid disease is a worldwide zoonosis caused by the larval stage of the echinococcus tapeworm, that is endemic in many parts of the world (in European, Middle Eastern, Mediterranean, South American and African countries)[1-4]. There are two types of Echinococcus infections: Echinococcus granulosis, the more common type, and Echinococcus multilocularis, the less common but more invasive. Hydatid disease is a relevant health problem in underdeveloped areas where veterinary control does not exist. The most frequent location of hydatid cystic lesions is in the liver (up to 80% of cases), followed by the lung (about 20% of cases), and with a lower reported incidence in any other organ or tissue in the body[1-4].
Dogs or other carnivores are definitive hosts, whereas sheep or other ruminants are intermediate hosts. Humans are secondarily infected by the ingestion of food or water contaminated by dog feces containing the eggs of the parasite. After the ingestion of the eggs, the freed embryo enters a branch of the portal vein by passing through the duodenal mucosa; most of these embryos become lodged in the hepatic capillaries where they either die or grow into hydatid cysts. Some embryos pass through the hepatic capillaries and become lodged in the lungs and other organs.
The definitive diagnosis of liver echinococcosis requires a combination of imaging, serologic, and immunologic studies[4].
At biochemical analysis, there is usually eosinophilia, and a serologic test is positive in 25% of patients[5]. At histopathologic analysis, a hydatid cyst is composed of three layers: the outer pericyst, which corresponds to compressed liver tissue; the endocyst, an inner germinal layer; and the ectocyst, a translucent thin interleaved membrane[5].
Imaging procedures are essential in diagnosis and evaluation of the extent of liver hydatidosis; ultrasound (US), computed tomography (CT), and magnetic resonance (MR) can depict hydathid disease[2-4,6].
The imaging method used depends on the involved organ, and the radiologic findings range from purely cystic lesions to a completely solid appearance[3]. US is the screening method of choice and is also used to monitor efficacy of medical therapy[2-4,6]. CT is always performed because it has a high sensitivity (94%)[7]. It is an important preoperative diagnostic tool to determine vascular, biliary or extrahepatic extension, to recognize complications, such as rupture and infections, and therefore to assess respectability[8-10]. MR is the best imaging procedure to demonstrate a cystic component. It helps to determine vascular or biliary tree involvement, as well as extrahepatic extension[10,11].
There are many potential complications such as exophytic growth, transdiaphragmatic thoracic involvement, peritoneal seeding, biliary communication, portal vein involvement, abdominal wall invasion and hematogenous dissemination in any anatomic location (lung, kidney, spleen, bone, brain)[6,10,11].
The ultrasonographic appearance of hydatid cysts may vary, from a simple aspect to a more complex one, in relation to the stage of evolution and maturity[5-7,10]. US can categorize cysts as solitary univesicular, solitary multivesicular, solid echogenic mass, multiple, either uni- or multivesicular, or collapsed, flattened and calcified[8].
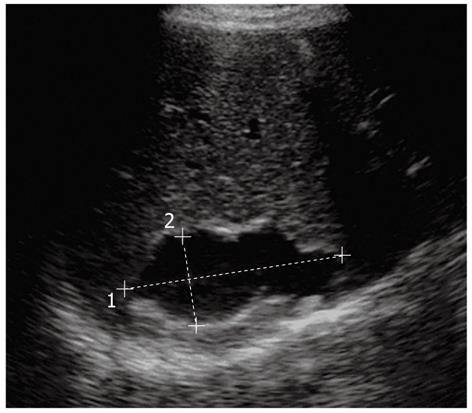
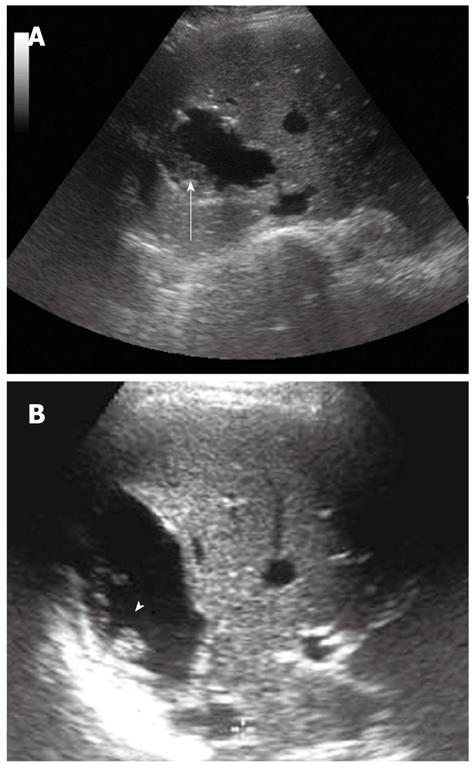
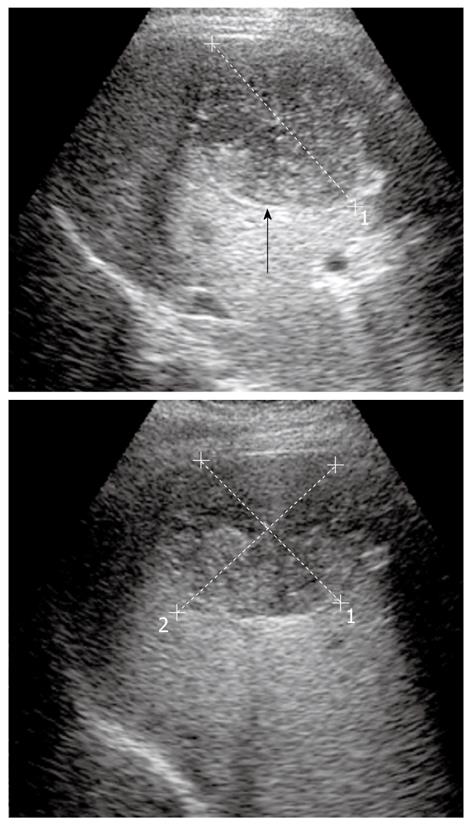
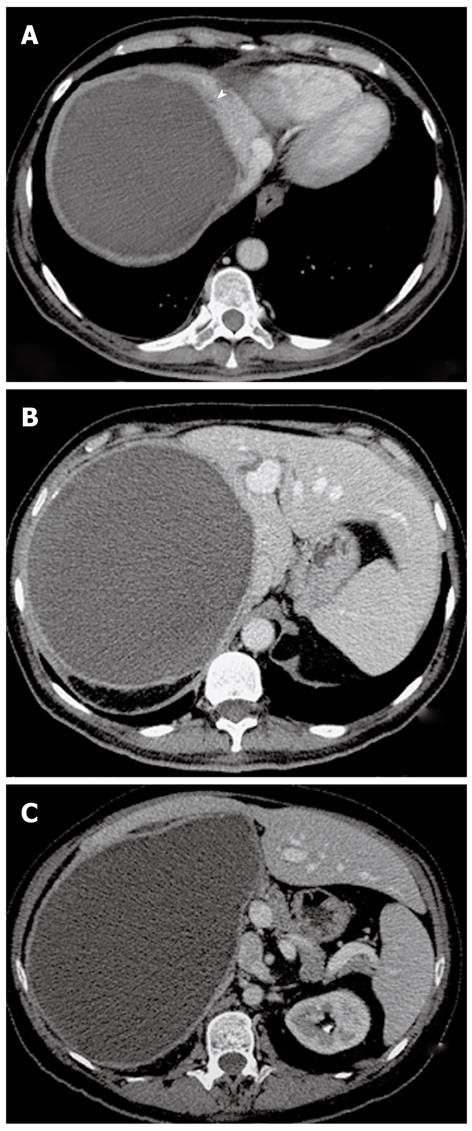
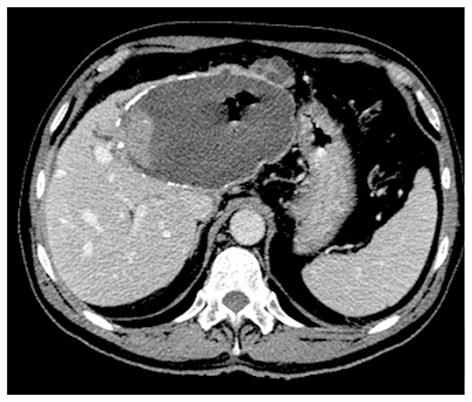
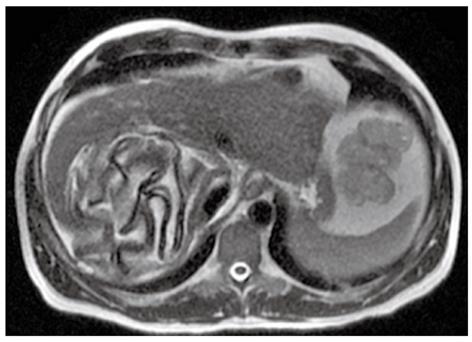
In the first stage, the hydatid cyst may manifest as a well-defined anechoic cyst (Figure 1), an anechoic cyst except for hydatid “sand”[2,6,7]. The more complex aspect is typical of the advanced stages and is related to the presence of multiple internal septa, daughter cysts, multiple echogenic foci and floating membranes inside the cavity (Figures 2 and 3)[7-9]. Membranes may appear as serpentine linear structures, a finding that is highly specific for hydatid disease[7,12,13]. The detachment of the membrane inside the cyst is considered the US “water lily sign”[13-16]. The cyst wall is visible as double echogenic lines separated by a hypoechogenic layer (Figure 3)[16].
Multivesicular cysts manifest as well-defined fluid collections in a honeycomb pattern with multiple septa representing the wall of the daughter cysts. Daughter cysts appear as cysts within a cyst[7-9]. Altering patient’s position may change the position of daughter cysts.
The more complex aspects of hydatid cyst may also mimic solid hepatic masses, and differential diagnosis becomes difficult but fundamental; it is important to look for daughter vesicles or membranes within the lesion that may help in differential diagnosis[7,8]. Cyst calcification is seen in dead hydatid cysts; US shows a hyperechogenic contour with a cone-shaped acoustic shadow[13,15,16].
When the cyst wall is heavily calcified, only the anterior portion of the wall is visualized and appears as a thick arch with a posterior concavity. Partial calcification of the cyst does not indicate the death of the parasite, on the contrary densely calcified cysts may be assumed to be inactive[8,9].
US is considered the preferred investigatory test to monitor efficacy of medical antihydatid therapy because of its low cost[12,14]. Positive response findings include reduction in cyst size, membrane detachment, progressive increase in cyst echogenicity and mural calcification[12].
CT is indicated in cases in which US is inadequate due to patient-related difficulties (obesity, excessive intestinal gas, previous surgery[3,5-7]. CT has high sensitivity and specificity for hepatic hydatid disease[7]. Intravenous administration of contrast medium is useful to give a vascular map to the surgeon, and when complications (especially infection and communication with the biliary tree) and extra-hepatic diffusion are suspected.
CT may show the same findings as US[6,7]. Calcification of the cyst wall, internal septa, floating membranes and daughter vesicles are easily detected at CT[3,5].
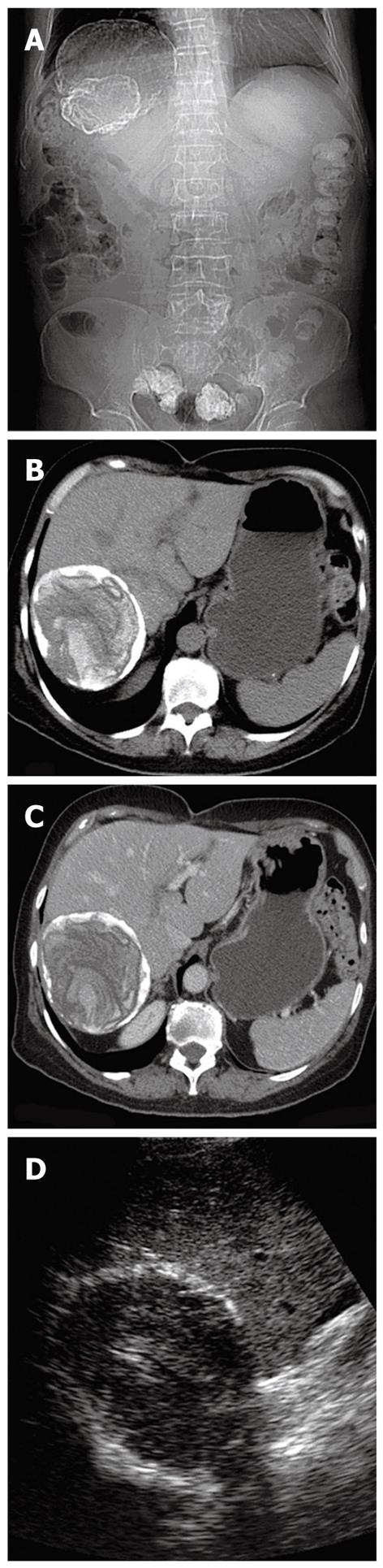
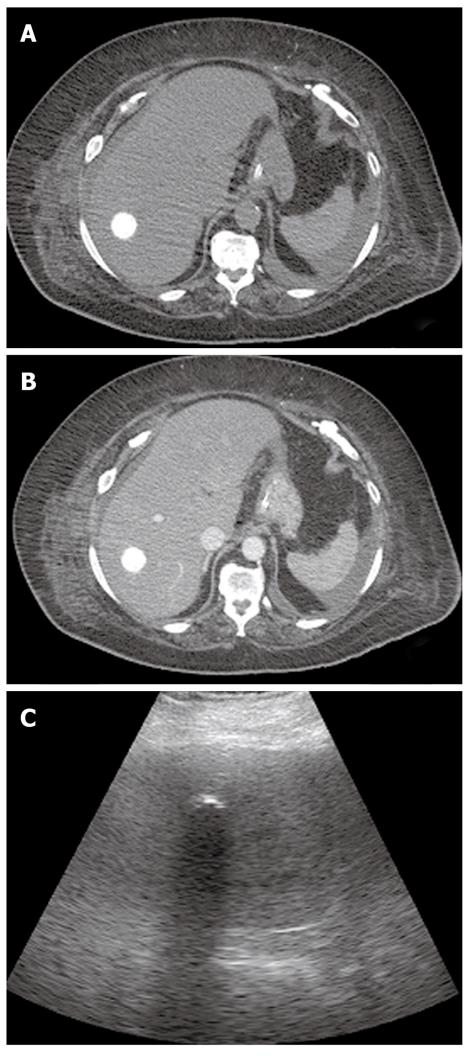
A hydatid cyst typically is seen as a round lesion with water attenuation density, surrounded by a calcified ringlike (Figure 4) or highly attenuated wall, representing the pericyst (Figure 5)[17]. Detachment of the laminated membranes from the pericyst are visualized as linear areas of increased attenuation within the cyst[17].
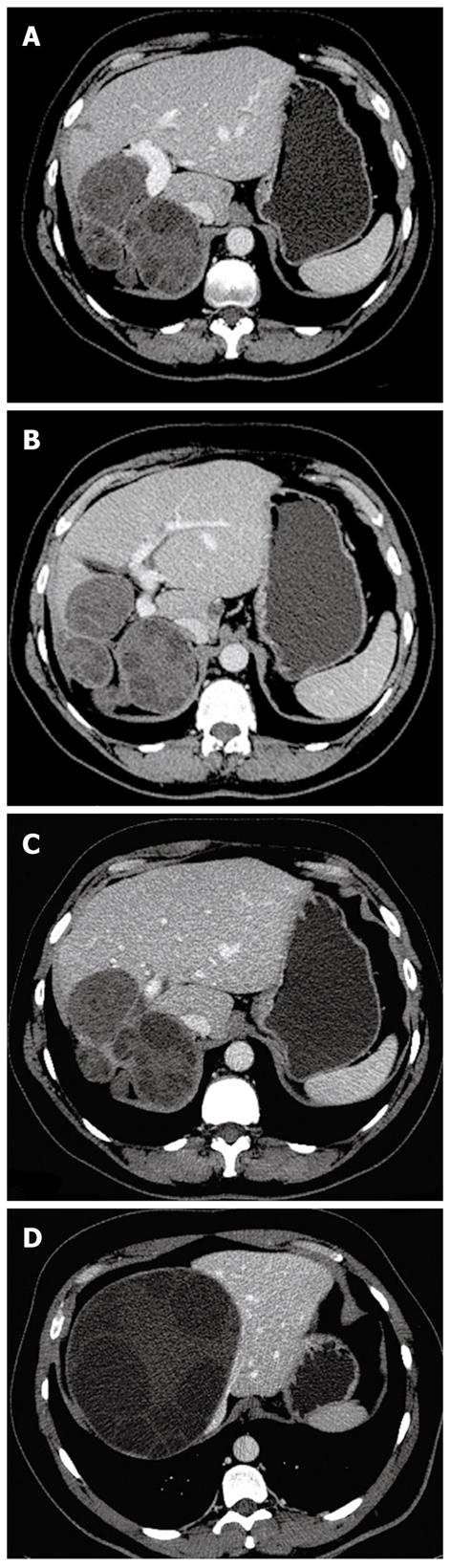
At CT daughter vesicles are visible as round structures located peripherally within the mother cyst; they usually contain fluid with a lower attenuation than that of the fluid of the mother cyst (Figure 6)[5,7].
Contrast-enhanced CT may show the typical high-attenuation rim representing abscesses surrounding the lesion. Sometimes, patchy areas of contras-enhanced liver parenchyma are seen in the vicinity of the lesion, representing inflammatory changes[18].
The dead cysts are totally calcified and at CT they appear as round hyperattenuating areas (Figure 7)[5,7].
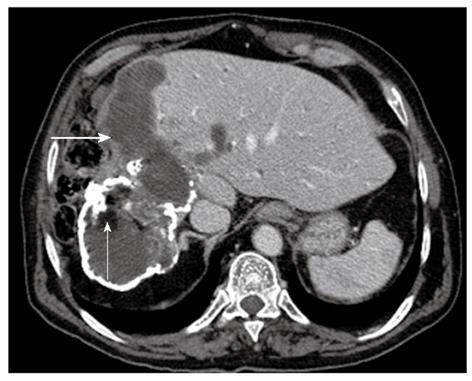
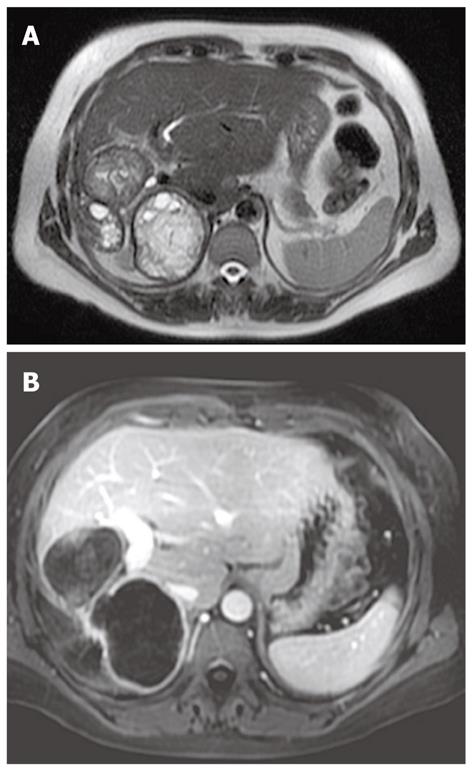
CT also may depict gas or air-fluid levels or fat inside the hydatid cyst, indirect signs of infection and/or communication with the biliary tree (Figures 8 and 9)[6,10,11].
CT is the modality of choice to study extra-hepatic diffusion because it allows imaging of the entire abdomen, pelvis and thorax.
Extra-hepatic diffusion may regard peritoneum, the diaphragm and the thorax cavity, the abdominal wall, the portal system, and the hematogenous dissemination[4,6,7].
MR may be performed to confirm the hypothesis of hepatic hydatidosis and visualize the lesion in different planes. It is the best diagnostic investigation to differentiate the cystic component from the others and to demonstrate a biliary tree involvement[13].
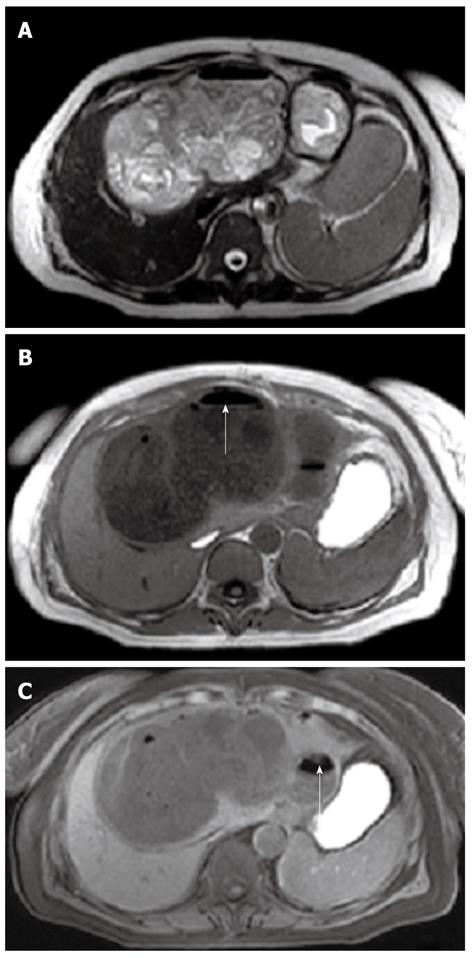
The hydatid cysts may show variable signal intensities on T1- and T2-weighted images, according to the different components inside the lesion[13,17,18].
The necrotic and the fluid components are hypointense on T1-weighted images and markedly hyperintense on T2-weighted images[13,18,19].
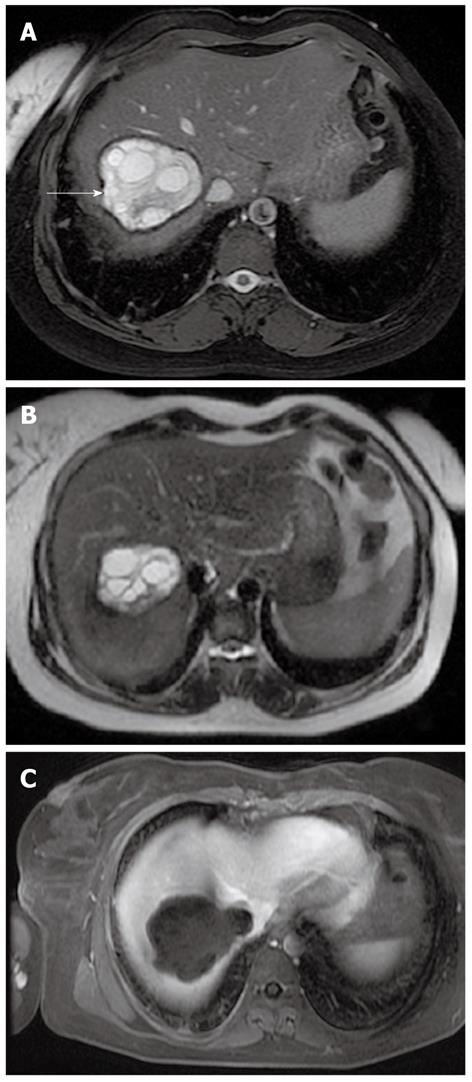
When present the daughter cysts are seen as cystic structures attached to the germinal layer that are hypointense relative to the intracystic fluid on T1-weighted images (Figure 10)[13].
The characteristic sign of hydatid disease is represented by the pericyst that usually appears as a low-signal-intensity rim on T2-weighted images (Figure 10)[17,19].
In addition, there may be an intermediate-signal-intensity inner ring representing the detachment of the membranes[19].
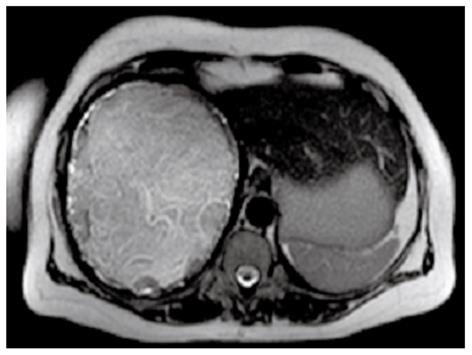
After the i.v. injection of gadolinium contrast agent the pericyst may show slight enhancement (Figure 11).
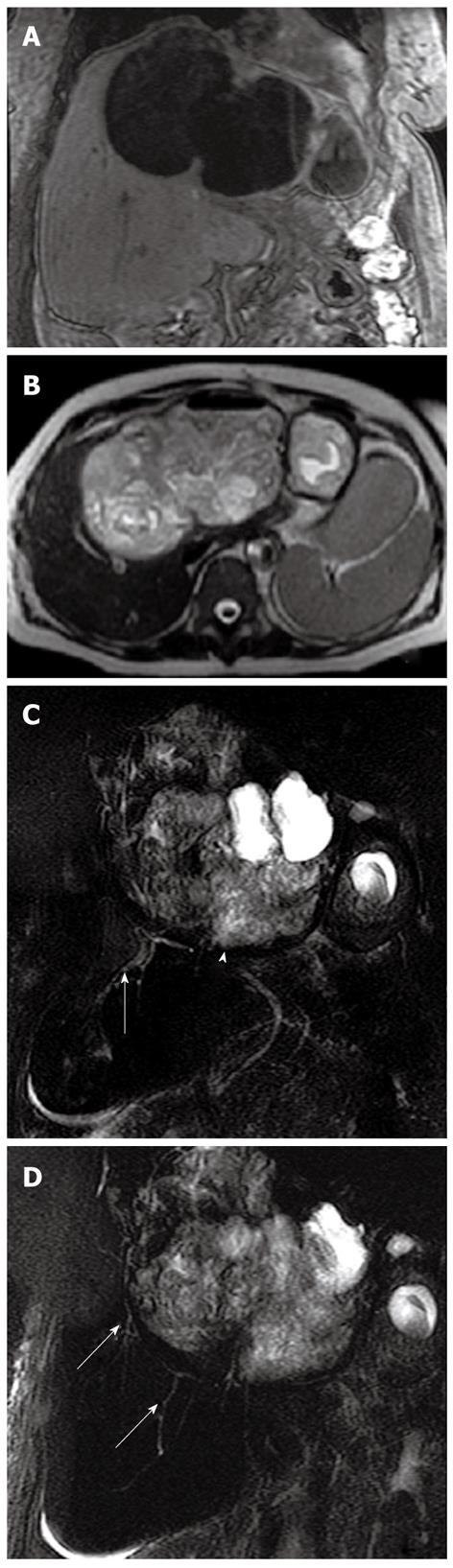
MR is the best diagnostic tool in demonstrating the floating membranes (Figure 12) and irregularities of the rim representing incipient detachment of the membranes (Figure 13)[17,19,20]. On the other hand MR is less sensitive than CT scan in showing cyst wall calcification.
The “snake sign” is another typical MR imaging feature: it represents collapsed parasitic membranes, secondary to damage or degeneration of the hydatid cyst: these membranes have low signal intensity with all sequences (Figure 13).
Intracystic air-fluid level may be visible on MR, as a possible sign of super-infection (Figure 14)[16,21].
MR cholangiopancreatography (MRCP) is useful to study potential involvement of the biliary tree: communication between the cysts and the biliary tree; dilatation of the biliary system secondary to compression of the hydatid cyst[20,21] (Figure 15).
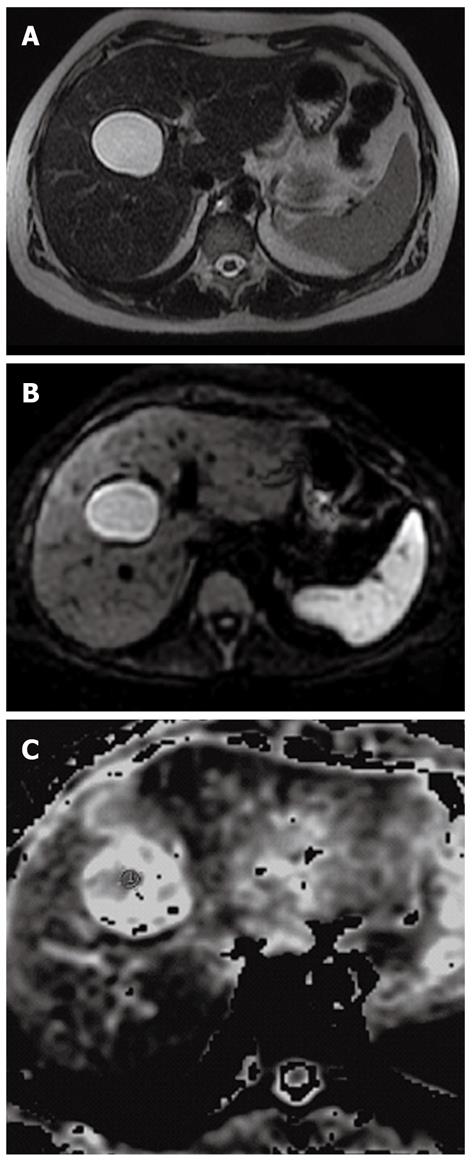
It is known that routine MRI does not adequately differentiate completely liquid hydatid cysts (type I, see following paragraph) from simple cysts: Inan et al[22,23] have demonstrated in their study that diffusion-weighted (DW-MRI), a recent MRI technique, can be helpful in the differential diagnosis.
DW-MRI has long been used exclusively in brain imaging due to technical problems and sensitivity to motion artifacts (caused by cardiac motion and respiration); with the advent of faster sequences, DW-MRI has been applied to abdominal imaging[22,23].
Using DW MRI with a high b factor (1000 s/mm2) the hydatid cysts are hyperintense, whereas none of the simple cysts show significant hyperintensity (Figure 16)[22-24].
In addition, using DW MRI it is possible to calculate a parameter, called the apparent diffusion coefficients (ADCs), that measures the difference in cellular density of hepatic lesions[22-24].
This quantitative parameter can be used to differentiate hydatid cysts from simple cysts. The difference between the ADCs of the hydatid cysts and those of simple cysts can be attributed to the difference in cyst contents[22-24].
Because the hydatid cyst contains viscous hydatid sand that consists of scolices, sodium chloride, proteins, glucose, ions, lipids, and polysaccharides, the ADC of the hydatid cyst is decreased; on the contrary the simple cyst has lower viscosity, hence the higher viscosity. In Inan’s series the mean ADCs of the hydatid cysts was significantly lower (2.5 × 10-3± 0.9) than that of the simple cysts (3.5 × 10-3± 0.5) (Figure 16)[22-24].
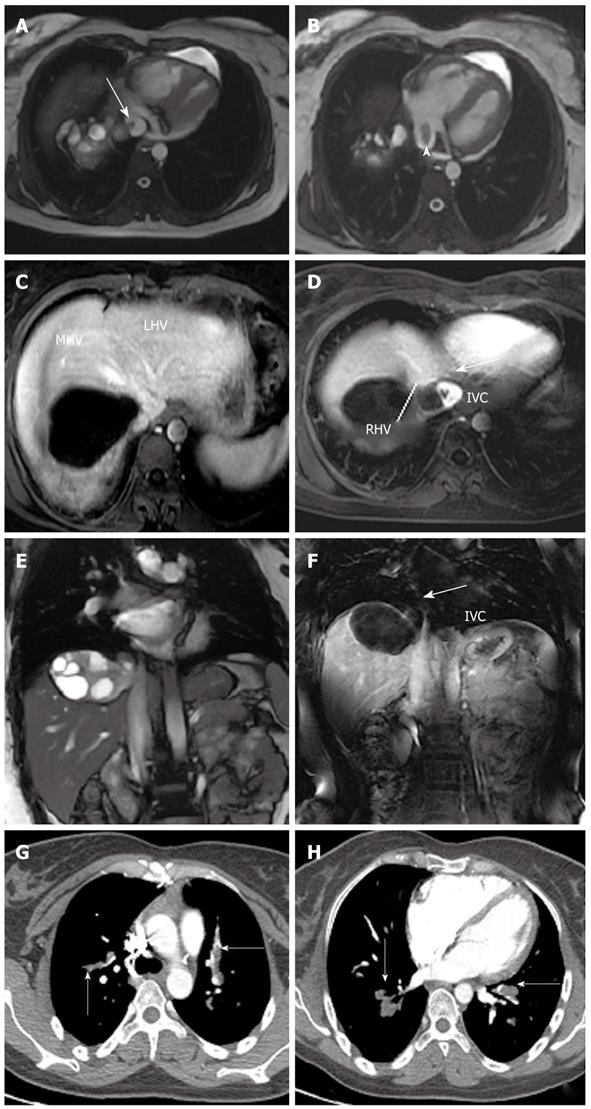
In patients affected by hepatic hydatidosis, contrast enhanced magnetic resonance angiography may be useful in detecting hepatic venous outflow obstruction or thrombosis or invasion[25]; in these patients, pulmonary embolism may be a possible complication (Figure 17)[26].
Hydatid disease is classified into four types on the basis of their radiologic appearance[27]:
Hydatidosis appear at US as a well-defined anechoic mass with or without hydatid sand and septa. Unilocular cysts are considered to be an initial stage in the development of the parasite[28]. A solitary type I cyst may be difficult to distinguish from a simple epithelial cyst[8].
At CT, a type I appears as a well-defined water-attenuation mass; after injection of contrast material the septa and cyst wall enhance, a finding that helps differentiate type I from a simple liver cyst[13,19]. MR images are also similar to those of a simple liver cyst, including hypointensity on T1-weighted images and marked hyperintensity on T2-weighted images; a low signal intensity rim (“rim sign”)[19,20], which is more evident on T2-weighted images, has been described as typical of hydatidosis, and it can be used to differentiate hydatid cysts from simple cysts; this finding represents the pericyst.
Recently the emerging role of DW MRI may play a decisive role in the differential diagnosis of hydatid liver disease and simple cysts[22-24] (Figures 1, 5 and 16).
Daughter cysts are inside the mother cyst, usually arranged at the periphery[15,18]. Floating membranes or vesicles can be also seen in the cyst. Multiple daughter cysts are enclosed together looking like an echogenic solid lesion. (Figures 6, 10, 11 and 12)
Type II may manifest as a well-defined fluid collection in a honeycomb pattern with multiple septa representing the walls of the daughter cysts, creating a “rosette” appearance[15]. Peripheral calcification may occur and involves the pericyst; it is easily detected in CT images as a curvilinear or ring-like structure. CT can distinguish the mother cyst: the average density attenuation of the mother cyst is higher than that of daughter cysts. At MR imaging, daughter cysts may appear hypointense or isointense relative to the maternal matrix on T1 and T2-weighted images[19,20].
Type III lesions are dead cysts with total calcification. At US calcified cysts show strong posterior shadowing, at CT they appear as round hyperattenuating areas, at MR they appear as hypointense areas (Figure 7).
Hydatid complications include rupture and superinfection and may be seen in both type I and type II. CT and MRI play a key role in recognizing the complications such as rupture and infection of cysts associated with hydatid disease.
Ruptures may occur in 50% of cases[6,9,11]; cyst rupture is mainly due to the degeneration of parasitic membranes. Cyst rupture is usually due to the degeneration of parasitic membranes, as a result of age, or a host defense mechanism[6,9,11]. The rupture may be contained, communicating or direct.
Fissures in the cyst wall can be visualized at both CT and MR imaging. Perforation to the biliary tree has been reported in up to 90% of hydatid cysts[7,10,11]. Hydatid cysts may also rupture into pleural and peritoneal cavities. Up to 25% of ruptured cysts may become infected[10,11]. Signs of cyst infection include air-fluid or fluid-fluid levels[9,11] (Figures 8, 9 and 14).
Imaging plays a primary role in liver hydatidosis. It is used for diagnosis, for assessment of extension, for identification of possible complications, for classification and for monitoring the response to therapy. US, MDCT and MR have different roles depending on accuracy in depicting the different goals.
Peer reviewer: Paul E Sijens, PhD, Associate Professor, Radiology, UMCG, Hanzeplein 1, 9713GZ Groningen, The Netherlands
S- Editor Shi ZF L- Editor O’Neill M E- Editor Zhang DN
| 1. | Eckert J, Deplazes P. Biological, epidemiological, and clinical aspects of echinococcosis, a zoonosis of increasing concern. Clin Microbiol Rev. 2004;17:107-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1121] [Cited by in RCA: 1185] [Article Influence: 56.4] [Reference Citation Analysis (1)] |
| 2. | Czermak BV, Akhan O, Hiemetzberger R, Zelger B, Vogel W, Jaschke W, Rieger M, Kim SY, Lim JH. Echinococcosis of the liver. Abdom Imaging. 2008;33:133-143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 85] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 3. | Rozanes I, Güven K, Acunaş B, Emre A. Cystic echinococcal liver disease: new insights into an old disease and an algorithm for therapy planning. Cardiovasc Intervent Radiol. 2007;30:1112-1116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | Filippou D, Tselepis D, Filippou G, Papadopoulos V. Advances in liver echinococcosis: diagnosis and treatment. Clin Gastroenterol Hepatol. 2007;5:152-159. [PubMed] |
| 5. | Mortelé KJ, Ros PR. Cystic focal liver lesions in the adult: differential CT and MR imaging features. Radiographics. 2001;21:895-910. [PubMed] |
| 6. | Pedrosa I, Saíz A, Arrazola J, Ferreirós J, Pedrosa CS. Hydatid disease: radiologic and pathologic features and complications. Radiographics. 2000;20:795-817. [PubMed] |
| 7. | Polat P, Kantarci M, Alper F, Suma S, Koruyucu MB, Okur A. Hydatid disease from head to toe. Radiographics. 2003;23:475-494; quiz 536-537. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 345] [Cited by in RCA: 342] [Article Influence: 15.5] [Reference Citation Analysis (0)] |
| 8. | Lewall DB. Hydatid disease: biology, pathology, imaging and classification. Clin Radiol. 1998;53:863-874. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 111] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 9. | Mortelé KJ, Segatto E, Ros PR. The infected liver: radiologic-pathologic correlation. Radiographics. 2004;24:937-955. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 277] [Cited by in RCA: 203] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 10. | Lim JH. Parasitic diseases in the abdomen: imaging findings. Abdom Imaging. 2008;33:130-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Turgut AT, Altin L, Topçu S, Kiliçoğlu B, Aliinok T, Kaptanoğlu E, Karademir A, Koşar U. Unusual imaging characteristics of complicated hydatid disease. Eur J Radiol. 2007;63:84-93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 65] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 12. | Scherer K, Gupta N, Caine WP, Panda M. Differential diagnosis and management of a recurrent hepatic cyst: a case report and review of literature. J Gen Intern Med. 2009;24:1161-1165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 13. | Coşkun A, Oztürk M, Karahan OI, Erdogan N, Işin S, Güleç M. Alveolar echinococcosis of the liver: correlative color Doppler US, CT, and MRI study. Acta Radiol. 2004;45:492-498. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 19] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 14. | Hosch W, Junghanss T, Werner J, Düx M. [Imaging methods in the diagnosis and therapy of cystic echinococcosis]. Rofo. 2004;176:679-687. [PubMed] |
| 15. | Turgut AT, Akhan O, Bhatt S, Dogra VS. Sonographic spectrum of hydatid disease. Ultrasound Q. 2008;24:17-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 28] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 16. | Caremani M, Lapini L, Caremani D, Occhini U. Sonographic diagnosis of hydatidosis: the sign of the cyst wall. Eur J Ultrasound. 2003;16:217-223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 17. | Katranci N, Elmas N, Yilmaz F, Mentes A. Correlative CT, MRI and histological findings of hepatic Echinococcus alveolaris: a case report. Comput Med Imaging Graph. 1999;23:155-159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 18. | Marani SA, Canossi GC, Nicoli FA, Alberti GP, Monni SG, Casolo PM. Hydatid disease: MR imaging study. Radiology. 1990;175:701-706. [PubMed] |
| 19. | Vilgrain V. [Cystic lesions of the liver]. Gastroenterol Clin Biol. 2001;25:B167-B177. [PubMed] |
| 20. | Kodama Y, Fujita N, Shimizu T, Endo H, Nambu T, Sato N, Todo S, Miyasaka K. Alveolar echinococcosis: MR findings in the liver. Radiology. 2003;228:172-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 109] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 21. | Mendez Montero JV, Arrazola Garcia J, Lopez Lafuente J, Antela Lopez J, Mendez Fernandez R, Saiz Ayala A. Fat-fluid level in hepatic hydatid cyst: a new sign of rupture into the biliary tree? AJR Am J Roentgenol. 1996;167:91-94. [PubMed] |
| 22. | Oruç E, Yıldırım N, Topal NB, Kılıçturgay S, Akgöz S, Savcı G. The role of diffusion-weighted MRI in the classification of liver hydatid cysts and differentiation of simple cysts and abscesses from hydatid cysts. Diagn Interv Radiol. 2010;16:279-287. [PubMed] |
| 23. | Inan N, Arslan A, Akansel G, Anik Y, Sarisoy HT, Ciftci E, Demirci A. Diffusion-weighted imaging in the differential diagnosis of simple and hydatid cysts of the liver. AJR Am J Roentgenol. 2007;189:1031-1036. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 49] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 24. | Chan JH, Tsui EY, Luk SH, Fung AS, Yuen MK, Szeto ML, Cheung YK, Wong KP. Diffusion-weighted MR imaging of the liver: distinguishing hepatic abscess from cystic or necrotic tumor. Abdom Imaging. 2001;26:161-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 135] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 25. | Haliloglu N, Erden A. Hepatic venous outflow obstruction after hydatid cyst surgery: evaluation with contrast enhanced magnetic resonance angiography. Eur J Gastroenterol Hepatol. 2009;21:776-780. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 26. | Menassa-Moussa L, Braidy C, Riachy M, Tabet G, Smayra T, Haddad-Zebouni S, Ghossain M, Aoun N. [Hydatid disease diagnosed following a pulmonary embolism]. J Mal Vasc. 2009;34:354-357. [PubMed] |
| 27. | Precetti S, Gandon Y, Vilgrain V. [Imaging of cystic liver diseases]. J Radiol. 2007;88:1061-1072. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 28. | Ermis F, Dursun M, Akyüz F, Bakir B, Güven K. Hydatid cysts: three different stages on the same image. Intern Med. 2007;46:1673. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |